Therapeutics 202 Small Group Discussion Case 4B Asthma
advertisement

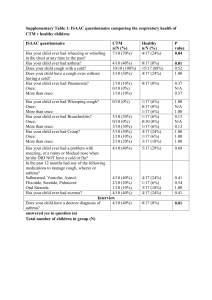
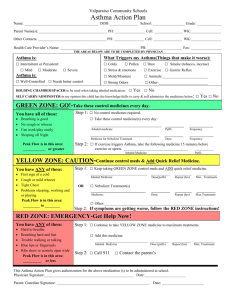
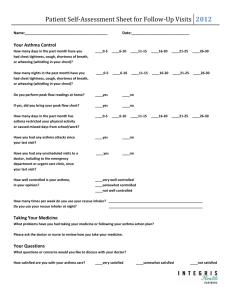
Therapeutics 202 Small Group Discussion Case 4B Asthma November 15, 2010 Submitted: November 22, 2010 Jason Arboleda Victor Arcega Kirth Asis Oyayi Atienza-Arellano Reysa Autentico Armando Balasbas Denise Nicole Baquiran Manuel Miguel Barnes Angelica Barrenechea Ray Anthony Bartolome Reinzi Luz Bautista Rachelle Dianne Benavidez Rhey Ian Buluag June Cathleen Castillo Reno Eufemon Cereno Case Summary: Willie Villamin, 3 year old male Chief complaint: clear rhinorrhea, nasal congestion and sneezing with continuous coughing ending up with vomiting of clear phlegm History of present illness: 2 month PTC, occasional cough Cough and wheezing occurs once every other week lasting less than 5 minutes Nocturnal cough happened only once a month Appetite and level of activity for the past 2 months are normal Family History and Personal/Social history not provided. Pertinent findings in physical examination: HR=90 RR=20 Temp=37.8 Nasal turbinates with clear and watery nasal discharge No cervical lymphadenopathy, erythematous tonsils, intercostals retractions Occasional wheezing on both lung fields Step 1. Define the Patient’s Problem Based on the data gathered from history and physical examination, several differential diagnoses can be made. Viral upper respiratory tract infection can be considered because of the patient’s slightly elevated temperature, cough, and rhinorrhea. However, since the patient has been experiencing the cough for 2 months already, a viral etiology may not be enough to cause the patient’s symptoms. Also, the wheezing heard upon physical examination may not point to a viral etiology of cough. We can also consider gastroesophageal reflux disease because cough is a common symptom in GERD. However, the patient does not experience heartburn and his appetite has been normal for the whole duration of the cough. Episodic wheezing and cough may be a strong consideration because this differential is common in the patient’s age group. The group also considered rhinosinusitis because of clear rhinorrhea, nasal congestion, cough, and wheezing. Tuberculosis was also considered because of cough, but it was immediately ruled out because of the absence of cervical lymphadenopathy on physical examination. Foreign body aspiration was also considered since it also presents with cough and wheezing. However, the other symptoms cannot be explained by this. Our strongest consideration for this case is asthma. The following are the reasons for the diagnosis: Wheezing more than once a month Nocturnal cough in periods without viral infection According to the GINA 2009 Guideline on Asthma Management and Prevention in Children 5 years and Younger, the following characteristics, when present in a patient are highly suggestive of the diagnosis of asthma: Wheezing more than once a month Activity induced cough Nocturnal cough in periods without viral infections Absence of seasonal variation in wheeze 1 Symptoms that persist after age 3 Wheeze plus one major risk factor (parental history of asthma or eczema) Wheeze plus two of three minor risk factors (eosinophilia, wheezing without colds, allergic rhinitis) The GINA 2009 on patients younger than 5 years old admits that diagnosing asthma is hard since it is difficult to perform diagnostic examinations on them so a trial of treatment with short-acting bronchodilators and inhaled glucocorticoids are sometimes done. As for our patient, we are committing on the diagnosis of asthma because of the reasons stated above. Apart from asthma, the group also speculated that the diagnosis may be asthma complicated by viral upper respiratory tract infection. However, this was disproved because of the time component. The group also considered asthma with allergic rhinitis because the presence of clear rhinorrhea, nasal congestion, and sneezing define allergic rhinitis. Primary Working Impression: Bronchial asthma, mild intermittent, not in acute exacerbation, to consider allergic rhinitis. The patient was classified under mild intermittent because: Frequency of symptoms (no more than 2 days per week) Frequency of nighttime awakenings with asthma symptoms (no more than 2 times per month) Use of a quick-relief inhaler (no more than 2 days/week) – N/A How much asthma interferes with daily activities (not at all) Peak flow readings (normal between asthma attacks) – not assessed Whether asthma flares require use or oral steroids (no more than once a year) – N/A As of now, we are still considering allergic rhinitis because of the symptoms presented. It also has a strong consideration for our case since a huge percentage of patients with asthma also have allergic rhinitis. Diagnosis cannot be confirmed as of the moment because it will be inconvenient for our patient to undergo a skin test because of his age. Instead, symptomatic treatment is suggested. Step 2. Therapeutic Objectives 1. 2. 3. 4. To come up with a therapeutic plan depending on the asthma severity a. To provide symptom relief b. To prevent future exacerbations To establish trust between the patient, the doctor, and the parents to ensure quality patient care and compliance To identify and reduce trigger factors To educate the patient and the caregivers a. To provide important information about the disease itself b. To teach the patient and caregivers on the proper use of inhalers c. To educate the caregivers on red flags that they must watch out on Step 3. Choosing the P-Drug Patients with mild intermittent asthma must be treated with a reliever medication according to the GINA guidelines. Inhaled therapy is the cornerstone of asthma treatment for children of all ages. An appropriate device must be selected since different inhalers have different indications based on age. The choice of inhaler must be individualized in children for treatment to be effective. For children less than 4 years of age, the preferred device is pressurized meter dose inhaler plus a dedicated spacer with face mask. A nebulizer with face mask may also be used as an alternative (GINA, 2009). 