Topic Presentation Sample
advertisement
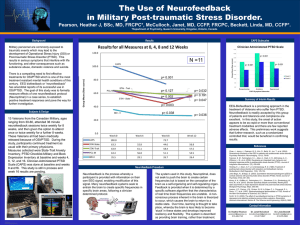
Stress Related Psychiatric Disorders Lorenzo Pitts MSIII HUCM “To understand the stress response, we must process a fundamental knowledge not only of psychology but of physiology as well.” —George Everly Physiology of Stress The ACTH Pathway Anxiety Disorders • Panic Disorder • Phobias • Obsessive Compulsive disorder • Generalized Anxiety Disorder First Rule Out • Medical Causes of Anxiety Disorders – Hyperthyroidism – Vitamin B12 deficiency – Hypoxia – Neurological disorders – Cardiovascular disease – Anemia – Pheochromocytoma – Hypoglycemia First Rule Out • Medication or Substance-Induced Anxiety Disorders – – – – – – – – – – Caffeine intake and withdrawal Amphetamines Alcohol and sedative withdrawal Other illicit drug withdrawal Mercury or arsenic toxicity Organophosphate or benzene toxicity Penicillin Sulfonamides Sympathomimetics Antidepressants Panic Attack Panic Disorder • A 24 yr old female comes to the ER complaining of a pounding heart, SOB, and sweating that began while she was shopping and lasted 20mins. She expresses that she thought she was going to die. Further questioning reveals that she has had 6 of these episodes in the last month and fears having another one. Diagnosis & DSM-IV Criteria 1. Spontaneous recurrent panic attacks with no obvious precipitant 2. At least one of the attacks has been followed by a minimum of 1 month of the following: – Persistent concern about having additional attacks – Worry about the implications of the attack – A significant change in behavior related to the attacks Treatment • Pharmacological – Acute Initial TX of Anxiety • Benzodiazepines- If necessary, continued for a brief period (<2 wk if prescribed on a scheduled basis). – Maintenance • SSRIs, especially Paroxetine (Paxil) and Sertraline (Zoloft) DOC for long term tx. • Tx should continue for at least 8-12 months, as relapse is common after discontinuation of therapy Treatment • Non-Pharmacological Psychotherapy – Cognitive Therapy – Behavioral Therapy – Relaxation training PHOBIAS Specific & Social Phobia • Phobia: irrational fear that leads to avoidance of the feared object or situation. • Specific Phobia: strong, exaggerated fear of a specific object or situation • Social Phobia: fear of social situation in which embarrassment can occur. Specific & Social Phobias • A 32 yr old construction worker states that he is terrified of heights. He came in to your office because he recently started a project on the 50th floor and has had trouble doing his job. Specific & Social Phobias • A 25 yr old HUCM student has always felt “shy” and avoids answering questions on rounds. Last Thursday, he stayed home although he had a presentation to give because he did not want to make a “fool out of himself” in front of his classmates. Diagnosis & DSM-IV Criteria of Specific Phobia • Persistent excessive fear brought on by a specific situation or object • Exposure to the situation brings about an immediate anxiety response • Patient recognizes that the fear is excessive • The situation is avoided when possible or tolerated with intense anxiety • If person under age 18, duration must be at least 6 months. Common Phobias • Specific Phobias – – – – – – Fear of animals Fear of heights Fear of blood or needles Fear of illness or injury Fear of death Fear of flying • Social Phobias – Speaking in public – Eating in public – Using public restrooms Treatment • Specific Phobia – Systemic desensitization (with or without hypnosis) and supportive psychotherapy. – If necessary, short course of Benzodiazepines or Beta Blockers may be used during desensitization to help control autonomic symptoms. Treatment • Social Phobia – SSRIs: Paroxetine (Paxil), Sertraline (Zoloft) both FDA approved. Standard first-line medication – Beta blockers are frequently used to control symptoms of performance anxiety – Treatment of choice is Assertiveness training a compound of CBT. Obsessive-Compulsive Disorder OCD • A 28 yr old medical student comes to your office because he is distressed by