149 KB - Department of Health, Social Services and Public Safety
advertisement

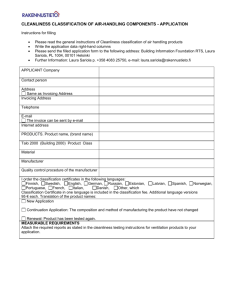
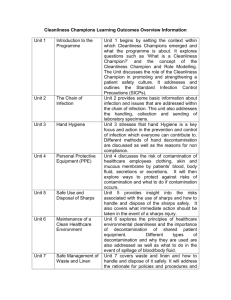
POLICY FOR THE PROVISION AND MANAGEMENT OF CLEANING SERVICES 15 January 2015 1 List of Contents Foreword Executive Summary SECTION 1 – Introduction and Background Strategic Context Aims Scope Key Principles Equality Screening SECTION 2 – Developments since 2005 Strategy Impact and Implementation of the Cleanliness Matters Strategy Other Departmental Initiatives Recent Developments NHS Initiatives Regional Healthcare Hygiene and Cleanliness Audit Tool SECTION 3 – The Way Forward Finance and General Management Audit Approach Elements to be Assessed Training Design and Other Issues Multi Disciplinary Working Colour coding Hospital Cleaning Equipment Sharing Best Practice Association of Healthcare Cleaning Professionals SECTION 4 – Appendices Appendix 1 – Reference List Appendix 2 – EQIA Screening Template Appendix 3 – GLOSSARY Page 3 4 5 6 9 9 10 12 13 14 14 17 18 19 23 24 27 27 31 32 32 32 33 33 34 35 37 47 Alternative Formats Consideration will be given to any request to make this document available, in alternative formats - Braille, audio, large print, computer disk or as a PDF document. The Department will consider requests to produce this document in other languages. If the document is required in these or other formats please contact Investment Directorate: Phone: 028 9052 3246 Text Phone: 028 9052 7668 Fax: 028 9052 2500 Email: investment.directorate@dhsspsni.gov.uk Post: Investment Directorate DHSSPS Room D1.4 Castle Buildings Belfast BT4 3SQ 2 Policy for the Provision and Management of Cleaning Services Foreword This policy sets out Policy for the Provision and Management of Cleaning Services in the Health and Social Care Sector. The policy is a reinforcement and clarification of previous policy and entails adopting a risk based approach using National guidelines prepared by the National Patient Safety Agency and a Publicly Available Specification (PAS 5748) issued in 2011 by the British Standards Institution and sponsored by the Department of Health. This reflects discussions with cleaning service providers which suggests that, whilst it is important that Trusts locally produce a cleaning frequency schedule, a single regional version is inappropriate since it cannot meet every organisation’s needs. The precise allocation of resources, and the actual frequency of cleaning, will therefore vary according to locally determined need. The logistics of this are an operational matter for each Trust, but the expectation is that HSC Managers will carry out annual risk assessments and that these will then receive approval at Board level as part of an annual self assessment exercise. This complements and strengthens the main themes of the policy: provision of rigorous programme of auditing to monitor standards of cleanliness; and, corporate governance systems and procedures, to ensure that clear accountability and management arrangements flow down from HSC Trust Boards. I am aware that PAS 5748 is currently being updated and Departmental officials have been part of the consultation process. Once this has been updated, it will be reviewed and promulgated to HSC bodies in due course. I would like to acknowledge the contributions made by, and also to thank, the interested groups and individuals who have helped to inform and shape this Policy. It has benefited greatly from the outcomes of the public consultation and I know that there will continue to be ongoing engagement with key stakeholders as the Action Plan is rolled out. Jim Wells MLA Minister of Health, Social Services & Public Safety 3 Policy for the Provision and Management of Cleaning Services Executive Summary This policy sets out the Department’s commitment to maintaining and improving environmental cleanliness in Northern Ireland (NI). It has been developed with the aim that best management practice, staff training and continued monitoring of performance will lead to services being maintained and improved in a challenging financial climate. The detail of the policy is presented in the three sections which follow this executive summary. Section 1 – Introduction and Background. This section sets out the aims, objectives and scope of the policy. It also sets out the key principles which should apply to cleaning services. Section 2 – Developments since the launch of Cleanliness Matters Strategy in October 2005. This outlines events and progress since 2005 and indicates how these are shaping the proposed strategic direction. Section 3 – The Way Forward. This section sets out the areas for attention over the coming years. Section 4 – Appendices. 4 Section One Introduction and Background 5 Introduction 1.1 Cleanliness is an integral part of healthcare services both in terms of safe treatment and quality of the environment. While there have been continuing issues with healthcare associated Infections (HCAIs), recent statistics demonstrate significant reductions in the rates of MRSA and Clostridium difficile infections. It is important to maintain the focus on cleanliness in this context. 1.2 The thrust of this policy is: maintaining the momentum of the previous strategy; good management practice, and developing staff. However, the policy also reinforces work carried out by a Regional Hospital Hygiene and Cleanliness Group which developed a new set of standards and a self assessment audit tool for use by the HSC Trusts. 1.3 This document is primarily aimed at cleaning in hospitals, but the principles are also relevant to the provision of cleaning services to patients and clients in other health service facilities such as, mental health and community facilities. The policy should be considered in any context where people using the health service receive cleaning services. Strategic Context 1.4 Providing a clean, safe environment for healthcare is a key priority for Trusts, and is a core standard in “Standards for better health” (see Appendix 1 for link). Other publications such as “Towards cleaner hospitals and lower rates of infection” (see Appendix 1 for link) and “A Matron’s Charter: An action Plan for Cleaner Hospitals” (see Appendix 1 for link) have further emphasised this, and also recognise the role cleaning has in ensuring that the risk to patients from healthcare associated infections is reduced to a minimum. 6 1.5 In the NHS, the Clean Hospitals Programme (in 2000) led to a series of initiatives which aimed to improve the patient environment and standards of infection prevention and control. Given increasing public awareness and concern about healthcare associated infection (HCAI), cleanliness gained recognition as being a key element in the provision of safe and high quality care, as opposed to a support service. 1.6 In Northern Ireland, the requirement to market test support services was abolished in 2001 and there was gradual movement back to in-house provision of services. HSC bodies wished to promote the advantages of integrating domestic services into care teams. 1.7 In response to GB initiatives, in October 2005 the DHSSPS issued “Cleanliness Matters - A Regional Strategy for Improving the Standard of Environmental Cleanliness in HSS Trusts 2005-08” (see Appendix 1 for link). The Strategy was developed with a multi-disciplinary Environmental Cleanliness Consultative Reference Group, which was largely drawn from Health & Social Services (HSS) Trusts. 