full text
advertisement

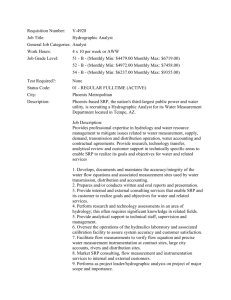
Re-submission to Journal of Clinical Periodontology Title A randomized controlled trial on immediate surgery versus root planing in patients with advanced periodontal disease: a cost-effectiveness analysis Running title Cost-effectiveness of periodontal treatment alternatives Keywords Periodontitis, randomized controlled trial, surgery, scaling and root planing, costeffectiveness, azithromycin Authors Seyed Reza Miremadi, Hugo De Bruyn, Harold Steyaert, Katrijn Princen, Mehran Moradi Sabzevar, Jan Cosyn Affiliations and Institutions Miremadi SR1, De Bruyn H1,2, Steyaert H1, Princen K1, Sabzevar MM3, Cosyn J1,3 1 University of Ghent, Faculty of Medicine and Health Sciences, Dental School, Department of Periodontology and Oral Implantology, De Pintelaan 185, B-9000 Ghent, Belgium 2 Malmö University, Faculty of Odontology, Department of Prosthodontics, 205 06 Malmö, Sweden 3 Free University of Brussels (VUB), Faculty of Medicine and Pharmacy, Dental Medicine, Laarbeeklaan 103, B-1090 Brussels, Belgium Contact address corresponding author Seyed Reza Miremadi University of Ghent, Faculty of Medicine and Health Sciences, Dental School, Department of Periodontology and Oral Implantology, De Pintelaan 185, B-9000 Ghent, Belgium E-mail: resa.miremadi@ugent.be Conflict of interest and source of funding statement The authors declare that they have no conflicts of interest. This study was supported by departmental funds. Clinical relevance Scientific rationale for the study: Studies focusing on cost-effectiveness of periodontal treatment are scarce. Yet, considering the limitations in individual and social economic resources, an economic assessment of different treatment modalities is an important issue. Principal findings: Immediate surgery and SRP, both followed by re-debridement and systemic azithromycin at 6 months, were equally effective in terms of clinical outcome. Surgery was significantly more expensive than SRP, but proved more beneficial in terms of supportive care and the need for systemic antibiotics. Practical implications: Surgery yields higher cost than SRP, but may reduce the need for supportive care and systemic antibiotics. ABSTRACT Aim: To compare immediate surgery to scaling and root planing (SRP) in the treatment of advanced periodontal disease focusing on the prevalence of residual sites and costeffectiveness (1); to evaluate the adjunctive effects of azithromycin in a second treatment phase (2). Materials and methods: Thirty-nine patients (18 males, 21 females; mean age: 54.6) received oral hygiene instructions and were randomly allocated to surgery (n=19) or SRP (n=20). Patients with residual pockets (≥6 mm) at 6 months received re-debridement of these sites and systemic azithromycin. Treatment groups were followed up to 12 months and evaluated in terms of clinical response parameters and cost-effectiveness. Chair-time was used to assess the financial impact of treatment. Results: Both treatment arms were equally effective in terms of clinical outcome demonstrating less than 1 % residual pockets at 12 months. Surgery imposed an extra 746 Euro on the patient up to 6 months when compared to SRP. At 12 months, 46 Euro of this amount could be offset as a result of a reduced need for supportive care. Only 6 patients in the surgery group needed systemic antibiotics, whereas 14 patients in the SRP needed such additional treatment. Conclusions: Although 700 Euro could be saved on average by performing SRP instead of surgery, the latter significantly reduced the need for supportive care and systemic antibiotics. Introduction The treatment of chronic periodontitis aims at arresting the inflammatory process of the disease through subgingival biofilm removal (Heitz-Mayfield et al., 2002). This can be performed using non-surgical and surgical approaches leading to significant clinical improvements, provided the patient maintains an adequate oral hygiene throughout the treatment and the maintenance phase (Lindhe and Nyman, 1975, Axelsson and Lindhe, 1981). The choice of the treatment approach can be a matter of debate. The traditional treatment concept includes plaque control measures and non-surgical scaling and root planing (SRP) followed by surgical re-treatment where indicated. A number of reasons can motivate this staged treatment concept. For one