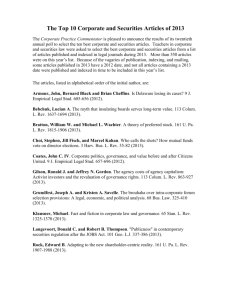
ClinicalDBBlank
advertisement

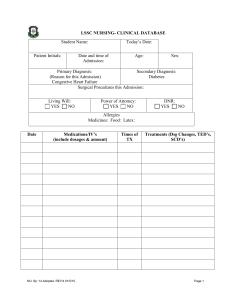
LSSC NURSING- CLINICAL DATABASE Today’s Date: Student Name: Patient Initials: Date and Time of Admission: Age: Primary Diagnosis: Sex: Secondary Diagnosis: Surgical Procedures this Admission: Living Will: YES NO Power of Attorney: YES NO DNR: YES NO Allergies Medicines: Food: Latex: Date Medications/IV’s (include dose, route, frequency) NU: Sp ‘14 Adopted. REV’d 01/5/15. Times Of TX Treatments (Dsg Changes, TED’s, SCD’s) Page 1 Chief Complaint on Admission: Past Medical History: Past Surgical History: Home Medications: Continued During Hospital Stay? Social History: Family History: Client Assessment Vital Signs: AM BP Pulse Respirations Temp. PM Activity Ordered: Diet: Intake: 24 hour mL Intake: POIV- mL mL NU: Sp ‘14 Adopted. REV’d 01/5/15. % Eaten Output: Output: O2 Sats. Pain %@ 0/10 RA or L/min %@ 0/10 RA or L/min Telemetry: YES NO Rhythm: mL mL Page 2 Ht/Wt: Subjective Objective HEENT: Head: HEENT: Head: Eyes: Eyes: Ears: Ears: Nose: . Nose: Tongue: Throat: . Tongue: Throat: Cardiovascular: Cardiovascular: Rate: Apical Radial Rhythm: Regular Irregular Pulse Quality/Strength: (0, 1+, 2+, 3+) Right Left Brachial Femoral Popliteal Pedal Post-Tibial Carotids Carotid Bruit: Yes___No___R____L____ S-1 S-2 Murmurs: Capillary Refill: R seconds L seconds PMI Location: Peripheral-Vascular: Legs: Color R (Pink, Pale, Cyanotic) L Temperature: R (Cool, Warm, Hot) L Trace: R R L L (1+, 2+, 3+, 4+) Present Absent Present Absent Pedal Edema Pitting Edema Leg Edema above ankle (Describe locations, amount, bilateral/unilateral): Respiratory: NU: Sp ‘14 Adopted. REV’d 01/5/15. Lesions: R L Describe: Respiratory: Rate: /min Ease/Effort: Non-labored Labored Depth: Shallow Normal Deep Character: Quiet/Silent Noisy Chest Expansion: Symmetrical Asymmetrical Intercostals: Bulging Retraction Normal Breath Sounds: Clear Wheezes Ronchi Crackles Anterior: Posterior: R-Lateral: L-Lateral: Bilaterally Page 3 Cough: None Describe: N/A Non-Productive Productive Odor: Color: Gastrointestinal: . Genitourinary: . Musculoskeletal: Integumentary: Neurological: Psychosocial (Erikson): NU: Sp ‘14 Adopted. REV’d 01/5/15. Gastrointestinal: Oral Mucosa: Pink Pale Dry Moist Intact Lesions Dentures: None Upper Lower Partial Plate Teeth Condition: None Abdominal Contour: Flat Rounded Scaphoid Protuberant Bowel Sounds: Normoactive Hypoactive Hyperactive Location: RLQ RUQ LLQ LUQ Abdominal Aortic Bruit: Present Not Present Illiacs Bruit: (R) Present Not Present (L) Present Not Present Renal Bruit: (R) Present Not Present (L) Present Not Present Abdomen: Soft Firm Tense Distended Tender Location: Presence of surgical incision: Umbilicus: Genitourinary: Urine Output: YES NO Color: Amber Light Dark Amber Bloody Blood Tinged Clear Sediment Odor: YES NO Describe: Musculoskeletal: Movement/Gait: Erect Steady Smooth and Coordinated Weak Flacid Strength: (5+, 4+. 3+, 2+, 1+, 0) = Able to turn self Bears own weight ROM: Full Limited Describe: Assistive Devices: None Walker Cane Wheelchair Crutches Integumentary: Color: Pink Pale Cyanotic Jaundiced Temperature: Cold Cool Warm Hot Condition: Dry Moist Clammy Diaphoretic Integrity: Intact Rash Wound Describe: Turgor: Immediate Remains Peaked Taut Neurological: Response: Alert Lethargic Stuporous Comatose Orientation: Person Place Time Situation PERRLA: Right Left Hand Grips: Weak Strong Bilaterally Mood: Appropriate Not Appropriate Attitude/Behavior: Cooperative Hostile Combative Withdrawn Psychosocial (Erikson): Page 4 Lab Values: Na HGB BUN Glucose PLT WBC HCT CCC CCC CCC CCX CC Cl \ K HCO CR jhjhjhjkj 1. Lab Values Interpretation. 2. Prioritize Actual problems (Problem + related to AEB). 3. List Interventions that you provided this shift for the above problems. 4. List teaching given to this patient (written, video, demonstration). 5. List diagnostic test. Critical Thinking Assignment: Answer the questions below based on your above assessment and data collection from your patient. 1. What are you alert for today with your patient? 2. What are the important assessments to make? 3. What complications may occur? What could go wrong? 4. What interventions will prevent complications? NU: Sp ‘14 Adopted. REV’d 01/5/15. Page 5