1.8 The Strategy was accompanied by the “Cleanliness Matters Toolkit -Practical Guidance for Assessment of Standards of Environmental Cleanliness in HSS Trusts” (The Toolkit), and an Environmental Cleanliness Controls Assurance Standard (see Appendix 1 for link). These two documents reflected the main themes of the Strategy: a rigorous programme of auditing to monitor standards of cleanliness; and, corporate governance systems and procedures to ensure that clear accountability and management arrangements flow down from Trusts’ Boards. 1.9 Hospital cleanliness continues to receive a high level of interest from the public; the media and politicians alike. Improving and sustaining levels of 7 environmental cleanliness in hospitals is important if the Health & Social Care sector is to retain public confidence, make a significant impact on reducing HCAIs and improve the overall quality of care and patient experience. 1.10 The Regulation and Quality Improvement Authority (RQIA) undertook a programme of unannounced hygiene inspections in hospitals, following the launch on 23 January 2008 of a package of new initiatives aimed at tackling HCAIs. 1.11 Significant reductions in MRSA and Clostridium difficile infections were highlighted, and examples of real improvement were provided in the RQIA reports. However, the RQIA reports also recorded areas of poor performance in some Trusts. 1.12 In November 2009, further work was undertaken to drive up hygiene and cleanliness standards in hospitals and other healthcare facilities. This was in response to the publication of several reports of unannounced inspections by RQIA which showed significant non-compliance and highlighted the need for improvement. 1.13 The Regulation & Quality Improvement Authority (RQIA) conducted an independent review which was commissioned by the Minister for Health, Social Services and Public Safety, following the serious outbreak and tragic deaths of babies from Pseudomonas. The final report was published on 31 May 2012 (see Appendix 1 for link) 1.14 The Interim report of the RQIA Independent Review of incidents of Pseudomonas aeruginosa infection in neonatal units in NI, was published on 31 March 2012. The report highlighted learning for all organisations involved and made 15 recommendations for action to the Minister for Health, Social Services and Public Safety. One of the recommendations related to cleaning of sinks and 8 taps. New standard guidance was developed for NI and issued on 31 May 2012 (see Appendix 1 for link). 1.15 During the second stage of this review, the governance arrangements and the effectiveness of communications in relation to the pseudomonas incidents were reviewed. Aims 1.16 The aims of the policy are as follows: To ensure high quality cleaning services are provided in a manner which meets all current best practice, regulations and legislation. To ensure that best use is made of available resources. To ensure staff receive training in order to help them perform as effectively as possible and to encourage personal development. To modify the audit arrangements introduced by the Strategy and Toolkit in 2005. To ensure that managers adopt the standards and tool developed by the Regional Hospital Hygiene and Cleanliness Group. To ensure that Trusts’ Boards continue to monitor the quality of provision of cleaning. Environmental cleanliness is a multi-disciplinary responsibility requiring Professionals from all disciplines to work together to achieve the highest standards of cleaning, hygiene, infection prevention / control and auditing. The logistics of this are an optional matter for each Trust. Scope 1.17 This policy applies to all staff. It applies particularly to all staff involved in the provision of services which improve environmental cleanliness, hygiene, infection 9 prevention / control and auditing or with responsibility for providing a clean and safe environment for patients and visitors. Key Principles 1.18 This document sets out the Department’s policy for the future development and delivery of cleaning services. The principles underpinning the development of this policy include: Quality 1.18.1 Trusts must continue to monitor cleanliness through implementation of appropriate audit and reporting procedures. Audit procedures should be reviewed and take account of local circumstances and the Regional Healthcare Hygiene and Cleanliness Tool (see Appendix 1 for link). Standards of environmental cleanliness should be maintained and improved in accordance with the goals and objectives set out in “Quality 2020 – A 10-Year Strategy to protect and improve quality in health and social care in Northern Ireland” (see Appendix 1 for link). 1.18.2 Trusts must deliver cleaning services to the standards set out in the Regional Hospital Hygiene and Cleanliness Standards and supporting standards (see Appendix 1 for link). Training 1.18.3 It is recognised that all staff associated with cleaning services must be competent and appropriately trained to a standard commensurate with their role and duties. An example of appropriate training for supervisors and basic grade cleaning staff is the Cleaning Professional Skills Suite (CPSS) of the British Institute of Cleaning Sciences (BICSc). Efficiency 10 1.18.4 Compliance with agreed standards of cleanliness, hygiene and auditing is an operational matter for each Trust. Trust Managers should implement best professional management practice and review cleaning frequencies, work schedules and budgets; this includes reviewing what is cleaned, how it is cleaned, how often it is cleaned and assessing risk. 1.18.5 Trusts must carry out an annual self-assessment of the management of cleaning services including a review of cleaning plans, resources and audit scores. Multi Disciplinary Working 1.18.6 Trust staff from different disciplines must work together to ensure the best possible standards of environmental cleanliness and hygiene. Governance and Accountability 1.18.7 Trusts should ensure that arrangements recommended in Cleanliness Matters, the Regional Healthcare Hygiene and Cleanliness Standards and the DHSSPS Environmental Cleanliness Controls Assurance Standard are maintained. These arrangements include: Definitions of roles, responsibilities and accountability. Reporting to Trusts’ Management Boards on performance. Creation of a multi-disciplinary group within each Trust which is charged with taking forward the local environmental cleanliness strategy. 1.18.8 The leading role of Ward Managers / Ward Sisters / Charge Nurses should be recognised, and authority over cleaning services at ward level should be delegated to an appropriate person within each facility who 11 should have the capacity to raise any cleanliness issues with the Cleaning Manager, and responsibility for appropriate escalation / risk management. Patient, Visitor and Staff Participation 1.18.9 Patients, visitors and staff must be involved in the planning, delivery and audit of cleaning services and Trusts must engage with patients, visitors and staff, and use regular surveys on the services provided. Equality Screening 1.19 Section 75 of the NI Act 1998 requires all public bodies in carrying out their functions relating to NI to have due regard to the need to promote equality of opportunity between: Persons of different religious belief, political opinion, racial group, age, marital status or sexual orientation; Men and women generally; Persons with a disability and persons without; and Persons with dependants and persons without. 1.20 In addition, without prejudice to the above, public bodies must also in carrying out their functions relating to NI, have regard to the desirability to promote good relations between persons of different religious beliefs, political opinion or racial group. 