Micro Revision Notes
advertisement
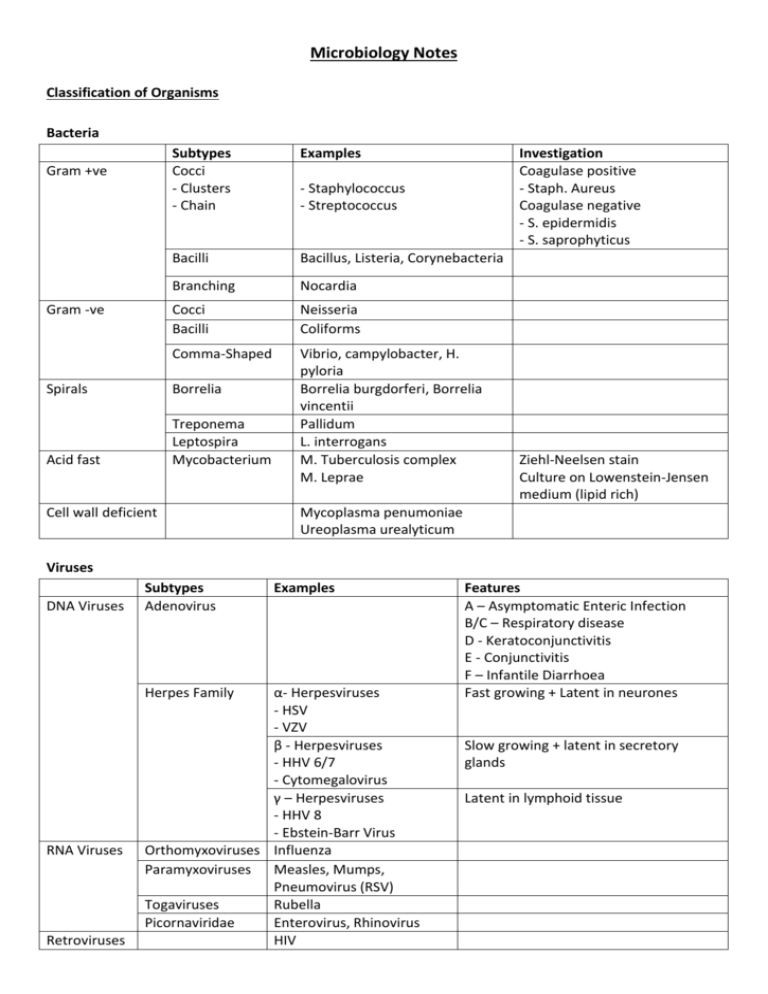
Microbiology Notes Classification of Organisms Bacteria Gram +ve Gram -ve Subtypes Cocci - Clusters - Chain Examples Bacilli Bacillus, Listeria, Corynebacteria Branching Nocardia Cocci Bacilli Neisseria Coliforms Comma-Shaped Vibrio, campylobacter, H. pyloria Borrelia burgdorferi, Borrelia vincentii Pallidum L. interrogans M. Tuberculosis complex M. Leprae Spirals Borrelia Acid fast Treponema Leptospira Mycobacterium Cell wall deficient Investigation Coagulase positive - Staph. Aureus Coagulase negative - S. epidermidis - S. saprophyticus - Staphylococcus - Streptococcus Ziehl-Neelsen stain Culture on Lowenstein-Jensen medium (lipid rich) Mycoplasma penumoniae Ureoplasma urealyticum Viruses DNA Viruses Subtypes Adenovirus Herpes Family RNA Viruses Retroviruses Examples α- Herpesviruses - HSV - VZV β - Herpesviruses - HHV 6/7 - Cytomegalovirus γ – Herpesviruses - HHV 8 - Ebstein-Barr Virus Orthomyxoviruses Influenza Paramyxoviruses Measles, Mumps, Pneumovirus (RSV) Togaviruses Rubella Picornaviridae Enterovirus, Rhinovirus HIV Features A – Asymptomatic Enteric Infection B/C – Respiratory disease D - Keratoconjunctivitis E - Conjunctivitis F – Infantile Diarrhoea Fast growing + Latent in neurones Slow growing + latent in secretory glands Latent in lymphoid tissue Anti-Microbial Therapy Anti-virals Target Viral binding Uncoating Replication Examples Fusion inhibitors (Important for future) Most current drugs e.g. acyclovir, ganciclovir e.g protease inhibitors e.g. interferons Assembly Release Organism HSV/VZV Rationale 1st line Aciclovir CMV HIV Chronic HBV Chronic HCV Influenza 2nd line Famciclovir Valaciclovir Valaciclovir Foscarnet Ganciclovir “HAART” 2 NRTI + NNRTI/PI 40% success rate 60% success rate Genotypes 2,3 - better prognosis. Rx for 6/12 Genotypes 1,4 - worse prognosis. Rx for 12/12 Only use in at-risk adults Must be started within 48h of symptoms Interferon-α + Lamivudine Peginterferon-α Ribavirin Famciclovir Influenza A - Amantadine Influenza A + B Neurainidase inhibitor (Zanamivir/Olseltamivir) Antibiotics Action Inhibit Cell Wall Synthesis Inhibit Protein Synthesis Inhibit Nucleic Acid Synthesis Inhibit Folate Synthesis Sub-types β- Lactams Glycopeptides Carbapenems Monobactams Aminoglycosides Tetracycline Macrolides Others Quinolones Others Sulphonamides Di-aminopyrimidines Drugs Penicillin, Cephalosporins Vancomycin, Teicoplanin Imipenem Aztreonam Gentamicin Tetracycline, Doxycycline Erythromycin, Clarithromycin Chormapheicol, Fusidic acid Ciprofloxacin, Ofloxacin Metronidazole, Trimethoprim, Rifampicin, Sulphonamides Trimethoprim, Septrin Type Basic Broad-spectrum β-lactamase resistant Anti-pseudomonal 1st Generation Generation rd 3 Generation 2nd Drugs Sides effects Penicillins Benzylpenicillin, penicillin G, Rash Phenoxymethypenicillin, Anaphylaxis penicillin Nausea/vomiting Amoxicillin Flucloxacillin, Co-amoxiclav Interactions/ Containdications Reduced efficacy of COC Hypersensitivity Tazocin Cephalosporins Cefelexin C. Difficile Bleeding Cefuroxime Thrombophlebitis Cefotaxime, Ceftazidime, Ceftriaxone Glycopeptides Vancomycin, Teicopanin Ototoxicity Nephrotoxicity Thrombophlebitis Carbapenems Imipenem, Meropenem Nausea/vomiting Seizures Aminoglycosides Gentamicin, Streptomycin Nephrotoxicity Ototoxicity Thrombophlebitis Tetracyclines Tetracycline, Doxycycline Teeth/bone deposits Macrolides Eryhtromycin, Clarithromycin Nausea/vomiting Cholestatic jaundice