Vocal Cord Dysfunction Vocal Cord Dysfunction, or VCD causes
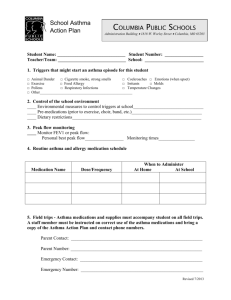
advertisement

Vocal Cord Dysfunction Vocal Cord Dysfunction, or VCD causes asthma-like symptoms because of an abnormal closing of the vocal cords. VCD can cause difficulty breathing and even wheezing. Based on these symptoms, many people with VCD may be diagnosed with asthma and treated with asthma medications, including oral steroids. Since VCD is not asthma, the symptoms do not improve with this treatment. When VCD is not treated properly, it may lead to frequent emergency room visits and hospitalizations. To complicate the situation, some people have a combination of asthma and Vocal Cord Dysfunction. Vocal Cord Disorder May Mimic Asthma Some people whose asthma symptoms aren’t helped by medicine may not have asthma at all. Instead, a disorder of the vocal cords may be to blame. The symptoms of vocal cord dysfunction, or VCD are similar to those of asthma; wheezing, coughing, and shortness of breath. In a study of 95 people who did not respond to asthma treatment, researchers found that 53 had both VCD and asthma and 42 had VCD alone. The people with only VCD had been misdiagnosed with asthma and many of them had been on medication for the treatment of severe asthma. What Happens with VCD? To understand VCD, it is helpful to know how the vocal cords function normally. When you breathe in, or inhale, the vocal cords open, allowing air to flow into your windpipe (trachea) and reach your lungs. However, with Vocal Cord Dysfunction, the vocal cords close together, or constrict, when you inhale. This leaves only a small opening for air to flow into your windpipe. How is VCD diagnosed? Making a diagnosis of VCD can be difficult. If your physician or healthcare provider suspects VCD you will be asked many questions about your symptoms. Common symptoms include a chronic cough, shortness or breath, difficulty breathing, chest tightness, throat tightness, “difficulty getting air in”, hoarseness and wheezing. Breathing tests may be normal and not show signs of asthma. A specific breathing test called a flow volume loop can be helpful in showing VCD, especially on the “breathing in” or inspiratory part of the loop. This is only helpful if it is done while you are having symptoms. A procedure called a laryngoscopy is the most important test in making a diagnosis of VCD. This procedure is performed by a specialized physician. Using a flexible tube, the physician can see how your vocal cords open and close. A laryngoscopy should be done when you are having symptoms because abnormal vocal cord movements do not occur all the time. Other tests may be 1 done to trigger symptoms so that your physician can observe your vocal cords when you are having symptoms. It is important to know that people with VCD cannot produce symptoms voluntarily. Vocal Cords OPEN CLOSED What Can Trigger VCD Symptoms? Possible triggers of VCD are often similar to asthma triggers. Triggers may include upper respiratory infections, fumes, odors, cigarette smoke, singing, emotional upset, postnasal drip, and exercise. Sometimes the trigger is not known. How is VCD treated? Once you are diagnosed with VCD, you can begin a specific treatment program. If VCD is your only condition, your asthma medications may be stopped. If you have a combination of asthma and VCD, asthma medications may be continued, but may often be decreased. Speech therapy is a very important part of the treatment of VCD. Special exercises increase your awareness of abdominal breathing and relax your throat muscles. This enables you to have more control over your throat. You will learn to practice these exercises while you are symptom-free in order to effectively use the exercises during VCD episodes. These exercises help overcome the abnormal vocal cord movements and improve airflow into your lungs. Another important part of treatment is supportive counseling. Counseling can help you adjust to a new diagnosis and a new treatment program. Counseling can also help you identify and deal positively with stress, which may be an underlying factor in VCD. Most people with VCD find counseling to be very beneficial. 2 Vocal Cord Disorder May Mimic Asthma Some people whose asthma symptoms aren’t helped by medicine may not have asthma at all. Instead, a disorder of the vocal cords may be to blame. The symptoms of vocal cord dysfunction, or VCD are similar to those of asthma; wheezing, coughing, and shortness of breath. In a study of 95 people who did not respond to asthma treatment, researchers found that 53 had both VCD and asthma and 42 had VCD alone. The people with only VCD had been misdiagnosed with asthma and many of them had been on medication for the treatment of severe asthma. Vocal cord dysfunction can be detected with a device called a laryngoscope, which allows a doctor to see the movement of the vocal cords. The vocal cords consist of two thin bands of tissue that stretch across the larynx, or voice box. Vocal cord dysfunction occurs when the vocal cords close up, limiting airflow. Attacks of VCD can be triggered by cigarette smoke or exercise; factors that can also trigger asthma. Doctors can treat VCD by teaching people how to relax the throat muscles, a technique called relaxed throat breathing. Other treatments include biofeedback and surgery. 3 Breathing Techniques Diaphragmatic Breathing The diaphragm is a major muscle used in breathing and is located at the level of the lowest two ribs. At rest, the diaphragm muscle is bell shaped, but during inspiration it lowers and flattens out. Optimizing the use of the diaphragm is beneficial because it pulls air into the lower lobes of the lungs where more gas exchange takes place. Not only is the diaphragm the most efficient of all respiratory muscles, but using it tends to be very relaxing and calming. Along with our diaphragm, we use intercostal muscles and abdominal muscles in the work of breathing. The intercostals, or muscles between the ribs, pull to lift the rib cage up and out. This causes the lungs to open in all directions and air can be pulled down the airways. To exhales, the muscles that have been pulling relax and air is forced out. Pursed Lip Breathing: The resistance created by breathing out through pursed lips Slows down the breathing rate Creates a back pressure which helps the lungs’ airways to remain open. Breathe in through your nose Purse lips slightly as if to whistle Breathe out slowly through pursed lips Do not force the air out 4 Relaxed Throat Breath with Abdominal Support A. Relaxed Throat Breath 1. Inhale with relaxed throat Tongue on floor of mouth Lips gently closed Jaw gently released 2. Exhale on gentle “S” with abdominal support or “SH” or “F” in public Hand on abdomen (above the belt or below the belt or both) Inhale into abdomen- abdomen goes out Exhale from abdomen-abdomen comes in As you pull in abdomen, exhale on gentle “S” 3. If more comfortable, use gentle sip for inhale, gentle blow for exhale, feeling air on the lips. 4. Do 10 of these breaths 10 x per day In the morning At noon Before bedtime Before medications As it fits into your schedule B. Use this breathing pattern at any sign of tightness or stridor If this occurs during activity, stop activity, do exercises until it stops and then resume activity gradually. C. Remember: 1. Tightness or stridor can be released by breathing exercises 2. Do exercises easily Don’t push or pull on shoulders, chest or neck Concentrate on letting air in and out Go into new activities and sports gradually using the breath as a basic part of your activity. 5