1.21 DHSSPS has carried out an initial screening of this policy and determined that a full Equality Impact Assessment is not required. A summary of the screening is contained in Appendix 2. If you consider that this decision is not correct please let us know why. Please provide details of any action(s) you need including any supporting evidence that you may have. 12 Section Two Developments since the issue of the Cleanliness Matters Strategy in October 2005 13 Impact and Implementation of the Cleanliness Matters Strategy 2.0 Cleanliness Matters and the associated controls assurance standard imposed significant new requirements; a rigorous audit regime and corporate governance procedures. Despite initial concerns by Trusts about the workload implications, the benefits were soon recognised. For example: Accountability requirements brought cleanliness to the attention of Trusts’ Boards and highlighted risk and funding issues. Audit processes clarified the respective responsibilities of nursing; estates and domestic services; facilitated cross-disciplinary working, and made it clear that cleanliness was not just a domestic services issue. The scoring process brought about a sharper focus on performance and associated issues, including estate condition. Trusts have reported that including estates conditions in the scoring process has been helpful in the speedier identification and rectification of estates issues. Other Departmental Initiatives 2.1 It is now accepted by Trusts that regular auditing is an essential element of maintaining and improving standards of cleanliness. Similarly, the governance aspects reflected in Cleanliness Matters and the Controls Assurance Standard are now embedded in the culture of health and social care bodies. 2.2 After the launch of Cleanliness Matters, the Department commissioned an independent assessment of environmental cleanliness which was carried out by KPMG in early 2006. This produced mixed results. One of the difficulties was that the basis of assessment was (and still) is, public perception of an element, as opposed to how well it has been cleaned. Consequently, in older hospitals, poor scores frequently reflected the age and condition of the estate as opposed to poor cleaning performance. It was also recognised that the design of older 14 buildings may make cleaning more difficult. A follow up audit by KPMG in late 2007 revealed a significant improvement, suggesting that Cleanliness Matters was having a positive impact. 2.3 The Ward Sisters’ Charter which was launched in October 2006, encouraged Ward Managers to take responsibility for ensuring that high standards of cleanliness are maintained. This was consistent with the principle in Cleanliness Matters, that cleanliness is everyone’s responsibility, not just the responsibility of the cleaners. 2.4 After the restoration of devolved government in 2007, healthcare associated infection (HCAI) became a major issue in healthcare and attracted continued media and MLA attention. While cleaning performance was generally not subject to criticism, the perceived association between HCAI and cleaning ensured that cleanliness standards remained a key issue. The Department produced HCAI action plans in 2006 and 2010 which acknowledged the role of environmental cleanliness but did not introduce significant new requirements on domestic services departments or change any of the principles or elements of Cleanliness Matters. 2.5 In particular, there was intensive media coverage of the outbreak of the Clostridium difficile (C diff) infection that occurred in Northern Health and Social Care Trust (NHSCT) hospitals between June 2007 and August 2008. The RQIA carried out an independent review of the outbreak, and in their final report, two of the recommendations (Rec. 7 and 14) are of relevance to this policy: Recommendation 7 -Consideration should be given to undertaking a baseline review of cleaning arrangements against current standards and methodologies. 15 Recommendation 14 -Trusts should review their ward environments to ensure that there is no impediment to safe, cleaner, tidier patient areas. The Public Inquiry, which was launched in 2009, was asked to establish how many deaths occurred in the Northern Health and Social Care Trust hospitals during the outbreak, for which C difficile was the underlying cause of death, or was a condition contributing to death. It was also asked to report on the experiences of patients and others who were affected directly by the outbreak. 2.6 The final report of the Public Inquiry into the Outbreak of Clostridium difficile in Northern Trust Hospitals, published in March 2011 (see Appendix 1 for link), made twelve main recommendations to help prevent and manage outbreaks. Environmental cleanliness has a strong part to play in contributing to the reduction of healthcare associated infections. 2.7 The outbreak of Pseudomonas in the Neonatal Unit at the Royal Jubilee Maternity Hospital in early 2012 also brought hygiene and cleanliness into sharper focus. Pseudomonas is a micro-organism that is found in many natural environments, including soil and water. There are many different types and strains of Pseudomonas and specialist tests are required to distinguish these. Pseudomonas can be found in sinks, taps and water systems and is difficult to eradicate completely and permanently. 2.8 The Interim report of the Independent Review of incidents of Pseudomonas aeruginosa infection in neonatal units in Northern Ireland was published in March 2012. One recommendation related to cleaning of sinks and taps, and new standard guidance was developed for NI. Further guidance in response to recommendations from the Troop Review, was issued on 31 May 2012 following the publication of the final report. 16 2.9 Guidance was developed to produce a new set of standards and audit tool for use in augmented care settings. This was piloted in Trusts in the late summer of 2012. Recent Developments 2.10 A Neonatal Infection Prevention and Control Audit Tool (from the Regional Infection Prevention and Control Audit Tools for Augmented Care Settings in Northern Ireland) has been launched (See Appendix 1 for link). This tool is applicable to all Neonatal Intensive care and special care baby units, and is based on existing documents from the DHSSPS; DH England; the British Association of Perinatal Medicine and a range of recognised research sources. The tool contains seven sections, each of which aims to consolidate existing guidance in order to improve and maintain a high standard in the quality and delivery of care and practice in neonatal care, to assist in the prevention and control of healthcare associated infections. 2.11 The introduction of unannounced hygiene and cleanliness inspections by RQIA was part of a package of measures to combat HCAI, which was announced in January 2008. In November 2009, publication of the third tranche of these reports generated intense media coverage and an Assembly debate. This led to the formation of the Regional Healthcare Hygiene and Cleanliness Reference Group, comprising representation from a wide range of stakeholders, which was charged with developing new hygiene and cleanliness standards and an accompanying audit tool. This audit tool has been implemented regionally, and has had a significant impact on the audit strand of the strategy. It is also being used for routine cleanliness audits. 2.12 In 2008, the Department commissioned specialist support services consultants FM Specific -, to review cleaning services in a sample of acute hospitals. The two main objectives were: 17 To compare the resources currently employed in acute hospitals, with the estimated resources needed to meet the input standards (cleaning frequencies) recommended for the NHS. To assess the scope for improved efficiency, effectiveness and economy within the current service delivery models. 