thing, peroperative conditions may be more favorable when marginal inflammation has subsided after non-surgical debridement. On the other hand, surgical treatment is usually needed in patients with advanced periodontal disease and therefore surgery without non-surgical pre-treatment could be considered valuable in these patients. Hence, the primary objective of the present clinical study was to compare the clinical outcome of immediate surgery to traditional SRP in patients with advanced periodontal disease focusing on residual or poorly responding sites and cost-effectiveness. The research hypothesis was that surgery would result in less residual sites when compared to SRP, yet at significantly higher cost. Residual sites are usually treated by means of systemic antibiotics when all mechanical approaches have failed. Azithromycin seems a promising drug because of a number of reasons. First, it has a relatively long half-life, allowing a once daily administration of 500mg during 3 days, hereby reducing the likelihood of noncompliance (Foulds et al., 1990). Second, azithromycin demonstrates limited adverse effects (Oteo et al., 2010). At least in a number of clinical studies, azithromycin significantly improved the outcome of non-surgical SRP in the treatment of periodontitis (Smith et al., 2002, Haffajee et al., 2007, Gomi et al., 2007), yet its potentially additional value in the management of residual sites remains to be investigated. Hence, the secondary objective was to evaluate the clinical outcome of adjunctive use of azithromycin to non-surgical re-treatment of residual sites. Materials and Methods Patient Sample A prospective, monocentre, single-masked, randomized controlled 12-month study was conducted in adult patients with generalized advanced chronic periodontitis. Patients were recruited between January 2009 and August 2009 at the specialist clinic of the Department of Periodontology of the University of Ghent, Belgium. The study was conducted in accordance with the Helsinki declaration of 1975 as revised in 2008 and the protocol was approved by the ethical committee of the University Hospital of Ghent. Inclusion and exclusion criteria were as follows. Inclusion criteria - At least 35 years old - At least 20 teeth present - At least one site per quadrant with probing pocket depth (PPD) ≥6 mm, bleeding on probing (BoP) and bone loss surpassing one third of the root length as assessed on peri-apical radiographs - Signed informed consent Exclusion criteria - Systemic disease - Subgingival instrumentation within 2 years prior to the study - Use of antibiotics within 6 months prior to the study - Compromised medical condition implying the need for prophylactic use of antibiotics - Subjects wearing removable prostheses or undergoing orthodontic therapy - Pregnancy or lactating female candidates - Confirmed or suspected intolerance to macrolides Patients who used systemic antibiotics during follow-up beyond the study protocol were excluded from that moment on. Third molars and sites adjacent to teeth that were extracted prior to or in the course of periodontal therapy were excluded. Such exclusion was carried out due to the recession of soft tissue occurring subsequent to extraction, which could bias the analysis of clinical attachment level. Screening and randomization After screening, baseline data were recorded by one examiner (S.R.M.) who also performed all registrations at subsequent timepoints. At baseline, full-mouth peri-apical radiographs were taken. On the basis of these radiographs and clinical measurements, the prognosis of each tooth was determined and teeth irrational to treat were extracted before or in the course of periodontal treatment. Group allocation was based on a computer-generated list using simple randomization provided by a study team member who was not clinically involved in the study (J.C.). According to the list, patients were assigned to one of the two treatment groups; scaling and root planing or surgery (figure 1). During the study period, the examiner who performed the measurements was blinded to the type of treatment. All treatment procedures were carried out by two periodontists (H.S. and K.P.) and surgical procedures were supervised by the same clinician (I.W.). One month prior to baseline registration, all patients were given meticulous instructions regarding self-performed