RATS ARE NOT PEOPLE AND PEOPLE ARE NOT HORSES
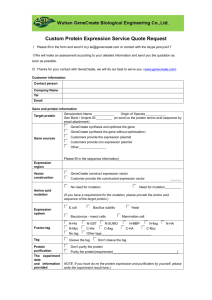
advertisement

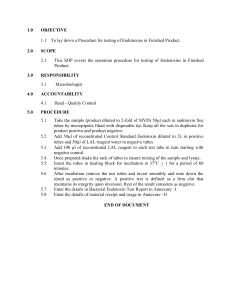
ONE HEALTH ASPECTS OF ENDOTOXEMIA Michelle Henry Barton DVM, PhD, DACVIM Department of Large Animal Medicine, College of Veterinary Medicine, University of Georgia, Athens, GA INTRODUCTION Richard Pfeifer first characterized endotoxin in the 1890s as a toxin that was an integral part of gramnegative bacteria that was distinctly different from actively secreted heat labile exotoxins .1 Endotoxin comprises approximately 75% of the outer cell membrane of gram-negative bacteria and serves as a structural permeability barrier. Pfeifer’s original observations were correct: bacteria do not actively secrete endotoxin. Rather, when gram-negative bacteria multiply or lyse upon bacterial cell death, endotoxin is released from the outer cell membrane. Endotoxin consists of three structural domains: a highly variable outer polysaccharide “O-antigenic” region, a core region consisting mostly of monosaccharides, and the highly conserved toxic moiety, lipid A. Variation in the number, length, saturation, and position of fatty acids on the glucosamine disaccharide backbone of lipid A confers its degree of toxicity. Endotoxin has been evolutionarily conserved as a pathogen associated molecular pattern that is immediately recognized by the innate immune system that subsequently initiates a series of inflammatory signals that serve to warn of and control the bacterial invasion. However, mammalian species vary considerably in their ability to recognize the presence of endotoxin. The main purpose of this discussion is to review what is known about endotoxemia among species, with particular emphasis on comparative aspects between human beings, laboratory animals used in research, and two common domestic companion-animals representing a large animal (horse) a small animal (dog) model. PATHOLOGY OF ENDOTOXEMIA Endotoxin is not directly toxic to epithelial barriers rather it must translocate through the epithelium to fully manifest its toxic effects. Once in the blood, endotoxin’s amphipathic properties cause it to form aggregates that resemble micelles. Lipopolysaccharide binding protein (LBP), a 65 kDa plasma constituent that belongs to a family of lipid transfer proteins, efficiently extracts molecules of endotoxin from aggregated micelles in the blood and serves as a transporter, shuttling molecules of endotoxin to various locations .2 Once at the cell surface, endotoxin is transferred to cluster differentiation antigen 14 (CD14), a well-conserved receptor attached by a glycosylphosphatidylinositol anchor. Mononuclear phagocytes (monocytes and macrophages) express abundant CD14, though other inflammatory cells also express minute amounts. CD14 is a 53 kDa glycoprotein that exists as both a cell membrane receptor (mCD14) and as a soluble form (sCD14) in the circulation .3 CD14 does not structurally transverse the cell membrane. Thus it must associate with a secondary protein, Toll-like receptor (TLR4)4 that contains a transmembrane portion that is capable of communication with the intracellular domain. Both CD14 and TLR4 are classified as bacterial recognition receptors, indicating that they are evolutionarily conserved receptors that are a part of the innate immune system. Once the CD14-TLR4-endotoxin complex is assembled at the cell surface, TLR4 requires the help of a 160 amino acid helper molecule, MD2, to transmit a signal to the cytosol.5 Numerous intracellular signaling pathways have been reported to link the endotoxin-occupied cell surface receptor to a response from the cell; however, the nuclear factor kB (NFkB) pathway is well characterized.4 Ultimately, the deleterious effects of endotoxin are the result of overzealous endogenous synthesis of pro-inflammatory mediators triggered by this cell receptor mediated pathway. The most widely studied of these mediators are the metabolites of arachidonic acid (the prostaglandins, thromboxane, and the leukotrienes), platelet activating factor, cytokines (tumor necrosis factor and interleukins 1 and 6), vasoactive and chemotactic peptides (histamine, serotonin, bradykinin, complement