2.13 The report concluded that: Additional resources would be needed to bring them up to the NHS recommended frequencies. There was a need to carry out a fundamental re-calculation of cleaning hours and budgets, and to develop cleaning plans in order to put service delivery models on a sound base. Since then, the NHS has shifted the emphasis away from recommended frequencies, and moved towards cleaning frequencies based on local risk assessment. Trusts should review their risk weighting; cleaning frequencies; cleaning budgets and allocation of funding across the functional areas. Attention to cleanliness is part of the holistic approach to maintaining quality of safety and care. In light of ongoing competing budgetary priorities, the Department continues to deliver significant investment in infrastructure and Maintaining Existing Services (MES) through the management of its capital programme. NHS Initiatives 2.14 In June 2011, the British Standards Institution sponsored by the Department of Health and the National Patient Safety Agency issued a Publicly Available Specification “PAS 5748: 2011 – Specification for the planning, application and measurement of cleanliness in hospitals” (see Appendix 1 for link). The Steering 18 Group which contributed to the development of the specification included the Association of Healthcare Cleaning Professionals, the British Institute of Cleaning Science and the Infection Prevention Society. 2.15 The specification set out requirements for the provision of cleanliness. These requirements include: responsibilities and accountabilities; risk assessment; management of cleaning tasks; auditing and reporting. To a large extent, it brought together existing good practice. The PAS builds on the experience and content of “The national specifications for cleanliness in the NHS (HSC),” the most recent version of which was published in April 2007. 2.16 The PAS is expected to be used in conjunction with The Revised Healthcare Cleaning Manual (see Appendix 1 for link), published by the National Patient Safety Agency in May 2009. It is also consistent with BS EN 13549:2001 (see Appendix 1 for link), Cleaning Services – Basic requirements and recommendations for quality measuring systems. REGIONAL HEALTHCARE HYGIENE AND CLEANLINESS STANDARDS AND TOOL 2.17 Work was carried out between 2009 and 2011 to develop: Hygiene and cleanliness standards for hospitals which are clear and evidence based. A regional tool for use by the HSC and the RQIA to provide a consistent measure. The purpose of the regional tool is to help to improve the monitoring of the quality of the service provided against those standards. 19 Background 2.18 The RQIA undertook a programme of unannounced hygiene inspections in hospitals following the launch on 23 January 2008 of a package of new initiatives aimed at tackling Healthcare Associated Infections. 2.19 In November 2009, further work was undertaken to drive up hygiene and cleanliness standards in hospitals and other healthcare facilities. This was in response to the publication of several reports of unannounced inspections by RQIA, which showed a great deal of non-compliance. These had been publicised in the media in a very adverse manner, with many headlines such as ‘dirty hospitals’, which had the potential to damage public confidence. 2.20 The progress made until then by Trusts, was acknowledged in relation to hygiene and cleanliness. Significant reductions in MRSA and Clostridium difficile infections were highlighted and examples of real improvement were provided in the RQIA reports. However, the RQIA reports also recorded areas of poor performance in some Trusts, which undermined both public confidence in the cleanliness of healthcare facilities and the morale of front-line staff working in those facilities. Development Work on New Standards and Tool 2.21 In 2010, a multi-disciplinary Regional Hospital Hygiene and Cleanliness Group, led by the Director of Nursing, and comprising representatives of the HSC Board; the Trusts and the Department, was set up to develop the new standards and regional tool. The standards were to be clear, unambiguous and consistent across the HSC. A regional tool was developed to replace the range of diverse tools which had been used across the HSC and the RQIA, sometimes resulting in different assessments for the same building. 20 2.22 In developing the revised standards and regional tool, the Group examined a number of - hygiene and cleanliness documents which have evolved over a number of years, and have been produced by a range of different individuals and organisations. One key aim was to reduce the incidence of healthcare associated infections through improved hygiene and cleanliness (in addition to other measures in place to reduce HCAIs). 2.23 The revised standards were intended to assess the general cleanliness and state of repair of healthcare facilities, as would be observed by patients, visitors and members of the public. The standards provided a common set of overarching hygiene and cleanliness standards for all hospitals and other healthcare facilities in Northern Ireland. 2.24 All Trusts were asked to assure themselves, at Trust board level, that they were compliant with the revised standards, and RQIA hygiene inspections would be carried out on the basis of these standards. 2.25 An audit tool explicitly linked to these standards for healthcare hygiene and cleanliness was developed for use by Trusts (for self-assessment) and by RQIA (for inspection). This work was taken forward by RQIA in conjunction with Trusts and DHSSPS. The audit tool was successfully piloted by RQIA in conjunction with the Trusts prior to its adoption throughout HSC and the commencement of any future RQIA hygiene inspection programme. 2.26 The Regional Healthcare Hygiene and Cleanliness Standards and Audit Tool was approved by the Health Minister on 7 July 2011, and is now being used during hygiene and cleanliness inspections by RQIA. The standards incorporate the critical areas which were identified through a review of existing standards, guidance and audit tools. They are used to assess healthcare hygiene; general cleanliness and state of repair of healthcare facilities, and aspects of infection 21 prevention and control - not only from a professional perspective, but also as would be observed, by patients, visitors and members of the public. 2.27 A great deal of work has already been carried out by Trusts to improve compliance scores in RQIA inspections, and it is important that this improvement is sustained in the future. Trusts already have audit processes in place for environmental cleanliness based on the Cleanliness Matters Strategy. The Regional Tool should be used to complement those procedures. 2.28 In using the common set of overarching hygiene and cleanliness standards, all organisations should assure themselves at Board level, that they are compliant with the standards. In seeking that assurance, the RQIA inspection reports are a matter not only of great public interest, but can also highlight issues which could indicate serious risks to public health. The RQIA reports will continue to be subject to a high level of scrutiny. 