oral hygiene measures. This included manual toothbrushing along with interdental cleaning (TePe toothbrushes and interdental brushes, TePe Munhygienprodukter AB , Malmö, Sweden). Two weeks afterwards as well as at all other timepoints (baseline, 3, 6 and 12 months), oral hygiene was evaluated and reinforced, if necessary. Group “scaling and root planing” Patients allocated to this group received SRP using an ultrasonic device (Satelec P5 Newtron®, Acteon group, Bilbao, Spain) and manual curettes. The treatment was carried out in 2 sessions (right side, left side) under local anesthesia with 1 week in between. There was no time limitation imposed and the endpoint of treatment was reached when a smooth calculus-free root surface was achieved as deemed by the clinician. Patients were provided with a prescription of paracetamol 500mg. At 3 months, supragingival plaque and calculus were removed, if spotted. Teeth were polished at each visit using rubber cups and a lowabrasive polishing paste (Zircate® prophy paste, Dentsply, Milford, DE, USA). Patients showing residual pockets ≥6 mm deep at the 6 month re-assessment, were additionally treated by means of systemic azithromycin (500mg, per os, once daily for 3 days) in conjunction to non-surgical re-debridement of these sites. Other patients did not receive additional active therapy. All patients were invited at 12 months to assess the final clinical outcome. Residual pocket at 12 months underwent re-debridement. Group “Surgery” Patients allocated to this group received open flap debridement (access flap at all sites, osseous re-contouring, soft tissue reposition) using an ultrasonic device (Satelec P5 Newtron®, Acteon group, Bilbao, Spain) and manual curettes. The treatment was performed in 4 sessions (quadrant basis) with 1 week in between. Osseous surgery was done in the sense of eliminating or reducing intra-osseous defects, hereby restoring a physiologic bone architecture. If necessary, soft tissue was thinned out for better adaptation. There was no time limitation imposed. Polylactic sutures (Vicryl Rapide, Ethicon, Johnson & Johnson, NJ, United States) were used to obtain wound closure and these were removed after 7 days. Patients were provided with a prescription of paracetamol 500mg. The follow-up of these patients was identical to the follow-up of patients allocated to the SRP group (see above). Again, patients with residual pockets received additional treatment at 6 months on the basis of non-surgical re-debridement and systemic azithromycin. Residual pocket at 12 months underwent re-debridement. (Here approximately Figure 1 please) Examinations At baseline, 6 and 12 months, the following clinical recordings were sequentially registered by the same clinician (S.R.M.). 1- Probing pocket depth (PPD) measured at 6 sites per tooth (mesial, central, distal; orally and buccally) using a manual probe (CP15 UNC, Hu-Friedy, Chicago, IL, United States). At follow-up, pockets ≤3mm in depth were defined as “closed” and pockets ≥6mm were defined as “residual”. 2- Bleeding on probing (BoP) registered 15 seconds following pocket probing. A dichotomous score (0: no bleeding; 1: bleeding) was given. The gathered data were subsequently transformed into percentage of bleeding sites. 3- Plaque index (PI) (Quigley & Hein, 1962) measured at six sites per tooth (mesial, central, distal; orally and buccally) following the application of a plaque disclosing agent (Svenska®, Svenska Dental Instrument AB, Upplands, Väsby, Sweden). The scores ranged from 0 to 5. 4- Clinical attachment level (CAL) calculated for each site as the sum of PPD and gingival recession (recession was given a positive value, overgrowth a negative one). 5- Patient discomfort was assessed using a VAS score (ranging from “no pain” to “extremely intolerable pain”) one week after each treatment session in a separate room without clinicians being present. The total number of painkillers taken by the patient after each treatment session was also noted. The breakdown of chair-time and cost is presented in table 1. The actual chair-time relating to the first active treatment phase was recorded for each patient. The chair-time and associated cost for all other visits were estimated based on the standard time schedule imposed by the administration of the University Hospital. Residual pockets and cost-effectiveness were considered