components), tissue factor, proteolytic enzymes, and reactive oxygen species. MODELS OF ENDOTOXEMIA It is well recognized that the response to endotoxin varies tremendously among mammalian species. It is often argued that human beings and horses are more sensitive to endotoxin than rodents, common laboratory models of endotoxemia. It is difficult to directly compare the response of endotoxin among species, as rarely are multiple species investigated under the exact same conditions. Variation in the source of endotoxin, doses, in vitro or cell culture systems, and species-specific methodologies to quantitate the response to endotoxin further hinder direct comparisons. The LA50 for endotoxin in dogs and mice is reported to be 1 mg/kg and between 1 to 25 mg/kg, respectively.6,7 High dose endotoxin infusion models are not performed in people for obvious reasons and to the author’s knowledge, the actual LD50 of endotoxin in horses is not known. However, it is known that doses in the µg/kg range can be lethal or near lethal in horses and people.8,9 In low dose infusion models, people and horses demonstrate a significant response to nanograms of endotoxin per kilogram of body weight, whereas to evoke a similar response in rodents and dogs, micrograms of endotoxin per kilogram of body weight are required. 10,11 Accounting for Species Differences in the Response to Endotoxin There are numerous explanations for the differential response to endotoxin, many of which reside at the cellular and molecular level. When endotoxin gains access to the circulation, differential concentrations and binding affinities of natural ligands of endotoxin, such as LBP, sCD14, high-density lipoproteins, and antibodies to endotoxin can influence the toxicity, transport, and final destination of endotoxin. Next, differential expression of and subtle differences in the molecular structure of the cellular receptors for endotoxin can have profound effects on the responsiveness to endotoxin. Gene knockout and transfection experiments have demonstrated that the type and degree of responsiveness to endotoxin is conferred by the species of origin of the receptors. Much of this discovery was afforded by the results of treatment trials with lipopolysaccharides. For example, Rhodobacter sphaeroides and a synthetic derivative of its lipid A moiety (E5531) are endotoxin antagonists in humans and mice. 12 That is, R. sphaeroides endotoxin is a nontoxic molecule that does not evoke an inflammatory response in humans and mice and in fact, will competitively inhibit the response to native toxic enteric endotoxin. However this same molecule is a potent agonist in hamsters and horses.12 Through a series of transfection experiments of a cell culture line with vectors encoding CD14, TLR4, and MD2 of either human or equine origin, it was determined that both TLR4 and MD2 must be of human origin to be recognized by R. sphaeroides lipopolysaccharide as an antagonist. Similarly, both TLR4 and MD2 must be of equine origin to be recognized by R. sphaeroides as an agonist. Interestingly, within this same study, comparison of the cellular response to E. coli endotoxin in the cells transfected with human receptors versus the same cells transfected with an equivalent amount of the equine receptors showed that the equine response was more sensitive than the human response. In addition to the importance of species-specific recognition of different sources of endotoxin, molecular differences in the endotoxin receptors themselves are important. For example, for decades, it was known that C3H/HeJ mice were incapable for responding to endotoxin. Only recently was it discovered that the inability of C3H/HeJ mice to respond to endotoxin was caused by a mutation in the gene encoding for TLR4. 