22 Section Three The Way Forward 23 The Way Forward Introduction 3.0 The way forward has been considered under the following headings, which are dealt with in turn: Financial and General Management Audit Approach Training Design and Other Issues Multi Disciplinary Working Colour Coding Hospital Cleaning Material and Equipment Sharing Best Practice Association of Healthcare Cleaning Professionals Finance and General Management 3.1 It is essential that Trusts make best use of resources by adopting good management practice for cleaning services. 3.2 The guideline NHS cleaning frequencies were the basis of an assessment of the adequacy of cleaning resources in acute hospitals in the HSC commissioned by DHSSPS in 2008 from FM Specific. In the NHS Specification these frequencies, which were a minimum for each element to be cleaned and varied according to the risk category of the area, are no longer regarded as the blueprint for the input required. NHS policy now states that cleaning frequencies for each element to be cleaned and each functional area should be determined locally based on risk. 3.3 A Publicly Available Specification (PAS 5748) (see Appendix 1 for link) was issued in 2011 by the British Standards Institution and sponsored by the Department of Health. PAS 5748 places a greater emphasis on a detailed risk 24 assessment methodology, which gives an equal weighting to the risks from both healthcare associated infection and public confidence - for example, public entrances might be very high risk from a public perception standpoint. It places less emphasis on cleaning frequencies which were a strong feature of Cleanliness Matters in 2005. The principles of risk management should be applied by Trusts when reviewing how often elements and locations are cleaned. 3.4 FM Specific recommended development of cleaning plans based on a fundamental review of the cleaning hours required. This should result in a revised budget and allocation of resources. Given that budgets may not have been fundamentally reviewed since compulsory competitive tendering, it is important that there is a budget build-up process which reflects the way healthcare is provided in the 21st century. This process will help to ensure that resources are allocated in accordance with local risks and priorities. 3.5 PAS 5748 specifies requirements for: Governance of cleanliness services Assessing the risk of a poor standard of cleanliness, both for infection and damage to patient; public or staff confidence Providing cleaning tasks Measuring cleanliness on the basis of visual inspection – including setting agreed performance levels Taking corrective action Conducting performance analysis and implementing improvement actions Providing a continuous service improvement plan Reporting cleanliness outcomes. 3.6 The specification also set out the basic management process for a fundamental review- from identification of items to be cleaned through to cleaning responsibilities, risk assessment, cleaning frequencies, method statements, and 25 work schedules. The FM Specific Cleaning Plan methodology includes much of the above and trusts should go through the process of fundamentally reviewing the service provided. 3.7 PAS 5748 should be regarded as good management practice for the HSC. Managers should review their service in the context of the principles in this document. The NHS Manual for Cleaning, which is to be revised by the Association of Healthcare Cleaning Professionals, contains operational detail of which managers should be aware. This policy will highlight areas to which managers need to pay attention. 3.8 In 2007 the National Patient Safety Agency issued guidance on standards of cleaning in hospitals. This guidance sets out the specifications for cleanliness in the NHS. These have been designed to provide a simple, easy-to-apply methodology within which hospitals in England can assess the effectiveness of their cleaning services. The specifications apply chiefly to ‘traditional’ hospitals – whether in the acute, mental health or primary care trust communities – but their principles apply equally to other settings. 3.9 They describe a comparative framework within which hospitals and trusts in England can set out details for providing cleaning services and assessing ‘technical’ cleanliness. 3.10 They give clear advice and guidance on: what is required; how trusts can demonstrate the way(s) in which cleaning services will meet these requirements; and how to assess performance. 26 3.11 HSC Trusts should make use of both PAS 5748 2011 and NPSA 2007 and develop a strategic cleaning plan which should enable identification of gaps between best practice and current capacity, match available resources to a risk based assessment and, demonstrate that sufficient resources have been allocated to meet local need. 3.12 The Cleaning Reviews also revealed some potential for revenue savings from investment in equipment. Examples included the use of ‘ride on’ mechanical cleaners to clean corridors etc. Trusts should consider where modest investment could produce revenue savings. Audit Approach 3.13 The audit requirements were the most significant change introduced by Cleanliness Matters. While Trusts now agree that a regular programme of self assessed audit is essential to maintain standards, the mechanisms require finetuning. 3.14 In line with latest NHS policy, flexibility is permitted to take account of local circumstances. Local circumstances and assessed risk may include giving more attention to areas which are performing badly, or less attention to those which are performing well. Strong local management and control procedures may justify a reduction in audit frequencies. However, the following should be regarded as good practice and policy reflecting audit frequencies. Elements to be Assessed 3.15 The Regional Hygiene and Reference Group drafted a new set of cleanliness and hygiene standards and an accompanying audit tool (the Regional Audit Tool). The elements in the Regional Audit Tool are broadly similar but not identical, to the 49 elements set out in Cleanliness Matters. The Cleanliness Matters Toolkit is used to assess 49 defined elements to be cleaned and Trusts 27 take a view internally, as to which discipline is responsible for the element. In contrast, the Regional Hospital Hygiene & Cleanliness Tool is used to assess a number of hygiene issues as well as cleaning. Therefore, in taking forward audits Trusts should: o recognise that it is unlikely that all functional areas can be reviewed annually. Trusts should aim to cover all very high risk and high risk areas. o develop policies/procedures for managerial audits which include frequency of reviews, sample sizes and team composition. o have a policy/procedure for what the NHS Specification describes as Board Assurance Visits. These were introduced locally in December 2009, when Trust Chief Executives and / or senior officials were asked to walk the wards at least every month to observe hygiene and cleanliness levels. This is a less formal process than managerial audits. Basis of Departmental Audit Assessment 3.16 Environmental cleanliness is a multi-disciplinary responsibility requiring Professionals from all disciplines to work together to achieve the highest standards of cleaning; hygiene; infection prevention / control and auditing. 3.17 The Regional Audit Tool is not focussed exclusively on the regular departmental audits which were introduced by Cleanliness Matters and are still regarded as best practice in the NHS. However, the cleanliness aspects of the Regional Audit Tool will be complemented by the current departmental/technical audits which are based on the Cleanliness Matters Toolkit 2005. Therefore, in broad terms the departmental audit approach introduced by Cleanliness Matters is retained with Departmental Audits as set out in Cleanliness Matters remaining the basis of assurance for Controls Assurance purposes. 