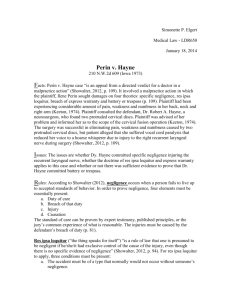
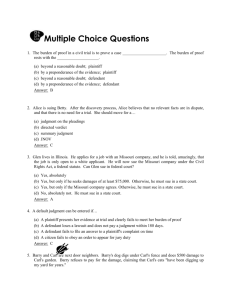
notes (2014) - The University of Queensland Law Society
advertisement

LAWS5126 Medical Law | Exam Notes 1 Table of Contents Three Elements of Medical Law .............................................................................................................3 1. Contract................................................................................................................................................................. 3 2. Battery ................................................................................................................................................................... 3 3. Negligence ............................................................................................................................................................ 3 Contract ..........................................................................................................................................................3 Elements of Contract ............................................................................................................................................. 3 Breach of Contract ................................................................................................................................................. 3 Eyre v Measday [1986] 1 All ER 488 ............................................................................................................................ 3 Thake v Maurice [1986] QB 644 .................................................................................................................................... 4 Battery – (Medical Law as Tort Law) ....................................................................................................5 The elements of battery ....................................................................................................................................... 5 Consent ...................................................................................................................................................................... 5 Elements of Consent ........................................................................................................................................................... 5 Emergency ................................................................................................................................................................ 9 Negligence – (Medical Law as Tort Law) .......................................................................................... 11 The elements of negligence .............................................................................................................................. 11 Duty of Care ............................................................................................................................................................ 12 Breach of Duty ....................................................................................................................................................... 16 The standard of care: ...................................................................................................................................................... 16 (i) Failure to take a medical history.......................................................................................................................... 16 (ii) Causing an injury to patient during surgery .................................................................................................. 17 (iii) Errors in treatment ................................................................................................................................................. 19 (iv) Error in diagnosis..................................................................................................................................................... 20 (v) Failure to follow-up .................................................................................................................................................. 22 (vi) Failure to counsel patient who might be seriously ill, against leaving hospital ............................ 23 (vii) Failure to properly train reception to detect and prioritise patients with urgent need ........... 24 Causation and Necessary Legal Principles .................................................................................................. 24 (viii) Failure to advise of material risks .................................................................................................................. 25 Summary of the Three Elements and Causes of Action .......................................................................... 36 1. Contract ....................................................................................................................................................................... 36 2. Battery.......................................................................................................................................................................... 36 3. Negligence .................................................................................................................................................................. 36 The Civil Liability Acts ............................................................................................................................. 38 Introduction ........................................................................................................................................................... 38 (1) CLA operates prospectively................................................................................................................................... 38 (2) CLA not entirely comprehensive ......................................................................................................................... 38 (3) CLA is not a codification of the law of negligence ........................................................................................ 38 Duty of care under the CLA ............................................................................................................................... 38 Breach under the CLA ......................................................................................................................................... 39 1. Work out ‘reasonable foreseeability’ – two sub-steps ............................................................................. 