EPIC-BEST Speaker`s Notes - Louisiana Breastfeeding Coalition
advertisement

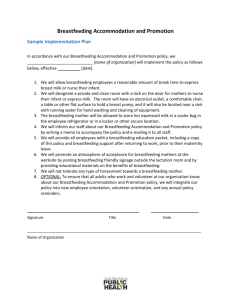
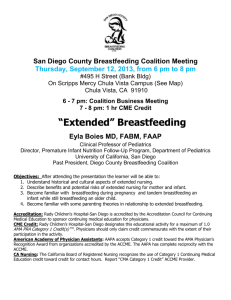
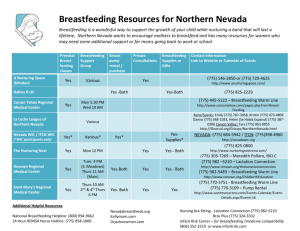
EPIC-BEST Speaker’s Notes Physician speaker’s notes: Lactation consultant speaker’s notes: WIC representative speaker’s notes: WHITE background GRAY background BLUE background Speaker: PHYSICIAN • • • Introduce the training team Hello and welcome to the EPIC-BEST program. Educating Physicians In their Communities – Breastfeeding Education, Support, & Training is designed to inform and educate physicians and their staff about steps that can be taken in the office setting to complement practices being implemented in the hospital setting to improve breastfeeding outcomes. The Louisiana Department of Health & Hospitals Office of Public Health Bureau of Family Health The WIC Program & The LBC Have partnered to provide education to HCPs about breastfeeding support. The faculty, planners and speakers of this program have no relevant financial relationships. IMPORTANT: To help us determine the effectiveness of this training, please take a few minutes to complete the pre-test. There is no need to spend a lot of time on it, just put down the first answer that comes to mind. Note: Be sure that name and e-mail are LEGIBLE on sign-in sheet HOUSEKEEPING: length of program (~90min), location of restrooms 1 The objectives of this program are to: • Discuss the importance of breastfeeding and national recommendations and policies promoting breastfeeding • Identify strategies & resources for physician offices that support breastfeeding • Identify community breastfeeding resources for patient referrals Breastfeeding…is it really important? Does it really make a difference? These are some of the questions that many people have and that we hope to address today. Speaker’s Note: To engage the audience, you could ask them what they think or know about breastfeeding. This may help you get an idea of the knowledge and attitudes that your audience has related to breastfeeding. Remember that breastfeeding is NORMAL in the human world, in the animal kingdom, and it has been throughout all of history. All mammalian mothers and babies are hard wired to breastfeed. As mammals, we make perfect nutrition for our newborns. The protein, carbohydrate & fat content changes dynamically as the baby grows for the perfect meal every time. Why would we stifle such a primitive survival instinct of our body to protect our young? It’s innate. This image demonstrates the differences between human breastmilk & formula ingredients. • Mother’s milk contains many more ingredients than formula and is custom-made for her baby’s needs. • Everything in formula comes from cows or soy plants or some other non-human source. LA Department of Health and Hospitals • Office of Public Health • Bureau of Family Health Human milk contains: living cells…(see slide) It also contains: • Compounds with unique structures that cannot be replicated in infant formula. Breastfeeding Reduces: • Economic burden to society, which pays $600 million for “Free” infant formula through WIC. • Environmental burden for the disposal of formula cans and bottles, and • Energy expenditure in the production and transport of formula The latest breastfeeding statement of the American Academy of Pediatrics clearly states the risks of not breastfeeding. The 1st table: When breastfeeding doesn’t occur, infants and mothers are more at risk for illness and disease. This is a table from an AHRQ publication in which the authors reviewed the evidence on the effects of breastfeeding on short- and long-term infant and maternal health outcomes in developed countries. Among infants who are NOT breastfed, there is an excess/increased risk for the listed diseases and conditions The 2nd table: Addresses excess risk for disease and illness among preterm infants and mothers who do not breastfeed. This slide depicts how obesity in the U.S. has evolved in an alarmingly short period of time. In 1990, some states had obesity rates over 10 percent (the darker blue), but none exceeded 15%. In 2000, data show Louisiana has been joined by many other states who share obesity rates in more than 20% of their adults In 2010, about 60 million adults, or 30 percent of the adult population, are now obese • This represents a doubling of the rate since 1980. LA Department of Health and Hospitals • Office of Public Health • Bureau of Family Health In 2011, a CDC Vital Signs report stated that breastfeeding for 9 months reduces a baby’s odds of becoming overweight by more than 30%. • • • Breastfeeding’s mechanism for lowering the risk of obesity is still unclear but is thought to be due to hormones in the breast milk itself which direct the formation of the child’s metabolism AND the selfregulation that a baby learns when he nurses naturally at the breast. Babies who breastfeed eat when they are hungry and stop when they are full. In contrast, bottle-fed babies are often scheduled and encouraged to finish the bottle even after they have shown signs of being full. CDC Vital Signs. (2011, August). Hospital support for breastfeeding. p.1. Retrieved from http://www.cdc.gov/vitalsigns/Breastfeeding/ See slide • • • • 911 children’s lives could be saved yearly More than $13 billion health care dollars would be saved annually in pediatric health care. The economic cost to society for women who breastfeed less than recommended is predicted at over $17.6 billion per year related to • Heart attacks • Hypertension • Breast cancer • Premenopausal ovarian cancer • Type 2 Diabetes Low US breastfeeding rates are associated annually with • 5,000 cases