4 Furthermore, polymorphism in TLR4 is associated with differences in the degree of response to endotoxin in people and offers explanation to the well-recognized clinical phenomenon that some individuals react violently to endotoxin, while others have little to no response.25 Polymorphisms in CD14 and TLR4 have been described in horses; however, it is yet to be seen if these molecular changes explain a differential response to endotoxin.13 Lastly, differences in the intracellular signaling cascades that transfer the signal of endotoxin-receptor complex to the nucleus for transrepression or transactivation of proinflammatory and anti-inflammatory genes may account for variable species sensitivity to endotoxin.14 Naturally Acquired Endotoxemia: Looking Back at the Big Picture The keystone of studying clinically important diseases is to secure a model that is most relevant to the naturally occurring scenario. Considering that endotoxin is released during gram-negative bacterial replication, the two most common sources of endotoxin in mammalian species are the gastrointestinal tract flora and acquired gramnegative bacterial invasion. Bacteria comprise 40% of the human fecal mass15 (which is even greater in horses) and thus clearly the resident population of gram negative bacteria in the intestinal tract is a virtual septic tank of endotoxin. For example, the cecum of the horse contains approximately 80 g of endotoxin per ml and thus only one ml of cecal liquor could be lethal to a horse.16 However, this source of endotoxin is normally confined to the lumen of the healthy intestine by protective mucosal barriers. If the intestinal wall is damaged, such as occurs in acute gastrointestinal diseases that cause inflammation or ischemia, the otherwise contained endotoxin gains access to the peritoneal cavity as well as the circulation. Interestingly, the natural flora, and therefore the source and amount of endogenous endotoxin, varies among species and this fundamental difference can account for some degree of the diverse response to endotoxin. For example, germ free animals have a dampened clinical response and lower mortality rate in intestinal strangulation and hemorrhagic shock models than do their nongerm free cohorts. 15 Differences in the anatomy and permeability of the mucosal barrier to endotoxin also determine the degree of translocation of both bacteria and endotoxin further contributing to diversity in the response to endotoxin. In the scenario of gram-negative bacterial invasion, endotoxin is released into the immediate environment as bacteria replicate. In the case of local sepsis, the endotoxin can eventually be absorbed into nearby lymphatics or blood vessels to gain access to the general circulation. In the situation of bacteremia, the bacteria and endotoxin are concurrently present in the circulation. For rodents, it is difficult to know how often endotoxemia occurs naturally and if it does, what is its epidemiology. In people, endotoxin has been detected in the plasma under many different scenarios including patients with severe burns, liver disease, gastrointestinal disease, hemorrhagic shock, and trauma and in patients undergoing dialysis, invasive procedures, cardiopulmonary by-pass surgery, organ transplantation and chemotherapy.17 Endotoxin is even detectable in exhausted marathon runners.17 However, it is sepsis in both neonates and adults that carries the greatest prevalence of endotoxemia. 17 Septic shock is the most common cause of death in noncardiac patients in the ICU and is currently among the top ten causes of death in the United States.18 In a 2003 report on the epidemiology of sepsis, gram negative infections predominated before 1987. 18 In infants, septicemia occurs in approximately 20 out of very 1000 live births with E. coli reported as the most commonly isolated pathogen in early onset sepsis.19 In one large study in human beings with sepsis, endotoxin was detected in the circulation of 33% of the patients (mean of approximately 100 pg/ml, range 40 to 1,100 pg/ml). 20 There are only a few studies that have investigated the incidence of endotoxemia in infants. Although it appears that the detection rate is lower in septic infants than in adults, large endotoxin concentrations are detectable in infants with necrotizing entercolitis.21,22 In horses, endotoxemia has been most intensively studied in the adult patient with acute gastrointestinal disease and the neonatal foal with septicemia.23-28 In mature horses referred to tertiary care centers with any etiology of acute gastrointestinal disease causing colic, endotoxin has been detected in the plasma of approximately 25% of the horses.23,24 In horses with surgical colic, endotoxin was detected in the plasma of 41% of referred cases (mean of 36 pg/ml, range 7-197 pg/ml).25 In the largest published study on detection of endotoxin in horses with acute gastrointestinal disease (n=155), endotoxin was detected in the plasma of 10% (mean 218 pg/ml) and peritoneal fluid of 30% (mean of 509 pg/ml) of all referred cases. 