Long-term outcome of deep brain stimulation in fragile X
advertisement
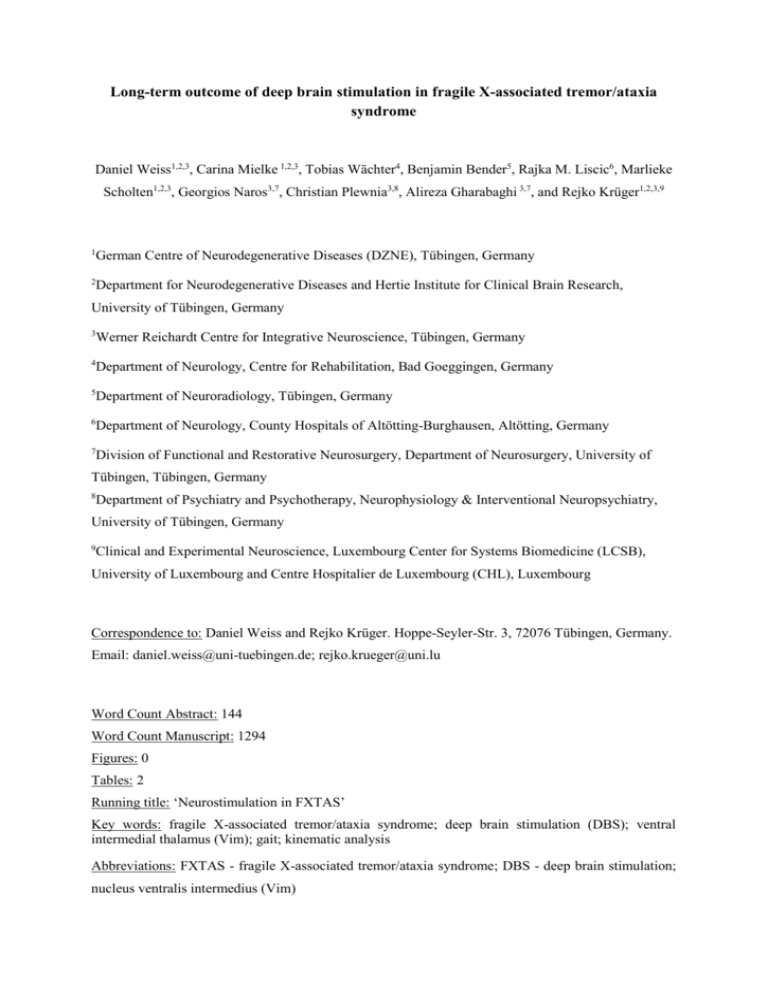
Long-term outcome of deep brain stimulation in fragile X-associated tremor/ataxia syndrome Daniel Weiss1,2,3, Carina Mielke 1,2,3, Tobias Wächter4, Benjamin Bender5, Rajka M. Liscic6, Marlieke Scholten1,2,3, Georgios Naros3,7, Christian Plewnia3,8, Alireza Gharabaghi 3,7, and Rejko Krüger1,2,3,9 1 German Centre of Neurodegenerative Diseases (DZNE), Tübingen, Germany 2 Department for Neurodegenerative Diseases and Hertie Institute for Clinical Brain Research, University of Tübingen, Germany 3 Werner Reichardt Centre for Integrative Neuroscience, Tübingen, Germany 4 Department of Neurology, Centre for Rehabilitation, Bad Goeggingen, Germany 5 Department of Neuroradiology, Tübingen, Germany 6 Department of Neurology, County Hospitals of Altötting-Burghausen, Altötting, Germany 7 Division of Functional and Restorative Neurosurgery, Department of Neurosurgery, University of Tübingen, Tübingen, Germany 8 Department of Psychiatry and Psychotherapy, Neurophysiology & Interventional Neuropsychiatry, University of Tübingen, Germany 9 Clinical and Experimental Neuroscience, Luxembourg Center for Systems Biomedicine (LCSB), University of Luxembourg and Centre Hospitalier de Luxembourg (CHL), Luxembourg Correspondence to: Daniel Weiss and Rejko Krüger. Hoppe-Seyler-Str. 3, 72076 Tübingen, Germany. Email: daniel.weiss@uni-tuebingen.de; rejko.krueger@uni.lu Word Count Abstract: 144 Word Count Manuscript: 1294 Figures: 0 Tables: 2 Running title: ‘Neurostimulation in FXTAS’ Key words: fragile X-associated tremor/ataxia syndrome; deep brain stimulation (DBS); ventral intermedial thalamus (Vim); gait; kinematic analysis Abbreviations: FXTAS - fragile X-associated tremor/ataxia syndrome; DBS - deep brain stimulation; nucleus ventralis intermedius (Vim) ABSTRACT Background: Fragile X-associated tremor/ataxia syndrome (FXTAS) presents as complex movement disorder including tremor and cerebellar ataxia. Deep brain stimulation of the nucleus ventralis intermedius (Vim-DBS) is an effective treatment for essential tremor, however, its efficacy and safety in atypical tremor syndromes like FXTAS remains to be determined. Methods: Here, we report the therapeutic long-term outcome of three male genetically-confirmed FXTAS patients treated with Vim-DBS for up to four years using standardized assessments. Results: All three patients demonstrated sustained improvement of both tremor and ataxia – the latter included improvement of intention tremor and axial tremor. Kinematic gait analyses further demonstrated a regularization of the gait cycle. Initial improvements of hand functional disability were not sustained and reached the preoperative level of impairment within one to two years from surgery. Conclusions: Our data suggest that genetic biomarkers may help to stratify patients for potential neurostimulation outcome. Introduction Fragile X-associated tremor/ataxia syndrome (FXTAS) is an inherited, X-linked, adult-onset neurodegenerative disorder caused by expanded trinucleotide repeats in the 5` untranslated region of the fragile X mental retardation 1 (FMR1) gene1. Typically, pathological increases in repeat length represent the most common cause for inherited mental retardation in males. However, premutation alleles with 55-200 repeats are known to cause a movement disorder based on elevated FMR1 mRNA levels and the related gain-of-function toxicity2. The clinical manifestation of FXTAS includes predominantly action and postural tremor, and cerebellar ataxia. Furthermore, rest and intention tremor, Parkinsonism, and non-motor features including cognitive impairment, peripheral neuropathy and autonomic symptoms may emerge to variable degree1. The penetrance of FXTAS was determined as 40% in male carriers over age 50 years and increases up to 75% at age 80 years3. Pharmacological tremor treatment showed limited efficacy using both first line medications, i.e. primidone or propranolol, and other second-line medications4. Deep brain stimulation was therefore considered in FXTAS with resistant tremor. To date, only few single cases with variable outcome of tremor and ataxia based on different surgical targeting approaches were reported5-9. As the tremor signal