of breast cancer • 54,000 cases of hypertension • 14,000 heart attacks in women For a summary of this article, go to: http://massbreastfeeding.org/2013/07/10/landmark-study-highlightseffect-of-breastfeeding-on-womens-health/ LA Department of Health and Hospitals • Office of Public Health • Bureau of Family Health As health care professionals (HCPs), according to the American Academy of Pediatrics, the American Congress of Obstetricians and Gynecologists and the American Academy of Family Physicians, HCPs should: • Support exclusively breastfed for 6 months, with no supplementation (unless medically necessary) or introduction of solid food until 6 months. • Support and encourage mothers who wish to go beyond that, hopefully at least until 1-2 years or longer, as long as the mom and baby want to breastfeed. (The World Health Organization recommends continued breastfeeding for at least 2 years). The Joint Commission (TJC) accredits hospitals and allows them to stay open and collect reimbursements. One reason hospitals are interested in increasing BF rates: • Starting Jan 1, 2016 all JC-accredited hospitals with >300 births/yr will be required to collect data on the number of Healthy Term Infants who leave the hospital having been exclusively fed human milk. The following qualifies as “Exclusive”…(see slide) Some of the key actions outlined in the Surgeon General Report relate specifically to health care providers and systems. For example: Action 6 – Ensure that the marketing of infant formulas is conducted in a way that minimizes its negative impacts on exclusive breastfeeding (The WHO Code) Action 7- Ensure that maternity care practices throughout the United States are fully supportive of breastfeeding. Action 8 – Develop systems to guarantee continuity of skilled support for lactation between hospitals and health care setting in the community Action 9 – Provide education and training in breastfeeding for all health professionals who care for women and children The new health care law has a requirement for employers to provide lactation support through reasonable break times and accommodations for expressing milk. • Applies to employees covered under the Fair Labor Standards Act or Non-Salaried employees • The pumping space has to be private and NOT a bathroom. Pumping supplies including pumps are now covered under some insurance plans and are available through WIC. LA Department of Health and Hospitals • Office of Public Health • Bureau of Family Health Ask yourself: • What do you do for your employees if they need to breastfeed? • Has your office had an employee who requested pumping breaks? This slide outlines the national Healthy People 2020 goals for breastfeeding. Not only are goals set for increasing the proportion of infants who are breastfed, but also for: • Increasing workplace support for breastfeeding • Decreasing formula supplementation for breastfed babies and • Increasing the proportion of births that occur in facilities that provide optimal care (Baby-Friendly Designated facilities). Although this isn’t a current map, the trends in breastfeeding initiation rates remain the same, with the lowest breastfeeding rates in the Southern region of the US. It’s interesting to note the similarity in this map and the obesity maps we showed in the beginning of this presentation. • Many of the strategies and best practices that we will talk about today can help lessen the racial and ethnic disparities. • There are many things that we can do as providers to remove barriers to breastfeeding. This graph represents racial/ethnic differences in breastfeeding rates among LA babies who were born in 2006. • There is a clear disparity between Blacks and their White and Hispanic counterparts. • Initiation rates for Blacks are approximately 30%(approximately half the rate of Hispanics and Whites) • While Hispanics and Whites are approx. 58% • At 6 and 12 months, Blacks continue to lag behind by almost 50%. Speaker: LACTATION CONSULTANT LA Department of Health and Hospitals • Office of Public Health • Bureau of Family Health • • Almost ALL women can and should breastfeed. With information, assistance and support, more women would breastfeed. • Many women in low risk pregnancies are able to breastfeed during their next pregnancy, with their obstetrician’s OK. • Some contraception methods do not interfere with BF if started after BF is well established. However, some do decrease or eliminate a mother’s milk supply, so mothers need correct information. There are only a few RARE CONTRAINDICATIONS TO BREASTFEEDING INCLUDING: • HIV, Human T-cell lymphotropic virus I or II • Active, untreated tuberculosis only • Herpes lesions on nipple • You can express and feed mother’s milk; babies can be put to breast after 14 days of maternal treatment and negative cultures • Active varicella (Chicken Pox) • isolate mother, give infant VZIG, express and feed mother’s milk when no breast lesions; resume breastfeeding when no longer contagious • Drugs of abuse and alcohol abuse, however, a mother who is on methadone maintenance can breastfeed • Maternal medications (very few, fewer than you may think) • Later in the presentation I will provide you with references to address concerns about medications and breastfeeding. • Infants with Classic form of Galactosemia • • What can HCPs do to promote/encourage moms to breastfeed? Start with evidence-based care. • The Ten Steps to Successful Breastfeeding are: • The foundation of the Baby-Friendly Hospital Initiative • Developed by a team of global experts • Consist of evidence-based practices that have been shown to increase breastfeeding initiation and duration. • Baby-Friendly hospitals and birthing facilities must adhere to the Ten Steps to receive and retain, a Baby-Friendly designation. The Ten Steps are: 1. Have a written breastfeeding/infant feeding policy that is routinely communicated to all staff. 