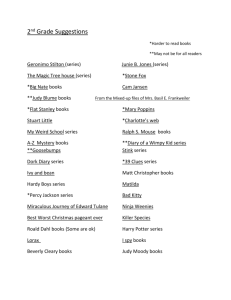
Can you feel her Pain?
advertisement

Can you feel her Pain? Stories of human interest "I can't go to work now because sitting down is worse than standing up" A personal perspective from Ireland She was a practising barrister in Dublin when she was hit from behind by a truck. What started off as numbness around the roof of her mouth would end up with Gina suffering from severe chronic pain: “I felt as though my fingers were stuck in an electric socket and the electricity was pulsing up and down my arm. The pain in my shoulder felt so severe I could have taken a knife to hack it off. At other times I felt as though my arm had been crushed against a concrete wall”. Because of the pain that was so severe she could not stand or sit or read for more than a few minutes she had to give up work. To make matters worse she experienced a nightmarish journey through the Irish healthcare system, being referred to one doctor after the other for the next seven years. Finally in 2002 after “a living hell”, not knowing whom to turn to for help, she was referred to a consultant specialising in the treatment and management of chronic pain. He duly carried out a procedure which reduced the level of pain and enabled Gina to resume living as normal a life as one could expect with constant pain. Her message: “Pain has to be recognised as a disease. A Person living with chronic pain needs to get an early diagnosis and then an early intervention”. Gina Plunkett Chairperson Chronic Pain Ireland and Interim Chair Pain Alliance Europe 1 A personal perspective from Finland Liisa reports: “The first time I felt back pain it was at the age of 15. “Inborn”, “construction failure” said the doctors who discovered two vertebra growing together. But I wanted to become truck driver and I became it. After a few years I was forced stop driving and I continued my studies. I then graduated from Jyväskylä Technical Institute in Finland and continued studies for a M.Sc. degree at Plymouth University in England. At the end of my studies I got a slipped disk and my life turned upside down. I finished my theses and got back to Finland to receive treatment. It took a whole year before I managed to have an operation and treatment. The operation did help, but the pain is still present. Some days are worse and some are better. Pain is part of everyday life which renders normal life impossible. Pain also caused me to lose the work community I had grown into. Getting to know my situation and learning to live with it became a new way of everyday living. I now have a wheelchair and a special pillow with me when I travel. Community action with Finnish Pain Association has helped me to cope with my condition and help others with the same fate. Pain should be understood, but not accepted.” Liisa Mikkonen, President Finnish Pain Association A personal perspective from UK Since her Teens Maggie Hayward had suffered crippling pains from her back which had wreaked havoc with her work and family, eventually leading to the break-up of her first marriage. “I had constant stabbing burning pain in my lower back and legs, so intense it felt like electric shocks”. After she had tried all kinds of treatments – from physio to acupuncture – without success, she agreed to have two vertebrae at the base of the spine fused. However, the operation which had cost GBP 35.000 made no difference to the pain. Maggie, meanwhile retired as an exhibition manager, was not able to work again. Eventually she was unable to dress herself or cook a meal for her family. It was a physiotherapist who was the first to mention that it could be neuropathic pain – resulting from tangled nerves and not from a mechanical disorder. With the proper exercise, a course in pain management and the right medication, making the nerves less excitable, she slowly improved. Maggie is still angry that her many doctors never investigated the possibility of nerve pain which at an early stage could have been cured. Maggie Hayward, Member of Backcare UK A personal perspective from The Netherlands A 35 year old woman suffered from severe chronic pain caused by a blockage of the sacroiliac joint. Her quality of life had decreased significantly and it was impossible for her to sit or stand for longer than 15 minutes. She followed the convoluted referral pattern from her GP, to a neurologist to exclude a herniated disc, then back to the GP. She was then referred to a rheumatologist and finally back to her GP. No clear cause for her pain could be found, so she was told it was probably psychosomatic and advised to see a psychologist. In the meantime she had lost not only her job but also her confidence in doctors. As the cause remained unexplained, no doctor was willing to refer her to a pain clinic. Aneka´s story (name changed) A personal perspective from the UK For nearly 40 years Judy Birch had suffered severe chronic pain and had to live with endometriosis since her twenties. The pain returned after the birth of her daughter but Judy continued to work for many years with worsening pain. Her gynaecologist said that pain was not his job without suggesting anyone who could help. Standing and sitting was increasingly difficult. Surgery in the UK, Belgium and France followed, Judy was unable to continue working. She asked to be referred to a pain specialist but her GP said she had other priorities. In France it was recognized that Judy had neuropathic pain due to pelvic nerve damage and she was referred to a multi-disciplinary team including a neurologist, pain specialist, gynaecologist, and physiotherapist where she received a range of intensive treatments which is ongoing. Judy Birch, Founder and Chief Executive, Pelvic Pain Support Network 2