28 3.18 Responsibility for ensuring that the Departmental audit is undertaken rests with the head of department being audited (e.g. ward manager /officer in charge) who should preferably lead the audit or delegate the responsibility to a senior member of staff .By leading the audit, the Head of department has key ownership in ensuring that the necessary level of Environmental Cleanliness Standards are achieved and maintained. 3.19 To highlight that otherwise good cleaning performance, may be thwarted by poor estates condition, the basis of assessment should be capable of excluding problems which reflect estate condition. However, whilst this disaggregation may be useful to allow cleaning performance to be benchmarked across different areas, the scores should not be disaggregated for the purposes of control assurance and Estates scores should be retained to aid performance management of that function. 3.20 Trusts have reported that including estate items has been helpful in the speedier identification and rectification of estates issues. Therefore, the basis of assessment should be able to mirror the NHS approach which is that “an element shall be identified as clean if all parts of the element have the visual appearance of being free of dirt and stains.” Dirt and stains are defined in some detail. 3.21 As a consequence of removing estate condition issues, the acceptable level of cleanliness in Departmental Audits which was set at 85% in Cleanliness Matters is increased to 90% though Trusts may of course set higher internal standards. Managerial audits 3.22 The purpose of managerial audits is to: Validate the results of departmental audits. Take a more multi-disciplinary perspective of the patient environment. 29 3.23 Unlike the NHS Specification, Cleanliness Matters offered detailed guidance on managerial audits. While much of this guidance was sound, some improvements were necessary: The Cleanliness Matters Audit Tool (2005-2008) as updated and developed by Trusts should continue to be used as the basis for departmental audits. The more comprehensive Regional Healthcare Hygiene Audit Tool should be used as a Managerial Audit Tool or, more frequently, as the departmental audit tool if serious risks have been identified. This is consistent with the existing managerial audit guidance which requires a multi-disciplinary audit team. Corrective Action 3.24 Corrective action is what should be done when shortfalls are revealed during audits. Under existing guidance, there is a danger that departmental audits will reveal problems but no remedial action will follow. 3.25 Corrective action may include: Assigning responsibility for remedying each defect and ensuring that action is taken within appropriate timescales. Re-auditing the area or the element(s). If there is no improvement, examining the reasons. Reviewing work schedules. Reporting problems to higher levels of management (escalation). Increasing cleaning frequencies. Training. 30 3.26 Trusts should draw up policies for the corrective actions to be taken following shortfalls revealed during audits. These may vary according to risk category of the area and element being audited. Training 3.27 The Workforce Learning Strategy (see Appendix 1 for link) for Northern Ireland Health and Social Care Services 2009-2014 aims to: Equip staff with the skills and knowledge to work effectively. Support staff in developing and realising their potential. Promote a culture of lifetime learning. 3.28 It has been shown that investment in training may not only enable staff to carry out their normal duties more effectively but also produce substantial benefits in terms of self esteem and motivation. 3.29 Cleanliness Matters referred to the need for human resources strategies for both cleaning staff and managers. All Trusts have now agreed that basic grade staff and supervisors should have the opportunity to obtain a minimum level of qualifications. The industry recognised standard qualification is the Cleaning Professionals Skills Suite (CPSS), which is accredited by the British Institute of Cleaning Science (BICS) (see Appendix 1 for link). This requires approximately sixteen hours of training by in-house accredited staff. All Trusts now have a BICSc accredited training centre. 3.30 Although BICS CPSS (see Appendix 1 for link) is a cost effective method of providing training, given the numbers of staff to be trained, Trusts will have to plan carefully to achieve this objective. While the financial outlay is modest, cover for staff undergoing training may present a challenge. 31 3.31 Staff should have appropriate training in: basic cleaning techniques; customer service; health and safety; control of substances hazardous to health (COSHH); manual handling and infection prevention and control. 3.32 With regard to training of managers, many of the skills needed relate to general management and can be taught in-house, with specialist cleaning skills and cleaning science procured externally as necessary. Design and Other Issues 3.33 Buildings designers, facilities planners and domestic services managers should co-operate to ensure that new buildings take account of “cleanability.” This includes considering accessibility of items to be cleaned; designing buildings to minimise cleaning required and selection of materials which will be easy to clean. Multi Disciplinary Working 3.34 In January 2010, DHSSPS issued “Changing the Culture 2010: Strategic action plan for the prevention and control of healthcare-associated infections in Northern Ireland” (see Appendix 1 for link). Whilst the focus of the document was on HCAIs, it recognised that infection control and prevention was an integral part of everyone’s responsibility. Environmental cleanliness has an important role to play in inflection prevention and control and it is also everyone’s responsibility. Therefore it is important that a multi disciplinary approach is applied to the management of cleaning. Colour Coding Hospital Cleaning Material and Equipment 3.35 Many sites in the HSC already have a colour coding scheme in place but there is a lack of consistency with colours having different meanings on different sites. Where it is not already in place, Trusts should standardise a common colour coding scheme to reduce the risk of possible cross contamination. 32 3.36 The National Reporting and Learning Service (NRLS) developed a National Colour Coding Scheme for cleaning materials, set out in this document. It was designed to standardise, and streamline, existing schemes. Adopting the code improves the safety of hospital cleaning, ensure consistency and provide clarity for staff. A Safer Practice Notice is available and outlines the scheme (see Appendix 1 for link). Sharing Best Practice 3.37 There are many examples of best practice across the HSC and pilot exercises are also in place to help develop new ways of working. 3.38 The Regional Support Services Steering Group is a forum through which patient environment issues can be raised and best practice can be shared. It comprises representatives from five HSC Trusts and DHSSPS representatives from Health Estates Investment Group. It meets four times a year. However, the sharing of best practice should be carried out continuously throughout the year via other methods of communication and appropriate Trust meetings. Association of Healthcare Cleaning Professionals 3.39 The establishment of a local branch of the Association of Healthcare Cleaning Professionals (AHCP) in NI represents a very positive step. It helps to provide a regional forum for the exchange, sharing and promotion of best practice. It also allows members to set local issues in regional and national contexts. It is important that Trust managers continue to support and encourage staff to attend the regular meetings and sharing of good practice. 