his repetitive checking of the car door to see if its locked. He states that after he parks the car and gets to his house, he feels as if the car door is not locked and goes back to check on it. This happens several times and has led to his being late for his clerkships and getting yelled at by his chief. Common Patterns of Obsessions & Compulsions • Obsessions about contamination followed by excessive washing or compulsive avoidance of the feared contaminant • Obsessions of doubt followed by repeated checking to avoid potential danger • Obsessions about symmetry followed by compulsively slow performance of a task • Intrusive thoughts with no compulsion. Thoughts are often sexual or violent Treatment • Pharmacologic – SSRIs are 1st line (fluoxetine, fluvoxamine, sertraline, paroxetine, citalopram, escitalopram) – Tricyclic antidepressants (Clomipramine) • Behavioral Tx – Considered as effective as pharmacotherapy. Best outcomes often achieved with both. Exposure and response prevention, involves prolonged exposure to the ritual-eliciting stimulus and prevention of the relieving compulsion. – Relaxation techniques are employed to help the patient manage the anxiety that occurs when the compulsion is prevented. Post Traumatic Stress Disorder PTSD • A 23 yr old female who was raped 5 months ago complains of recurrent thoughts of that event every time a coworker touches her. She states this has been happening for the past 2 months often accompanied by nightmares that wake her up at night. She feels extremely anxious when these thoughts “pop in” and lately has had trouble working at her job. Diagnosis & DSM-IV Criteria • Having experienced or witnessed a traumatic event. The event was potentially harmful or fatal, and the initial rxn was intense fear or horror • Persistent reexperiencing of the event • Avoidance of stimuli associated with the trauma • Numbing of responsiveness • Persistent symptoms of increased arousal • Symptoms must be present for at least 1 month Treatment • Pharmacological – TCAs- imipramine and doxepin – SSRIs, MAOIs – Anticonvulsants- for flashbacks and nightmares • Non-Pharmacological – Psychotherapy – Relaxation training – Support groups, family therapy Diagnosis and Treatment of Post-traumatic Stress Disorder FIGURE 1. Algorithm for the diagnosis and treatment of post-traumatic stress disorder. (DSM-IV = Diagnostic and Statistical Manual of Mental Disorders, 4th ed.; PTSD = post-traumatic stress disorder; SSRI = selective serotonin reuptake inhibitor) PTSD vs. Acute Stress Disorder PTSD • Event occurred at any time in past • Symptoms last GREATER than 1 month Acute Stress Disorder • Event occurred LESS than 1 month ago • Symptoms last LESS than 1 month PTSD in the Military • A case of PTSD is defined as an individual having at least two outpatient visits or one or more hospitalizations at which PTSD was diagnosed. The threshold of two or more outpatient visits is used to increase the likelihood that the individual actually had PTSD • The Army has 67% of the cases, the Air Force has 9%, the Navy has 11%, and the Marines have 13%. Annual New Post-Traumatic Stress Disorder Diagnoses in All Services • • • • • • • • • • • • • • • As of September 7, 2010 Year Not Deployed Deployed 2000 1,614 0 2001 1,703 0 2002 1,709 138 2003 1,524 1,169 2004 1,577 3,901 2005 1,648 6,788 2006 1,714 7,762 2007 2,069 11,660 2008 2,371 14,183 2009 2,432 13,595 2010 1,423 7,739 Total 21,784 66,935 Source: Personal communication with Dr. Michael Carino, Army Office of the Surgeon General, September 21, 2010. Data source is the Defense Medical Surveillance System (DMSS). PTSD in the Military • According to the Department of Veterans Affairs, experts believe PTSD occurs in: – 11-20% of Veterans that served in Operation Iraqi Freedom and Operation Enduring Freedom. – 10% of Desert Storm Veterans. – 30% of Vietnam Veterans. Thank you References • www.emedicine.com • http://www.aafp.org/afp/2003/1215/p2401.h tml#afp20031215p2401-f1 • http://www.psychiatryonline.com/pracGuide/ pracGuideTopic_9.aspx • First aid for the psychiatry clerkship