2. Train all health care staff in the skills necessary to implement this policy. 3. Inform all pregnant women about the benefits and management of breastfeeding. 4. Help mothers initiate breastfeeding within one hour of birth (skin to skin care for all mothers-babies). Continued LA Department of Health and Hospitals • Office of Public Health • Bureau of Family Health • • 5. Show mothers how to breastfeed and how to maintain lactation, even if they are separated from their infants. 6. Exclusive breastfeeding. Give infants no food or drink other than breast-milk, unless medically indicated. 7. Practice rooming in - allow mothers and infants to remain together 24 hours a day (all babies). 8. Encourage breastfeeding on demand. 9. Give no pacifiers or artificial nipples to breastfeeding infants. 10. Foster the establishment of breastfeeding support groups and refer mothers to them on discharge from the hospital or birth center. In LA, The LA DHH-OPH-Bureau of Family Health’s GIFT Program provides resources and a framework to help birthing facilities improve breastfeeding outcomes through incremental adoption of the internationally recognized Ten Steps to Successful Breastfeeding. Gift hospital designation recognizes hospitals that are implementing evidence-based maternity care practices that are aligned with progress toward pursuit of the Baby-Friendly™ designation. • In June 2015: 27 of 52 LA birthing facilities were Gift designated. The gold standard for evidence-based maternity care is the BFHI. This is a global initiative of the World Health Organization (WHO) and the United Nations Children's Fund (UNICEF). A National hospital designation for excellence in practice that encompasses breastfeeding education/support. Implemented in the United States by Baby Friendly, USA. Currently, >250 Baby-Friendly designated hospitals in the U.S. >20,000 BF Hospitals globally and that number is growing quickly. • • As of June 2015, 5 hospitals in LA have achieved this designation Many other Louisiana hospitals have entered into Baby-Friendly’s 4-D Pathway towards designation. LA Department of Health and Hospitals • Office of Public Health • Bureau of Family Health In Louisiana, there is a new consumer messaging resource available as part of Louisiana’s Gift Breastfeeding program to help with preparing families for these practices: Skin to skin care…. It all starts with skin to skin care – An evidence based practice facilitating bonding & breastfeeding. Delaying routine procedures during this time until after the first breastfeeding Skin to skin care is an important practice even if the mom has made an informed decision not to breastfeed Safe S2S care requires: • Position the infant with head turned to the side with infant’s eyes, nose, and mouth visible. • The chin should not be flexed to the infant’s chest • The infant should be in the sight of an alert mother or of a support person. Nursing and medical support of rooming-in with bedside assessments increases maternal confidence in her ability to care for her infant and the confidence a mother has in her infant’s health care providers. • • • • Early subtle feeding cues can indicate, “I’m getting ready for my feeding” or “I’m hungry” When put S2S at this time, early communication is reinforced, with the infant learning that when “I need something” or “someone”, I know who will respond. Babies whose early cues are recognized get better at them and parents gain a better understanding of their infants needs, whether it is hunger or comfort that is needed. Parents who are responsive to early infant needs, are building an early trusting relationship with their newborn. If the early cues are not recognized with a response, an infant’s cues will intensify with mid-cues of stretching, increasing movement, and rooting by bringing hands to mouth, etc. These cues mean “I’m really hungry” and “I’m ready to eat”. These are the most commonly known feeding cues. LA Department of Health and Hospitals • Office of Public Health • Bureau of Family Health Crying, lots of movement and turning red in color are late cues and may indicate “Calm me, then feed me.” These cues may follow early cues that are not recognized with a response. If these are the only cues that get a response, an infant may resort to these instead of early cues. This next section covers resources that are available to help prepares families for these Evidence-Based Hospital Practices Moms & supporters can download a free mobile app to help prepare her for these evidence-based practices and a smooth hospital visit. It will help them understand what maternity care services (such as rooming in, skin to skin etc) are available and why they are ‘best practices.’ Prenatal Preparation Checklists are being tailored to local hospitals to enable mothers to learn of maternity care practices that are offered at their hospital of choice. It is essentially, a structured to-do list for prenatal education. • Assists the mom with identifying her breastfeeding support team • Informs the mom of the evidence-based practices to discuss with her health care provider. • Facilitates her contacts with physicians and community resources. The checklist is designed to be provided to mothers prenatally by their physicians, hospitals and community resources. Ideally it is provided prenatally, but is also valuable during the postpartum period to inform her of breastfeeding resources. The final tool includes counseling sheets that are designed for prenatal teaching and can also be used at hospital bedside. They are written at an appropriate literacy level with material that includes best practices to help moms get off to a good start. Through The Gift program, Louisiana hospitals will be provided with sets of these counseling sheets to facilitate breastfeeding education/counseling. LA Department of Health and Hospitals • Office of Public Health • Bureau of Family Health Speaker: PHYSICIAN Initiating breastfeeding conversations is key. • OB and Pediatric settings offer perfect opportunities for starting the conversation about breastfeeding. • When an expectant mother comes into the OB appointment or brings an older child in for a pediatric visit, take that moment to ask her about breastfeeding. • If she had a negative experience with breastfeeding another child, explore the issues and offer guidance or referral to a lactation resource. This may cause her to be more open-minded and confident about nursing the new baby. How often are we really taking advantage of chances to talk with women while they are still pregnant? “In one recent study researchers found that less than a third of visits included any discussion of breastfeeding, and only 2% included an explicit recommendation that breastfeeding is superior to artificial feeding.” Those numbers clearly reflect some missed opportunities. And they also point out that, doctors-in-training need direction from their faculty about why and how to discuss breastfeeding. At prenatal care visits, early in the pregnancy, assess the mother’s knowledge about breastfeeding. Ask open-ended questions…..(see slide) After proper education on the benefits of BF, respect the mother’s informed decision and allow for her to change her mind at any time. A woman’s knowledge-level about BF is significantly linked with her decision on how to feed her baby The prenatal visit is a perfect opportunity to dispel myths the parents may have heard Myth: BF takes too much time • BF takes more time during the first 5-6 wks, but is known to take ¼ of the time it takes to formula feed during 6-52 weeks and even less after that. (Mohrbacher, Nancy et al., “Breastfeeding Made Simple”, www.NewHarbinger.com) • • Myth: Breastfeeding mothers get less sleep In a recent study, women who breastfed slept as well, if not better than formula feeding mothers. There were no significant differences in total sleep time. In fact, over time, quality of sleep improved for BF vs Formula feeding moms. (Montgomery-Downs, H. E. et al. Pediatrics, 2010; 126:e1562-1568) Sleep deprivation is part of being a parent no matter how the baby is fed Additional Q’s: LA Department of Health and Hospitals • Office of Public Health • Bureau of Family Health • • • • • • What are your plans for feeding your baby? Continued What have you heard about breastfeeding? How can I help you breastfeed? How does your family/partner feel about your breastfeeding? What are your concerns about breastfeeding? What are your expectations for breastfeeding including work, social and family? -Resource CD contains a Breastfeeding FAQ-A Guide for Physicians. The leave behind books are also both good references. Provide accurate information (informed mothers do not feel guilty) • “Did you know that breastfeeding is healthier for baby and for you?” Discuss the reduction in risks for mother and baby • If mother has a personal or family history of diseases linked with lower rates of breastfeeding (inflammatory bowel disease, diabetes, etc.) – “Did you know breastfeeding can lower your baby’s/your later risks of…?” • You may be the only person to inform her and tell her this information. Almost any woman can breastfeeding successfully to reach her goals. • Most conditions with potential for lower supply can be managed to prevent breastfeeding problems (esp. with collaboration of lactation consultant and MD) A mother that has factors that can affect breastfeeding should be referred to a lactation consultant for evaluation and collaboration. These factors include: Flat or inverted nipples Previous breast surgeries Breast surgeries PCOS poly-cystic ovarian syndrome Tubular and asymmetry breasts Hypothyroidism Encourage S2S contact without interruption until completion of 1st Bfding Delay weighting & measuring infant until after 1st feed LA Department of Health and Hospitals • Office of Public Health • Bureau of Family Health • • All babies should be seen by a pediatrician by age 3-5 days. If risk factors exist then baby should be seen by pediatrician within 2448 hours after discharge. • After a mom is discharged from the hospital, the first few days are critical to her success. • Latch-on discomfort can be normal – it should resolve in 30-60 seconds. Pain at other times is NOT normal. Ask Open-ended Q’s… (see slide) Continued Discuss: • Frequent feedings are not an indicator of insufficient milk supply, in early weeks • Expect Growth Spurts • Signs of adequate feedings • Support cue-based feeding -- Watch the baby, not the clock! Encourage breastfeeding 8-12 times in 24 hours. Do not put time limits on breastfeeding! Other open – ended Q’s • What are your expectations? Speaker Note: Reference the Resource CD which contains a Breastfeeding Assessment Tool that was developed for use on or around Day 5. The OB’s first postnatal visit: • Assess the breast: Ask the mother about any breast or nipple pain. Possible problems that could arise include mastitis (especially common when mothers return to work or start to become more active at home), plugged ducts, nipple infections, issues with milk production • Examine the breast for masses. Never postpone a work-up of a mass because of lactation. Pregnancy-associated