as primary outcome variables, while others were considered as secondary. (Here approximately Table 1 please ) Calibration session The clinician (S.R.M.) who performed all clinical recordings was calibrated prior to the start of the study. Four patients suffering from chronic periodontitis were enrolled for this purpose. Duplicate measurements (n=489) for PI, PPD and CAL were collected with an interval of 30 minutes between the first and the second recording. Sample size calculation Calculations were based on data from a randomized controlled study comparing different types of periodontal therapy in patients with advanced periodontal disease (Cosyn et al., 2007). Based on a mean difference in PPD of 0.5mm between the groups at 6 months, standard deviations of 0.55 mm for both groups, an alpha error of 5% and statistical power of 80%, a sample size of 15 patients per group was found. To compensate for drop-outs, 20 patients were included in the SRP group and 20 in the surgery group. Statistical analysis Data analysis was performed using the patient as the experimental unit. Data from all patients were utilized, as an intention-to-treat analysis was conducted. Intra-examiner repeatability on PI, PPD and CAL was evaluated using Spearman’s correlation coefficient. Mean values were calculated for all continuous variables and frequency distributions were constructed for categorical variables. The Mann-Whitney test was used to compare groups in terms of age, mean number of teeth per patient (overall and split up into molars and teeth with furcation involvement), mean baseline PPD (full-mouth and per stratum), mean baseline CAL (fullmouth and per stratum), mean baseline PI (full-mouth), mean baseline BOP (full-mouth), mean chair-time , mean cost, mean VAS scores and the percentage of closed and residual pockets. The Fisher’s exact test was used to compare the number of drop-outs and males/females between the groups. PPD, CAL, PI and BOP alterations were evaluated using repeated measures ANOVA with the patient as a random factor and the group and time as fixed factors. The level of significance was set at 0.05. Results Forty patients were initially recruited; yet, 1 patient withdrew from the study prior to treatment. Of the 39 patients undergoing treatment, 35 patients completed the 12-month follow-up period. A description of the patient sample is given in table 2. Three patients dropped out due to lack of compliance with the scheduled appointments and 1 patient withdrew from the study after the first flap operation due to “intolerable pain” as described by the patient. As can be seen in table 1, there were no significant differences between the groups at baseline in terms of drop-outs, gender, age, smoking habits, number of teeth and degree of periodontal destruction (p≥0.061). An individual smoking more than 5 cigarettes per day was considered a smoker. Intra-examiner repeatability on PI, PPD and CAL was satisfying (Spearman’s correlation coefficients ≥0.851; p<0.001). (Here approximately table 2 please) Results up to 6-months Closed and residual pockets At the 6-month reassessment, on average 77.3%±14.0 of the pockets in the SRP group were ≤ 3mm deep and were considered “closed” by definition, whilst in the surgery group 88.8%±8.3 of the pockets were “closed”. At the same time point, 8.6%±9.4 of the pockets in the SRP group were ≥ 6mm and were considered “residual” by definition. In the surgery group this amounted to 1.0%±1.8. The differences between the groups in terms of both “closed” and “residual” pockets were statistically significant at 6 months (p<0.001) (fig. 2). (Here approximately Figure 2 please) Cost-effectiveness Chair-time was significantly longer for surgery than for SRP (315 min vs. 441 min, p<0.001) and resulted in 7.6% less residual pockets at 6 months as already described (Table 3). This difference in chair-time corresponded to a disparity in cost of 746 Euro in favor of SRP. Hence, the ICER at 6 months amounted to 98, meaning an extra 98 Euro would be spent on average by the patient to achieve 1% extra reduction in the proportion of residual pockets. (Here approximately Table 3 please) Probing pocket depth (PPD) alterations Initially, there were no significant differences between the groups with respect to PPD (p=0.663). Baseline mean full-mouth PPD was 3.7±0.7mm for the SRP group and 3.6±0.5 for