ED SOAP Note Name: Jane Doe DOB: xx-xx
advertisement
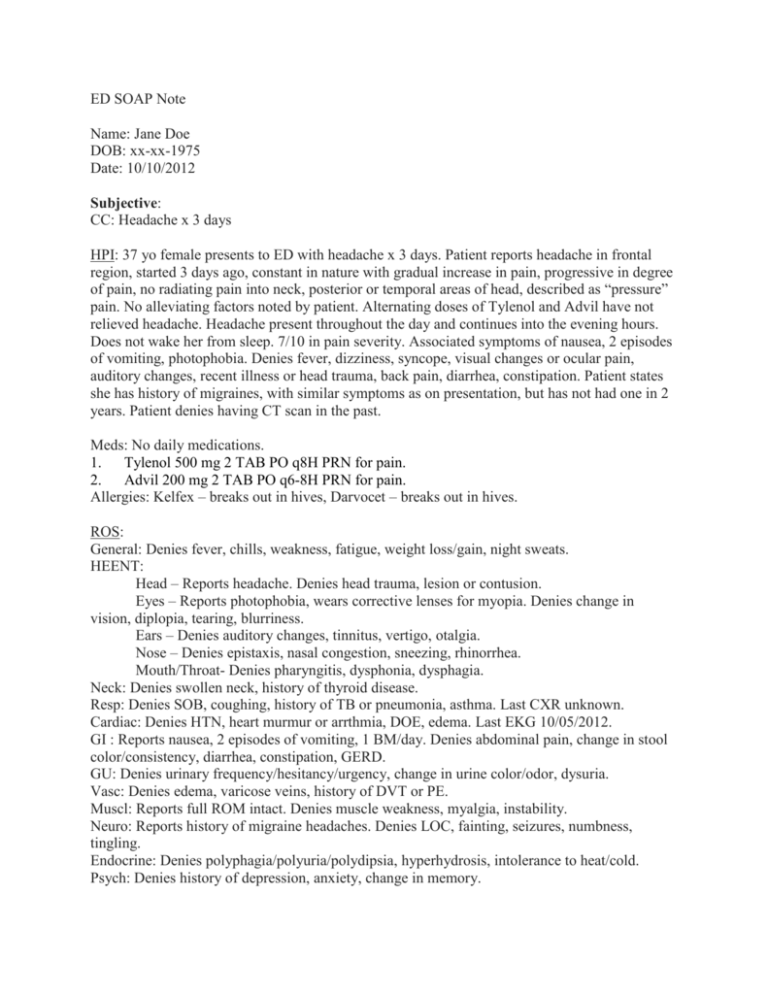
ED SOAP Note Name: Jane Doe DOB: xx-xx-1975 Date: 10/10/2012 Subjective: CC: Headache x 3 days HPI: 37 yo female presents to ED with headache x 3 days. Patient reports headache in frontal region, started 3 days ago, constant in nature with gradual increase in pain, progressive in degree of pain, no radiating pain into neck, posterior or temporal areas of head, described as “pressure” pain. No alleviating factors noted by patient. Alternating doses of Tylenol and Advil have not relieved headache. Headache present throughout the day and continues into the evening hours. Does not wake her from sleep. 7/10 in pain severity. Associated symptoms of nausea, 2 episodes of vomiting, photophobia. Denies fever, dizziness, syncope, visual changes or ocular pain, auditory changes, recent illness or head trauma, back pain, diarrhea, constipation. Patient states she has history of migraines, with similar symptoms as on presentation, but has not had one in 2 years. Patient denies having CT scan in the past. Meds: No daily medications. 1. Tylenol 500 mg 2 TAB PO q8H PRN for pain. 2. Advil 200 mg 2 TAB PO q6-8H PRN for pain. Allergies: Kelfex – breaks out in hives, Darvocet – breaks out in hives. ROS: General: Denies fever, chills, weakness, fatigue, weight loss/gain, night sweats. HEENT: Head – Reports headache. Denies head trauma, lesion or contusion. Eyes – Reports photophobia, wears corrective lenses for myopia. Denies change in vision, diplopia, tearing, blurriness. Ears – Denies auditory changes, tinnitus, vertigo, otalgia. Nose – Denies epistaxis, nasal congestion, sneezing, rhinorrhea. Mouth/Throat- Denies pharyngitis, dysphonia, dysphagia. Neck: Denies swollen neck, history of thyroid disease. Resp: Denies SOB, coughing, history of TB or pneumonia, asthma. Last CXR unknown. Cardiac: Denies HTN, heart murmur or arrthmia, DOE, edema. Last EKG 10/05/2012. GI : Reports nausea, 2 episodes of vomiting, 1 BM/day. Denies abdominal pain, change in stool color/consistency, diarrhea, constipation, GERD. GU: Denies urinary frequency/hesitancy/urgency, change in urine color/odor, dysuria. Vasc: Denies edema, varicose veins, history of DVT or PE. Muscl: Reports full ROM intact. Denies muscle weakness, myalgia, instability. Neuro: Reports history of migraine headaches. Denies LOC, fainting, seizures, numbness, tingling. Endocrine: Denies polyphagia/polyuria/polydipsia, hyperhydrosis, intolerance to heat/cold. Psych: Denies history of depression, anxiety, change in memory. PMH: Migraines, SLE. Denies HTN, HLD, MI, CAD, CVA, seizures, DM. Family Hx: Mother and father still alive. Father has HTN, HLD. No known maternal medical conditions. Denies family history of MI, CAD, CVA, seizures, DM. Social Hx: Smokes ½ ppd. Approximate pack years: ½ ppd x 10 years = 50 years. Denies alcohol or illicit drug use. Objective: Physical Examination General: NAD, well-nourished, well-developed 37 yo female. VS: Ht. 60 in., Wt 175 lbs., BMI 34.2, T 98.6 F, BP 132/70, P 108, RR 16, SaO2 99% on room air HEENT Head: Normocephalic. No signs of head trauma, abrasions, lacerations, contusions. Eyes: White sclera. No conjunctival injection or subconjunctival hemorrhage. PERRLA and EOMI. Direct and consensual ocular reflexes intact. Fundoscopic exam revealed 1:2 cup to disc ratio and 4 arcades noted bilaterally. No retinal edema, hemorrahages, cotton wool patches or AV nicking noted. Fundoscopic exam limited by pupil restriction to light and patient discomfort. Ears: Pearly gray TMs identified bilaterally, mild cerumen present in left ear. No signs of trauma to auricles or external auditory canals bilaterally. Non-tender tragus bilaterally. No discharge in external canal or behind membrane, bulging or ruptured membrane, fluid or hemotympantum noted behind TM B/L. Nose: Patent nares bilaterally, pink