Issues surrounding the classification and diagnosis of
advertisement
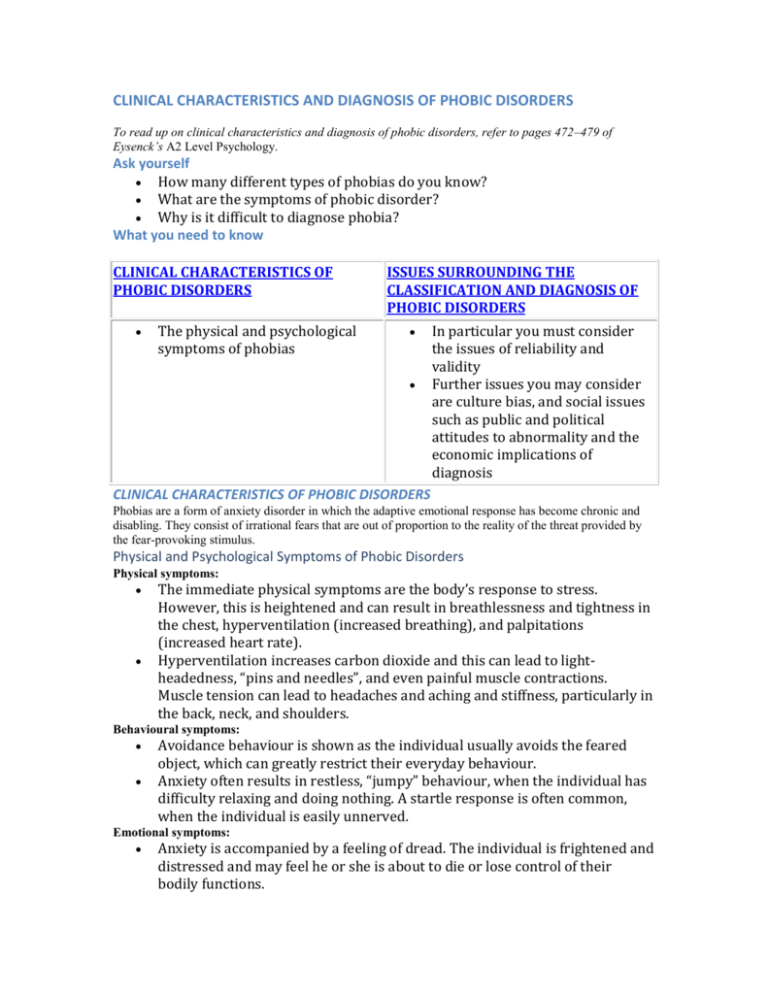
CLINICAL CHARACTERISTICS AND DIAGNOSIS OF PHOBIC DISORDERS To read up on clinical characteristics and diagnosis of phobic disorders, refer to pages 472–479 of Eysenck’s A2 Level Psychology. Ask yourself How many different types of phobias do you know? What are the symptoms of phobic disorder? Why is it difficult to diagnose phobia? What you need to know CLINICAL CHARACTERISTICS OF PHOBIC DISORDERS The physical and psychological symptoms of phobias ISSUES SURROUNDING THE CLASSIFICATION AND DIAGNOSIS OF PHOBIC DISORDERS In particular you must consider the issues of reliability and validity Further issues you may consider are culture bias, and social issues such as public and political attitudes to abnormality and the economic implications of diagnosis CLINICAL CHARACTERISTICS OF PHOBIC DISORDERS Phobias are a form of anxiety disorder in which the adaptive emotional response has become chronic and disabling. They consist of irrational fears that are out of proportion to the reality of the threat provided by the fear-provoking stimulus. Physical and Psychological Symptoms of Phobic Disorders Physical symptoms: The immediate physical symptoms are the body’s response to stress. However, this is heightened and can result in breathlessness and tightness in the chest, hyperventilation (increased breathing), and palpitations (increased heart rate). Hyperventilation increases carbon dioxide and this can lead to lightheadedness, “pins and needles”, and even painful muscle contractions. Muscle tension can lead to headaches and aching and stiffness, particularly in the back, neck, and shoulders. Behavioural symptoms: Avoidance behaviour is shown as the individual usually avoids the feared object, which can greatly restrict their everyday behaviour. Anxiety often results in restless, “jumpy” behaviour, when the individual has difficulty relaxing and doing nothing. A startle response is often common, when the individual is easily unnerved. Emotional symptoms: Anxiety is accompanied by a feeling of dread. The individual is frightened and distressed and may feel he or she is about to die or lose control of their bodily functions. Cognitive symptoms: Anxiety can decrease concentration and so decrease the person’s ability to perform complex tasks. Reduced cognitive capacity can inhibit workplace functioning. Social symptoms: Anxiety may reduce the individual’s ability to cope with social settings and so inhibit personal and social functioning. Types of Phobias The main categories of phobia are specific phobia, social phobia, and agoraphobia. The latter usually causes more disturbances to the individual’s daily life than specific phobias, which are more easily avoided. Specific phobia: This is the phobia of a specific object, which usually fall into four main subtypes: 1. 2. 3. 4. Animal type. Environmental dangers type. Blood-injection-injury type. Situational type (planes, lifts, enclosed spaces). A fifth, “other type” is an umbrella type that covers any specific phobia that does not fall into the four main types. The prevalence is 11% of the American population (Comer, 2001, see A2 Level Psychology page 473). In Europe, the United States, and Canada at least twice as many females as males develop specific phobia (Comer, 2001). Social phobia: Social phobia is a fear of social situations due to self-consciousness of own behaviour and fear of others’ reactions. This can be generalised, where the individual suffers social anxiety in most situations, or specific where the individual fears a particular situation, such as public speaking. The prevalence is 8% of the population, 70% of which are female. Agoraphobia: This is the fear of open or public places, which can include open or closed spaces, public transport, or crowds. It is very rare on its own as it is co-morbid with panic disorder. The panic disorder usually occurs first and then the individual avoids open or public places so as not to have a panic attack, and thus the agoraphobia develops. Approximately 50% of all phobics suffer with agoraphobia with panic disorder. The prevalence is 3–4% of the population, and 75% are female. Classification of phobias DSM-IV (Diagnostic and Statistical Manual, 4th edition; see A2 Level Psychology pages 473–474), which is the American classification system, and ICD-10 (International Classification of Diseases), the tenth edition of which was published by the World Health Organization in 1992 (ICD-10; see A2 Level Psychology pages 473–474), are the two most common classification systems. Diagnosis of phobias: The DSM-IV diagnostic criteria are: 1. 