39 2. Standard of care ....................................................................................................................................................... 39 3. Factors indicating a breach – calculus of negligence ................................................................................ 39 Causation under the CLA.................................................................................................................................... 40 Doctors’ duties under the CLA ......................................................................................................................... 40 Competency ................................................................................................................................................ 42 Capacity, Autonomy and Beneficence ........................................................................................................... 42 The Definitions of Capacity............................................................................................................................... 42 LAWS5126 Medical Law | Exam Notes 2 An Application of the Understanding Approach .................................................................................................. 43 Factors that impair competency? ................................................................................................................... 44 Temporary factors ........................................................................................................................................................... 44 Permanent Factors ........................................................................................................................................................... 46 Information and Medical Practice ...................................................................................................... 51 Part 1 - Confidentiality ....................................................................................................................................... 51 Exceptions to Confidentiality....................................................................................................................................... 52 Is there a duty of disclosure? ....................................................................................................................................... 54 Part 2 - Access to Records ................................................................................................................................. 55 Constitutional Limitations on Health Care ...................................................................................... 57 Relevant heads of power ................................................................................................................................... 57 Conjoined Twins ....................................................................................................................................... 60 Concepts .................................................................................................................................................................. 60 Property Rights in Human Body Parts.............................................................................................. 63 Bio-Ethics .................................................................................................................................................... 66 Four Principles of Bio Ethics ............................................................................................................................ 66 LAWS5126 Medical Law | Exam Notes 3 Three Elements of Medical Law 1. Contract 2. Battery 3. Negligence Contract Elements of Contract 1. Offer to contract (patient’s request/need for medical services); 2. Acceptance to create legal relations (provision of medical services); 3. Intention to create legal relations (patient and physician have a conversation/concluding a contract for medical services); and 4. Consideration (the patient making, or promising to make, a payment for medical services provided by the physician: Sidaway v Board of Governors of Bethlem Royal Hospital or submitting to medical services provided by the physician): Coggs v Bernard; Banbury v Bank of Montreal. Medicare system does not change the existence of consideration between a private patient and a physician, but no consideration exists between patient at a private hospital and a physician there who performs public services. Breach of Contract Actions for breach of contract for medical services between a patient are complicated because: There may not be a contract at all – e.g. public hospital; The action may be statute-barred (6 years, LAA s10); The relevant contracts contain few express terms; and Courts are unwilling to imply a contractual term that the medical treatment will be successful, although they will imply a contractual warranty that the physician will exercise reasonable care and skill in the provision of medical services to the patient: o Eyre v Measday; o Thake v Maurice Eyre v Measday [1986] 1 All ER 488 Facts: E consulted gynaecologist to arrange a sterilisation operation. Dr Measday recommended to E and her husband an operation as ‘irreversible’. Dr Measday did not warn of a 1% risk that the operation would prove unsuccessful and expose E to having children. E underwent the operation and later had children. Issue: The plaintiff sued the defendant for breach of contract, claiming that: The nature of the contract was one by which the defendant contracted to render the plaintiff LAWS5126 Medical Law | Exam Notes 4 100% sterile; or in the alternative That the contract contained a warranty by the defendant, express or implied to the effect that the operation which he was to perform would have the effect of sterilising her. Held: Plaintiff’s claims dismissed at trial and on appeal. Reasoning: to ascertain the terms of the contract, have to apply an objective rather than subjective test. It depends on what the court objectively considers that the words used by the respective parties must be reasonably taken to have meant. The contract was, plainly a contract by the defendant to perform that particular operation. As to warranty, the reference to irreversibility simply meant the operative procedure in question is incapable of being reversed. It cannot be reasonably construed as a representation that the operation is bound to achieve its acknowledged object. Applying Moorcock, an term can only be implied if it necessary to give efficacy to the contract – there was no doubt