File - Prepared Rescuer, LLC
advertisement

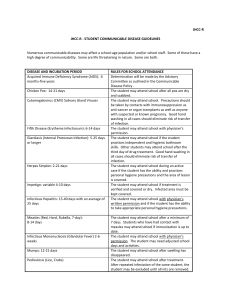
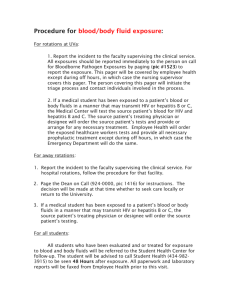
PREHOSPITAL PROVIDERS INFECTION CONTROL GENERAL GUIDELINES & POST-EXPOSURE PROPHYLAXIS (PEP) (References: CDC, Massachusetts CMRs, NIOSH, OSHA 2013) PURPOSE In accordance with State and National regulations, these guidelines have been developed to standardize prehospital infection control prevention and education. This document provides general guidelines and procedures for prehospital personnel, to reduce risk of infectious disease exposure to themselves and patients, and to evaluate and report suspected exposures to communicable diseases. Apparently healthy persons may carry and be capable of transmitting disease in blood and body fluids. Precautions in this policy are intended to provide providers with information to safely care for all patients, regardless of known disease status. Equipment and education must be consistent with national standards including reporting of concern for exposure/contamination and use of designated infection control officers (DICOs) in each agency. Standard practice for all patient contacts should emphasize body substance isolation and, as appropriate, respiratory isolation procedures. Standard Precautions: Good hand hygiene, gloves, gown, face shield/eye protection as indicated by patient care activities and risk of exposure to blood/body fluids. Aerosol / Airborne / Droplet Precautions: When medically essential, all EMS personnel engaged in aerosol generating activities (i.e. advanced airways) should follow airborne precautions including utilizing a fittested disposable N95 respirator or powered air purifying respirator [PAPR], gloves, eye protection, gown plus standard precautions. Droplet precautions also include a face / surgical mask for all direct patient care activities on provider and patient (if feasible). Each agency is responsible for meeting OSHA standards in infection control screening, tracking, training, and equipment procedures to prevent cross contamination during patient care or transport where risk of exposure includes: aerosol, airborne, droplet; Blood and body fluid (BBF); Closed environments (limited ventilation / air circulation); Disaster / mass casualty situations; and Situational awareness. EXPOSURE DEFINITION A significant communicable disease exposure is defined by criteria set by the CDC including: 1. Contact with blood, tissues, or body fluids containing blood on non-intact skin or mucous membranes. 2. Contaminated needle stick injury 3. Unprotected mouth-to-mouth resuscitation 4. Face-to-face contact in restricted ventilation areas in patients with airborne communicable diseases ASSESSING NEED FOR OCCUPATIONAL EXPOSURE FOLLOW-UP 1. Exposure Type: a. Percutaneous b. Mucous membrane c. Non-intact skin (i.e. rash, abrasion) d. Bites resulting in blood exposure to either person 2. Type and Amount of Fluids / Tissue a. Blood or fluids containing blood b. Other potentially infectious material (OPIM) including CSF, synovial, pleural, peritoneal, pericardial and amniotic fluids 3. Source Infectious Status a. Presence of HBsAg (hepatitis B surface antigen), HBeAg (hepatitis B envelope antigen which indicates highly infectious) b. Presence of HCV antibody (hepatitis C antibody) c. Presence of HIV antibody 4. Exposed Provider Susceptibility a. Hepatitis B vaccine and vaccine response status b. HBV, HCV abd HIV immune status EXPOSURE RISK REDUCTION 1. Providers a. Follow agency’s policies and procedures for infection control. b. Universal precautions must be employed for all patient contacts. Additional barrier precautions used based on potential for exposure to BBF and OPIM. c. Hand-washing prior to and following patient contact (minimum), regardless of use of gloves or other barrier precautions. Thorough hand washing with soap and water is the most effective infection control activity for providers. Waterless hand sanitizers are an option if soap and water not available and there is no debris contamination. d. Adequate ventilation is important for air quality. If feasible, while transporting a patient with acute febrile respiratory illness, keep vehicle windows open and set heating and air-conditioning systems on a non-recirculating cycle. Notify receiving healthcare facility so appropriate infection control precautions taken prior to patient arrival. e. Place a mask on patients with possible airborne diseases and have them cover mouth/nose when coughing. Facemasks are often problematic for children to wear consistently. f. Standard plus droplet precautions should be used for patients with acute febrile respiratory illness i.e. suspected or confirmed influenza. 