Lecture 28 - Management of chronic musculoskeletal
advertisement
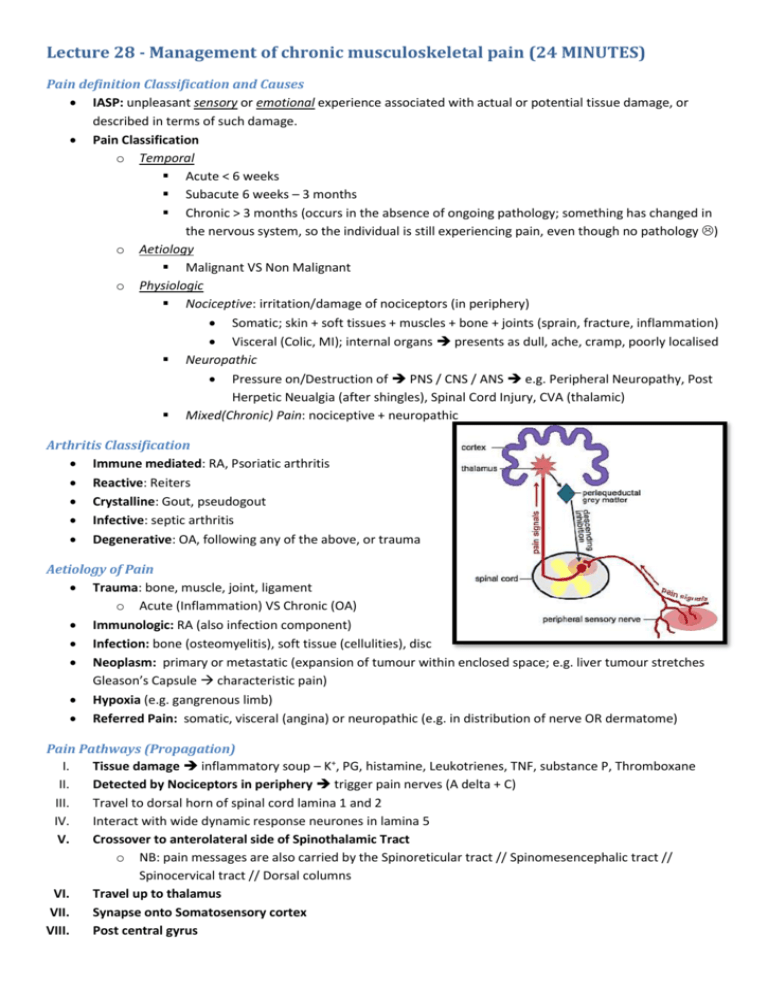
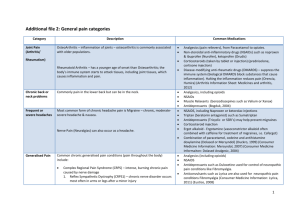
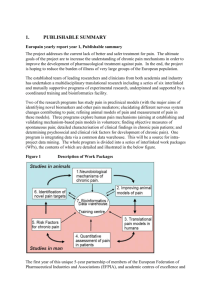
Lecture 28 - Management of chronic musculoskeletal pain (24 MINUTES) Pain definition Classification and Causes IASP: unpleasant sensory or emotional experience associated with actual or potential tissue damage, or described in terms of such damage. Pain Classification o Temporal Acute < 6 weeks Subacute 6 weeks – 3 months Chronic > 3 months (occurs in the absence of ongoing pathology; something has changed in the nervous system, so the individual is still experiencing pain, even though no pathology ) o Aetiology Malignant VS Non Malignant o Physiologic Nociceptive: irritation/damage of nociceptors (in periphery) Somatic; skin + soft tissues + muscles + bone + joints (sprain, fracture, inflammation) Visceral (Colic, MI); internal organs presents as dull, ache, cramp, poorly localised Neuropathic Pressure on/Destruction of PNS / CNS / ANS e.g. Peripheral Neuropathy, Post Herpetic Neualgia (after shingles), Spinal Cord Injury, CVA (thalamic) Mixed(Chronic) Pain: nociceptive + neuropathic Arthritis Classification Immune mediated: RA, Psoriatic arthritis Reactive: Reiters Crystalline: Gout, pseudogout Infective: septic arthritis Degenerative: OA, following any of the above, or trauma Aetiology of Pain Trauma: bone, muscle, joint, ligament o Acute (Inflammation) VS Chronic (OA) Immunologic: RA (also infection component) Infection: bone (osteomyelitis), soft tissue (cellulities), disc Neoplasm: primary or metastatic (expansion of tumour within enclosed space; e.g. liver tumour stretches Gleason’s Capsule characteristic pain) Hypoxia (e.g. gangrenous limb) Referred Pain: somatic, visceral (angina) or neuropathic (e.g. in distribution of nerve OR dermatome) Pain Pathways (Propagation) I. Tissue damage inflammatory soup – K+, PG, histamine, Leukotrienes, TNF, substance P, Thromboxane II. Detected by Nociceptors in periphery trigger pain nerves (A delta + C) III. Travel to dorsal horn of spinal cord lamina 1 and 2 IV. Interact with wide dynamic response neurones in lamina 5 V. Crossover to anterolateral side of Spinothalamic Tract o NB: pain messages are also carried by the Spinoreticular tract // Spinomesencephalic tract // Spinocervical tract // Dorsal columns VI. Travel up to thalamus VII. Synapse onto Somatosensory cortex VIII. Post central gyrus Pain Pathways (Modulation) Frontal / temporal lobes o Emotional and cognitive responses (interpretation) to pain Descending inhibitory pathways o Hypothalamus, Periaqueductal grey, Locus ceruleus, Ventromedial and ventrolateral medulla Gate Control theory o modulation of nociceptive input by descending influences at dorsal horn Other influences o Pain triggers arousal (Autonomic Nervous System aroused) o Withdrawal – reflex (if danger, automatic withdrawal) and higher level (behavioural; if someone trying to hurt you) o Autonomic stress response primitive responses from brainstem eg nausea, sweating (particularly with visceral pain) o Hormonal stress response Chronic Pain: No Nociception “Wind up” – sustained nociceptive input (eg damaged nerves) [due to changes in Spinal Cord + Brain] I. CNS becomes sensitised to experiencing pain II. Activates NMDA receptors dorsal horn (NB: important for treatment) III. Lower threshold for pain in injured and surrounding tissue NB: also spontaneous nociceptive activity IV. Expansion of nociceptive field (in 2 ways): Allodynia (perception of pain, from a not normally painful stimulus) hyperalgesia (increased sensitivity to pain, which may be caused by damage to nociceptors or peripheral nerves) Chronic Pain: Psychosocial Physical Changes (following can magnify pain they are experiencing right now) (people with pain tend NOT to move around as much causes secondary effects ) o Weakness, poor fitness, joint stiffness o Fatigue, insomnia, appetite changes o Iatrogenic complications (medications) Psychological Changes – mood, anxiety, grieving Social