2 Table 1. Different drug classes of asthma relievers DRUG CLASS EFFICACY SAFETY SUITABILITY COST Inhaled ++++ ++++ ++++ ++++ Oral +++ +++ +++ ++++ Anticholinergic +++ ++++ 0 ++ Epinephrine ++++ + + +++ Theophylline ++ + + +++ SABA The table above shows the different classes of drugs that can be used as relievers. Inhaled rapid acting beta-2 agonists get a grade of 4+. According to the GINA guidelines, they are the most effective group of bronchodilators available. Oral SABAs are less effective as compared to the inhaled route. Epinephrine also gets a grade of 4+ since its efficacy in terms of bronchodilation is comparable to the inhaled rapidly acting beta-2 agonists. Anticholinergic agents and theophylline are inferior to inhaled rapidly acting beta agonists in terms of efficacy as a reliever. When comparing the safety of the different groups of relievers, inhaled rapidly acting beta agonists and inhaled anticholinergics have the highest scores. Inhaled rapidly acting beta-2 agonists provide rapid relief at lower doses with fewer side effects as compared to the oral SABAs. Inhaled anticholinergics are also relatively safe since the route of administration decreases the risk of systemic toxicity. Epinephrine and theophylline have low scores in terms of safety profile. Epinephrine, given intravenously, is associated with higher rates of adverse events while theophylline has a narrow margin of safety. Inhaled rapidly acting beta-2 agonists were given a grade of 4+ under the suitability criterion. According to the GINA guidelines, this group is the preferred treatment for acute asthma in children of all ages. Oral SABAs are rarely needed and are reserved for children who cannot use inhaled therapy. Inhaled anticholinergics are not recommended for the long term management of children with asthma (GINA, 2009). Epinephrine’s route of administration makes this drug not suitable for children. This gives it a low grade under the suitability criterion. Theophylline’s narrow margin of safety is also not appropriate for children. Aside from this, theophylline comes in tablet and syrup preparations which are less suitable as compared to inhaled agents, especially during acute asthma attacks. Thus, score for the suitability criterion is also low. Since the other groups of drugs aside from rapidly acting beta-2 agonists are not suitable for this patient, ranking under the cost criterion is not necessary. However, for discussion purposes, cheaper drugs have higher scores and the more expensive drugs receive lower scores. Hence, overall, the drug of choice for this patient is inhaled rapidly acting beta-2 agonists. Table 2: Inhaled rapidly acting beta-2 agonists DRUG EFFICACY SAFETY COST SUITABILITY Salbutamol ++++ ++++ ++++ ++++ Terbutaline ++++ ++++ ++ ++++ Formoterol ++++ +++ +++ +++ 3 Formoterol is a long-acting beta-2 agonist which can be used as a reliever. This drug is usually in combination with inhaled corticosteroids. Furthermore, the use of this drug is not established in children. Salbutamol and terbutaline are comparable in terms of efficacy, safety and suitability. However, salbutamol is cheaper as compared to terbutaline. Therefore, the drug of choice for this patient is salbutamol 100 mcg given as meter dosed inhaler with dedicated spacer and face mask. Step 4. Writing the Prescription Name: Willie Villamin Address: Malate, Manila Date: Nov. 22, 2010 Sex: M Age: 3 y.o. R/ Salbutamol pressurized MDI 100mcg Step 4. Write the Prescription #1 Sig. 2 puffs during acute attacks, use with face mask and spacer Step 5. Patient Advice and Education Step 6. Monitoring and Follow-up EVA FONDA,MD Lic.# 14344 Step 5. Patient Education and Advice 1. 2. 3. 4. 5. 6. 7. Educate the family about the illness a. Natural progression, symptoms b. Genetic predisposition Inform the family on proper use of medication a. Explain the mechanism of action of the drug b. How to use the MDI, spacer, face mask, nebulizer if necessary c. Compliance to medication d. Possible side effects like tachycardia, nervousness, palpitation, dizziness Identify and avoid triggers a. Ex. Pollen, dust, animal dander, certain foods and drugs, obesity, stress, precipitating illnesses b. Advocate proper environmental sanitation c. Warn against exposure to smoke Inform family when hospital admission is required a. No response to 3 administrations of salbutamol within two hours, with tachypnea b. Breathlessness, unable to speak or drink c. Cyanosis d. Subcostal retractions Inform the family on the importance of vaccination a. Complete the vaccinations included in the expanded program on immunization b. Stress importance on yearly influenza vaccines Check other family members for asthma Make sure the family has understood instructions and warnings a. Allow them to ask questions b. Make the family members repeat the pertinent things stated 4 Step 6. Monitoring and Follow-up 1. 2. Monitoring a. Monitor the response of the patient to the medication, as well as compliance b. Record asthma exacerbations (characteristics, duration, timing, symptoms) Follow-up a. Initial follow-up is done 1-3 months after the consultation b. After the initial follow-up, consultation is done every three months thereafter c. Continuous assessment and evaluation of the regimen is warranted, in order to determine whether to step up or step down Reference: Global Initiative for Asthma: Guideline on Asthma Management and Prevention in Children 5 years and Younger (2009) 5