2. 3. 4. 5. Marked and persistent fear of a specific object or situation. Exposure to the fear-provoking stimulus produces a rapid anxiety response. The individual recognises that the fear experienced is excessive. The phobic stimulus is either avoided or responded to with great anxiety. The phobic reactions interfere significantly with the individual’s working or social life, or there is marked distress about the phobia. Specific phobia: According to DSM-IV-TR (APA, 2000, see A2 Level Psychology page 472), the diagnostic criteria for specific phobia are: Marked and persistent fear of a specific object or situation. Exposure to the phobic stimulus nearly always produces a rapid anxiety response. The individual recognises that his or her fear of the phobic object or situation is excessive. The phobic stimulus is either avoided or responded to with great anxiety. The phobic reactions interfere significantly with the individual’s working or social life, or he or she is very distressed about the phobia. In individuals under the age of 18, the phobia has lasted for at least 6 months ICD-10 has fewer criteria and these overlap with those in DSM-IV-TR. For example, the anxiety must be restricted to the presence of the phobic object or situation and avoidance is shown. Social phobia: The DSM-IV-TR (APA, 2000, see A2 Level Psychology page 473) diagnostic criteria for social phobia are: Marked and persistent fear of social or performance situations involving exposure to unfamiliar people or possible scrutiny by others lasting at least 6 months. There is concern about humiliating or embarrassing oneself. Anxiety is usually produced by exposure to the social situation. There is recognition that the fear is excessive and/or unreasonable. There is significant distress or impairment. The ICD-10 diagnostic criteria closely resemble those in DSM-IV-TR. For example, the anxiety must be restricted to social situations, and frequent avoidance of these social situations must be shown. Agoraphobia: Agoraphobia is accompanied by panic disorder when open or public spaces are experienced and so the DSM IV criteria reflect this. The DSM-IV-TR (APA, 2000, see A2 Level Psychology page 474) criteria for panic disorder with agoraphobia are: Recurrent unexpected panic attacks. At least one panic attack has been followed by at least 1 month of worry about the attack, concern about having more panic attacks, or changes in behaviour resulting from the attack. Agoraphobia, in which there is anxiety about being in situations from which escape might be hard or embarrassing in the event of a panic attack. The situations are either avoided, endured with marked distress, or manageable only with the presence of a companion. The ICD-10 criteria are similar except they focus on the agoraphobia rather than the agoraphobia plus panic. The main criterion is that anxiety is largely restricted to: crowds, public places, travelling away from home, and travelling alone. A second criterion is that there is frequent avoidance of the situations causing anxiety. Issues surrounding the classification and diagnosis of phobic disorders For any diagnostic system to work effectively, it must possess reliability and validity. Reliability means that there is good consistency over time and between different people’s diagnosis of the same patient; known as inter-judge (or inter-rater) reliability. If diagnosis of depression is valid then patients who are diagnosed as suffering from depression must have the disorder. If a diagnostic system is to be valid, it must also have high reliability. Clearly if a disorder cannot be