the surgery group. At 6 months, both groups showed significant reduction compared to baseline with mean full-mouth PPD of 2.9±0.6mm for the SRP group and 2.7±0.3mm for the surgery group (p<0.001), yet a significant treatment-time interaction could not be demonstrated (p=0.100). PPD data were also analyzed on the basis of different pocket depth strata, defined as follows: shallow (≥ 3mm), medium (4-5mm) and deep (≥6mm). All strata followed a similar course as full-mouth PPD demonstrating a significant time effect (p<0.001), yet a significant treatment-time interaction could not be demonstrated (p≥0.082) (Table 4). CAL alterations Initially, there were no significant differences between the groups in terms of CAL (p=0.325) as mean full-mouth CAL was 5.0±1.0mm for the SRP group and 4.7±0.6 for the surgery group. At 6 months, both groups showed significant reduction compared to baseline with mean full-mouth CAL of 4.9±0.2mm for the SRP group and 4.4±0.1mm for the surgery group (p<0.001), without any significant treatment-time interaction (p=0.811). CAL data were also analyzed on the basis of different pocket depth strata. All strata followed a similar course as full-mouth CAL demonstrating a significant time-effect (p<0.001). No significant treatmenttime interaction could be established (p≥0.081) (Table 4). (Here approximately Table 4 please) PI and BOP alterations There were no significant differences between the groups at baseline with regard to PI values, pointing to 1.1±0.4 and 1.3±0.5 for SRP and surgery, respectively. At 6 months, a significant reduction was observed in both groups as PI amounted to 0.7±0.4 and 0.7±0.4 for SRP and surgery, respectively (p<0.001). A significant treatment-time interaction could not be demonstrated (p=0.317). No significant differences were found between the groups at baseline in terms of BOP (p=0.694), pointing to 70.1%±22.0 and 68.0%±22.9 for SRP and surgery, respectively. At 6 months, both groups demonstrated a significant reduction in BOP (p<0.001) as BOP values amounted to 21.9%±12.6 and 15.9%±2.9 for SRP and surgery, respectively. No significant treatment-time interaction was found (p=0.903). Patient discomfort The mean VAS score for the SRP group was 40±19, while it amounted to 43±32 for the surgery group. The difference between the groups was not statistically significant (p=0.780). The mean number of painkillers taken by the patients in the SRP group was comparable to the amount taken by patients in the surgery group (p=0.272) pointing to 10.6 and 7.5, respectively. 6-to 12-month results Closed and residual pockets As shown in figure 2, 14 patients out of 17 in the SRP group showed residual pockets at 6 months, while in the surgery group 6 patients out of 18 met this criterion. At the 12-month reassessment, the 14 patients of the SRP group who received the second phase of treatment, showed significant improvements compared to the 6-month re-assessment in terms of fullmouth PPD, CAL and BOP. Similar observations were found for the 6 patients of the surgery group who received the second phase of treatment. The percentage of “closed” and “residual” pockets also showed significant improvements between 6 and 12 months in both groups, finally pointing to 87.4±5.0% and 1.0±1.8%, respectively for the SRP group (p<0.001). In the surgery group, the percentage of “closed” and “residual” pockets were 91.0±8.0% and 1.0±1.2% at study termination, respectively (p≤0.027). When comparing the groups with each other in terms of the percentage of residual and closed pockets at study termination, there were no statistically significant differences (p≥0.130). Cost-effectiveness As can be seen in table 3, chair-time and associated cost between 6 and 12 months were statistically significantly lower for the surgery group compared to SRP. That is, 27 minutes on average could be saved by surgery corresponding to a cost saving of 45 Euro. Yet, this cost saving could not offset the higher initial cost of surgery when calculating the total cost of up to 12 months (1445 Euros vs. 745 Euros, p<0.001). This is especially important since the outcome in the proportion of residual pockets was very low and similar after 1 year in both groups (< 1%). Discussion In this randomized controlled trial, surgery as initial treatment was compared to SRP in patients with advanced periodontal disease. Both therapies were