Counseling & Designer Babies Instructions 2014
advertisement
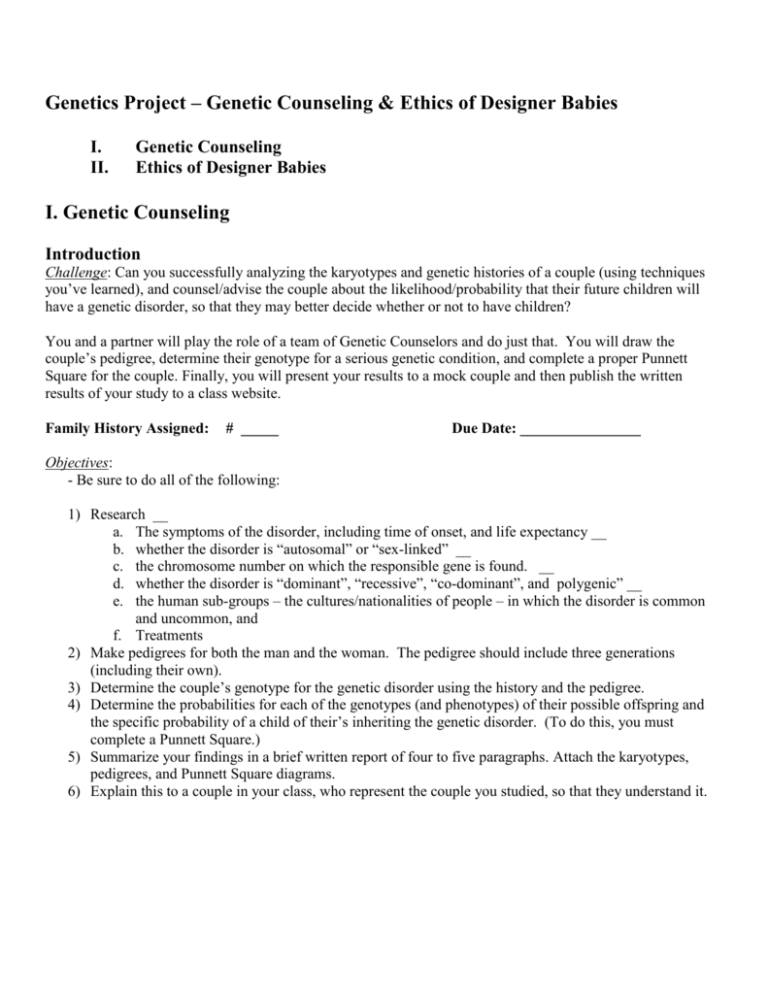
Genetics Project – Genetic Counseling & Ethics of Designer Babies I. II. Genetic Counseling Ethics of Designer Babies I. Genetic Counseling Introduction Challenge: Can you successfully analyzing the karyotypes and genetic histories of a couple (using techniques you’ve learned), and counsel/advise the couple about the likelihood/probability that their future children will have a genetic disorder, so that they may better decide whether or not to have children? You and a partner will play the role of a team of Genetic Counselors and do just that. You will draw the couple’s pedigree, determine their genotype for a serious genetic condition, and complete a proper Punnett Square for the couple. Finally, you will present your results to a mock couple and then publish the written results of your study to a class website. Family History Assigned: # _____ Due Date: ________________ Objectives: - Be sure to do all of the following: 1) Research __ a. The symptoms of the disorder, including time of onset, and life expectancy __ b. whether the disorder is “autosomal” or “sex-linked” __ c. the chromosome number on which the responsible gene is found. __ d. whether the disorder is “dominant”, “recessive”, “co-dominant”, and polygenic” __ e. the human sub-groups – the cultures/nationalities of people – in which the disorder is common and uncommon, and f. Treatments 2) Make pedigrees for both the man and the woman. The pedigree should include three generations (including their own). 3) Determine the couple’s genotype for the genetic disorder using the history and the pedigree. 4) Determine the probabilities for each of the genotypes (and phenotypes) of their possible offspring and the specific probability of a child of their’s inheriting the genetic disorder. (To do this, you must complete a Punnett Square.) 5) Summarize your findings in a brief written report of four to five paragraphs. Attach the karyotypes, pedigrees, and Punnett Square diagrams. 6) Explain this to a couple in your class, who represent the couple you studied, so that they understand it. II. Ethics of Genetic “Designer Babies” Introduction Challenge: Is it “right” for humans to have the ability to eliminate genetic mutations and to choose the gender – and possibly other traits – of their unborn children? Is it right to make changes in an individual’s genes – the genetic code inherited via sexually reproduction and passed down for thousands of years? Will this disrupt natural balance, introduce new problems, and possibly even create monsters? Take an ethical position and argue it using what you learn, below, and your feelings. Background: Because of advances in genetic biotechnology starting with the Human Genome Project, geneticists are 1., studying certain therapies/treatments for genetic disorders and, 2., have moved genes across species to make “transgenic” organisms known as Genetically Modified Organisms (GMOs) – especially in crops in order to increase farming production. Now, 3., two genetic technologies – PGD and IVF – allow prospective parents, with the assistance of medical doctors, to determine the gender of their unborn children, as well as to choose whether to allow certain genetic disorders, and possibly to select other – preferred – traits of their unborn children, such as eye and hair color. This phenomenon is called “Designer Babies”. You will discover the Human Genome Project and read and view one or more sources about each of these developments in order to share your opinion on each in a social media format. You will be required to, 1., post your understanding and, 2., your opinion about these three advances, and then, 3., engage in discussion with at least three fellow classmates about the ethics of Designer Babies. Objectives: - Be sure to do all of the following: 7) Review the provided web, text, and video resources in order to understand a. The Human Genome Project & Gene Therapy i. Doc: “What is the Human Genome Project (HBP)?” ii. YouTube: “BBC iScience Human Genome” (Lammas Science; 4:33) iii. Google: “BBC - GCSE Bitesize: The Human Genome Project” iv. Doc: What is Genetic Engineering? v. Doc: What is Gene Therapy? vi. YouTube: “Gene Therapy” (BioethicsBytes; 5:00) vii. YouTube: “How Does Gene Therapy Work?” (DNews 2:28) b. GMO’s – genetically modified organisms, and the adjective “transgenic” i. YouTube: What is genetically modified food? – Instant Egghead#45” (Scientific American; 3:13) ii. YouTube: GMOs (Healthcare Triage; 5:34) iii. Doc: “Genetically Modified Foods” iv. Doc: “What are GMOs?” c. Designer Babies i. PGD (Pre-implantation Genetic Diagnosis) & IVF (In-vitro Fertilization) ii. http://www.today.com/id/26184891/vp/29478705#29478705 iii. http://www.cbsnews.com/news/designer-babies-ethical/ 8) Post a web-based explanation of each item in “#7” (above) - Mr. Z will provide the website. 