Michelle - U
advertisement
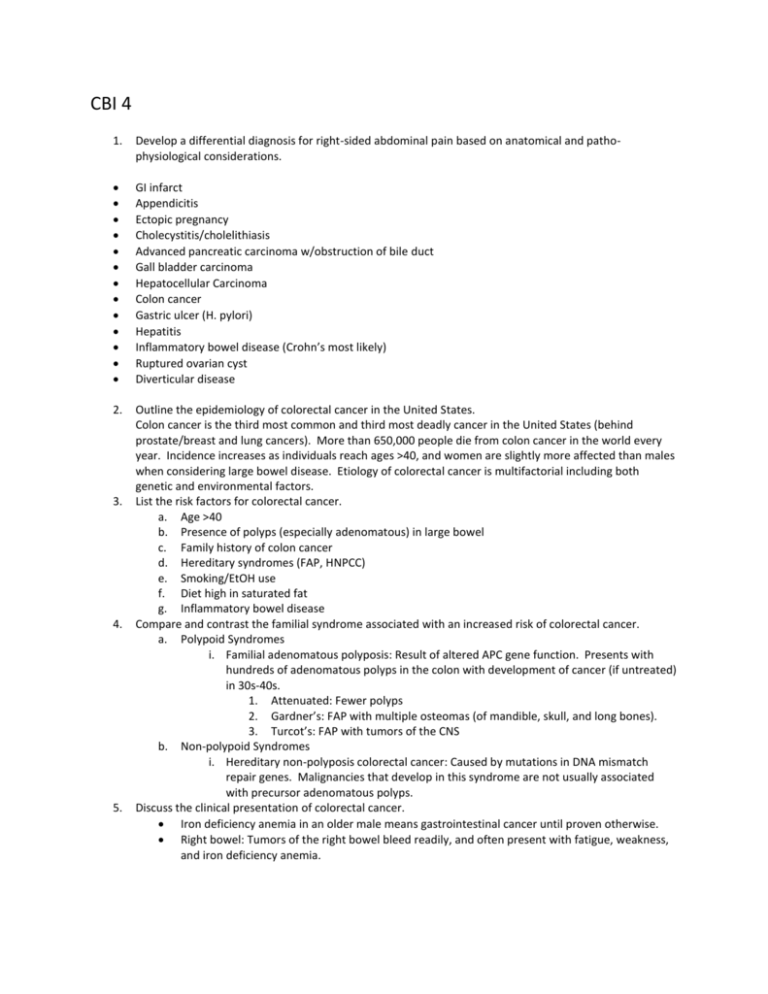
CBI 4 1. Develop a differential diagnosis for right-sided abdominal pain based on anatomical and pathophysiological considerations. GI infarct Appendicitis Ectopic pregnancy Cholecystitis/cholelithiasis Advanced pancreatic carcinoma w/obstruction of bile duct Gall bladder carcinoma Hepatocellular Carcinoma Colon cancer Gastric ulcer (H. pylori) Hepatitis Inflammatory bowel disease (Crohn’s most likely) Ruptured ovarian cyst Diverticular disease 2. Outline the epidemiology of colorectal cancer in the United States. Colon cancer is the third most common and third most deadly cancer in the United States (behind prostate/breast and lung cancers). More than 650,000 people die from colon cancer in the world every year. Incidence increases as individuals reach ages >40, and women are slightly more affected than males when considering large bowel disease. Etiology of colorectal cancer is multifactorial including both genetic and environmental factors. List the risk factors for colorectal cancer. a. Age >40 b. Presence of polyps (especially adenomatous) in large bowel c. Family history of colon cancer d. Hereditary syndromes (FAP, HNPCC) e. Smoking/EtOH use f. Diet high in saturated fat g. Inflammatory bowel disease Compare and contrast the familial syndrome associated with an increased risk of colorectal cancer. a. Polypoid Syndromes i. Familial adenomatous polyposis: Result of altered APC gene function. Presents with hundreds of adenomatous polyps in the colon with development of cancer (if untreated) in 30s-40s. 1. Attenuated: Fewer polyps 2. Gardner’s: FAP with multiple osteomas (of mandible, skull, and long bones). 3. Turcot’s: FAP with tumors of the CNS b. Non-polypoid Syndromes i. Hereditary non-polyposis colorectal cancer: Caused by mutations in DNA mismatch repair genes. Malignancies that develop in this syndrome are not usually associated with precursor adenomatous polyps. Discuss the clinical presentation of colorectal cancer. Iron deficiency anemia in an older male means gastrointestinal cancer until proven otherwise. Right bowel: Tumors of the right bowel bleed readily, and often present with fatigue, weakness, and iron deficiency anemia. 3. 4. 5. Left bowel: Tumors of the left bowel present with occult bleeding, crampy left lower quadrant discomfort, diarrhea, and constipation. These are easier to detect due to significant changes in bowel habit. 6. Discuss the clinical work up for suspected colorectal cancer. a. Labs: CBC, liver function panel, pancreatic enzymes. b. Imaging: CT with contrast, PET-CT. c. Procedures: Sigmoidoscopy/colonoscopy. Biopsy. 7. Discuss the pathology of colorectal cancer and correlate stage with survival outcomes. Pathology: Structures within a colorectal adenocarcinoma may range from well differentiated (presence of glands that look similar to normal colonic epithelium containing tall columnar cells with normal appearing nucleii) to poorly differentiated (absence of gland formation with formation of anaplastic masses and irregular cellular features). Stages: o Tis: Carcinoma in-situ o T1: Carcinoma penetrates through muscularis mucosa o T2: Carcinoma enters muscularis propria o T3: Carcinoma penetrates through muscularis propria o T4: Carcinoma penetrates through serosa/adventitia o N0: No nodal involvement o N1: 1-3 nodes involved o N2: 4+ nodes involved o M0: No distant metastases o M1: + distant metastases The more advanced the stage (indicating more extensive disease) the worse the prognosis. 8. Present the treatment options for colorectal cancer and the follow-up plan. a. Local excision b. Partial or complete bowel resection c. Systemic Chemotherapy: 5FU is the gold standard for treatment of colorectal cancer, but studies are being done that examine the effectiveness of multi-drug therapy regimens (5FU + pyrimidine antagonists/platinums/topoisomerase inhibitors. d. Surgery + adjuvant chemotherapy e. VEGF Inhibitors f. Radiation therapy: Palliation of metastasis and locally advanced disease. Not standard of care for CRC. Follow-up should occur regularly for approximately 5 years (since likelihood of recurrence is increased within the first 3 years after treatment). Recommendations