effective in reducing PPD, CAL and BOP, which is in accordance with a number of studies (Lindhe et al., 1984, Pihlstrom et al., 1984, Ramfjord et al., 1987, Badersten et al., 1990, Serino et al., 2001). At least in terms of mean changes up to 6 months, surgery performed equally well as SRP. Interestingly, Serino and co-workers (2001) evaluated the outcome of immediate surgery versus SRP in single-rooted teeth and demonstrated significantly more PPD and CAL reduction following surgical treatment, particularly in deep pockets. Although this could not be confirmed in this study, frequency distributions on residual and closed sites did reveal significant disparities between the groups with surgery delivering 7.6% less residual pockets than SRP. This finding illustrates that the assessment of clinical effectiveness on the basis of mean values can be misleading as residual pockets might be overlooked in the shadow of calculating such mean values. However, the prevalence of residual sites is imperative as these have been shown to be at risk for additional attachment loss, which in turn increases the risk for tooth loss (Claffey and Egelberg, 1995, Matuliene et al., 2008). In the present study, surgery took significantly more time than SRP. Consequently, surgery imposed significantly higher cost on the patient than SRP, thereby confirming our research hypothesis. Calculation revealed that patients undergoing surgical treatment would need to pay on average an extra 746 Euro up to 6 months for delivering 7.6% less residual pockets than SRP. This difference could be reduced to 700 Euro at 12 months since surgery reduced the need for supportive treatment. Considering the fact that both treatment modalities were equally effective in the end in terms of residual pockets (< 1%), one could question the costeffectiveness of surgery. On the other hand, surgery reduced the need for antibiotic therapy by more than half (6 vs. 14 patients). This is important as it lowers the risk for antibiotic resistance and its associated cost for society. To the best of our knowledge there are no comparable studies on cost-effectiveness of periodontal therapy in the literature. Economic assessment of periodontal treatment can be approached from different angles using cost-effectiveness, cost-utility or cost-benefit analyses (Antczak-Bouckoms and Weinstein, 1987, Gaunt et al., 2008). A cost-utility analysis was performed by Antczak-Bouckoms and Weinstein (1987) using an index called “qualityadjusted tooth years” (QATY). They concluded that SRP imposed lower cost on the patient than surgical alternatives, while maximizing expected QATYs. However, the study was criticized for not taking the maintenance phase into account (Kraal, 1988). In addition, it seems that the side effects of treatment alternatives were heavily weighted, hereby somewhat overshadowing the clinical effectiveness of therapy. Despite the fact that our results also showed higher cost for surgery, the present study cannot be compared to the study of Antczak-Bouckoms and Weinstein (1987). For one thing, we performed a cost-effectiveness analysis, while Antczak-Bouckoms and Weinstein (1987) assessed cost-utility. Furthermore, well-defined and generally accepted success criteria to which cost can be related, would be needed for an unbiased comparison. Tooth loss can be considered an ideal variable for the assessment of periodontal treatment effectiveness in the long term (Serino et al., 2001, Rosling et al., 2001). However, short-term studies can only adopt surrogate variables such as residual sites. In the current trial, a second phase of treatment commenced for patients with residual sites at 6 months due to the ethical obligation of limiting ongoing disease. Azithromycin was chosen for this purpose given earlier promising results in the context of periodontal therapy (Smith et al., 2002, Gomi et al., 2007). The combination of SRP and systemic azithromycin led to significant improvements in PPD, CAL, BOP and the percentage of residual pockets. A number of limitations must be considered when interpreting the results of the present study. First, a model for cost assessment was used in this study, which may compromise the external validity of research findings. In this respect, variability in terms of surgical skills and associated chair-time and variability in the charge for certain care, may