9) Post 2-3 paragraphs about your opinion in a web-based, class discussion of the ethics of Designer Babies a. Respond to the posts of at least three fellow classmates. Family Histories for “Part I: Genetic Counseling” 1) Cystic Fibrosis Background & Family Histories Cystic fibrosis (CF), also known as mucoviscidosis, is an autosomal, recessive genetic disorder most common in Central and Northern European people. It is rare in Asia and the Middle East. As CF is an autosomal recessive disorder, those with a single [healthy gene] are carriers and otherwise mostly normal. CF affects mostly the lungs but also the pancreas, liver, kidneys and intestine.[1][2] Long-term issues include difficulty breathing and coughing up sputum [phlem] as a result of frequent lung infections. Other symptoms include sinus infections, poor growth, … clubbing of the finger and toes, and infertility in males among others. The main signs and symptoms of cystic fibrosis are salty-tasting skin,[8] poor growth, and poor weight gain despite normal food intake,[9] accumulation of thick, sticky mucus,[10] frequent chest infections, and coughing or shortness of breath.[ Symptoms often appear in infancy and childhood…. As the children grow, they must exercise to release mucus in the alveoli. Cells in the person have a mutated protein that leads to abnormally viscous [thick] mucus production. As CF is an autosomal recessive disorder, hose with a single working copy are carriers and otherwise mostly normal. There is no cure for cystic fibrosis.[3] Lung infections are treated with antibiotics [that] may be given intravenously, inhaled, or by mouth. Sometimes the antibiotic azithromycin is used long term. Lung transplantation may be an option if lung function continues to worsen. Pancreatic enzyme replacement [by pill] and … vitamin supplementation are important, especially in the young. The average life expectancy is between 37 and 50 years in the developed world.[6] Lung problems are responsible for death in 80% of people.[1] CF affects about one out of every three thousand newborns. [1] About one in twenty five are carriers.[3] It is least common in Africans and Asians.[1] (Wikipedia) Woman’s History Woman carries one gene for cystic fibrosis. Her mother’s genotype is homozygous dominant/healthy for this trait. Her father had a brother (who died at age 13 of cystic fibrosis) and a sister who carries the gene but never had children. Father carries the gene. Her one brother does not carry the gene. Her mother’s parents were both from Kenya and lived to the ages of 86 and 88. Cystic fibrosis never existed in their family. Her father’s family came from Norway, in Northern Europe. Make the Pedigree. What must the genotype be of this woman’s paternal grandparents – her father’s parents? Man’s History The man is also a carrier of cystic fibrosis. His father’s genotype is homozygous dominant/healthy for this trait. His mother is a carrier but was an only child and had no siblings. His maternal grandmother, who carried the gene, had a sister who died at the age of two and a brother who died at the age of five. His maternal grandfather was homozygous dominant. His paternal grandparents were both homozygous dominant. 2) Huntington’s Disease (HD): (autosomal dominant mutation) There is no cure for HD, and full-time care is required in the later stages of the disease. Existing pharmaceutical and non-drug treatments can relieve many of its symptoms. It is much more common in people of Western European descent than in those of Asian or African ancestry. Huntington's disease (HD) is a neurodegenerative genetic disorder with symptoms that affects muscle coordination and leads to mental decline and behavioral symptoms.