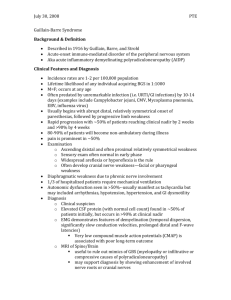
Guillain-Barré Syndrome
advertisement
Guillain-Barré Syndrome Heather Hetler CD 502 Motor Speech Disorders Spring, 2011 What is Guillain-Barré Syndrome? • Guillain-Barré Syndrome is an idiopathic, acute, progressive, inflammatory, peripheral neuropathy, characterized by progressive muscle weakness over hours to several days. • May involve degeneration of axons, demyelination, or a combination of both, though demyelination is most common. • Considered a group of disorders rather than a single disease. • An autoimmune disease, involving the immune system attacking the myelin (in demyelination types of GBS) • Most important cause of acute flaccid paralysis in the United States, but still rare, with a prevalence between 1.5 and 3 cases per 100,000 per year in North America. Causes • The exact triggers or causes of Guillain-Barré Syndrome (GBS) are unknown. • It often follows a minor respiratory or abdominal infection. • May occasionally follow a vaccination: • The swine flu vaccine in 1976 is suspected to have caused several cases. • According to the CDC, “As of February 25, 2008 … Vaccine Adverse Event Reporting System (VAERS) has received 26 confirmed case reports of GBS within 6 weeks of receipt of MCV4 Menactra meningococcal vaccination. ” This indicates there may be a small increased risk, though the data is not conclusive. • The risk, if in fact present, is very slight, compared to the risk presented from the diseases for which vaccines are administered. Symptoms • Most common type of GBS seems to start with weakness in legs, gradually ascending to arms and head. • Weakness is most often bilateral, unlike a stroke. • Weakness in legs can cause difficulty with walking, general clumsiness, and difficulty going up and down stairs. • As the weakness ascends and affects arms and hands, difficulty is seen in holding up arms for self-care tasks (brushing teeth, combing hair) and difficulty with fine motor tasks (writing, buttoning clothing). Symptoms • Approximately 40% of those with GBS will have respiratory system muscles impacted, and one fourth will require respiratory support. • Difficulty taking breath or deep breath, difficulty with coughing, feeling of suffocation. • Cranial Nerve involvement in one half of those affected. • Seventh cranial nerve (facial nerve) damage leads to inability to smile or fully close eyes. • Ninth (Glossopharyngeal) and Tenth (Vagus) cranial nerve damage may cause weakness in throat musculature which compromises airway, causing choking even on saliva. • Occasionally damage to Twelfth (Hypoglossal) cranial nerve, resulting in weakness of tongue and affecting speech. • Rarely, loss of all voluntary muscle movement, resulting in a “Locked-in” phenomenon. Sensory Symptoms • Abnormal sensations (paresthesias) present in 50-70% of those with GBS. • Include “pins and needles” sensation, tingling, numbness • First occur hours to days before muscle weakness. • Painful muscle cramping in 30% of patients. • Between shoulder blades, lower back, thighs • Other sensory symptoms include: feeling of insects crawling on body, sense of vibration, sense of pressure. • Loss of sensation, such as ataxia • May cause abnormal gait due to lack of proprioception • May be undetectable until neurological exam. Symptoms • Loss of reflexes is undetectable to patient, but is notable and may help to make a diagnosis. • Deep tendon reflexes (muscle stretch reflexes), commonly elicited by tapping the tendon just below knee, leading quadriceps muscle to contract and jerk leg forward. • More than 80% of patients may present with pain. • Often unrecognized and undertreated by doctors, who may believe pain is not part of GBS. • May predate weakness, and also occurs during recovery and rehabilitation. • Pain level in proportion to level of weakness. Symptoms • Damage to autonomic nerves, part of peripheral nervous system that automatically regulates internal organs. • Increased heart rate most common. • Difficulty urinating, heart palpitations, constipation, low or high blood pressure are some possible symptoms. Diagnosis • Can be difficult to diagnose early, compromising effective treatment. • Antecedent event, such as virus, may be assumed cause of weakness, particularly in children. • New weakness after surgery is difficult to note. • Several other diseases resemble GBS, making diagnosis more difficult, such as: • Polio, though nearly eradicated in Western world, can still occur in those from other countries who have not been vaccinated, or in older non-vaccinated adults recently exposed to young vaccinated babies or children. • West Nile Virus • When facial paralysis is unilateral, often mistaken for Bell’s Palsy. Diagnosis, continued • Several more rare forms of GBS complicate diagnosis as they follow a different pattern. • Miller Fisher Syndrome (MFS) • Sensory GBS: never develop weakness, only sensory symptoms • Bulbar GBS: begin in muscles around face and throat, causing difficulty swallowing and slurred speech, usually descends to involve limbs. • Axonal GBS: damage to axons in addition to demyelination. Approximately 10% of all cases. Rapid progression of paralysis, more severe, and prognosis is poor. Diagnosis • Symptom diagnosis: The medical personnel take a case history, and identify symptoms, and make a diagnosis based on information. • Nerve conduction studies: electrical testing of nerve function, which can confirm diagnosis of GBS and exclude other disorders of acute, progressive weakness. • Electrical shocks are administered through the skin to determine nerve function, by examining time it takes current to go from stimulation to recording site. • Cerebral Spinal Fluid Testing (lumbar puncture): increased protein concentration with normal number of cells. • If the protein level is above the established threshold, then investigate other disease or disorder, such as West Nile. Treatment • Because the severity of GBS can vary widely, it is often recommended to hospitalize any patient with suspected or confirmed GBS to monitor during the acute phase. • Vital signs (including breathing, heart rhythm, blood pressure, and swallowing) should be monitored closely. • Watch for complications, such as additional infections like pneumonia. • Individual complications will be treated (such as breathing difficulties, high blood pressure), but there is no immediate cure for GBS. Treatment • The SLP will be involved when cranial nerves affecting swallowing and speech are impacted. • Symptoms of drooling, gagging, and choking should result in stopping of eating until an assessment can be done. • A bedside swallow exam may indicate the need for a video swallow study. • The monitoring of thirst and hydration is also very important in a paralyzed patient who cannot self-monitor hydration. • Rehabilitation should begin as soon as patient is medically stable, and continue after need for acute care has passed. • Occupational and Physical Therapy, including range of motion exercises, splints, positioning Treatment • Speech Therapy in Rehabilitation: For patients who have had swallowing and speech affected, therapy within rehabilitation will be necessary. • Those who required a tracheostomy may also need speech therapy in rehabilitation to regain ability to speak clearly. • Rehabilitation may need to continue into the home, with accommodations made to home environment. References • Brandt, A.K. (2002). Learning to Walk Again: How Guillain Barre Taught Me to Walk a Different Path. Lincoln, NE: iUniverse, Inc. • Davids, H.R., MD (2010, March 29). Guillain-Barre Syndrome. Retrieved from http://emedicine.medscape.com/article/315632overview • GBS/CIDP Foundation International (n.d.). Guillain-Barré Syndrome. Retrieved from http://www.gbs-cidp.org/index.html • Mayo Clinic Staff (2009, May 30). Guillain-Barre syndrome. Retrieved from http://www.mayoclinic.com/health/guillain-barresyndrome/DS00413 • National Institute of Neurological Disorders and Stroke (2011, March 23). Guillain-Barré Syndrome Fact Sheet. Retrieved from http://www.ninds.nih.gov/disorders/gbs/detail_gbs.htm • Parry, G.J. (2007). Guillain-Barré Syndrome: From Diagnosis to Recovery. New York, N.Y.: Demos Medical Publishing.