turbinates, clear nasal discharge, nasal septum midline. No blood noted. Throat: Uvula midline, equally rises and falls. MMM, non-erythematous or edematous pharynx, no exudates or post nasal drainage noted on inspection. Neck: No carotid bruits identified on auscultation. Supple, non-tender neck. Thyroid equally rises and falls. No asymmetry or nodules noted on palpation. No meningeal signs – negative Brudzinski reflex or Kernig’s signs. Lymph: No palpable lymphadenopathy in pre/post auricular, occipital, anterior/posterior cervical chain, tonsillar, submental, submandibular areas, supraclavicular, infraclavicular or axillary areas. Resp: AP/Lateral chest ratio 2:1, lungs symmetrically rise and fall. No asymmetry or deformities of chest wall, accessory muscle use. Resonant sounds throughout lung fields on percussion B/L, CTA B/L. No wheezes, rhonchi, or rales appreciated on auscultation. Cardiac: RRR, S1 and S2 identified, no M/G/R, S3 or S4 appreciated on auscultation. No obvious lifts or heaves noted on inspection, no palpable lifts, heaves or thrills. PMI not identifiable on inspection. GI: Symmetric, mildly obese abdomen. Active bowel sounds noted x4 quadrants. No abdominal/femoral bruits appreciated on auscultation. Tympanic abdomen with percussion in 4 quadrants. No ascites. Palpable liver 6.5 cm right MCL. No palpable spleen, masses, organomegaly with light/deep palpation. NTND. Extremities: No deformities or edema noted. Gross ROM intact. Vasc: Distal pulses +2/+2 radial, +2/+2 dorsal pedal pulses +2/+2. Skin: Warm, moist skin. No cyanosis or rash. Neuro: AAOx3. Cranial Nerves CN1 – not assessed on exam CN2 – Visual acuity 20/20 bilaterally with corrective lenses. CN3,4,6 – EOMI, PEERLA. CN5 – sharp vs. dull distinction intact in ophthalmic, maxillary and mandibular regions. CN7 – Patient able to smile, frown, keep eyelids closed against resistance. CN8- Hearing grossly intact, assessed through appropriate responses in conversation. CN9- Swallowing intact CN10- Uvula midline, equally rises and falls. No lateral deviation. CN11- Shoulder shrug intact CN12- Tongue midline, moves against resistance. No lateral deviation. Sensory - Dermatomes randomly sampled from fingertips to shoulders and facial area intact to light touch sensation B/L. Sharp vs. dull distinction intact from fingertips to shoulders and facial area. Vibratory sensation in UE/LEs intact. Two point discrimination, graphesthesia, stereognosis. Motor - Voluntary movement intact on inspection, symmetrical muscle mass in upper/lower extremities. No cogwheeling or stiffness with passive ROM in upper/lower extremities. Strength (AROM against resistance): Muscle group Left Biceps +5 Triceps +5 Forearm flexors +5 Forearm extensors +5 Grip +5 Shoulder add/abductors +5 Quads +5 Hamstrings +5 EHL +5 Plantar flexors +5 LE add/abductors +5 Right +5 +5 +5 +5 +5 +5 +5 +5 +5 +5 +5 Reflexes: Reflexes Triceps Biceps Brachioradialis Patellar Left +2 +2 +2 +1 Right +2 +2 +2 +2 Achilles +2 +1 Cerebellar – Rapid tongue movements intact, finger-to-nose intact B/L, heel slides intact B/L, heel to toe walking intact. No loss of balance when standing in Rhomberg position. Negative pronator drift. ED Course Order: 1. Labs – a. CBC b. CMP c. UA d. Values within range on CBC and CMP. No glucose, ketones, RBCs found in urine. 2. Head CT a. Report – no acute intracranial process. 3. Fluids/Medications to be given: a. Saline lock. b. IV NSS 125 mg/hr. c. 10 mg Reglan IV immediately in ED at 1335 i. Side effects of Reglan – drowsiness, restlessness, fatigue, extrapyrimidal effects, dizziness. d. 30 mg Toradol IV immediately in ED at 1335 i. Side effects of Toradol – headache, abdominal pain, nausea, dyspepsia. ii. Confirmed with patient that she had no history of ulcers which could be made worse with Toradol. e. 25 mg Benadryl PO immediately in ED at 1335 i. Side effects of Benadryl - allergic reaction, drowsiness, dizziness, headache, dry mucus membranes. f. Addendum to orders: 1 mg Diluadid IV i. Patient did not have pain relief with Reglan, Benadryl and Toradol. ii. Dilaudid given for pain relief. 