33 SECTION FOUR APPENDICES 34 Appendix 1 Standards for Better Health, http://www.dh.gov.uk/prod_consum_dh/groups/dh_digitalassets/@dh/@en/documents/digitalasset/dh _4132991.pdf Towards cleaner hospitals and lower rates of infection http://www.dh.gov.uk/prod_consum_dh/groups/dh_digitalassets/@dh/@en/documents/digitalasset/dh _4085861.pdf A Matron’s Charter: An Action Plan for Cleaner Hospitals http://www.dh.gov.uk/en/Publicationsandstatistics/Publications/PublicationsPolicyAndGuidance/DH_4 091506 Cleanliness Matters – A Regional Strategy for Improving the Standard http://www.dhsspsni.gov.uk/cleanliness-matters-strategy-2005.pdf Cleanliness Matters Toolkit – Practical Guidance for Assessment of Standards of Environmental Cleanliness in HSS Trusts http://www.dhsspsni.gov.uk/index/hss/governance/governance-controls.htm Independent review of incidents of pseudomonas aeruginosa infections in neonatal units in Northern Ireland – RQIA Final Report http://www.rqia.org.uk/cms_resources/Pseudomonas%20Review%20Phase%20II%20Final%20Repo rt.pdf Guidance on cleaning sinks/basins and taps in clinical settings – including augmented care settings/neonatal units www.dhsspsni.gov.uk/sub-611-2012-policy-cleaning-services.doc Regional Healthcare Hygiene and Cleanliness Tool - RQIA http://www.rqia.org.uk/cms_resources/RHHC%20Audit%20Tool%20072011.pdf Quality 2020 – A 10-Year Strategy to protect and improve quality in health and social care in Northern Ireland http://www.dhsspsni.gov.uk/quality2020.pdf Regional Healthcare Hygiene and Cleanliness Standards - RQIA http://www.rqia.org.uk/cms_resources/SUB%201137%202011%20%20Regional%20Healthcare%20 Hygiene%20and%20Cleanliness%20Standards%20-%20Jun%202011.pdf The Public Inquiry into the Outbreak of Clostridium Difficile in the Northern Trust Hospitals Northern Ireland http://www.cdiffinquiry.org/inquiry-report.htm A Neonatal Infection Prevention and Control Audit Tool http://www.rqia.org.uk/cms_resources/Reg%20IPC%20Audit%20Tool_Sec%203_Neonatal_%20DHS SPS.pdf 35 The Revised Healthcare Cleaning Manual http://nrls.npsa.nhs.uk/EasySiteWeb/getresource.axd?AssetID=61814&type=full&servicetype=Attach ment BS EN 13549:2001 http://shop.bsigroup.com/ProductDetail/?pid=000000000030012952 PAS 5748:2011 - Specification for the planning, application and measurement of cleanliness services in hospitals http://shop.bsigroup.com/en/ProductDetail/?pid=000000000030208877 Workforce Learning Strategy http://www.dhsspsni.gov.uk/workforce-learning-strategy-apr-2009.pdf British Institute of Cleaning Science, http://www.bics.org.uk/ Cleaning Professionals Skill Suite http://www.bics.org.uk/files/download/Cleaning-Professional-Skills-Suite-13.pdf Changing the Culture 2010: Strategic action plan for the prevention and control of healthcare associated infections in Northern Ireland http://www.dhsspsni.gov.uk/changing_the_culture.pdf National Colour Coding Scheme – Safer Practice Notice http://www.nrls.npsa.nhs.uk/EasySiteWeb/getresource.axd?AssetID=60086& 36 Appendix 2 SCREENING TEMPLATE See Guidance Notes for further information on the ‘why’ ‘what’ ‘when’ and ‘who’ in relation to screening. For background information on the relevant legislation and for help in answering the questions on this template (follow the links). For further help contact Evaluation, Equality and Human Rights Branch at ext. 20539 (1) INFORMATION ABOUT THE POLICY/DECISION 1.1 Title of policy/decision Policy for the Provision & Management of HSC Cleaning Services 2012-2016 1.2 Description of policy/decision what is it trying to achieve? (aims/objectives) how will this be achieved? (key elements) what are the key constraints? (e.g. financial, legislative) The aims of the strategy are as follows: The provision of high quality cleaning services is important and it is vital that standards are met and maintained. Cleaning services must be provided in a manner which meets all current best practice, regulations and legislation. To ensure that best use is made of available resources. To ensure staff receive training in order to help them perform as effectively as possible and encourage personal development. To modify the audit arrangements introduced by Strategy and Toolkit in 2005. To encourage managers to adopt best practice developed for the NHS contained in the Specification for Cleanliness in Hospitals and the NHS Cleaning Manual. To ensure that Trusts’ Boards continue to monitor the quality of provision of cleaning. The aims will be achieved by ensuring that cleaning services are delivered in accordance with the Regional Hospital Hygiene and Cleanliness Standards. This will be supported by a hierarchy of audits using the Regional Hospital Hygiene and Cleanliness Audit Tool. This will also be supported by a programme of announced and unannounced inspections by the Regional Quality & Improvement Agency. Key constraints are primarily financial as there are increasing pressures on a limited cleaning budget as the demand for discharge cleans etc increases. 1.3 Main stakeholders affected (E.g. staff, actual or potential service users, other public sector organisations, voluntary and community groups, trade unions/professional organisations or private sector organisations) The main stakeholders are patients, visitors and HSC staff. 1.4 Other policies/decisions with a bearing on this policy/decision what are they? who owns them? Infection control procedures will need to work together with and in support of this strategy. Infection control staff within each site should work 37closely with colleagues in cleaning services to improve hygiene and cleanliness. 2) SCREENING THE POLICY/DECISION 2.1 In terms of groupings under Section 75, what is the make up of those affected by the policy/decision? Group Please provide details Gender Both genders are affected. It is widely accepted and Workforce Monitoring would confirm that the majority of HSC staff in each of the Trusts is female. It is also acknowledged that the majority of cleaning staff is female. It is further accepted that women live longer than men therefore this could impact on more women using HSC facilities. However, the policy aims to improve cleaning services for all patients, visitors and staff members regardless of gender. All ages are affected. It is widely accepted that hospital admission tends to increase with age. However, the policy aims to improve environmental cleanliness for everyone who attends hospital. All religions are affected. It is accepted that there is significant differences in the religious backgrounds of patients, visitors and staff in different Trusts throughout the region. However, the policy aims to improve environmental cleanliness for everyone People of all political opinions are affected. It is accepted that there is likely to be significant differences in the political opinions of patients, visitors and staff in different Trusts throughout the region. However, the policy aims to improve environmental cleanliness for all patients, visitors and staff regardless of political opinion. There is no data available which suggests any obvious positive or negative impact in terms of marital status, the policy aims to improve environmental cleanliness for all patients, staff and visitors regardless of marital status. It is accepted that the majority of HSC staff in each of the Trusts is female, it is further accepted that most carers are female. However, the policy aims to improve environmental cleanliness for