[1] [These] symptoms of the disease can vary between individuals and affected members of the same family, but usually progress predictably. The earliest symptoms are often subtle problems with mood or cognition. A general lack of coordination and an unsteady gait often follows. As the disease advances, uncoordinated, jerky body movements become more apparent, along with a decline in mental abilities and behavioral symptoms.[1] Physical abilities gradually worsen until coordinated movement becomes difficult. Mental abilities generally decline into dementia. Complications such as pneumonia, heart disease, and physical injury from falls reduce life expectancy to around twenty years from the point at which symptoms begin. Physical symptoms can begin at any age from infancy to old age, but usually begin between 35 and 44 years of age. The disease may develop earlier in life in each successive generation. About 6% of cases start before the age of 21 years…. (Wikipedia) Woman’s History Woman has one Huntington’s disease gene. Her father developed the disease in his 50’s and is still alive. Her father’s father, who was from Germany, died at the age of 47, when her father was just 20. Her father had one brother who had no Huntington’s genes. Her mother, also from Germany, has no history of Huntington’s disease in her family. Her one sister, fortunately, does not carry the gene. Man’s History The man is also a carrier of cystic fibrosis. His father’s genotype is homozygous dominant/healthy for this trait. His mother is a carrier but was an only child and had no siblings. His maternal grandmother, who carried the gene, had a sister who died at the age of two and a brother who died at the age of five. His maternal grandfather was homozygous dominant. His paternal grandparents were both homozygous dominant. 3) Melanoma Family History Melanoma is an autosomal dominant type of skin cancer which forms from melanocytes (pigment-containing cells in the skin).[2] Melanomas are usually caused by DNA damage resulting from exposure to ultraviolet (UV) light from the sun. In women, the most common site of occurrence is on the legs, and melanomas in men are most common on the back.[3] It is particularly common among Caucasians, especially northern Europeans and northwestern Europeans, living in sunny climates. There are higher rates in Oceania, North America, Europe, Southern Africa, and Latin America.[4]This geographic pattern [is due to] the primary cause, ultraviolet light – sun – exposure[5] in conjunction with the amount of skin pigmentation in the population.[6][7] Melanocytes produce the dark pigment, melanin, which is responsible for the color of skin. These cells predominantly occur in skin, but are also found in other parts of the body, including the [intestines] and the eye. Melanoma can originate in any part of the body that contains melanocytes. (Wikipedia) The treatment includes surgical removal of the tumor. If melanoma is found early, while it is still small and thin, and if it is completely removed, then the chance of cure is high. The likelihood that the melanoma will come back or spread depends on how deeply it has gone into the layers of the skin. For melanomas that come back or spread, treatments include chemo- and immunotherapy, or radiation therapy. Five year survival rates in the United States are on average 91%.[8] Melanoma is less common than other skin cancers. However, it is much more dangerous if it is not found in the early stages. It causes the majority (75%) of deaths related to skin cancer.[9] Globally, in 2012, melanoma occurred in 232,000 people and resulted in 55,000 deaths.[10] Australia and New Zealand have the highest rates of melanoma in the world.[10] It has become more common in the last 20 years in areas that are mostly Caucasian.