have a substantial impact on final treatment cost. In addition, one should take into account that chair-time for aftercare was estimated in this study based on the standard time schedule imposed by the administration of the University Hospital. Second, elucidating the exact effects of azithromycin on the final outcome might be complicated considering no placebo was used in this trial. On the other hand, repeated SRP has been shown to be of little value (Badersten et al., 1984), and therefore a relevant impact of Azithromycin seems realistic. In conclusion, immediate surgery and SRP, both followed by re-debridement and systemic azithromycin at 6 months, were equally effective in terms of clinical outcome demonstrating less than 1 % residual pockets at 12 months. Surgery imposed an extra 746 Euro on the patient up to 6 months when compared to SRP. At 12 months, 46 Euro of this amount could be offset as a result of a reduced need for supportive care. Although the final cost disparity of 700 Euro remains discernible, surgery reduced the need for antibiotic therapy by more than 50 %. Acknowledgements The authors wish to thank Mrs. Iris Wyn for her valuable contribution to this study. References Antczak-Bouckoms, A. A. & Weinstein, M. C. (1987) Cost-effectiveness analysis of periodontal disease control. J Dent Res 66, 1630-1635. Axelsson, P. & Lindhe, J. (1981) The significance of maintenance care in the treatment of periodontal disease. J Clin Periodontol 8, 281-294. Badersten, A., Nilveus, R. & Egelberg, J. (1984) Effect of nonsurgical periodontal therapy. III. Single versus repeated instrumentation. J Clin Periodontol 11, 114-124. Badersten, A., Nilveus, R. & Egelberg, J. (1990) Scores of plaque, bleeding, suppuration and probing depth to predict probing attachment loss. 5 years of observation following nonsurgical periodontal therapy. J Clin Periodontol 17, 102-107. Claffey, N. & Egelberg, J. (1995) Clinical indicators of probing attachment loss following initial periodontal treatment in advanced periodontitis patients. J Clin Periodontol 22, 690-696. Cosyn, J., Wyn, I., De Rouck, T. & Sabzevar, M. M. (2007) Subgingival chlorhexidine varnish administration as an adjunct to same-day full-mouth root planing. I. Clinical observations. J Periodontol 78, 430-437. doi:10.1902/jop.2007.060221. Foulds, G., Shepard, R. M. & Johnson, R. B. (1990) The pharmacokinetics of azithromycin in human serum and tissues. J Antimicrob Chemother 25 Suppl A, 73-82. Gaunt, F., Devine, M., Pennington, M., Vernazza, C., Gwynnett, E., Steen, N. & Heasman, P. (2008) The cost-effectiveness of supportive periodontal care for patients with chronic periodontitis. J Clin Periodontol 35, 67-82. doi:CPE1261 [pii] 10.1111/j.1600-051X.2008.01261.x. Gomi, K., Yashima, A., Nagano, T., Kanazashi, M., Maeda, N. & Arai, T. (2007) Effects of full-mouth scaling and root planing in conjunction with systemically administered azithromycin. J Periodontol 78, 422-429. doi:10.1902/jop.2007.060247. Haffajee, A. D., Torresyap, G. & Socransky, S. S. (2007) Clinical changes following four different periodontal therapies for the treatment of chronic periodontitis: 1-year results. J Clin Periodontol 34, 243-253. doi:CPE1040 [pii] 10.1111/j.1600-051X.2006.01040.x. Heitz-Mayfield, L. J., Trombelli, L., Heitz, F., Needleman, I. & Moles, D. (2002) A systematic review of the effect of surgical debridement vs non-surgical debridement for the treatment of chronic periodontitis. J Clin Periodontol 29 Suppl 3, 92-102; discussion 160-102. doi:012 [pii]. Kraal, J. H. (1988) Cost-effectiveness analysis of periodontal disease control. J Dent Res 67, 611. Lindhe, J. & Nyman, S. (1975) The effect of plaque control and surgical pocket elimination on the establishment and maintenance of periodontal health. A longitudinal study of periodontal therapy in cases of advanced disease. J Clin Periodontol 2, 67-79. Lindhe, J., Westfelt, E., Nyman, S., Socransky, S. S. & Haffajee, A. D. (1984) Long-term effect of surgical/non-surgical treatment of periodontal disease. J Clin Periodontol 11, 448-458. Matuliene, G., Pjetursson, B. E., Salvi, G. E., Schmidlin, K., Bragger, U., Zwahlen, M. & Lang, N. P. (2008) Influence of residual pockets on progression of periodontitis and tooth loss: results after 11 years of maintenance. J Clin Periodontol 35, 685-695. doi:CPE1245 [pii] 