26 Although endotoxemia is also implicated in pleuropneumonia, peritonitis, and metritis in mature horses, there are no comprehensive clinical studies documenting its occurrence in these scenarios. Accurate data on the incidence of septicemia in foals is lacking, though it is generally agreed that septicemia is a major cause of morbidity and mortality in the first week of life. Like human infants, gram-negative septicemia with E. coli predominates. The incidence of endotoxemia in foals suspected to have septicemia ranges from 28 to 50% (mean plasma concentrations of roughly 240 to 400 pg/ml). 27,28 When gram negative sepsis was detected by blood culture in foals, up to 269,600 pg of endotoxin was concurrently detected per ml of plasma! 27 In dogs, endotoxemia is reported to occur most commonly with primary septic diseases, such as peritonitis and pyometria, or secondary to gastrointestinal diseases that culminate in translocation of luminal endotoxin, such as occurs in puppies with parvovirus enteritis and adult dogs with gastric dilatation and volvulus.29,30 There are only a few clinical studies that document naturally-occurring endotoxemia in dogs. In puppies with parvovirus, the mean concentration of endotoxin was 46 pg/ml,31 which is similar to that reported in bitches with pyometria. 32 Whether released from endogenous sources from the intestinal lumen or from overwhelming gram-negative sepsis, the systemic features of endotoxemia are very similar in people and horses. Within an hour of intravenous injection of low doses of endotoxin (2 to 4 ng/kg body weight), human subjects experience symptoms ranging from chills, headache, back pain, myalgias, fever, nausea, and photophobia. Tachycardia, mild hypertension, and leukocytosis ensue.33 Within the first hour of intravenous challenge with endotoxin (10 to 30 ng/kg), horses yawn frequently, have mucous membrane pallor, become depressed, anorectic, tachypneic, tachycardic, and restless, develop fasciculations and mild to moderate signs of abdominal pain, and pass loose feces. 34,35 This period is the early hyperdynamic phase of endotoxemia that is characterized by pulmonary hypertension and ileus. Mucous membranes are often hyperemic and capillary refill time is prolonged. By 1 to 2 hours after challenge, depression and anorexia continue and are affiliated with the onset of fever and hypotension. With reduced tissue perfusion, the classic “toxic line” develops as a red to blue-purple line at the periphery of the gums. If hypotension advances, mucous membranes become diffusely congested, progressing to cyanosis and then a grayish-purple pallor. One notable difference between people and horses/dogs is the hemogram changes that occur during endotoxemia. In people, lymphopenia and neutrophilia are reported with low dose infusion of endotoxin,33 whereas in horses (both neonates and adults) and dogs, profound neutropenia with toxic neutrophil morphology is a cardinal sign of endotoxemia and/or acute overwhelming bacterial infection.34 With the similarities in the systemic features of sepsis and endotoxemia, it should not be surprising that documentation of pro-inflammatory mediator release in human patients and horses is abundant and, in general, similar profiles are described in both experimental infusion models and naturally-occurring endotoxemia.10,33,34 The cytokines tumor necrosis factor (TNF) and interleukin 6 (IL6) have probably received the most attention as early and late markers, respectively, of endotoxemia, Specifically, in horses, TNF and IL6 were detected in the serum of 10% and 67% of equine patients with acute surgical abdomens.25 TNF and IL6 in serum or peritoneal fluid are greater in horses with strangulating or inflammatory lesions and are significantly correlated with the concurrent detection of endotoxin and a poor prognosis for survival to discharge. 