1. Side effects of Dilaudid – nausea, vomiting, constipation, dizziness, drowsiness. 2. Patient educated on risk of rebound headache after Dilaudid wears off. Assessment: Diagnosis: Migraine headache DDx: Migraine headache, tension headache, sinusitis, subarachnoid hemorrhage, epidural hematoma 1. Migraine headache – Her PMH supports the possibility of a recurrence of migraine headaches. Migraine headaches present with throbbing unilateral pain, nausea, vomiting, photosensitivity. Patient presented with many of these symptoms including nausea, vomiting and photosensitivity as well as a history of similar migraine pain in the past. These symptoms support the diagnosis of migraine headache. 2. Tension headache – This type of headache are associated with emotional stressors. On exam, tenderness may be noted over frontal region. Patient did not note any tenderness on exam, nor did she express any recent stressor in her life which would have caused the sudden increase in headache. 3. Sinusitis – Patients usually present with frontal headache, fever, nasal congestion, coughing and other signs of acute inflammation and irritation in facial region. The patient did not have any nasal congestion or post-nasal drip, cough or tenderness of frontal or maxillary regions on physical exam when noting sensation. Because there was no congestion noted on physical exam or tenderness, sinusitis was not the most probable diagnosis based on clinical findings. 4. Subarachnoid hemorrhage – This condition presents with head pain referred to as a “thunderclap” headache which comes on suddenly as the “worst headache.” On exam, there may be nuchal rigidity noted. The patient stated that her headache had insidious onset and gradually worsened over last 3 days. No nuchal rigidity was noted on physical exam, patient was able to shrug shoulders and turn head bilaterally without discomfort. Although the CT exam was negative for brain bleeding, subarachnoid hemorrhage could still be present. The confirmative test would be lumbar puncture. This was deferred at this time because the patient was not presenting with the clinical symptoms of thunderclap headache or nuchal rigidity. It symptoms worsen, lumbar puncture would be performed. 5. Epidural hematoma – this diagnosis usually presents after head trauma with LOC. There also may be associated symptoms of nausea, vomiting, headache and pupil dilation. Patient was nauseated and had been vomiting, but she did not have any recent head trauma and her pupils were equal and reactive to light. Because her clinical presentation did not have either head trauma or pupil changes, epidural hematoma was low on the differential. Plan: 1. 2. 3. Medications a. Patient given following prescriptions at discharge from ED: i. Zofran 4 mg PO QID PRN for nausea 1. Side effects- headache, fatigue, constipation, diarrhea, dizziness. ii. Toradol 10 mg PO Q4-6H PRN pain 1. Side effects – nausea, abdominal pain, dizziness, headache, constipation, flatulence. Patient education a. Patient recommended to continue alternating Tylenol and Advil PRN along with Toradol until follow up with family physician. b. Patient to avoid bright lights, loud sounds until headache resolves. c. Smoking cessation – patient educated on smoking cessation. Patient educated on the different modalities to use to stop smoking: Nicotine patches, nicotine gym, Chantix tablets, electric cigarettes, “cold turkey” method. Follow up a. Patient advised to contact family physician, Dr. Kreider, tomorrow to schedule appointment to further address migraine headaches. b. Patient to return to ED if headache worsens, nausea and vomiting return or if additional symptoms occur. Alyson Wattai, PA-S