breast cancer is deadlier not due to a more aggressive course but due to delayed diagnosis. Most diagnostic procedures including mammography and biopsies can be done during lactation. • Instruct mother about the Lactational Amenorrhea Method: If she is breastfeeding exclusively, her menses have not returned, and the infant is less than 6 months old, she has a 1-2% chance of pregnancy. • Discuss the need for other contraceptive measures as needed. If hormonal contraception is to be used in a breastfeeding mother, avoid starting it before lactation is well established, e.g. 6 weeks postpartum. Ideally, a progestin-only method should be used. Note: The Academy of Breastfeeding Medicine has an evidence-based protocol about Contraception and Breastfeeding, however, this protocol is currently under revision and is not available on their site. Resource for moms: http://kellymom.com/bf/can-i-breastfeed/meds/birthcontrol/ • • • • • • Inquire about sleep now that, hopefully, a routine is emerging. Always advocate for baby being in the same room as the mother in a safe position consistent with SIDS prevention recommendations. Separate, but adjacent surface (or at least in the same room). This is the time to help moms who must return to work at 6-8 weeks postpartum with their transition Ask Q’s about child care and milk storage/transport. Warn against abrupt weaning, prolonged times without pumping, and signs of mastitis Discuss changes in stooling patterns Continued LA Department of Health and Hospitals • Office of Public Health • Bureau of Family Health • • • • • • • • • • • Less frequent stools Decreases to every 3 to 7 days at 1 to 3 months for some but not all breastfed babies Praise mom for continued success! The first month is the hardest. She should have some confidence now, a rhythm with baby’s demand and her supply, and can bottle feed some if necessary for outings or work. Continue to remind her that continued natural nursing carries the most benefits and ensures the best milk supply. The World Health Organization and the AAP recommend that infants start receiving complementary foods at about 6 months of age. Early introduction of solids has been implicated in childhood obesity. Encourage mom to enjoy 6 months of exclusive breastfeeding. There will be plenty of time for real food (and stinky bowel movements) later. Dispel myths about solid foods helping babies to sleep through the night… that is unproven… in fact, solid foods only bring digestion problems and potential allergy risk when introduced too soon. Formula reps may talk about wanting what is best for infants, but remember that their ultimate goal is to make money. When a HCP hands out marketing materials, he/she is acting as their agent. You are putting the office’s stamp of approval on the product. Think about what other products you specifically market on behalf of a company (probably none). • Formula ads, free samples, coupons, vouchers etc in doctors’ offices send the wrong message to families • Free formula samples in hospital discharge packs give an impression that formula is endorsed by hospitals • Promotional items (e.g., pens, baby name cards, mugs, calendars) are marketing tools … which is fine at the mall, but they have no place in a doctor’s office or a maternity hospital! • Free lunches are to buy your favor. Reference the Resource CD which includes a Fact Sheet about formula marketing in Doctor’s offices and health clinics. http://www.citizen.org/infant-formula-marketing-clinics. See slide LA Department of Health and Hospitals • Office of Public Health • Bureau of Family Health Speaker: LACTATION CONSULTANT See slide In February 2012, the American Academy of Pediatrics, in their policy statement “Breastfeeding and the Use of Human Milk”, stated that • “Infant growth should be monitored with the World Health Organization (WHO) Growth Curve Standards to avoid mislabeling infants as underweight or failing to thrive.” • The CDC also recommends that the WHO growth charts be used for children age 0-2. Healthy breastfed infants tend to grow more rapidly than their formula-fed peers in the first 2-3 months of life and less rapidly from 3 to 12 months. Because many doctors are not aware of this difference in growth, they see the baby dropping in percentiles on the growth chart and often come to the faulty conclusion that the baby is not growing adequately. At this point they often recommend that the mother (unnecessarily) supplement with formula or solids, and sometimes recommend that they stop breastfeeding altogether. Breastfeeding is all about supply and demand. The more a mother breastfeeds, the more milk she makes. Fussy baby symptoms are often a reflection of a normal baby who is cluster feeding or in a growth spurt or normally helping mom build a better milk supply. • • • • • Include in your dialogue “8 or more in 24 at early cues” Avoid dialogue such as, “You should be feeding every _ to _ hours”. No scheduled feedings. Babies may need to feed more frequently (cluster feeding) when going through a growth spurt. Encourage frequent feedings at early cues (rooting, sucking hand) Breastfeeding & pumping cause hormone levels to spike LA Department of Health and Hospitals • Office of Public Health • Bureau of Family Health Early casual formula supplements or bottles (without reasons) can lead to lower milk supply. Delay pacifier/bottle use until baby is several weeks old • Concerns about milk supply are a major reason that mom’s give up on breastfeeding. • • • • Common concern is “whether baby is getting enough” esp. early days when breasts are soft. A woman’s milk supply is perfectly matched with the infant’s stomach size. Informed