25,26 In foals with presumed septicemia, endotoxemia correlated with a positive sepsis score, a positive blood culture, increased cytokine concentrations, and poor outcome.27,28 Likewise, cytokine profiles in dogs and rodents experimentally infused with endotoxin is similar to that reported for people and horses36 and in endotoxemic dogs with parvovirus, TNF levels correlated with mortalitiy.29 Recent work comparing the cytokine gene profiles between people and mice demonstrated very poor correlation, again questioning the use of the mouse as a human model.37 Although it generally takes a much larger dose of endotoxin to elicit similar cytokine profiles in rodents, their role in understanding the pathophysiology of endotoxemia cannot be undermined for it was mice and rat models that first led to the discovery of TNF and the role of eicosanoids in endotoxemia.10 Advanced Sepsis and Endotoxemia When the systemic pro-inflammatory response to infection or endotoxemia is uncontrolled and malignant, the clinical state of Systemic Inflammatory Response Syndrome (SIRS) ensues. Based on a consensus statement issued by the American College of Chest Physicians and Society of Critical Care Medicine, a patient should be considered to have SIRS if at least two of the following signs are present: fever/hypothermia, tachycardia, tachypnea and/or altered white blood cell count.38 Though specific criteria for SIRS have not been developed for equine or canine patients, the syndrome of SIRS is applicable. And in fact, the sepsis scoring system proposed in the 1980's for foals contains several of the human SIRS criteria.39 However, SIRS criteria have been proposed for horses and dogs and are patterned after the human criteria, taking into account species differences on variation from normal (see Table 1 below). As endothelial damage, the release of vasoactive and unregulated inflammatory mediators, and microthrombi formation progress, Multiple Organ Dysfunction Syndrome (MODS) develops.38 In people, the syndrome is defined by criteria for identification of individual organ dysfunction with the respiratory, renal, hemostatic, cardiovascular, gastrointestinal, hepatic, nervous, musculoskeletal, and adrenal systems most commonly affected and has been reviewed early in this series.40 Multiple organ dysfunction is a syndrome that is definition dependent and unfortunately, a consensus of definition has not yet been accepted for horses or dogs, though there have been some proposed criteria suggested for the dog (see Table 2 below).41 In general terms, many of the diagnostic criteria that have been proposed in people could also be applied to the horse, with some exceptions. For example, bilirubin concentration, the criteria used for liver dysfunction in people, may not be specific in the horse owing to physiologic hyperbilirubinemia that occurs with anurexia. One body system affected by endotoxemia and sepsis that has been extensively studied in horses with SIRS is coagulation. In mature horses with colic, an abnormally prolonged prothrombin time (PT) was reported in 25-80% of all colic cases at admission and 58% of cases diagnosed with disseminated intravascular coagulopathy (DIC). 42 Similarly, prolonged activated partial thromboplastin time (APTT) was reported in 43-100% of all colic admissions, and 60% of horses with colic in DIC.42 Both PT and APTT were prolonged in septic foals and both were correlated with detection of endotoxin in the blood.28 Thus PT or APTT may be better criterion for coagulopathy in horses than a citrated platelet count. Finally, laminitis is a recognized manifestation of endotoxemia and systemic illness in the horse and thus could be proposed as a unique musculoskeletal manifestation of MODS in this species. Concluding Remarks Collectively considering species-specific pathophysiologic responses, it would appear that the horse more closely approximates the human clinical response to endotoxin, than does the mouse or dog. Advantages of the horse as a model of endotoxemia and sepsis are that horses and foals have a high rate of naturally-acquired disease