Quinolones Ciprofloxacin, Ofloxacin GI disurbance Tendon damage Metronidazole Nitromidazoles GI disturbance Antabuse reaction with alcohol Hypersensitivity (10% who are allergic to penicillin will also be allergic) Loop diuretics ↑ ototoxicity, Cyclosporin or Aminoglycosides ↑ nephrotoxicity Pregancy, MG Loop diuretics or cyclosporine ↑ nephrotoxicity Antagonise anitcholinesterases Renal impairement Absorption affected by Ca2+, Iron tablets, Mg2+ CP450 inhibitor, Stop statins CP450 inhibitor Epilepsy (lower seizure threshold) Hx of tendon damage Hepatic impairement, Hx of tendon damage, ↑phenytoin levels, ↑warfarin levels Anti-Mycobacterium Drugs Drug Rifampicin Indications Tuberculosis, Leprosy Contact prophylaxis in meningitis Isoniazed Tuberculosis Pyrazinamide Ethambutol Tuberculosis Tuberculosis (if isoniazid resistance is likley) Adverse effects Deranged LFTs Orange secretions CP450 inducer Peripheral neuropathy (Rx pyridoxine), Hepatotoxicity Hepatocellular toxicity Retrobulbar neuritis (< 8 weeks therapy) Infections by Organ system Cerbral Infections Disease Organisms Cerebral Local infection: Bacterial Abscess (strep milleri, bacteroides, staph) or fungal Metastatic infection: pneumonia, infective endocarditis Encephalitis Meningitis Bacterial: secondary to meningitis Viral: Herpes simplex, rabies Fungal: histoplasma, cryptococcus Protozoal: toxoplasma, plasmodium Viral: Enteroviruses Bacterial: N. meningitidis, Group B strep, Gram -ve bacilli, Listeria Fungal: Cryptoccous, candida Features/Ix An acute focal suppuration in the brain substance Cerebrum or cerebellum 25% mortality General: usually none Specific: mass effects Signs pyrexia (50%), focal signs, papilloedema Inflammation of the brain substance Ill (fever, headache, malaise) Alt consciousness/seizures, Photophobia Confirmed with viral picture in CSF sample +/- focal inflammation on CT and slow EEG activity. Inflammation of the meninges Stiff neck, headache, fever, photophobia, non-blanching rash, vomiting, confusion, joint pain, seizures Ix: LP Treatment Aerobes - cephalosporin Anaerobes – metronidazole + dexamethasone +/- antifungal ? Surgery to reduce pressure Mostly due to herpes simplex so use acyclovir I.V. Emergency: 1.2 g benzypenicillin IM Cefotaxime 2g 6-hourly IV +/- ampicillin for Listeria Contacts – rifampicin or ciprofloxacin Vaccination Lung Infctions Disease Organisms CAP Typicals (85%) S. pneumoniae, H. influenza, staph. aureus (elderly), M. catarrhalis (smoking), Klebsiella (alcoholic) Atypicals (15%) Mycoplasma, Legionella Zoonoes: Chlamydia, Coxiella, bordetella HAP AP TB Viruses: Influenza A & B, Varicella and Herpes pneumonitis Gram -ve, few Gram +ve Klebsiella, Serratia, Enterobacter, Pseudomonas Nearly always Gram -ve organisms from the gut Mycobacterium tuberculosis Features/Ix General symptoms, Cough +/- sputum, SoB, Pleuritic chest pain Reduced air entry, Dullness to percussion, Tactile vocal fremitus, Bronchial breathing, Crackles coarse Treatment Typicals - β lactams, Amoxicillin, Cefuroxime Atypicals – Macrolides, Clarithromycin/Erythromycin Anti-virals - amantadine +/neuraminidase inhibitors Chest X-ray: Consolidation Gram +ve - Vancomycin, Gram –ve – Ceftazidime, Gentamicin Cefuroxime and metronidazole AFB on Ziehl-Neelson staining Rifampicin, Isoniazed, Culture up to 7 weeks! Pyrazinamide, Ethambutol Mantoux - Does not distinguish vaccinated and infected/Not reliable in HIV GI Infections Disease Throat Infections Upset Tummy Hepatitis A Hepatitis B Hepatitis