is generally propagated through the cerebello-thalamic pathway, the Vim and subthalamic fibre tracts can be considered plausible neurostimulation targets. Here, we report the long-term therapeutic outcomes of neurostimulation in a series of three subsequent FXTAS patients followed for up to 4 years. Methods Three genetically confirmed male FXTAS patients (Table 1) received DBS after medical treatment failure (Activa® PC pulse generator; Medtronic, Meerbusch, Germany). No sufficient treatment effect on tremor had been achieved with conventional medication therapy including propranolol, primidone and several further second-line medications in all three patients. A detailed clinical assessment was performed preoperatively during the regular DBS screening. All three patients were rescheduled at two months, at one year, and at two years from DBS surgery (FXTAS-3 not available at one year) in both ‘stimulation off’ (StimOff) and ‘stimulation on’ (StimOn) conditions. Two patients underwent the four year assessment (FXTAS-2, FXTAS-3). Clinical motor outcome was monitored with the Tremor Rating Scale (TRS) and International Co-operative Ataxia Rating Scale (ICARS). The tremor-related hand functional disability was assessed with the “Columbia University Assessment of Disability in Essential Tremor” (CADET-A, anamnestic part)10. We further evaluated the PDQ-39 quality of life, Mini-Mental Status Examination (MMSE) for cognitive functions, and Beck`s Depression Inventory (BDI). The perioperative procedure was free from complications. Electrode localization was confirmed by postoperative T1-weighted MR imaging and confirmed localization of the most caudal active electrode contacts in the bilateral Vim region (FXTAS-2, FXTAS-3), or the bilateral caudal border zone of Vim and subthalamic fibre tracts (FXTAS-1) (Table 1) as generally applied in tremor1113 . Patients FXTAS-1 and FXTAS-2 were available for kinematic gait analysis (APDM, Portland, USA) in both StimOff and StimOn at final assessment. Results At final assessment, all three patients reported overall subjective improvement when comparing StimOff and StimOn conditions under physician survey. All three patients revealed considerable and sustained tremor improvement (TRS) when comparing StimOff and StimOn conditions (Table 1), and the TRS in StimOn at final assessment was superior to the preoperative score in all three patients. Postoperatively, all three patients showed a gradual increase of tremor in consecutive StimOff assessments, presumably reflecting the underlying disease progression. Ataxia scores (ICARS) gradually worsened in StimOff over time and improved with StimOn throughout the whole observation period. This finding may in part reflect the sustained improvement of intention tremor. Additionally, at final assessment, we found a positive effect of Vim-DBS on gait based on kinematic gait measures in two patients (FXTAS-1, FXTAS-2). Gait analysis revealed improved step length, more regular gait cycles, and improved axial tremor around 3 Hz (Appendix 1). Preoperatively, hand functional disability was severe (CADET-A). All three patients reported a considerable improvement at two-month assessment, however functional disability worsened and reached the preoperative level within one to two years from surgery (Table 1). Outcome on quality of life was heterogeneous at final assessment compared to the preoperative state with one patient improved, one patient worsened and one patient similar (Appendix 2). Cognitive function according to the MMSE was stable in FXTAS-1, but worsened slightly in FXTAS-2 and FXTAS-3, presumably according to disease progression (Appendix 3). Nevertheless, patients and relatives confirmed preserved daily life functioning. BDI scores were generally normal, except FXTAS-2 who presented once with an elevated score of 28 (Appendix 4). Discussion We present a series of three consecutive FX-TAS patients treated with DBS of the Vim or subthalamic area and regular prospective long-term assessments up to four years. All patients showed sustained tremor improvement, which at final assessment still was superior to the preoperative state. We observed an additional improvement on the ICARS ataxia score, which presumably reflected improved upper extremity intention tremor and