2. Provider Agency a. Each agency must comply with all federal, state and local regulations regarding infectious disease precautions. b. Agency must establish and maintain a written exposure control plan designed to eliminate or minimize employee exposures. This readily accessible plan should include procedures utilized if an employee is exposed to a communicable disease. c. Designates an ICO to evaluate and respond to provider disease exposure. d. Make available equipment, supplies and training necessary for providers to reasonably protect themselves and patients against infectious disease exposure. 3. Receiving Facility a. Receiving hospitals should have procedures for evaluating exposed providers in assessing significance of exposure and the need for / provision of prophylaxis. b. Appropriate testing to determine if source patient infected with a communicable disease. c. Provide recommendations for post-exposure prophylaxis and further evaluation. CDC RECOMMENDED POST-EXPOSURE PROPHYLAXIS RECOMMENDATIONS (see Appendix B) CDC recommendations used for HIV and hepatitis prophylaxis following significant exposures. Prehospital Agencies, DICOs, occupational injury treatment centers and hospitals must coordinate efforts to ensure rapid evaluation and treatment for providers with high-risk exposures. 1. Provider: a. Immediately notify DICO and supervisor of actual or suspected exposure. b. Standardized exposure form should be completed by the EMS provider or DICO in additional to any hospital/clinic paperwork (see Appendix A) c. After initial treatment and decontamination, provider will document patient contact in which potential exposure occurred. A copy of all paperwork should be provided to the hospital, patient, and agency’s DICO. All treatments, recommendations and follow-up care must also be documented, with copies of the treatment plan going to each of the above individuals. This information is confidential and must be HIPPA compliant. d. Each agency will be responsible for completing their own feedback loop to the affected EMS personnel through the agencies' infection control officer. e. Recommendations for the contents of the occupational exposure report: i. Date and Time of exposure ii. Details of the procedure being performed, including when and how the exposure occurred. If related to a “sharp”, the type / brand should also be noted, in addition to when the exposure occurred (i.e. after venipuncture). 2. 2. iii. Details of the exposure, including tyle and amount of fluid / material and severity of exposure (i.e. depth of injury & if fluid injected). iv. Details (if known) about exposure source, i.e. known HBV, HIV, HCV. If HIV positive, stage of disease, antiretroviral medications and viral load, and ID physician. v. Details about the exposed provider, including vaccination status. vi. Details regarding counseling, PEP / management and recommended follow-up. Employer/Agency a. Assess potential exposure to determine if meets “exposure” definition. b. Assure provider with suspected exposure instructed to report immediately to emergency department, or other health treatment facilities for risk assessment and determination of need for post-exposure prophylaxis (PEP). In situations where exposed individual does not report to the hospital that received the source patient, the form should be faxed to that receiving Hospital’s ED Charge Nurse. c. If there is a significant exposure (i.e. an entire crew exposed to bacterial meningitis) the DICO should notify all providers by phone, in addition to completing and submitting the necessary forms. Receiving Hospital a. Receiving hospitals should have procedures for evaluating exposed providers in assessing significance of exposure and the need for / provision of prophylaxis. b. Appropriate testing to determine if source patient infected with a communicable disease. i. Known Source: 1. Test for HBsAg, anti-HCV, HIV antibody (rapid screen if available) 2. Direct virus assays for routine screening not recommended. 3. If source not infected with BBP, baseline testing or further follow-up of exposed provider not necessary. 4. If source refuses testing, or unknown test results, consider clinical symptoms and presence of high-risk behaviors (i.e. IVDA). 