C Organisms Herpes Tonsillitis Glandular fever Candidiasis Bacteria - staph. aureus, bacillus cereus, lostridium, listeria Viruses - Rota virus, Noraviruses, Adenovirus, Hepatitis A Protozoa - Entamoeba histolytica, Giardia lamblia Cryptosporidium Features/Ix Treatment Diarrhoea - Frequent passage of loose stools Dysentry - Frequent passage of blood and mucus in the stools” Staph. aureus - rapid onset of vomiting and diarrhoea Bacillus cereus in reheated rice Clostridium botulinum in canned food C. difficile pseudomembranous colitis (usually cephalosporin related) Travellers’ Diarrhoea - due to exposure of new E.coli strains Rotavirus - kids, explosive and distinctive smell Salmonella - eggs and poultry Camplylobacter complications – GB syndrome or Reiter’s Faeco-oral spread Incubation: few weeks Acute never chronic Systemic symptoms + jaundice Elevated AST/ALT Spread through sex, blood products, vertical Incubation - up to 6 months Acute or chronic Increased risk of cirrhosis and HCC Support with fluids, loperamide As for Hep. B - but blood spread most common Acute or chronic Complications of chronicity 30% cirrhosis, 5% hepatocellular carcinoma Antibiotics for neonates, elderly and immunocompromised (Ciprofloxacin) Treat protozoals with metronidazole Interferon alpha, lamuvudine (NRTI) or adefovir Only a 40% success rate Vaccination for certain groups Transplantation Peginterferon alpha Sexually Transmitted Infections Disease Organisms Chlamydia Chlamydia trachomatis Gonorrhoea Gram -ve intracellular cocci NSU Syphilis LGV HSV HPV Treponema pallidum Lymphogranuloma venereum caused by L1/L2/L3 variant of Chlamydia Type I - cold sores, gingivostomatitis Type II - genital sores Features/Ix Incubation a few weeks Clear mucoid discharge Mucopurulent cervicitis Asymptomatic (80% female, 50% male) Dx requires: Urine, Endocervical swab Site of infection: cervix, urethra, rectum and pharynx Short incubation period 95% symptomatic in men, 50% in women Diagnosis - Microscopy for gram ve intracellular diploccoci Men only Inflammation of the urethra leading to discharge and dysuria Dx of exclusion (absence of gram neg. cocci on microscopy) e.g. chlamydia, mycoplasma, uroplasma, trichomonas Primary (painless ulcer/chancre + lymphadenopthy) Secondary (serocoversion illness and condylomata late) Latent syphilis Tertiary syphilis (granulomata, meningovascular disease, tabes, bone and skin gumma) Diagnosis Cannot be cultured Visualised with dark ground microscopy or using serology (VDRL) Painless ulcerative papule Heals to give painful lymphadenopathy/buboes Ciprofloxacin/ofloxacin 3rd gen cephalosporin ceftriaxone Single dose azithromycin Complication - epidydimoorchitis, reactive arthritis 2.4 MU penicillin Doxycycline Topical or systemic acyclovir Low Grade (types 6/11) - painless warts High Grade (types 16/18/31/32) CIN/AIN HIV Treatment Single dose of azithromycin A retrovirus with an RNA genoma Relies on reverse transcriptase to integrate into genome Podophyllin extract Cryotherapy Infects the immune system CD4+ T helper cells (reduced number and function) CD4+ dendritic cells (failure of antigen presentation and immune memory) Primary Infection (first 12 weeks) Large increase in viral load Dramatic decline in CD4 and gradual increase in CD8 that control viral load Asymptomatic phase (CD4 & CD8 stable) AIDS Virus seeps out of cell and alters CD4 function and number. CD4+ < 200 or AIDs-defining illness Diagnosis Anti-HIV antibodies (ELISA) o Screening test Viral