axial tremor during gait as confirmed by the kinematic gait analysis. Despite of this clear-cut formal motor improvement – however – improvements of daily life hand function were rather short-lived and reached the preoperative level of impairment already within one to two years after DBS surgery. Quality of life showed constant worsening in one patient (FXTAS-2), whereas FXTAS-1 showed stable improvements for two years, and FXTAS-3 exhibited stable quality of life over four years similar to the preoperative state. This might still be considered a treatment success in the light of the disease progression as was supported by the increasing TRS scores in StimOff over time in all three patients. Our data give a quite differentiated view on effects and limitations of neurostimulation therapy in FXTAS. When stratifying potential treatment success from DBS in FXTAS patients preoperatively, clinical counseling should in particular address the fine motor requirements of an individual patient and inform on the limited long-term fine-motor capabilities despite of a clear-cut formal tremor improvement as identified in all of our three patients. Moreover, quality of life might also depend on ataxia severity, and it should be kept in mind that the slight improvement in ataxia was mainly driven by reduced axial and intention tremor. Of note, no aggravation of pre-existing ataxia was observed in our patients. Another factor to consider carefully is the preoperative cognitive state, as a proportion of FXTAS patients may present with cognitive impairments up to dementia. Previous experience in DBS and FXTAS is very limited and encompasses few single case reports. As a common finding across individual reports tremor improvement was supported in most cases. In these reports, there was considerable variability of targeting and this included the unilateral Vim5, 6, unilateral posterior subthalamic area9, or unilateral thalamic Vim / ventralis oralis posterior border zone implantation with mild efficacy followed by thalamic ventralis oralis anterior / ventralis oralis posterior border zone implantation with superior efficacy in the same patient8. The effects on ataxia were less consistent with some reports showing unchanged gait ataxia6, 9, acute7 or delayed deterioration, the latter most likely along disease progression14, or improvement5 of gait ataxia. Previous work in essential tremor demonstrated that mild ataxia may improve at ‘optimal’ stimulation intensity, but worsens with ‘supratherapeutic’ stimulation15, 16. Our data support that gait ataxia was improved in all three patients from DBS, and our analyses support that this effect was mainly mirrored by reduced intention tremor, reduced axial tremor, and regularization of the gait cycle. In summary, previous data were based on few single case reports with considerable variability of both clinical outcome and surgical targeting. Our case series supports a role of neurostimulation of both Vim and cerebello-thalamic fibre tracts as effective and safe. Some of our findings are encouraging, and proper patient selection may help to achieve favorable treatment outcome. Therefore, our findings encourage clinical registers to characterize clinical outcomes of DBS in atypical tremor syndromes like FXTAS. Increasing evidence converges that genetic predictors may assist treatment stratification of personalized neurostimulation therapy in future17, 18. Author Roles Daniel Weiss 1A, B, C; 2A, B, C, 3A, B; Carina Mielke 1C, 2B, 2C, 3A, 3B; Tobias Wächter 1A, 1B, 1C, 3B; Benjamin Bender 1C, 2B, 2C, 3B; Rajka M. Liscic 2B, 2C, 3B; Marlieke Scholten 1C, 2A, 2B, 3B; Georgios Naros 1C, 3B; Christian Plewnia 1C, 2C, 3B; Alireza Gharabaghi 1A, 1C, 2C, 3B; Rejko Krüger 1A, 1B, 1C, 2C, 3A, 3B Conflict of interest Daniel Weiss is supported by a research grant of the German Research Council (DFG) WE5375/1-1. Daniel Weiss received speaker’s honoraria and a travel grant from Medtronic, and the Movement Disorder Society. Carina Mielke reports no conflict of interest. Tobias Wächter reports no conflict of interest. Benjamin Bender reports no conflict of interest. Rajka M. Liscic reports no conflict of interest. Marlieke Scholten reports no conflict of interest. Georgios Naros reports no conflict of interest. Christian Plewnia reports