[10] (Wikipedia) Melanoma accounts for six percent of cancer cases in teens 15-19 years old and is the most common form of cancer for young adults 25-29 years old and the second most common form of cancer for young people 15-29 years old.17 On average, a person’s risk for melanoma doubles if he or she has had more than five sunburns.19 Half of all adults aged 18-29 report at least one sunburn in the past 12 months.47 Sustaining 5 or more sunburns in youth increases lifetime melanoma risk by 80 percent.20 (http://www.skincancer.org/skin-cancer-information/skin-cancer-facts) A number of rare mutations, which often run in families, are known to greatly increase one's susceptibility to melanoma. Several different genes have been identified as increasing the risk of developing melanoma. Some rare genes have a relatively high risk of causing melanoma; some more common genes, such as a gene called MC1R that causes red hair, have a relatively lower elevated risk. Genetic testing can be used to determine whether a person has one of the currently known mutations. One class of mutations affects the gene CDKN2A. An alternative reading frame mutation in this gene leads to the destabilization of p53, a transcription factor involved in apoptosis and in fifty percent of human cancers. Another mutation in the same gene results in a nonfunctional inhibitor of CDK4, a cyclin-dependent kinase that promotes cell division. Mutations that cause the skin condition xeroderma pigmentosum (XP) also seriously predispose one to melanoma. Scattered throughout the genome, these mutations reduce a cell's ability to repair DNA. Other mutations confer lower risk, but are more prevalent in the population. People with mutations in the MC1R gene, for example, are two to four times more likely to develop melanoma than those with two wild-type (typical unaffected type) copies of the gene. MC1R mutations are very common; in fact, all people with red hair have a mutated copy of the gene. Mutation of the MDM2 SNP309 gene is associated with increased risk of melanoma in younger women. (Wikipedia) Woman’s History This 29 year old woman has red hair and is of Irish descent. She has not had skin cancer but her eldest brother (of two) has, at the age of 40. Her 60 year old, Welsh born father had surgery to remove a melanoma and so has the 58 year old sister of her native (red-haired) Irish mother. Her paternal grand father and maternal grandmother both passed away from cancer. Both of her grandmothers survived past 90 with no signs of cancer. Man’s History This man and his four girls and two brothers, of central African heritage, have no history of skin cancer between them. As well, neither his mother’s and her two sisters, or her father and his one sister had skin cancer, either. Neither grandparent had skin cancer, although both men and one of the women passed away at early ages due to illness and violence in the region of their births. 4) Sickle-Cell Anemia (SCA) Sickle-Cell anemia is a slightly co-dominant, autosomal, recessive disorder striking approximately 1 of every 1,875 US African Americans. It is rare in other peoples. It is a blood disorder characterized by an abnormality in the oxygen-carrying haemoglobin molecule in red blood cells. This leads to cells having an abnormal, rigid, sickle-like shape. Sickle-cell disease is associated with a number of acute [severe] and chronic [long-term] health problems, such as severe infections, attacks of severe pain ("sickle-cell crisis"), and stroke, and there is an increased risk of death. Several subtypes exist, depending on the exact mutation in each haemoglobin gene. A person with a single abnormal gene copy does not experience symptoms and is said to have sickle-cell trait. The complications of sickle-cell disease can be prevented to a large extent with vaccination, preventative antibiotics, blood transfusion, and the drug hydroxyurea/hydroxycarbamide. Almost 300,000 children are born with a form of sickle-cell disease every year, mostly in sub-Saharan Africa, but also in other countries such as the West Indies and in people of African origin elsewhere in the world. The condition was first described in the medical literature by the American physician James B. Herrick in 1910, and in the 1940s and 1950s contributions by Nobel prize-winner Linus Pauling made it the first disease [whose] exact genetic and molecular defect was [identified]. (Wikipedia) Woman’s History This woman carries one gene for SCA and one each of her two sisters and two brothers, all of west African heritage, are homozygous recessive for sickle cell anemia. Her mother had no apparent symptoms, but one of her mother’s two sisters suffered and died young; her father also carried one gene as did his one. Neither of her grandparents suffered from the condition, but her grandmother’s brother did as did one of her grandfather’s two brothers. Man’s History The man, an only child, is not aware whether he has a gene for SCA. His father was sometimes strangely ill, finding it difficult to participate in athletics. His father’s father had a brother with full SCA. His mother, also an only child, has been identified with SCA. His maternal grandmother, who carried the gene, had a sister who died young and a brother who suffered much and died in middle age. His maternal grandfather was heterozygous. His paternal grandparents were both homozygous dominant. 