load (PCR) o Very sensitive and definitive test o Initial baseline plasma viral load predict time for active disease to appear Monitoring Viral load CD4+ T cell counts HIV-resistance tests o Expensive tests that look at resistance to anti-retroviral medication Therapies “HAART” o Reverse transcriptase inhibitors o Protease inhibitors Type NNRTs - nucleoside analogues Drug Zidovudine (AZT) Didanosine (DDI) Zalcitabine (DDC) Lamivudine (3TC) Abacavir NNRTI - non-nucleoside analogue Nevirapine Efavirenz Protease Inhibitors Saquinavir Efavirenz Indinavir Side Effects Myelotoxicity -anaemia and neutropenia Muscle wasting Pancreatitis Peripheral neuropathy Peripheral neuropathy Well tolerated so used first line May cause SJS so required screening before using May cause SJS Enzyme inducer Popular at present - O.D. dosing 25% develop minor skin rash Deranged LFTs Perioral hyperaesthesia Kidney stones Urinary Tract Infections Disease Organisms Simple Cystitis E.coli, proteus, staphylococcus saprophyticus, Pyelonephritis Klebsiella, Enterococcus Skin Infections Disease Cellulitis Infected eczema Dermatophytosis Organisms Staph. and strep. Impetigo -Usually caused by Strep. pyogenes Eczema herpeticum Caused by HSV 1 & II Trichophyton and microsporum are most common Features/Ix Dysuria, Frequency, Suprapubic pain, urgency Systemic sx, Loin pain and tenderness Treatment Trimethoprim, amoxicillin, nitrofurantoin, cephalosporin Requires IV antibiotics Cefuroxime + Gentamicin Men and children require urography post-infection Features/Ix Infection and inflammation of connective tissue underlying skin Often following minor skin trauma Superficial bacterial skin infection common in kids Serious Widespread vesicular rash A group of skin infections caused by dermatophytes - Tinea corporis - Tinea crucris - Tinea pedis - Onychomycosis Treatment Flucloxacillin + coamoxiclav Topical fusidic acid, mupirocin oral if severe Topical and oral aciclovir Cotrimazole (Imidazole) Miconazole (Imidazole) Terbinafide (Allylamines) Tropical Infections Disease Organisms Malaria P. falciparum P. vivax P. ovale P. malariae Features/Ix Anyone returning from endemic area Fever/rigors, Headache/myalgia, Nausea and vomiting, Diarrhoea, Dark urine, Jaundice Thick film (it is present?) Thin film (what species?) Leptospirosis Lyme Disease Spirochaete - Borreli burgorferi Schistosomiasis Schistosomal cerceriae Trypanosomiasis Trypanosomal protozoans Leishmaniasis a.k.a Weil’s disease Contact with animal resorvoirs e.g. rat urine Systemic upset + conjunctival suffusion + hepatosplenomegaly Haemolysis and renal failure if severe IgM antibodies Ticks on infected deer/mice Localised early disease: erythema chronic migrans + minor systemic Disseminated disease: systemic disease (arthritis, carditis, neurol symptoms) Common but people are rarely unwell Penetrate skin after fresh water exposure and spread to Swimmer’s itch - transient rash 1-2 days after exposure Bladder - haematuria, urinary symptoms and eosinophilia Gut (intestinal schistosomiasis) vague abdo. symptoms 2 types: • African (Sleeping sickness) Gambiense/rhodesiense • American (Chagas disease) - Cruzi Baghdad boil, kala azar, dum-dum fever Spread by sandflies Cutaneous (skin sores) or Visceral (hepatosplenomegaly, anaemia) Treatment Prophylaxis Avoid getting bitten nets, repellants etc. Treatment P. Falciparium - quinine + tetracycline Non-falciparium chloroquine + primaquine Erythromycin Erythromycin Priziquantel Amphotericin or Miltefosine