that allows study of endotoxemia in a clinical setting and their size allows collection of large amounts of blood and body cavity fluids or tissue samples in either a clinical or experimental setting. The largest disadvantage is the cost of maintenance of horses with the per diem approaching 30 times that of a mouse in an exclusive research setting. The ability to use horses in teaching herds at veterinary colleges for nonlethal, ex vivo, and in vitro studies significantly offsets the per diem, making them an attractive animal model for the study of endotoxemia. Table 1. Systemic Inflammatory Response Syndrome Criteria in Humans and Proposed Criteria for Horses and Dogs. HUMAN38 HORSE43 DOG44 Temperature < 96.8F or > 100.4F (98.6F)* <98 or >101.5 (99-100.9)* < 99 or > 103 (100-102.5)* Heart Rate > 90 bpm (60 to 100) > 50 (24-48) >150 (60-140) Respiratory Rate >20 or PaCO2 < 32 (12 to 18) > 25 (8-20) >40 (18-24) WBC < 4,000 or > 12,000/µL or > 10% bands (4,500 to 10,000) < 5,000 or > 14,500/µL or > 10% bands (4,500-12,000) < 5,000 or >19,000/µL (5,000-14,000) *numbers in parentheses represent normal reference range. Table 2. Proposed Canine Criteria for Multiple Organ Dysfunction41 Organ System Criteria Respiratory Renal SpO2 < 95% Need for supplemental O2 A-a O2 gradient > 10 mmHg* Serum creatinine > 0.5 mg/dl Hepatic Bilirubin > 0.5 mg/dl Cardiovascular If pressors needed Hematologic PT or APTT > 25% above upper range or platelet count < 100,000/µL None proposed Neurologic *on room air, A-a gradient = [150-5/4(PaCO2)] – PaO2 REFERENCES 1. Pfeiffer R. Untersuchungen ueber das choleragift. Z Hyg 1892;11:393-412. 2. Fenton M, Golenbock D. LPS-binding proteins and receptors. J Leukocyte Biol 1998;64:25-32. 3. Antal-Szalmas P. Evaluation of CD14 in host defense. European J Clin Invest 2000;30:167-179. 4. Brightbill H, Modlin R. Toll-likereceptors: molecular mechanisms of the mammalian immune response. Immunology 2000;101:1-10. 5. Dziarski R, Wang Q, Miyake K, et al. MD2 enables Toll like receptor mediated responses to lipopolysaccharide. J Immunolog 2001;166:1938-1944. 6. Goldfarb RD, Tambolini W, Wiener SM, et al. Canine left ventricular performance during LD50 endotoxemia. Am J Physiol 1983;244:H370-377. 7. Fink MP. Animal models of sepsis. Virulence 2014;5:143-153. 8. Burrows G, Cannon J. Endotoxemi induced by rapid injection of E. coli in anesthesized ponies. Am J Vet Res 1973;31:1967-1973. 9. Taveira da Silva A, Kaulbach H, Chuidian F, et al. Brief report: shock and multiple-organ dysfunction after self-administration of Salmonella endotoxin. N Engl J Med 1993;328:1457-1460. 10. 11. 12. 13. 14. 15. 16. 17. 18. 19. 20. 21. 22. 23. 24. 25. 26. 27. 28. 29. 30. 31. 32. 33. 34. 35. 36. Copeland S, Warren S, Lowry S, et al. Acute inflammatory response to endotoxin in mice and humans. Clin Diagnostic Lab Immunol 2005;12:60-67. Yoshizawa M, Ohtake K, Kubota T. [Evaluation of the dose of endotoxin to produce endotoxin shock models in dogs]. Masui 1991;40:605-610. Lohmann K, Vandenplas M, Barton M, et al. The equine TLR4/MD2 complex mediates recognition of lipopolysaccharide from Rhodobacter sphaeroides as an agonist. J Endotoxin R 2007;13:235-242. Vychodilova-Krenkova L, Matiasovic J, Horin P. Single nucleotide polymorphism in four functionally related immune response genes in the horse: CD14, TLR4, Ce and FceR1 alpha. International J Immunogenetics 2005;32:277-283. Scare S, Andreakos E, Feldman M, et al. Endotoxin signaling in human macrophages: signaling via an alternative mechanism. J Endotoxin R 2004;10:445-452. Wells C, Hess D, Erlandsen S. Impact of the indigenous flora in animal models of shock and sepsis. Shock 2004;22:562-568. Moore J, Garner H. Intracecal endotoxin and lactate during the onset of equine laminitis. Am J Vet Res 1979;40:722-723. Hurley J. Endotoxemia: Methods of Detection and Clinical Correlates. Clin Microbiol Reviews 1 995;8:268-292. Martin G, Mannino D, Eaton S, et al. The epidemiology of sepsis in the United States from 1979 through 2000. NEJM 2003;348:1546-1554. Stoll B, Hansen N, Higgins R, et al. Very low birth weight preterm infants with early onset neonatal sepsis. Ped Infect Disease J 2005;24:635-639. Ketchum