mothers who know • the size of a newborns stomach (Day1-2) is that of a marble and • feeding adequacy is 5 drops to a teaspoon • with adequate diapers of 1 wet and 1 black stool are reassured and less likely to unnecessarily supplement Knowledge of adequacy each day in the first week yields more confident mothers who exclusively BF in the hospital and longer. Breastmilk is always changing to best meet a human infant’s needs, from: • Colostrum of early days to mature milk • Volume changes based on principle of supply and demand (nurse often, make more) • From foremilk at beginning of a feeding to hind milk that follows • Morning milk is higher volume • Premature infant’s mothers make milk specific for the preemie’s needs • Each exposure of the mother causes her milk to change to protect the baby • • • • Describe in more detail. Talk about “let down” Colostrum is the first breastmilk produces after birth. Colostrum is high in protein which stabilizes baby’s blood sugar levels. Later, breastmilk composition changes during each feeding period. Initially, a baby receives the fore milk which is made up of mostly proteins. This is followed by hind milk which has a higher fat content. Mothers should let the infant begin on a different breast at each feeding and actively breastfeed until infant stops before offering the 2nd breast for decreased fussiness. Ensure that baby is receiving the hind milk (empty 1st breast before feeding on 2nd breast) LA Department of Health and Hospitals • Office of Public Health • Bureau of Family Health • Mother’s milk often gets blamed for the “fussy baby” and other problems, even though it is rarely the real problem. • Ensure that positioning and latch are correct • Evaluate signs of adequate milk production and transfer With assistance during early feeds, prevention and management of nipple pain can promote continued breastfeeding. If nipples are more than tender: refer to LC to assess latch. Breast comfort during first week often depends on whether a mother is breastfeeding often without unnecessary supplements, to avoid excessive engorgement. This is what a successful asymmetric latch should look like Positioning Hold head behind ears Nose to nipple Belly to belly Offer the breast Sandwich hold Stroke nipple from nose to chin rolling out lower lip Bring baby to breast, not breast to baby Check the latch-on Flanged lips, open mouth to 140degrees No pain, no wedged or creased nipple Chin touching breast, asymmetrical latch-on Assess milk transfer Wide jaw excursion Consistent sucking Audible swallowing (after milk “comes in”) **See Resource CD: Checklist for Essentials of Positioning and Latch-on from Lactation Education Resources. Candidiasis: Gradual onset of nipple pain, itching, burning, shooting pains. Pink and/or painful nipple, diaper rash, tongue can be yeast – refer to LC as needed. For external nipple or diaper rash symptoms management may include topical creams (prescribed or over-the-counter) For systemic symptoms PO medications may be prescribed. A tight frenulum has potential to interfere with breastfeeding. Often overlooked, it’s important to know what this looks like Consider frenotomy (clipping of frenulum) or referral to a physician who performs frenotomies Get it early! Some questions to ask o How mobile is the tongue? Can baby stick the tongue out far? Is it heart shaped? o Are there any issues with nipple pain or milk transfer? Continued LA Department of Health and Hospitals • Office of Public Health • Bureau of Family Health A referral to an International Board Certified Lactation Consultant can facilitate a lactation consultation with a breastfeeding assessment and evaluation, as well as collaboration with a physician in the development of a plan that identifies any problems with latch, milk supply or milk transfer, as well as in developing a feeding plan that results in adequate infant feedings, increasing/maintaining an adequate milk supply and developing strategies for resolving any identified milk transfer problems during breast feedings. See slide Late Pre-term: (Birth at 34- 36 6/7 weeks gestation) • The late preterm baby is sometimes described as a “wimpy” baby that’s big enough to room in with mom but really isn’t fully ready to enter the world. • At risk for: hypoglycemia, jaundice, and weight loss due to difficulty with feedings- resulting low milk supply • Late preterm infant disorganization, weak suck, low tone, inability to sustain sucking, and less airway control during feeding combined with maternal high risk conditions (diabetes or PIH treated with magnesium sulfate or diuretics) can result in lower milk supply. • Need more vigilant surveillance to ensure adequate intake, weight gain, and hydration. • • • • • • When a mother calls the office because • “baby won't latch” • “baby is crying a lot" Instead of recommending: “Give a bottle until the nurse gets back to you” Discuss risks of inappropriate formula supplements And provide referrals to lactation consultant Don’t miss opportunities to support breastfeeding at sick visits. Most illnesses will improve more rapidly if the mother continues to provide breast milk • Breastmilk is the easiest thing for baby to digest • And it potentially provides antibodies for the mother’s illness to the baby LA Department of Health and Hospitals • Office of Public Health • Bureau of Family Health • It is perfectly normal, and accepted to continue breastfeeding into toddlerhood in other states/countries • There is no evidence to support adverse outcomes of continuing breastfeeding, and it should be the mother’s decision. • WHO recommendations for breastfeeding: “Exclusive breastfeeding is recommended up