that the plaintiff would be entitled to believe defendant was warranting that the operation would be performed with care and skill. ‘In the absence of any express warranty the court should be slow to imply against a medical man an unqualified warranty as to the results of an intended operation, for the very simple reason that, objectively speaking, it is most unlikely that a medical man would intend to give a warranty of this nature’ Authority: In order to interpret a contract for medical services, consider what the reasonable bystander would have taken the words used by the parties to have meant. Contractual terms will only be implied if they are necessary to give business efficacy to the contract for medical services. Thake v Maurice [1986] QB 644 Facts: The plaintiff, Thake and wife had a consultation with defendant, Dr Maurice. Defendant did not advise the plaintiff that after the vasectomy, recanalisation could occur and that the plaintiff could have children again. The plaintiff signed the contract and the operation was performed competently. However, couple had further children. Issue: Plaintiff and wife sued for breach of contract, with damages for the distress of discovering the pregnancy and the costs of birth and maintenance of the child until adulthood. Plaintiff’s wife also sued for pain and discomfort. Held: Dismissed on appeal Reasoning: The object of the operation was to render Thake sterile and incapable of parenthood. The contract contains an implied warranty that in carrying out the operation, the defendant would exercise the ordinary skill and care of a competent surgeon. It did not contain an implied warranty that come what may, the objective would be achieved. A physician cannot objectively be regarded as guaranteeing the success of any operation or treatment unless he says as much in clear and unequivocal terms. The defendant did not do that in the present case. Authority: A contract for medical services is contained in both the conversation between the parties and in any relevant consent form. Contracts for medical services contain an implied warranty that the physician will exercise reasonable care in the provision of medical services to the patient. LAWS5126 Medical Law | Exam Notes 5 Battery – (Medical Law as Tort Law) The elements of battery 1. Direct action by the tortfeasor (the medical examination or treatment of the patient by the physician) – Reynolds v Clarke (1726) 93 ER 747; 2. Intentional action by the tortfeasor (the physician’s choice to provide medical services to the patient); 3. An application of force by the tortfeasor to another (any physical contact), even the least touching can constitute an application of force: Cole v Turner; 4. A lack of consent to the action by the tort victim (usually a defence). Hostility by the tortfeasor is not an element – Re F [1990] 2 AC 1 (Lord Goff). The causation of damage as a consequence is not an element – it is actionable per se. Consent In Re F (Lord Donaldson) – ‘In the absence of consent all, or almost all, medical treatment and all surgical treatment of an adult is unlawful, however beneficial such treatment might be. This is incontestable.’ Elements of Consent 1. Volition – the decision to consent must be a free one; 2. Information – the patient must have explained to him information about the procedure; 3. Capacity – the patient must possess sufficient age and intelligence. Volition In order to provide valid consent, the patient must make the decision of her own volition Modern approach – volition is not vitiated simply because patient is in a vulnerable position Beausoleil v Sisters of Charity Facts: B had discussion with Dr Cusson, where B requested a general anaesthetic, not a spinal. Cusson was prepared to operate under either and agreed and told his patient that she should advise the anaesthetist. On the day of the operation, B was given a sedative and taken to the operating room. Dr Forest, chief anaesthetist then talked B into taking a spinal. Cusson came into the room and was advised the spinal anaesthetic had been administered. The operation was performed competently but patient became paralysed waist down. Issue: Plaintiff sued in battery claiming no valid consent had been given to the spinal. Held: Plaintiff’s claim upheld on appeal. Reasoning: In cases where there is no urgency the doctor for one reason or another is unwilling to render the services agreed upon by the patient the only course of action open to him is to withdraw. He may not overrule his patient and submit him to risks that he is unwilling and in fact has refused to accept. And if he does so and damages result, he will be responsible without proof of negligence or LAWS5126 Medical Law | Exam Notes 6 want of skill. Dr Forest had not discharged the burden that he assumed by taking the position that the defendant had consented to the change from the general to spinal anaesthetic. Authority: Volition is not vitiated simply because the patient is in a vulnerable position in comparison to the physician. It must be the case that for some other reason the patient’s freedom to consent or refuse medical services is overborne. Freeman v The Home Office (No. 2) Facts: Plaintiff (Freeman) was a psychiatric patient. Dr Xavier was psychiatrist in care. Xavier prescribed Stelazin orally but the patient refused treatment. After refusals to take oral medication, Xavier prescribed Serenace to be injected intra-muscularly. Further oral medication was spat out each time. Plaintiff contended this was done by force. A prison hospital officer contested the use of force and that only minimum effective force would ever be used. There was other evidence of the plaintiff’s refusal to take electro-convulsive therapy and tooth extraction was respected. Issue: Plaintiff sued in battery claiming he had not provided valid consent. Held: Plaintiff’s claims were dismissed. Reasoning: There was ample evidence to justify his finding of fact and accordingly the decision to which he came. TJ also took into account a prison setting where a doctor has the power to influence a prisoner’s situation and prospects. Authority: A prisoner has sufficient volition to consent to or refuse medical services of a prison hospital officer. Being in a circumstance of vulnerability is not enough. Information What information is relevant and needs to be explained to a plaintiff prior to treatment? Chatterson v Gerson [1981] QB 432 Facts: Woman who suffered chronic pain in the region surrounding a scar saw Dr Gerson for treatment. Dr Gerson recommended an intrathecal block to stop pain messages along the nerves. He