5. Discarded needles cannot be tested without source’s permission. ii. Unknown Source: 1. Evaluate likelihood of exposure to source at high risk for infection 2. Consider likelihood of BBP infection among patients in exposure setting (i.e. mass casualty with significant blood exposure). c. Provide recommendations for post-exposure prophylaxis and further evaluation. Expert consultation with an Infectious Disease Specialist may be necessary (see the CDC website www.cdc.org for current recommendations). DISPOSAL OF USED/CONTAMINATED EQUIPMENT/SUPPLIES 1. All providers will observe disposal guidelines at all times without exception. 2. All used disposable equipment and supplies that have come into direct or indirect contact with a patient shall be placed in designated contaminated waste receptacles at the receiving facility, or at the provider's base of operations. 3. All used or exposed needles must be placed in designed sharps containers immediately after use. Containers should be located in transport vehicles and at receiving facilities. Disposal of sharps containers determined by agency contracts.. 4. Failure to utilize proper disposal methods or containers by providers shall result in education and / or remediation. Failure by the employing agency to correct repeated infractions shall result in a formal grievance. OCCUPATIONAL EXPOSURE MANAGEMENT RESOURCES National Post-Exposure Prophylaxis Hotline (PEPLine): 1-888-448-4911. Website: www.ucsf.edu/hivcntr Needlestick!: www.needlestick.mednet.ucla.edu Hepatitis Hotline: 1-888-443-7232. Website: www.cdc.gov/hepatitis To Report to the CDC or Confirm Current PEP Guidelines: 1-800-893-0485. Website: www.cdc.gov HIV Antiretroviral Pregnancy Registry: 1-800-258-4263. Website: www.glaxowellcome.com HIV/AIDS Treatment Information Service: www.hivatis.org NOTIFICATION OF POSSIBLE COMMUNICABLE DISEASE EXPOSURE Notify shift supervisor and / or DICO immediately upon possible exposure. Provider Name: Employer: Employer Address: Home Phone: ___________________________ ___________________________ ___________________________ ___________________________ __Completed hepatitis B series Date/Time: Work Phone: Employer Fax: Email: __Partial hepatitis B series ___________________ ___________________ ___________________ ___________________ __No hepatitis B vaccinations Source Name: Address: Unknown: ___________________________ ___________________________ ___________________________ Source DOB: Home Phone: ___________________ ___________________ Known (Circle): HIV/AIDS Hepatitis B Hepatitis C Tuberculosis Meningitis Other: ________________________________________________ Incident Location: _________________________________________________________________ Incident Date / Time: _________________________________________________________________ PCR # Source: ___________________________ PCR # Provider: ___________________ Source Destination: _________________________________________________________________ Provider Destination: ___________________________________________________________________ Exposure Type: __Needle stick (circle): Hollow Solid Used Clean __Blood / OPIM exposure to (circle): Eyes Mouth Non-Intact Skin __Meningitis (circle): Suspected Confirmed __Close exposure to (circle): Known TB Suspected TB __Other: _____________________________________________________________________________ Describe Incident: ______________________________________________________________________ _____________________________________________________________________________________ _____________________________________________________________________________________ _____________________________________________________________________________________ _____________________________________________________________________________________ _____________________________________________________________________________________ PPE used during exposure (circle): Standard Precautions Gloves Gown Face shield Other Eye protection N95 mask Other: _______________________________________________________________________________ Occupational Health Provider: ___________________________________________________________ Address: ______________________________________ Phone Number: ___________________ Name of person completing form: _________________ Date / Time: ___________________ Occupational Health Follow-Up Date/ Time: ___________________ __No reportable communicable disease identified in source person __Recommendations given to Employee with copies for employee and DICO __Further Actions: _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ APPENDIX B: The following recommendations are taken from the “Updated U.S. Public Health Service Guidelines for the Management of Occupational Exposures to HBV, HCV, and HIV and Recommendations for Postexposure Prophylaxis” MMWR. 2001. www.cdc.gov/mmwr/preview