to 6 months of age, with continued breastfeeding along with appropriate complementary foods until two years of age or beyond.” • Biting may be a concern as the child gets older, but can be addressed. Mother to mother support is helpful in this situation. • Mom’s menstrual cycle will eventually return, and if she does become pregnant, it can be possible for her to continue breastfeeding with the right support if she chooses to. Emphasize that breastfeeding is a relationship, not just food. It also continues to provide disease/illness preventing substances. • Breastfeeding during a subsequent pregnancy is not unusual. • If the pregnancy is normal and the mother is healthy, breastfeeding during pregnancy is the woman's personal decision. • If younger than two years, the child is at increased risk of illness if weaned. Breastfeeding the nursing child after delivery of the next child (tandem nursing) may help provide a smooth transition psychologically for the older child. Source: Breastfeeding, Family Physicians Supporting (Position Paper). Accessed from http://www.aafp.org/about/policies/all/breastfeeding-support.html. Working moms who are trying to continue breastfeeding need the most support of all. Physicians can play a role in promoting breastfeeding support in workplaces: - Link mothers with pumping supplies. - Educate families about new tax laws which allow mothers to include breastfeeding equipment and supplies as deductible items in their healthcare spending accounts, or use as a tax deduction. - Write letters supporting the mother’s right to pumping breaks; a doctor’s note may give her courage to ask for the breaks and provide some leverage with her employer. Hints for Success: • Encourage mothers to begin a dialogue with their employers • Start storing milk weeks before return date • Express and store at least 1x/day • Pump early AM (to take advantage of high prolactin level at night and larger volume of milk early in morning) • BF and pump as if at work few days before return date • After returning to work • Breastfeed all feedings on weekends/days off and evenings • Some babies will decrease daytime feedings and increase feedings when mother is home Address common concerns: Storing and using expressed milk (resource will be in toolkit) Caution: Do not heat milk in microwave • Remind moms that any breastfeeding is better than none, and her body can adjust if necessary to feeding her infant only in the evenings and mornings if needed. LA Department of Health and Hospitals • Office of Public Health • Bureau of Family Health Presenter: PHYSICIAN Most medications are compatible with breastfeeding • There is a need to be more careful about medicines in the neonatal period (1st month) or in the premature infant because of immaturity of infants’ livers and kidneys. But, historically, far too many mothers have been told that they should not breastfeed because of medication. • There are many easy-to-access resources. • LACTMED can be accessed quickly on rounds with an iPhone. • Tom Hale’s Infant Risk Center of Texas Tech University Health Science Center. Resource for both providers and parents. http://www.infantrisk.com/ • Contraception: If hormonal contraception is to be used in a breastfeeding mother, avoid starting it before lactation is well established, e.g. 6 weeks postpartum. Ideally, a progestin-only method should be used. Do not go into this detailed info unless questions are asked (not enough time) -A newly-released clinical report from the American Academy of Pediatrics (AAP) provides guidance on drug exposure and breastfeeding and reaffirms the recommendation that most medications and immunizations are safe during lactation. The Transfer of Drugs and Therapeutics Into Human Breast Milk: An Update on Selected Topics appears in the journal Pediatrics and clarifies that few medications are contraindicated in breastfeeding mothers, despite the fact that women are often advised to stop taking necessary medications or to discontinue nursing because of potential harmful effects on their infants. The key message of the report is that, after a careful risk/benefit assessment, many medications can and should be continued in lactating women. There are still some drug classes that should be avoided or used cautiously, but overall, when a healthy nursing mother presents to primary care with a common, mild illness, providers can feel comfortable treating her and encouraging her to continue nursing. *Reference the Resource CD and the Leave Behind Materials (Medications and Mothers Milk) Since the AAP supports breastfeeding as the best way to feed infants, many mothers are resistant to discontinue breastfeeding to take a medication. Most medications, antibiotics are fine. We have information to help us make informed decisions. Risks of formula feeding & mother losing milk supply are significant & should not be trivialized. LA Department of Health and Hospitals • Office of Public Health • Bureau of Family Health Just Get Started 1. Pick someone who seems passionate and have them form a team. The team leader must have encouragement and the full support of the doctors and administration. After you establish your team, begin developing a plan to tackle the other steps. The team leader should become familiar with the leave behind materials and Resource CD contents. 2. The next step is to conduct an environmental scan of the office. Are your pictures, posters, print materials commercial-free? Does your office make it obvious that women are welcome to breastfeed? Is there a space for patients (and your own staff) to nurse their babies or express milk? 3. Take a look at how breastfeeding education is delivered to families. It helps to have a structured plan or routine for how individual practitioners (and the office in general) threads breastfeeding education into all regular patient encounters. 