all patients, visitors and staff members regardless of whether or not they have dependents. It is widely accepted that hospital admission tends to increase with disability. However, the policy aims to improve environmental cleanliness for all patients, visitors and staff members regardless of whether or not they have any disability. All ethnic backgrounds are affected. It is accepted that there is significant differences in the ethnic backgrounds of patients, visitors and staff in different Trusts throughout the region. However, the policy aims to improve environmental cleanliness for all patients, visitors and staff members regardless of ethnicity. There is no data available which suggests any obvious positive or negative difference between persons of different sexual orientation, the policy aims to improve environmental cleanliness for all patients and visitors regardless of sexual orientation. Age Religion Political Opinion Marital Status Dependent Status Disability Ethnicity Sexual Orientation 38 2.2 Is there any indication or evidence of higher or lower participation or uptake by different groups? Group Yes/No/ Please provide details Don’t Know Gender No Age No Religion No Political No Opinion Marital No Status Dependent No Status Disability No Ethnicity No Sexual No Orientation 2.3 Is there any indication or evidence that different groups have different needs, experiences, issues and priorities in relation to the policy/decision? Group Yes/No/ Please provide details Don’t Know Gender No Age No Religion No Political No Opinion Marital No Status 39 No Dependent Status Disability No Ethnicity No Sexual No Orientation 2.4 Is it likely that the policy/decision will meet those needs? Group Yes/No/ Please briefly give details Don’t Know Religion N/A Ethnicity N/A 2.5 Is there an opportunity to better promote equality of opportunity or good relations by altering the policy/decision or working with others in government or in the larger community? Group Suggestions N/A 2.6 What changes to the policy/decision – if any – or what additional measures would you suggest to ensure that it promotes good relations? Group Religion Suggestions N/A Political Opinion N/A Ethnicity N/A 40 2.7 Have previous consultations with relevant groups, organisations or individuals indicated that particular policies create problems that are specific to them? Also, please detail information used to answer any of the questions above (e.g. statistics; research reports; views of colleagues, service users, or other stakeholders). N/A 2.8 Please detail what data you will collect in the future in order to monitor the effect of the policy/decision on any of the groups under Section 75? The Department will review the policy in light of any data which provides evidence of any adverse effect on any of the groups under Section 75. 41 (3) SHOULD THE POLICY/DECISION BE SUBJECT TO EQUALITY IMPACT ASSESSMENT? Equality impact assessment procedures are confined to those policies/decisions considered likely to have significant/major implications for equality of opportunity. If your screening has indicated that a policy/decision is likely to have an adverse differential impact, how would you categorise it? Please tick. Significant/major impact Low impact X Do you consider that this policy/decision needs to be subjected to a full equality impact assessment? Yes No X Please give reasons for your decision. There is no evidence that the guidance policy is likely to have a significant impact on any categories within the nine groupings. The purpose of the policy is to improve environmental cleanliness for all HSC patients, visitors and staff, regardless of their circumstances and background. The Department would expect HSC Trusts to consult locally and equality screen each local decision. 42 (4) DISABILITY DISCRIMINATION 4.1 Does the policy/decision in any way discourage disabled people from participating in public life or does it fail to promote positive attitudes towards disabled people? NO 4.2 Is there an opportunity to better promote positive attitudes towards disabled people or encourage their participation in public life by making changes to the policy/decision or introducing additional measures? No changes required. 4.3 Please detail what data you will collect in the future in order to monitor the effect of the policy/decision with reference to the disability duties? None 43 (5) CONSIDERATION OF HUMAN RIGHTS 5.1 Does the policy/decision affect anyone’s Human Rights? [PLEASE COMPLETE THE TABLE BELOW] POSITIVE IMPACT ARTICLE NEGATIVE NEUTRAL IMPACT = IMPACT human right interfered with or restricted Article 2 – Right to life Article 3 – Right to freedom from torture, inhuman or degrading treatment or punishment Article 4 – Right to freedom from slavery, servitude & forced or compulsory labour Article 5 – Right to liberty & security of person X X Article 6 – Right to a fair & public trial within a reasonable time Article 7 – Right to freedom from retrospective criminal law & no punishment without law. Article 8 – Right to respect for private & family life, home and correspondence. Article 9 – Right to freedom of thought, conscience & religion Article 10 – Right to freedom of expression X Article 11 – Right to freedom of assembly & association X Article 12 – Right to marry & found a family Article 14 – Prohibition of discrimination in the enjoyment of the convention rights 1st protocol Article 1 – Right to a peaceful enjoyment of possessions & protection of property 1st protocol Article 2 – Right of access to education X X X X X X X X X X If the effect you have identified is positive or neutral please move on to Question 5.3. 5.2 If you have identified a likely negative impact who is affected and how? At this stage we would recommend that you consult with your line manager to determine whether to seek legal advice and to refer to Human Rights Guidance to consider: whether there is a law which allows you to interfere with or restrict rights whether this interference or restriction is necessary and proportionate 44 What action would be required to reduce the level of interference or restriction in order to comply with the Human Rights Act (1998)? N/A 45 5.3 Outline any actions which could be taken to promote or raise awareness of human rights or to ensure compliance with the legislation in relation to the policy/decision. None Policy/Decision Screened by: Conrad Kirkwood Date: 21 February 2012 Please note that having completed the screening; you will need to ensure that: the screening decision is shared with key stakeholders and other interested parties (e.g. Trusts); and that consultation takes place on the outcome of screening in line with Equality Commission guidance. Contact the Evaluation, Equality and Human Rights Branch at ext. 20539 for advice regarding the above actions. 46 Appendix 3 GLOSSARY BHSCT Belfast Health & Social Care Trust BICSc British Institute of Cleaning Sciences BSI British Standards Institute Cleaning Operatives Proficiency Certificate DHSSPS Department of Health, Social Services and Public Safety EQIA Equality Impact Assessment GB Great Britain HCAI Healthcare Associated Infection HSC Health and Social Care HSCB Health and Social Care Board HSS Health and Social Services HSCT Health and Social Care Trust IPC Infection Prevention & Control NHSCT Northern Health & Social Care Trust NI Northern Ireland NPSA National Patient Safety Agency PHA Public Health Agency RQIA Regulation and Quality Improvement Authority SEHSCT South Eastern Health & Social Care Trust SHSCT Southern Health & Social Care Trust UK United Kingdom UN United Nations WHSCT Western Health & Social Care Trust 47