Changes – sick role, illness behaviour, secondary gain, financial, employment changes Why Pain is Important: Epidemiology Common: 70% > 65 = pain in the previous year // 30% report persistent pain (>6 mo) Personal - aim to avoid chronicity – physical, functional, psychological and social impacts Economic - $34 000 000 000 / year o 20:80 rule (80% of costs come from 20% of chronic patients) o Off work 1 year, 2% chance of ever Returning To Work Importance of Assessing Pain o 70% of Answers from History o 20% from Examination o 10% from Investigation Pain History Taking SOCRATES o Description of Pain Nociceptive Somatic: ache, sharp, throbbing, well localised Visceral: throbbing, deep Organ capsule: sharp Obstruction: crampy, colicy Neuropathic Burning, stinging, lancinating, electrical qualities, allodynia, deep aching. Along peripheral nerve, dermatomal distribution o Associated Symptoms Systems review, fevers, chills, night sweats, weight loss, weakness, sensory changes, bowels, bladder sexual dysfunction Other Important Points o Past and present treatments for pain o Co-morbidities – HIV, Cancer, IVDU o Medications – past and present, Prescription, and over the counter, side effects, steroids? o Social History – where, with who, financial, o Smoking, Alcohol, Caffeine, Illicit drugs (may lower threshold of pain) Functional Assessment o Sleep o Appetite o Mood / anxiety o Mobility o Activities of Daily Living Personal – eat, dress, shower, toilet Domestic – cook, clean, wash, Community – Work, drive, shop, recreation Pain Assessment in the Elderly o NB: important to get the carer input o Atypical Presentations Confusion, Delirium, Fatigue, Insomnia, ↓ Appetite, Weight loss, Constipation, Frustration, Withdrawal, Anxiety, Depression, Agitation, Stop walking, Refuse to self care Impact of Pain on Person (Pscyhosocial) o Finances o Expectations for treatment o Responses of others to pain (family, friends, colleagues, HCW) hostile, helpful, supportive? Red Flags o Major/minor trauma o Steroids in past o Systemically unwell; fevers, chills, night sweats, weight loss o History of cancer, bacterial infection o IVDU, HIV o Night pain o Severe localised pain o Neurological changes Tools for Assessing Pain Visual Analogue Scale: 10cm line, patient says how bad it is Numeric Rating Scale: out of 10 Verbal descriptor – 7 point scale (mild, modersate, severe etc.) Abbey pain scale – cognitive impairment – includes behaviours Brief Pain Inventory McGill Pain Questionnaire Psychology and Pain Psychosocial Yellow Flags o Attitudes and beliefs Incorrect: pain is dangerous, movement will cause damage, rest and passive modalities best o Behaviours fear avoidance, reliance of medications, 5 Waddell signs o Compensation issues ½ rate full recovery // Catastrophisation o Diagnosis (unclear) and treatment (passive); different doctors say different things o Emotions anxiety, depression Employment risk fx = Poor job satisfaction, Unstable job history, Stress at work, Poor work relationships, Unsupportive work envt, Low education, low SES, Bad previous injury mx, Heavy work, shift work o Family and social support – too much / little Examination Usually focus on MSK / neurological Functional assessment – walking, ADL Palpation, Percussion Observe behaviour, non verbal cues Waddell signs Tenderness tests: Superficial, diffuse, non anatomic o Simulation: pain with no movement axial loading, simulated rotation (hurting in wrong place = faking LOLOL) o Distraction: SLR in seated position o Regional Disturbances: deviation from accepted neuroanatomy o Over Reaction Mental state examination – psych issues Multi-disciplinary assessment – medical, PT, OT, Psychology Investigation Rational use of Ix – will the result affect your clinical decision making and management? Overexpectations X-rays – functional views; flexed etc. // Ultrasound – soft tissue // CT – bone, when MRT c/i MRI – tumor, infection, soft tissue, acute bony injury // PET: malignancy // Bone Scan – fracture, malignancy Others for red flag conditions Rainbow Flags Faking Pain