agreed upon (so low reliability) then all of the different views cannot be correct (so low validity). In terms of classification, DSM-IV and ICD-10 take a categorical approach, which assumes that all mental disorders are distinct from each other, and that patients can be categorised with a disorder based on their having particular symptoms. However, diagnosing abnormality is not as straightforward as this approach suggests. If a diagnostic system is to be valid, it must also have high reliability. Clearly if a disorder cannot be agreed upon (so low reliability) then all of the different views cannot be correct (so low validity). Whereas a diagnostic system can be reliable but not valid—it can produce consistently wrong diagnoses. The categorical approach Classification systems such as DSM-IV-TR (revised version of DSM-IV in 2000) and ICD-10 are categorical systems. This is an all-or-none approach in which patients are assumed to have the disorder or not. This seems straightforward but using the system in practice is not because many individuals may not meet all of the criteria for diagnosis, but nevertheless have many of the symptoms of phobia. For example, many people are very frightened of snakes and/or spiders, but the fear isn’t quite strong enough to qualify as a specific phobia. The validity of DSM-IV and ICD-10 is reduced by the strict and arbitrary criteria used in the all-or-none approach. Despite the weaknesses of such as classification, strict criteria are needed to achieve reliability in diagnosis. Comorbidity Comorbidity is when a patient has two or more mental disorders at the same time. Approximately 50% of social phobics have one or more related disorders such as depression, substance abuse, agoraphobia, or generalised anxiety disorder (Rachman, 2004, see A2 Level Psychology page 477). Patients with agoraphobia often suffer from panic disorder or depression. Comorbidity affects reliability and validity because it makes it more difficult to diagnose what exactly is wrong and so the diagnosis may be wrong (not valid) or lack consistency (not reliable). Diagnosis: Semi-structured interviews Patients are generally diagnosed on the basis of one or more interviews with a therapist. Some interviews are very unstructured and informal. This can produce good rapport between the patient and the therapist, but reliability and validity of diagnosis tend to be low. The most reliable and valid approach involves the use of semi-structured interviews in which patients are asked a largely predetermined series of questions. EVALUATION Semi-structured interviews do have good reliability and validity. Two of the most used semi-structured interviews for phobia are the Structured Clinical Interview for DSM-IV-Patient Version (SCID-I/P) and the Anxiety Disorder Interview Schedule for DSM-IV (ADIS-IV). Both interviews involve systematic questioning about a range of symptoms common to phobias. strong>Research evidence for high reliability. Brown et al. (2001) studied the reliability of DSM-IV. 1400 patients were interviewed twice with the second interview occurring within 2 weeks of the first one. They found inter-rater agreement was excellent for specific phobia, social phobia, and panic disorder with agoraphobia, and reliability was higher than for other mental disorders such as generalised anxiety disorder and major depressive disorder. Easy to diagnose. The high reliability of diagnosis is because phobias have clear behavioural symptom (avoidance of the feared stimulus or situation) that makes it relatively easy for therapists to diagnose them. The “threshold issue”. The lack of reliability was mainly due to the categorical approach and what is described as the “threshold” issue. Did the patient’s symptoms cause sufficient distress or interference with his or her life to warrant a phobia diagnosis? There were inconsistencies and so lack of reliability in judgements on level of interference. Other issues included patients’ reports of their symptoms sometimes changed between interviews, or interviewer errors or subjectivity in categorisation of symptoms. Content validity High content validity means that