Literature Review on the use of the Pupillometer
advertisement

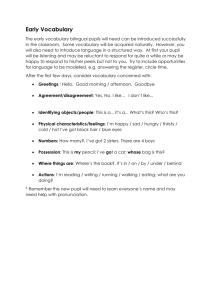
Literature Review Article Meeker M, Du R, Bacchetti P, Privitera C, Larson M, Holland M, Manley G. (2005). Pupil examination: Validity and clinical utility of an automated pupilometer.Journal of Neuroscience Nursing, 37(1). Chen J., Gombart Z., Rogers S., Gardiner S., Cecil S., Bullock R. (2011). Pupillary reactivity as an early indicator of increased intracranial pressure: The introduction of neurologic pupil index. Surgical Neurology International, 2(1), 82-86. Number of Subjects 20 randomly selected patients, ages 4-87, who were in the ICU of the San Francisco General Hospital. Clinical Outcomes A manual exam may assess pupil size accurately; distinguishing from a brisk or nonreactive pupil is problematic. The manual exam has a median error in pupillary size measurement (0.55mm) that is 2x that of the Pupilometer (0.23mm) -more susceptible to errors and differences 134 patients in the ICU at eight different clinical sites Pupillary signs could be detected earlier with a portable infrared Pupilometer Pts who had continuous or sporadic abnormal pupil reactivity, as defined by NPi, also had peaks of sustained ICP. The use of the Pupilometer and NPI value provides a rapid and non-invasive method for screening and triage of patients with suspected increased ICP. Conclusions “Performing frequent pupil assessments provides critical and time-sensitive information regarding new or worsening intracranial pathology; therefore, an accurate examination is essential”. “Automated Pupilometry may be useful in providing ICU nurses with a precise and reliable measurement or pupil size and reactivity.” Using NPi there was an inverse relationship between decreasing pupil reactivity and increasing ICP. Using NPI may be a useful tool in the early management if pts with causes of increased ICP. Values can help determine pupillary reactivity and may have clinical relevance in guiding neuroprotective and neurosurgical interventions. Fountas, K., Kapsalaki, E., Machinis, T., & Boev, A. (2006). Clinical implications of quantitative infrared pupillometry in neurosurgical patients. Neurocritical Care,5. Full literature review to apply clinical findings in the assessment of neurological diseases. Pupillometer can produce accurate, reproducible pupillary measurements, superior to the manual exam. Limiting factors include: amyloidosis, Horner’s Syndrome, familial dysautonomia, MS, migraines, morphine, tramadol, fentanyl. “The development of a portable, automated, infrared Pupilometer has recently transformed pupillary parameter measuring from a subjective and highly variable methodology to an accurate and reproducible one”. “Meticulous standardization Taylor, W., Chen, J., Meltzer, H., Gennarelli, T., Kelbch, C., Knowlton, S., . . . Marshall, L. (2003). Qualtitative pupillometry, a new technology: Normative data and prelimary observations in patients with acute head injury. J Neurosurg, 98, 205213. More clinical studies are needed to identify and support Pupilometer parameters The data obtained with parameters routinely used in patient assessment at the bedside can be quantitatively measured and are useful in assessing brain volume. of the technique can minimize the observed variations”. “The pupillometer is a reliable and safe method that provides detailed and accurate information regarding patterns of pupillary responsiveness”. CV is sensitive to elevations in ICP and resistant to large doses of morphine and propofol. - Likelihood that the ICP will become elevated in 20 pts seen in cardiology 15-30 minutes with a clinic receiving CaCh CV below 0.6 blockers and/or narcotics %CH of less than 10% was always associated with an 26 pts with ABI whom increase in ICP above 20mmHg ICP was continuously monitored. “There is a relationship with an ICP above 20 mmHg, and a reduction in CV. A percentage of reduction in pupil size of less than 10% following stimulation is strongly associated with increases in brain volume”. 310 healthy volunteers under a variety of light conditions. 17 pts undergoing nonintracranial surgical procedures or endoscopic procedures with no history of IC or opthalmological disease who are receiving IV morphine. Early detection of changes in brain volume with the use of the Pupilometer may reduce the mortality rate.