4. Also, take a look at whether or not your office doctors and staff know where to refer mothers if they need extra help? Your office team should connect with your local resources and maintain a current directory for referrals. *Resource CD also contains the Academy of Breastfeeding Medicine’sProtocol #14- Breastfeeding-Friendly Physician’s Office: Optimizing Care for Infants and Children, Revised 2013 Being a “breastfeeding-friendly” practice makes good financial sense. • Bill for visits which support breastfeeding. • Billing for time may work better if >50% of the visit is for counseling. • The AAP has a variety of resources to facilitate proper coding, billing and reimbursement for these services. • If a pediatrician is actually diagnosing, examining, and treating a mother, he should be able to bill for that as a visit too. Source: www2.aap.org/breastfeeding/files/pdf/coding.pdf Resource CD: “Supporting Breastfeeding and Lactation: The Primary Care Pediatrician’s Guide to Getting Paid pdf.” Speaker: LACTATION CONSULTANT You may be familiar with the concept of a primary care practice being a patient’s Medical Home. • In this model, you are a connection to and coordinator of resources. Thus it’s important that you know your community! Continued LA Department of Health and Hospitals • Office of Public Health • Bureau of Family Health • Don’t underestimate the mother’s support system, especially the partner’s support. Fathers can be very effective supporters of breastfeeding when they are on board. However, it is important to Know where to send a mom in your area if she is having problems with lactation or if she qualifies for other resources, such as WIC benefits. Any time is a good time to link moms to community support. • Labreastfeedingsupport.org is a website which allows mothers to easily access breastfeeding support by simply entering her zip-code. • Mothers benefit from seeing and talking with other breastfeeding mothers. It’s nice to hear, “my baby did that last month” and realize that her baby’s behavior is normal. • La Leche League and other support groups are a wonderful way for breastfeeding mothers to connect and share experiences. • WIC provides prenatal breastfeeding education and ongoing support after delivery for its participants. Mothers can call their peer counselor for help and information. • Lactation Consultants are available to provide more in depth help when needed. • The Louisiana Breastfeeding Coalition and its regional affiliates like the Acadiana Breastfeeding Coalition and the Greater New Orleans Breastfeeding Awareness Coalition are also available to assist mothers with questions and to promote breastfeeding to the public. -Reference the Resource CD and the medical home one-pager and talking points. Speaker: WIC REPRESENTATIVE • • • • WIC’s mission has always been to provide healthy nutrition for “at-risk” women and children. From the 1950’s to the 1980’s formula feeding became the normal practice for most American women. Now that breastfeeding has been making a resurgence, and its many benefits are being increasingly recognized by public health experts, WIC has become committed to becoming a prime source of breastfeeding support for its clients. Supporting breastfeeding is a top priority for Louisiana WIC. Both hospital grade and personal pumps are available. The Resource CD has the WIC Foods brochures and breastfeeding package. • • The WIC Peer Counselor model can be a very effective way to break down cultural barriers and connect the mother with someone she can talk to on her level. Families receiving WIC benefits visit the site often, so this is an important source of consistent, regular, ongoing support. Continued LA Department of Health and Hospitals • Office of Public Health • Bureau of Family Health • Combining peer counseling with on-going breastfeeding promotion efforts has the potential to: o impact breastfeeding rates among WIC participants, who have traditionally had very low breastfeeding rates o Help moms maintain breastfeeding for longer periods of time. This picture shows the WIC package for fully breastfeeding mothers and babies. The package for the breastfeeding dyad is considered the most generous package that WIC gives out. Speaker: LACTATION CONSULTANT LBC links mothers, families and all sectors of the community to breastfeeding information and resources. Professionals: training & patient education resources, EPICBEST, Ban the Bags, and Bag Free Hospital information Legislation: covers current state & federal breastfeeding laws Partners for Healthy Babies is a project of the Louisiana Department of Health and Hospital's Bureau of Family Health and WIC program. Started in 1993 to help reduce infant mortality in Louisiana. Provides information and resources to women and their families via toll-free helpline (800) 251-BABY (2229) and this website. The website also serves as a resource for Providers and those working to improve the health of mothers and babies in LA. Please spend some time getting familiar with the Resource CD. There are a lot of valuable information and resources. See slide LA Department of Health and Hospitals • Office of Public Health • Bureau of Family Health These materials have been adapted from resources originally developed and used in New Jersey through similar collaboration with state chapters of the American Academy of Pediatrics and the Centers for Disease Control. LA Department of Health and Hospitals • Office of Public Health • Bureau of Family Health