5) Down Syndrome (Trisomy 21) Down syndrome, also known as trisomy 21, is a genetic disorder caused by the presence of all or part of a third copy of chromosome 21.[1]It is typically associated with physical growth delays, characteristic facial features, and mild to moderate intellectual disability.[2] People with Down syndrome may have some or all of these physical characteristics: a small chin, slanted eyes, poor muscle tone, a flat nasal bridge, a single crease of the palm, and a protruding tongue due to a small mouth and large tongue.[19] These airway changes lead to sleep apnea in around half of those with Down syndrome.[11] Other common features include: a flat and wide face,[19] a short neck, excessive joint flexibility, extra space between big toe and second toe, abnormal patterns on the fingertips and short fingers. Growth in height is slower, resulting in adults who tend to have short stature—the average height for men is 154 cm (5 ft 1 in) and for women is 142 cm (4 ft 8 in). The average IQ of a young adult with Down syndrome is 50, equivalent to the mental age of an 8- or 9-year-old child, but this varies widely.[3] The parents of the affected individual are typically genetically normal.[14] Those who have one child with Down syndrome have about a 1% risk of having a second child with the syndrome, if both parents are found to have normal karyotypes.[42] The extra chromosome content can arise through several different ways. The most common cause (about 92–95% of cases) is a complete extra copy of chromosome 21, resulting in trisomy 21. Failure of the 21st chromosome to separate happens during egg or sperm development.[43]As a result, a sperm or egg cell is produced with an extra copy of chromosome 21; this cell thus has 24 chromosomes. When combined with a normal cell from the other parent, the baby has 47 chromosomes, with three copies of chromosome 21.[1][43] About 88% of cases of trisomy 21 result from nonseparation of the chromosomes in the mother. Education and proper care have been shown to improve quality of life.[6] Some children with Down syndrome are educated in typical school classes, while others require more specialized education.[7] Some individuals with Down syndrome graduate from high school and a few attend post-secondary education.[8] In adulthood, about 20% in the United States do paid work in some capacity[9] with many requiring a sheltered work environment.[7] Support in financial and legal matters is often needed.[10] Life expectancy is around 50 to 60 years in the developed world with proper health care.[3][10] Down syndrome is the most common chromosome abnormality in humans,[3] occurring in about one out every 1000 babies born each year.[2] It is named after John Langdon Down, the British doctor who fully described the syndrome in 1866.[11] The genetic cause of Down syndrome—an extra copy of chromosome 21—was identified by French researchers in 1959.[11] (Wikipedia) Woman’s History This healthy woman is married to her male partner. Together, they have a son with Down Syndrome. The woman has a healthy sister and brother and both her father and her mother were healthy. Her father passed a way in a work accident when he was 47. Her mother had one healthy brother. Her father had two brothers, both of whom were healthy. Man’s History This healthy man, who is married to this woman, has two healthy sisters. Both of his parents were healthy as well. Unfortunately, both of his parents are both deceased as the result of an automobile accident. His father has a surviving healthy sister and his mother has a surviving and healthy brother and sister. Karyotype – Couple # _5_ (First Child) Karyotype – Couple # __ Parent Parent Sample Pedigree