the given form of assessment, such as interview or checklist, succeeds in eliciting adequate information from patients concerning all of the symptoms of the phobia in question. The semi-structured interviews such as ADIS-IV and SCID-I/P have high content validity because they have been carefully constructed to cover all symptoms of phobias contained in DSM-IV. Criterion validity This involves considering various aspects of the behaviour of those diagnosed with a given phobia. High criterion validity means that those with a diagnosis of, say, social phobia, differ in predictable ways from those not receiving that diagnosis. EVALUATION Evidence for differences. Evidence for criterion validity is that those diagnosed with agoraphobia or social phobia report significant problems of work and social adjustment (Mataix-Cols et al., 2005, see A2 Level Psychology page 478). Lower for specific phobia. However, criterion validity is lower for specific phobia because impaired adjustment is usually quite low. If you imagine the specific phobia is of frogs it’s not that difficult to just avoid them and so in every other way live a normal life! The level of impairment will depend on the commonness of the feared object. Difficult to distinguish phobias from other mental disorders. There is some evidence for criterion validity for phobias, but note that poor social and work functioning are found in those suffering from most mental disorders and so this doesn’t distinguish patients with phobias from patients with other mental disorders. Construct validity This type of validity is more theoretical in nature than the others. It involves testing hypotheses based on our understanding of the particular phobia. For example, we might predict that patients diagnosed with social phobia would underestimate their own social skills. It is sometimes hard to know what to do if a hypothesis isn’t supported—it might mean that the diagnostic assessment was inaccurate or that the hypothesis itself was at fault. The diagnosis of phobias has reasonable construct validity because hypotheses are supported, for example the fact that phobics have faulty cognitions. Predictive validity This is concerned with the extent to which we can use the diagnosis of, say, social phobia, to predict the eventual outcomes for patients. Suppose, for example, that most social phobics respond well to a given form of treatment but that nevertheless it generally took a long time for recovery to occur. Since we would be able to predict the eventual outcome (in this case recovery) reasonably well from the diagnosis, this would indicate high predictive validity. Phobias have some predictive validity because we can predict a better outcome for specific phobia compared to social phobia and agoraphobia because the latter are much more serious disorders. This is supported by the fact that specific phobia is generally easier to treat than social phobia or agoraphobia. So what does this mean? Overall, then, it seems that the main ways of diagnosing major phobias possess reasonable content, criterion, construct, and predictive validity. The various symptoms within phobias inevitably raise some issues of reliability and validity in diagnosis. However, diagnosis of phobias tends to be more reliable than other disorders because the behavioural symptoms are quite clear-cut. The two main systems of diagnosis, DSM-IV and ICD-10, have reasonably good content validity as the research findings suggest they have sufficient detail of symptoms for accurate diagnosis. However, there are many issues that question the reliability and validity of diagnosis, such as the categorical approach and comorbidity. Unstructured clinical interviews can lack reliability and validity. However, the semistructured interviews, SCID-I/P and ADIS-IV, have been found to have reliability as two therapists’ diagnoses have been found to be high in consistency, and they have high diagnostic accuracy (validity). Over to you 1. Outline the clinical characteristics of one anxiety disorder. (5 marks) 2. Discuss the issues associated with the classification and diagnosis of one anxiety disorder. (20 marks)