for follow-up are every 3-5 months for the first 3 years, and every 6 months for the next 2 years. Subsequent follow-up to be determined by doctor and patient. CBI 5 1) Explain how thyrotoxicosis/hyperthyroidism causes weight loss, tachycardia and memory loss. It is important to understand the normal physiologic function of thyroid hormone in order to understand how it causes weight loss, tachycardia, and memory loss. TRH is secreted from the hypothalamus in response to physiologic stress, growth hormone release, consumption of food, etc. TRH causes TSH release from the anterior pituitary. TSH acts at a Gs receptor in the thyroid and stimulates thyroid follicular cells to release T3 and T4 into circulation. T3 and T4 interact with TH receptors in many tissues throughout the body causing the following physiologic outcomes: Increasing activity of the Na/K/ATPase Increasing carbohydrate and fat metabolism Stimulation of protein synthesis Increasing basal metabolic rate Increase in cardiac contractility, heart rate, and CO Bone growth Brain growth In thyrotoxicosis/hyperthyroidism, too much T3 and T4 circulate in the body. The increase in basal metabolic rate that occurs in hyperthyroidism is out of proportion to the amount of calories usually consumed by an individual, resulting in weight loss. A natural effect of thyroid hormone is to increase HR, and too much thyroid hormone would cause tachycardia. Memory loss in hyperthyroidism is due to _____. 2) Discuss the expected results of a thyroid function test in a hyperthyroid patient. Thyroid function tests examine T3, T4, and TSH levels. Variations of these levels in hyperthyroidism are determined by the etiology of disease. Primary hyperthyroidism: High T3, T4. Low TSH. Secondary hyperthyroidism: High T3, T4, TSH. Tertiary hyperthyroidism (Rare): High T3, T4, TSH. 3) Explain why hypokalemia and paralysis can be a complication of thyrotoxicosis. In thyrotoxicosis, T3 and T4 levels are greatly increased. Thyroid hormone has stimulatory effects on the Na/K/ATPase causing increased inward flux of potassium and outward flux of sodium. This causes a relative hypokalemia. Resting membrane potential for a cell is determined by the potassium gradient in a cell, and the relative hypokalemia causes hyperpolarization of electrically active cells. With the drop in resting membrane potential, the cell becomes harder to bring to threshold (a more potent stimulatory signal is required) resulting in paralysis. 4) Discuss the long term treatment for a patient with hypokalemic thyrotoxicosis Avoidance of stimulating factors (carbohydrates, exercise, etc) Thyrotoxic iodine181 Beta blockers 5) Compare the biochemical and physiological consequences of hyperthyroidism and hypothyroidism. Hyperthyroidism: o Biochemical: Induction of Na/K/ATPase o Physiological: Increased BMR (weight loss, feeling of warmth), CHO and fat metabolism, protein synthesis, brain development, bone growth, stimulation of B adrenergic receptors (increased heart rate and contractility). Hypothyroidism: o Biochemical: Decreased activity of Na/K/ATPase o Physiological: Decreased BMR, decreased CHO and fat metabolism, (weight gain, sluggishness, hair loss). CBI 6 CBI #6 Learning Objectives 1) Discuss the 6 documented prognostic indicators for breast cancer and identify the most significant adverse prognostic sign. Major prognostic Indicators: In-situ VS Invasive Lymph node metastasis Distant metastasis * Tumor size Locally advanced disease Inflammatory breast cancer Minor prognostic indicators: Her2/Neu Status ER/PR status Grade Histologic subtype Lymphovascular invasion Proliferative rate DNA content 2) Describe the three main treatment modalities for breast cancer and the goal of treatment for each. 1. Surgery: Remove bulk of tumor cells 2. Radiation: Remove microscopic tumor left behind after surgery 3. Chemotherapy: a. Hormone Therapy: In ER/PR or Her2/NEU + cancers this suppresses growth signals b. Standard multi-agent chemotherapy: Removing any micromets present in the body. 3) Explain the mechanism of action for targeted therapy for breast cancer. Tamoxifen/Raloxifene: Antagonize estrogen receptors on the tumor cells to decrease ligand bindingdecreased transduction of growth signals. Anastrazole: Aromatase inhibitor that decreases in-vivo production of estrogen (estrogen is stimulatory for growth in ER+ breast cancers). Leuprolide: Binds to GnRH receptor in the pituitary causing initial increase in LH/FSH followed by suppression. Decreased LH/FSH results in reversible ovarian suppressiondecreased estrogen production. Her2/NEU: Antibody to the Her2/NEU receptor on the tumor cells that decreases ligand bindingdecreased transduction of growth signals. 