no conflict of interest. Alireza Gharabaghi reports no conflict of interest. Rejko Krüger has received research grants of the German Research Council (DFG; KR2119/3-2 and KR2119/8-1), the Michael J Fox Foundation, the Fritz Thyssen foundation (10.11.2.153), the Federal Ministry for Education and Research (BMBF; COURAGE-PD 01ED1406) and the Fonds National de Recherche (FNR; PEARL P13/6682797), as well as speakers honoraria from Medtronic GmbH, St Jude Medical and Abbvie. References 1. Berry-Kravis E, Goetz CG, Leehey MA, et al. Neuropathic features in fragile X premutation carriers. American journal of medical genetics Part A 2007;143A(1):19-26. 2. Jacquemont S, Hagerman RJ, Leehey M, et al. Fragile X premutation tremor/ataxia syndrome: molecular, clinical, and neuroimaging correlates. American journal of human genetics 2003;72(4):869-878. 3. Jacquemont S, Hagerman RJ, Leehey MA, et al. Penetrance of the fragile X-associated tremor/ataxia syndrome in a premutation carrier population. JAMA : the journal of the American Medical Association 2004;291(4):460-469. 4. Hall DA, Berry-Kravis E, Hagerman RJ, Hagerman PJ, Rice CD, Leehey MA. Symptomatic treatment in the fragile X-associated tremor/ataxia syndrome. Movement disorders : official journal of the Movement Disorder Society 2006;21(10):1741-1744. 5. Senova S, Jarraya B, Iwamuro H, et al. Unilateral thalamic stimulation safely improved fragile X-associated tremor ataxia: a case report. Movement disorders : official journal of the Movement Disorder Society 2012;27(6):797-799. 6. Xie T, Goodman R, Browner N, et al. Treatment of fragile X-associated tremor/ataxia syndrome with unilateral deep brain stimulation. Movement disorders : official journal of the Movement Disorder Society 2012;27(6):799-800. 7. Peters N, Kamm C, Asmus F, et al. Intrafamilial variability in fragile X-associated tremor/ataxia syndrome. Movement disorders : official journal of the Movement Disorder Society 2006;21(1):98102. 8. Oyama G, Thompson A, Foote KD, et al. Deep brain stimulation for tremor associated with underlying ataxia syndromes: a case series and discussion of issues. Tremor and other hyperkinetic movements 2014;4:228. 9. Oyama G, Umemura A, Shimo Y, et al. Posterior Subthalamic Area Deep Brain Stimulation for Fragile X-Associated Tremor/Ataxia Syndrome. Neuromodulation : journal of the International Neuromodulation Society 2014. 10. Wendt KJ, Albert SM, Pullman SL, Schneier FR, Louis ED. Columbia University Assessment of Disability in Essential Tremor (CADET): methodological issues in essential tremor research. Parkinsonism & related disorders 2000;6(1):17-23. 11. Barbe MT, Liebhart L, Runge M, et al. Deep brain stimulation of the ventral intermediate nucleus in patients with essential tremor: stimulation below intercommissural line is more efficient but equally effective as stimulation above. Experimental neurology 2011;230(1):131-137. 12. Plaha P, Patel NK, Gill SS. Stimulation of the subthalamic region for essential tremor. Journal of neurosurgery 2004;101(1):48-54. 13. Herzog J, Hamel W, Wenzelburger R, et al. Kinematic analysis of thalamic versus subthalamic neurostimulation in postural and intention tremor. Brain : a journal of neurology 2007;130(Pt 6):1608-1625. 14. Ferrara JM, Adam OR, Ondo WG. Treatment of fragile-X-associated tremor/ataxia syndrome with deep brain stimulation. Movement disorders : official journal of the Movement Disorder Society 2009;24(1):149-151. 15. Fasano A, Herzog J, Raethjen J, et al. Gait ataxia in essential tremor is differentially modulated by thalamic stimulation. Brain : a journal of neurology 2010;133(Pt 12):3635-3648. 16. Groppa S, Herzog J, Falk D, Riedel C, Deuschl G, Volkmann J. Physiological and anatomical decomposition of subthalamic neurostimulation effects in essential tremor. Brain : a journal of neurology 2014;137(Pt 1):109-121. 17. Weiss D, Brockmann K, Srulijes K, et al. Long-term follow-up of subthalamic nucleus stimulation in glucocerebrosidase-associated Parkinson's disease. Journal of neurology 2012;259(9):1970-1972. 18. Angeli A, Mencacci NE, Duran R, et al. Genotype and phenotype in Parkinson's disease: lessons in heterogeneity from deep brain stimulation. Movement disorders : official journal of the Movement Disorder Society 2013;28(10):1370-1375.