P, Parsonnet J, Stotts L, et al. Utilization of a chromogenic Limulus amebocyte lysate blood assay in a multi-center study of sepsis. J Endo Res 1997;4:9-16. Pavcnik-Arnol M, Hojker S, Derganc M. Lipopolysaccharide binding protein, lipopolysaccharide, and soluble CD14 in sepsis of critically ill neonates and children. Intensive Care Med 2007;33:1025-1032. Sharma R, Tepas J, Hudak M, et al. Neonatal gut barrier and multiple organ failure: role of endotoxin and proinflammatory cytokines in sepsis and necrotizing enteritis. J Ped Surg 2007;42:454-461. King J, Gerring E. Detection of endotoxin in cases of equine colic. Vet Record 1988;123:269-271. Meyers K, Reed S, Keck M, et al. Circulating endotoxin-like substances and altered hemostasis in horses with gastrointestinal disorders: an interim report. Am J Vet Res 1982;43:2233-2236. Steverink P, Sturk A, Rutten V, et al. Endotoxin, interleuking 6 and tumor necrosis factor concentrations in equine acute abdominal disease: relations to clinical outcome. J Endotoxin R 1995;2:289299. Barton N, Collatos C. Tumor necrosis factor and interleukin 6 activity and endotoxin concentration in peritoneal fluid and blood of horses with acute abdominal disease. J Vet Intern Med 1999;13:457-464. Breuhaus B, Gegraves F. Plasma endotoxin concentration in clinically normal and potentially septic equine neonates. J Vet Intern Med 1993;7:296-302. Barton M, Morris D, Norton N, et al. Hemostatic and fibrinolytic indices in neonatal foals with presumed septicemia. J Vet Intern Med 1998;12:26-35. Otto CM, Drobatz KJ, Soter C. Endotoxemia and tumor necrosis factor activity in dogs with naturally occurring parvoviral enteritis. Journal of Veterinary Internal Medicine 1997;11:65-70. Davidson JR, Lantz GC, Salisbury SK, et al. Effects of Flunixin Meglumine on Dogs with Experimental Gastric Dilatation-Volvulus. Veterinary Surgery 1992;21:113-120. Isogai E, Isogai H, Onuma M, et al. Escherichia-Coli Associated Endotoxemia in Dogs with Parvovirus Infection. Japanese Journal of Veterinary Science 1989;51:597-606. Hagman R, Kindahl H, Lagerstedt AS. Pyometra in bitches induces elevated plasma endotoxin and prostaglandin F-2 alpha metabolite levels. Acta Veterinaria Scandinavica 2006;47:55-67. Lowry S. Human endotoxemia: a model for mechanistic insight and therapeutic targeting. Shock 2005;24:94-100. Barton M, Parviainen A, Norton N. Polymyxin B protects horses against induced endotoxaemia in vivo. Equine Veterinary Journal 2004;36:397-401. Moore J. Recognition and treatment of endotoxemia. Vet Clin North Am Equine Pract 1988;4:105-113. Yu DH, Kim B, Park J. Pathophysiologic and Immunologic Changes in a Canine Endotoxemia over a Period of 24 Hours. Journal of Veterinary Medical Science 2012;74:537-544. 37. 38. 39. 40. 41. 42. 43. 44. Seok J, Warren HS, Cuenca AG, et al. Genomic responses in mouse models poorly mimic human inflammatory diseases. Proceedings of the National Academy of Sciences of the United States of America 2013;110:3507-3512. Bone R, Balk R, Cerra F, et al. Definitions of sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. The ACCP/SCCM Consensus Conference Committee. American College of Chest Physicians/Society of Critical Care Medicine. Chest 1992;101:1644-1655. Brewer B, Koterba A. Development of a scoring system for the early diagnosis of equine neonatal sepsis. Equine Vet J 1988;20:18-22. Balk R. Pathogenesis and management of multiple organ dysfunction or failure in severe sepsis and septic shock. Crit Care Clin 2000;16:337-352. Kenney EM, Rozanski EA, Rush JE, et al. Association between outcome and organ system dysfunction in dogs with sepsis: 114 cases (2003-2007). Javma-Journal of the American Veterinary Medical Association 2010;236:83-87. Barton M. Dyshemostatis in sepsis. Proceedings of the International Veterinary Emergency and Critical Care Society, Atlanta GA 2005. Borde L, Amory H, Grulke S, et al. Prognostic value of echocardiographic and Doppler parameters in horses admitted for colic complicated by systemic inflammatory response syndrome. J Vet Emerg Crit Care (San Antonio) 2014;24:302-310. Otto C. Sepsis in veterinary patients: what do we know nad where can we go? J Vet Emerg Crit Care 2007;17:329-332.