lecture_2014-12-0114174414201965016629547c708c8212b
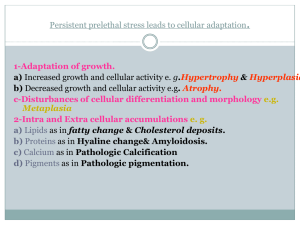
advertisement

Intracellular accumulations 2014-2015 Dr.Ban Jumaa Intracellular accumulations Definition: abnormal accumulation of some products within the cell is a manifestation of metabolic derangement of cells. Three categories of substances: – Normal cellular constituent • – – Water, lipids, proteins, carbohydrates. Abnormal substance • Exogenous: ex. Mineral • Endogenous: product of abnormal metabolism Pigments Lipid Accumulations Accumulations of: • Triglycerides – • Fatty change (seen in alcoholics) Cholesterol – Atherosclerosis – Xanthomas – Cholesterolosis Fatty Change (Steatosis) • It is abnormal accumulation of triglycerides in parenchymal cells. • Organs affected – Liver (most common). – Heart, muscles and kidneys. 1 Intracellular accumulations 2014-2015 • Dr.Ban Jumaa Mechanism of fatty change Free fatty acids from adipose tissue or ingested food are normally transported into hepatocytes. In the liver, they are esterified to triglycerides, converted into cholesterol or phospholipids, or oxidized to ketone bodies. Release of triglycerides from the hepatocytes requires apoproteins to form lipoproteins. Excess accumulation of triglycerides within the liver may result from defects in any one of the events in the sequence from fatty acid entry to lipoprotein exit. Causes of fatty change of the liver 1 .Alcohol is the MCC (most common cause) of fatty change in the liver: alter mitochondrial and SER function and thus inhibit fatty acid oxidation 2. Anoxia inhibits fatty acid oxidation 3. Starvation increases fatty acid mobilization from peripheral stores 4. CCl4 and Kwashiorkor (Decreased Protein intake) decrease the synthesis of apoproteins 5.Diabetes Mellitus 6. obesity 2 Intracellular accumulations 2014-2015 Dr.Ban Jumaa Morphology of fatty change of Liver • Gross: normal size or enlarged liver with a yellowish discoloration. • Microscopically: • Clear spaces (vacuoles) in the cytoplasm pushing the nucleus of the hepatocytes to the periphery. • Special stains: Sudan IV and Oil Red O (orange red color to lipid). Cholesterol and Cholesterol Esters • Cells use cholesterol for synthesis of cell membrane. • Accumulation of cholesterol seen in many pathological conditions: 1. Atherosclerosis (will be taught in CVS) 2. Xanthomas 3. Cholesterolosis Xanthomas • Tumor-like masses composed of Clusters of macrophages (foamy cells) containing cholesterol. • Occur in the Subepithelial connective tissue of skin & in tendons. • Seen in hereditary hyperlipedemic states. Cholesterolosis • Refers to focal accumulation of cholesterol laden macrophages in the lamina propria of the gallbladder. Hyaline change • Non-specific term used to describe any intracellular or extracellular accumulation that has a pink homogenous appearance. • Most commonly occurs due to accumulation of proteinaceous material (protein accumulation). • Accumulation can be: 3 Intracellular accumulations 2014-2015 • • Dr.Ban Jumaa Intracellular hyaline – Protein within proximal tubule of kidney. – Russell bodies. – Mallory Alcoholic hyaline. Extracellular hyaline – Collagen in old scars – Amyloid Resorption protein droplets • Most commonly seen in proximal renal tubular cells. • In patients with protein loss in the urine (proteinuria) Ex Nephrotic syndrome Russell Body • Excess immunoglobulin accumulation in RER of plasma cells. • Fuse to form eosinophilic globules known as Russell bodies. Mallory bodies (=Alcoholic Hyaline) • Are masses of keratin intermediate filaments within hepatocytes. • Seen in patients with alcoholic liver disease. Hyaline arteriolosclerosis Refers to arterioles that have a glassy, amorphous eosinophilic material in the vessel wall that often narrows the lumen seen in small vessels in DM and hypertension. Pigment Accumulations • Pigments are colored substances. 1. Exogenous: from outside the body – Carbon / coal dust – Tattoo ink 4 Intracellular accumulations 2014-2015 Dr.Ban Jumaa 2. Endogenous: synthesized within the body – Lipofuscin – Melanin – Bilirubin – Hemosiderin Carbon or coal dust • Anthracotic pigment – Air pollution Inhalation of carbon dust alveolar macrophages accumulation in lymphatics, regional lymph nodes and lungs blacken the tissues of the lungs (anthracosis) and the involved lymph nodes. • Coal dust: – In Coal miners accumulation of coal dust composed of carbon and silica induces fibroblastic reaction lung disease = coal worker’s pneumoconiosis. – Localized pigmentation of skin. Pigments phagocytosed by dermal macrophages. Tattooing Endogenous pigments • Lipofuscin: (Latin: fuscus = brown) • Also known as Lipochrome, wear and tear or aging pigment. • Is an end-product of membrane lipid peroxidation. • Not injurious to cell. • Sign of free radical injury and lipid peroxidation. • Appearance: yellow brown, finely granular, intracytoplasmic, often perinuclear. • Seen in liver and heart of 5 Intracellular accumulations 2014-2015 Dr.Ban Jumaa – Aging patients. – Patients with malnutrition or cancer cachexia. Melanin • A brown black pigment • Tyrosinase catalyses the oxidation of tyrosine into Dihydroxyphenylalanine (DOPA) in the melanosomes • Synthesized in melanocytes within the epidermis. • Sunlight and ACTH stimulate melanin synthesis in the skin. Melanin excess 1.Conditions associated with an increase in ACTH: – Functioning pituitary adenoma – Ectopic ACTH – Addison’s disease (destruction of adrenal gland) • All associated with increased skin pigmentation. 