4) Relate prognostic indicators to treatment choice. Stage 1: Lumpectomy with or without radiation. Stage 2 and 3: Surgery (lumpectomy or mastectomy with or without lymph node removal), radiation (sometimes), and chemotherapy (plus trastuzumab for HER2+ cancers). Stage 4, metastatic cancer, (i.e. spread to distant sites) is not curable and is managed by various combinations of all treatments from surgery, radiation, chemotherapy and targeted therapies Herceptin-Her2/Neu Tamoxifen, Raloxifene, Leuprolide, Anastrozole-ER/PR + 5) Outline the staging system for breast cancer and correlate the staging system for breast cancer with the prognostic indicators. T0: DCIS/LCIS T1: Tumor <2 cm T2: Tumor <5cm w/nodes or >5cm w/o nodes T3: Tumor >5 cm w/nodes T4: Distant spread 6) Delineate the main side effects of each treatment modality, including the life threatening side effects, along with options for self-care. Surgery: Lymphedema, scarring, limited range of motion, infection Radiation: Radiation burns, damage to normal tissue (both skin and underlying organs), lymph node reactivitylymphedema, cancer Chemotherapy (General): Nausea, vomiting, diarrhea, neurologic changes, hand and foot syndrome, mucositis, skin rash. Other side effects relate to specific drug used. Tamoxifen: Hot flashes, vaginal dryness or atrophy, elevated LDL, thromboembolic events, endometrial cancer. Raloxifene: Hot flashes, vaginal dryness or atrophy, thromboembolic events Anastrazole: Osteoporosis, elevated LDL Trastuzimab/Herceptin: Cardiomyopathy w/arrhythmias, CHF, MI, etc. Self Care: Exercise Healthy diet Support groups Stress relief CPC 4 CPC #4: Carcinoid Tumors and Carcinoid Syndrome Learning Objectives Describe the pathophysiology behind carcinoid syndrome. Carcinoid syndrome is the symptomatic presentation of a carcinoid tumor that has as its primary location the lung or other extra-intestinal site, or has begun in the gut and metastasized to the liver (the hormonal products of these tumors can be metabolized by the liver and lungs, explaining the location specificity). These tumors originate from stem cells in the intestinal crypts and differentiate into endocrine tumors that secrete a variety of peptide and non-peptide hormones (serotonin, tachykinins, kalikrein, prostaglandins, histamine, insulin, gastrin, VIP). The most common symptoms found in carcinoid syndrome are caused by the secretion of serotonin (5-HT) and histamine by the carcinoid tumor. Serotonin increases gastric motility causing hypermotility diarrhea and abdominal cramping, and activates fibroblasts in the heart causing the formation of valvular fibrotic deposits that eventually lead to valvular insufficiency and right sided heart failure. Flushing occurs as a result of histamine release which causes vasodilation of the vasculature in the skin. Describe the effects/action of gastrointestinal peptides secreted by carcinoid tumors. GI peptides secreted by carcinoid tumors: Serotonin: Diarrhea VIP: Diarrhea, hypokalemia, achlorhydria Gastrin: Refractory gastric ulcers (Zollinger-Ellison syndrome) Somatostatin: Steatorrhea, gallstones, DM, hypochlorhydria Explain what causes the flushing response in carcinoid syndrome. Some carcinoid tumors secrete histamine or kalikrein which are vasoactive substances and cause flushing. Characterize the symptoms most commonly associated with carcinoid syndrome. o Diarrhea o Abdominal pain/discomfort o Facial flushing o Telangiectasia o Bronchospasm o Cardiac valvular lesions Describe the laboratory test is used to confirm the diagnosis of carcinoid syndrome. Elevated urine or serum 5-HIAA (byproduct of serotonin metabolism) Elevated serum chromogranins (should mirror the rise in 5-HIAA) Elevated serum serotonin