Developing microRNA`s as biomarkers for cutaneous melanoma
advertisement

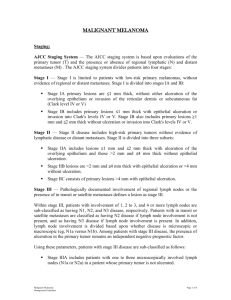
Pathological Society abstract Developing microRNAs as biomarkers for cutaneous melanoma Prashant Shah INTRODUCTION: Cutaneous melanoma is an aggressive disease. Currently, the 2009 American Joint Committee on Cancer (AJCC) staging system is used for malignant melanoma. Clinical and histological features act as indicators of survival. Accurate staging following excision biopsy is vital to ensure appropriate management. Features used for AJCC staging are Breslow’s thickness, ulceration, mitotic rate (stage I/II), lymph node metastases (stage III), site of distant metastases and serum LDH (stage IV). The stage of melanoma at diagnosis strongly relates to prognosis. Several clinico-pathological variables affect prognosis including AJCC features as well as age, gender, anatomical site, subtype and Clark’s level. Breslow’s thickness is established as the single most valuable prognostic guide. Patients with thin lesions less than 1mm thick have a 5-year survival rate greater than 95%. This falls to less than 50% for tumours greater than 4mm. Metastatic spread can occur early in development, with appalling outcome in patients. Metastatic tumours have a 5-year survival rate ranging from 5-22%. This highlights the necessity to detect melanoma at an early stage. The staging protocol used at present is not supported by any molecular tests of analogous value. Despite the general reliability of AJCC staging in predicting outcome, limitations exist. Some individuals with several poor prognostic factors can still survive for a long time without any metastases, yet patients with thin primary cutaneous melanoma can develop metastases and die from their disease. Thus, a proportion of people exist in whom prognosis cannot be accurately determined using clinico-pathological features. The unpredictable behaviour of melanomas that are morphologically similar makes prognostication for histopathologists very difficult. The clinical application of biomarkers known to reliably act as independent prognostic variables would be desirable. Using PCR, miR-10b has been identified as a purported prognostic biomarker in our lab. The primary aims of this study were firstly to validate a method for miR-10b detection. Secondly, miR-10b levels were determined on a melanoma cohort using this method. Finally, miR-10b was evaluated as a biomarker to support our earlier lab findings. METHODS: 8 breast cancer and 5 melanoma cell lines were surveyed for miR10b controls by RNA extraction and real-time quantitative reverse-transcription PCR (q-RT-PCR). Cell line controls with highest, intermediate and lowest miR10b levels were selected for pre-designed miR-10b Colorimetric In-Situ Hybridisation (C-ISH) probe assay validation and C-ISH on melanoma cases. Cell lines were cultured according to standard cell culture methods. C-ISH results in cytoblock section controls were compared against q-RT-PCR data. Similar miR10b levels were expected from both techniques. Melanoma tissue from patients with primary cutaneous malignant melanoma was used in this study. All cases were FFPE tissue that had been used for pathology reports. Histology specimens were obtained from the University Pathological Society abstract Hospital Leicester NHS Trust’s Histopathology diagnostic archive, diagnosed before 2004-5. C-ISH evaluated the clinico-pathological significance of miR-10b against outcome measures in 107 melanoma cases and H scores quantified miR10b. The independent variable was miR-10b expression. The dependent variable was patient outcome, which was defined as time to first metastases. All-cause death time and melanoma-specific death time were measured for survival analyses. Kaplan-Meier plots and Cox proportional hazard regression analysis determined the prognostic value of miR-10b and other variables in melanoma. A relationship between miR-10b expression and these clinico-pathological variables was also determined. RESULTS: MCF7 (RQ=1), MDA-MB-231 (RQ=44) and SK-MEL-28 (RQ=753) were used as miR-10b cell line controls based on their Relative Quantification (RQ) values. There was a general drop in detection of miR-10b between fresh cells and fixed cytoblock tissue. After troubleshooting, C-ISH results corresponded to qRT-PCR data in the majority of controls, thus validating the probe assay. Preliminary C-ISH runs showed systematic bias in methodology, likely due to technical variation. Attempts to alleviate this still left slight systematic bias between repeat C-ISH runs on the same cases over 4 different days with an Intraclass correlation coefficient of 0.51, indicating moderate agreement. After proceeding to melanoma cases, H scores were allocated to 105/107 cases with high and low miR-10b expression groups formed around a median score of 100. 2 sections were not scored due to overdigestion with Proteinase K. The same 15 sections were scored twice on separate days to check reliability in the operator’s scoring. The ICC value was 0.92 suggesting very good agreement in H scoring. Univariate analysis indicated miR-10b was not significantly predictive of patient outcome (p>0.05). Multivariate analysis showed Breslow thickness independently predicted all outcome measures (p<0.05). Ulceration independently predicted time to all-cause death (p=0.02) and melanoma-specific death (p=0.021). MiR-10b was not related to known powerful prognostic variables. Reasons behind the lack of significance of miR-10b on outcome effects were sought. Batch variation was present, F(10,94)=2.047, p=0.037. However, this was not due to inherent batch bias because there was no significant difference in independent outcome predictors, Breslow thickness (p=0.095) and ulceration (p=0.219) between batches. The batch variation was therefore presumably due to technical differences from C-ISH technique or H scoring. During analysis, some cases were difficult to score because of invasive parts of tumour section that were separated from the main tumour, thus producing different staining intensities. CONCLUSIONS: The miR-10b C-ISH probe assay was validated and deemed suitable for melanoma case application. Diminishing C-ISH signal was seen from SKMEL-28, MDA-MB-231 through to MCF7 in the majority of cytoblock sections. However, a slight discrepancy still remained. Our study showed miR-10b was not associated with outcome after analysis of 105/107 cases. This was most likely due to technical issues from personal C-ISH technique or cases that were difficult to score. The fact that Breslow thickness and Pathological Society abstract ulceration significantly predicted outcome showed us that our cohort was representative of melanoma. No relationship between miR-10b and other prognostic variables further supported our findings of miR-10b having no significant effect on outcome. If miR-10b was an important marker, it would have related to these variables. The lack of outcome effects was most probably due to intra-operator variability in CISH technique or case scoring. Genuine biological difference causing these effects were unlikely because the previous study used a robust RT-PCR technique on 2 independent cohorts and screened more than 300 miRNA’s to identify miR-10b as a sole, independent predictor of outcome. Measures were taken to minimise technical error by reducing batch variation in preliminary C-ISH runs, but systematic differences persisted. Due to time constraints, it was deemed suitable to proceed to CISH analysis of cases, keeping in mind technical variation being responsible for any outcome effects. The lack of support in our study in comparison to the previous study indicates further research must be performed to mitigate technical error and confirm our previous lab findings of miR-10b as a prognostic biomarker. Words - 1100