2. Nevocellular nevi or moles: Benign proliferation of nevus cells which are modified melanocytes. 3.Malignant melanoma: A malignant tumor of melanocytes. Absence of Melanin Albinism – Characterized by absence of tyrosinase. – Melanocytes are present but do not contain melanin within melanosomes. – Autoimmune destruction of melanocytes produces patchy areas of depigmentation. Vitiligo 6 Intracellular accumulations 2014-2015 Dr.Ban Jumaa Accumulation of hemosiderin and bilirubin Bilirubin and hemosiderin: – Derived from breakdown of hemoglobin by macrophages that have phagocytosed RBCs. – Hb = heme (iron+protoporphyrin) + globin (α,β,γ,and δ chains). – Bilirubin: derived from protoporphyrin. – Hemosiderin: composed of packets of ferritin (soluble form of iron). Hemosiderin: – Iron containing pigment, consists of aggregates of ferritin. – Normally found within macrophages in bone marrow, spleen and liver. – Appears as golden yellow to brown in color on H&E stain. – Identification: Prussian blue stain. Hemosiderin Excess Hemosiderosis: is defined by accumulation of hemosiderin, primarily within tissue macrophages, without associated tissue or organ damage. – Local Hemosiderosis: • Results from congestion or hemorrhage into tissues • – Ex: Pulmonary congestion (left heart failure) ,common bruise Systemic hemosiderosis: • Generalized hemosiderin deposition without tissue damage. • Results from multiple blood transfusions, excessive Fe intake, hemolytic anemias. Hemochromatosis: is more extensive accumulation of hemosiderin, often within parenchymal cells, with accompanying tissue damage and organ dysfunction. 7 Intracellular accumulations 2014-2015 • Occurs in two forms: • Hereditary hemochromatosis: • Dr.Ban Jumaa – Most often caused by mutation in HFE gene on chromosome 6. – Chraracterized by hemosiderin deposition and organ damage in the liver, pancreas, myocardium and multiple endocrine glands. – These result in triad of findings: cirrhosis, Diabetes mellitus and skin pigmentation. – This set of findings = BRONZE DIABETES Secondary hemochromatosis: – Is most often caused by multiple blood transfusions as in beta thalassemia major. Bilirubin • Derived from the breakdown of hemoglobin by macrophages in the spleen and bone marrow. • Released from macrophages as lipid soluble, unconjugated bilirubin (UCB). – Bound in plasma to albumin. – Delivered to hepatocytes for conjugation into conjugated bilirubin (CB) – An increase in CB or UCB (or both) produces jaundice = yellow discoloration • – • First noted in sclera when conc > 2mg/dL Hyperbilirubinemia: increased bilirubin in the blood. UCB increase: – Hemolytic anemias (hereditary spherocytosis) 8 Intracellular accumulations 2014-2015 – Problem with uptake and conjugation of bilirubin (physiologic jaundice of newborn). – Newborns with Rh disease of newborns may develop kernicterus • • Dr.Ban Jumaa Due to entry and dissolution of UCB in brain tissue. CB increase: – Hepatitis and – Obstructive jaundice (gallstone in CBD) Pathologic Calcification • It is the abnormal tissue deposition of calcium salts. • Two forms: – Dystrophic calcification: – The deposition of calcium salts occurs locally in dead or dying tissues; with normal serum levels of calcium and in the absence of derangements in calcium metabolism. – Seen in areas of necrosis and/or damage eg. in the atheromas of advanced atherosclerosis or in aging or damaged heart valves. – Calcium salts appear macroscopically as fine, white granules or clumps, often felt as gritty deposits. – Sometimes a tuberculous lymph node is virtually converted to stone – Microscopically, calcification appears as intracellular and/or extracellular basophilic deposits. – In time, heterotopic bone may be formed in the focus of calcification. – Progressive deposition on outer layers may create lamellated configurations, called psammoma bodies (papillary cancers). 9 Intracellular accumulations 2014-2015 Dr.Ban Jumaa Metastatic calcification: The deposition of calcium salts in normal tissues, and it almost always results from hypercalcemia secondary to disturbance in calcium metabolism. Metastatic calcification can occur widely throughout the body but principally affects the interstitial tissues of the vasculature, kidneys, lungs, and gastric mucosa. The calcium deposits morphologically resemble those described in dystrophic calcification. Extensive calcifications in the lungs may produce remarkable respiratory deficits .Massive deposits in the kidney (nephrocalcinosis) can cause renal damage. Causes 1) Increased secretion of parathyroid hormone (PTH) with subsequent bone resorption, as in hyperparathyroidism 2) Destruction of bone tissue: Bone tumors (e.g., multiple myeloma, leukemia) or metastatic bone cancers 3) Vitamin D-related disorders, including vitamin D intoxication 4) Renal failure: causes retention of phosphate, leading to secondary hyperparathyroidism. 10