10.1111/j.1600-051X.2008.01245.x. Oteo, A., Herrera, D., Figuero, E., O'Connor, A., Gonzalez, I. & Sanz, M. (2010) Azithromycin as an adjunct to scaling and root planing in the treatment of Porphyromonas gingivalis-associated periodontitis: a pilot study. J Clin Periodontol 37, 1005-1015. doi:CPE1607 [pii] 10.1111/j.1600-051X.2010.01607.x. Pihlstrom, B. L., Oliphant, T. H. & McHugh, R. B. (1984) Molar and nonmolar teeth compared over 6 1/2 years following two methods of periodontal therapy. J Periodontol 55, 499-504. Ramfjord, S. P., Caffesse, R. G., Morrison, E. C., Hill, R. W., Kerry, G. J., Appleberry, E. A., Nissle, R. R. & Stults, D. L. (1987) 4 modalities of periodontal treatment compared over 5 years. J Clin Periodontol 14, 445-452. Rosling, B., Serino, G., Hellstrom, M. K., Socransky, S. S. & Lindhe, J. (2001) Longitudinal periodontal tissue alterations during supportive therapy. Findings from subjects with normal and high susceptibility to periodontal disease. J Clin Periodontol 28, 241-249. Serino, G., Rosling, B., Ramberg, P., Socransky, S. S. & Lindhe, J. (2001) Initial outcome and long-term effect of surgical and non-surgical treatment of advanced periodontal disease. J Clin Periodontol 28, 910-916. doi:281003 [pii]. Smith, S. R., Foyle, D. M., Daniels, J., Joyston-Bechal, S., Smales, F. C., Sefton, A. & Williams, J. (2002) A double-blind placebo-controlled trial of azithromycin as an adjunct to non-surgical treatment of periodontitis in adults: clinical results. J Clin Periodontol 29, 54-61. doi:290109 [pii]. Table 1. Chair-time and cost calculation algorithm Baseline up to 6 months Baseline diagnosis (60’, 100€) Initial treatment (SRP: 100€/h, Surgery: 200€/h) 3 months: supragingival plaque control (30’, 50€) 6 months: re-evaluation (30’, 50€) 6 to 12-month analysis 6 months: supportive treatment (30’, 50€) + supplement of 15’ and 25€ per quadrant with residual pockets 12 months: re-evaluation (30’, 50€) 12 months: supportive treatment (30’, 50€) + supplement of 15’ and 25€ per quadrant with residual pockets Table 2. Overview of the study population at baseline Treatment groups SRP Surgery Total No. of Enrolled 20 20-1* 39 patients Drop-out 3 1 4 p=0.322 Gender (male/female) 9/11 9/10 18/21 p=0.560 Mean age (range) Smoker 57.7(35.0- 51.2(35.0- 54.6(35.0-79.0) 79.0) 75.0) p=0.061 5 5 10 p=0.600 Mean number of teeth / 24.7 (22-28) 25.4 (22-30) patient (range) Mean number of molars / p=0.259 5.9 (4-8) 6.2 (4-8) patient (range) Mean number of teeth with 25.0 6.0 p=0.408 4.4 (3-6) 4.5 (3-6) 4.4 p=0.678 furcation involvement / patient (range) Mean full-mouth PPD (± 3.7 (± 0.7) 3.6 (± 0.5) p=0.663 SD) Mean full-mouth CAL (± 5.0 (± 1.0) 4.7 (± 0.6) 4.8 (± 0.9) p=0.325 SD) Mean full-mouth PI (± SD) 3.6 (± 0.6) 1.1±0.4 1.3±0.5 1.19 (± 0.6) p=0.191 Mean full-mouth BOP (± SD) * 1 patient was never treated SD Standard deviation 70.1% (± 22.0) 68.0% (± 22.9) 69.9% (± 22.1) p=0.694 Table 3. Chair-time and estimated imposed cost on the patient for the two treatment arms Chair-time up to 6 months Cost up to 6 months Chair-time 612 months Cost 6 -12 months Total cost up to 12 months SRP group 315 (240360) 525 (400600) 131 (90-150) 219 (150250) 745 (625850) Surgery group 441 (400480) 1271 (12001400) 104 (90-165) 174 (150275) 1445 (12501650) Inter-group p-value p<0.001 p<0.001 p=0.002 p=0.002 p<0.001 Mean (range) Table 4. The evolution of PPD and CAL through the first 6 months of the study for each pocket depth stratum (± Standard deviation) Timepoint Outcome variable PPD (shallow pockets) PPD (medium pockets) PPD (deep pockets) CAL (shallow pockets) CAL (medium pockets) CAL (deep pockets) Inter-group p-value Baseline 3 months 6 months SRP: 2.7±0.4 Surgery: 2.6±0.2 SRP: 4.2±0.3 Surgery: 4.4±0.3 SRP: 6.3±0.7 Surgery: 6.2±0.6 SRP: 4.1±0.8 Surgery: 3.6±0.7 SRP: 5.8±0.9 Surgery: 5.6±0.5 SRP: 7.9±1.1 Surgery: 7.3±0.7 SRP: 2.4±0.2 Surgery: 2.3±0.2 SRP: 2.4±0.2 Surgery: 2.3±0.2 p=0.193 SRP: 3.0±0.3 Surgery: 2.8±0.3 SRP: 3.0±0.3 Surgery: 2.8±0.2 p=0.082 SRP: 3.3±0.6 Surgery: 3.0±0.3 SRP: 3.4±0.6 Surgery: 3.0±0.3 p=0.449 SRP: 4.0±0.8 Surgery: 3.7±0.7 SRP: 4.0±0.8 Surgery: 3.8±0.7 p=0.081 SRP: 5.3±0.9 Surgery: 5.1±0.5 SRP: 5.4±0.9 Surgery: 5.1±0.5 p=0.133 SRP: 6.8±1.0 Surgery: 6.1±0.5 SRP: 6.9±1.0 Surgery: 6.1±0.5 p=0.577 Figure Legends: Figure 1: The study flowchart Figure 2: Evolution of the periodontal health of the study population during the study period