mentioned a possible side effect of the procedure, but not the one suffered (loss of sensation in right leg and worse pain). She sued Dr Gerson alleging that the failure to warn of the risk sounded in damages for battery and negligence. Issue: Whether failure to advise of the relevant side effect vitiated consent by lack of information. Held: Plaintiff’s claims were dismissed on appeal. Reasoning: In order to vitiate the reality of consent there must be a greater failure of communication between doctor and patient than that involved in a breach of duty if the claim is based on negligence. Once the patient is informed in broad terms of the nature of the procedure which is intended, and gives her consent, that consent is real, and the cause of the action on which to base a claim for failure to go into risks and implications is negligence, not trespass. Of course, if information is withheld in bad faith, the consent will be vitiated by fraud. Example – boy admitted for tonsillectomy and circumcised instead. Plaintiff was under no illusion as to the general nature of what an intrathecal injection would be, and in the case of each injection her consent was not unreal. LAWS5126 Medical Law | Exam Notes 7 Authority: The test of ‘broad terms’ – is meant to distinguish between the physical intrusions involved in treatment and the attendant risks of undertaking that treatment. The first are within the nature of the treatment, the latter are more properly the concern of an action for negligence in failing to advise. The dividing line between risks that are incidental (not forming part of the nature of the treatment) and those side effects which are so serious as to alter the nature of the treatment is a fine one. D v S (1981) LS (SA) JS 405 Facts: Plaintiff experienced neck pain and headaches. Went to see defendant for treatment who advised of an operation to reduce breast size. Plaintiff asked about scarring and defendant drew up diagram which showed little scarring would be involved. Defendant said he had done a lot of these operations and that there would be no problem – a minor operation. Defendant did not mention any incisions around nipples or that they would be moved or use of drips or drains. Plaintiff woke up with unevenly relocated nipples, great pain and scarring. Issue: Was the plaintiff adequately informed so that any consent was real? Held: Plaintiff’s claims were upheld Reasoning: Defendant should have told the plaintiff that there would be incisions around the circumference of the areolae, that the incisions would require stitching, that there could be a loss of sensation in the nipples and the areolae, that there would be some permanent scars and that she would see drips and drains and she would have substantial pain. Had she been told all of these things she would not have sonneted and it follows her consent was not truly given. ----Margaret Somerville’s McGill article – ‘… only the unintentional non-disclosure of a risk that relates to the basic nature and character of an act would not be actionable in battery.’ --- R v Maurantonia [1968] 1 OR 145 Facts: Appellant was convicted of six counts of indecent assault. Appellant had made the following admissions: 1. That he was not a medical doctor and did not have any formal education or training and was not entitled to practise medicine; 2. That he represented to the public and specifically to the complainants that he was a doctor of medicine and licensed to practise; and 3. That the complainants consented to be treated or examined by him only because they believed he was licensed to practise medicine. Urged by appellant’s counsel that ‘nature and quality of the act’ have reference only to the physical touching, to which each complainant did consent. The fraud of the appellant was only fraud in inducement and not fraud in the factum. Issue: Was there valid consent given to the touching? Held: Appellant’s claims were dismissed Reasoning: ‘Nature and quality of the act’ should not be so narrowly construed as to include only the physical action but rather must be interpreted to encompass concomitant circumstances which give meaning to the particular physical activity in question. The touching was bound up with and consented to as a part of the medical treatment. If that to which they were subjected was not in fact of the nature of a bona fide medical examination or treatment then it was something entirely different to which they LAWS5126 Medical Law | Exam Notes 8 consented. Authority: Misrepresentations as to the nature and quality of an action (e.g. claiming that it is for a medical purpose when it is not) do invalidate consent and constitute battery. Issue of defendant as having qualifications/licensing is an issue of fact as to whether the touching is part of a bona fide medical examination. The weight to be given to qualifications and other relevant facts would depend on the circumstances. R v Mobilio [1991] 1 VR 339 Facts: The applicant, Mobilio, performed trans-vaginal examinations on several complainant women. The examinations were not requested by the referring physicians and were not clinically indicated. It was not apparent whether this was for the applicant’s sexual gratification. The applicant was convicted of several counts of rape and appealed. Issue: Had the complainants provided valid consent to the applicant’s examinations? Held: Applicant’s claim was upheld. Reasoning: If the prosecutrix has knowledge or understanding of what the act comprises, ie the fact of penetration, and of its character … then she has all that the law requires for capacity to consent … if a woman understands that a proposed act is an act of sexual intercourse she knows its nature and character. This knowledge is not affected by a mistake as to the purpose for which the man proposes to perform that act of known nature and character. Authority: Misrepresentations as to the nature and quality of an action (i.e. claiming a medical purpose when it is not) do not invalidate consent to medical services. R v Richardson (1998) 43 BLMR 21 Facts: Appellant Richardson was a registered dental practitioner but was suspended from practice. While suspended, she performed dental work on a number of patients. One patient complained to the police because she thought the appellant was under the influence. Appellant was charged with assault for practising whilst disqualified. Issue: Operating without a license for medical services vitiate consent? Held: Consent was real notwithstanding the appellant’s suspension. Reasoning: The patients were not deceived as to the nature and quality of the act involved, nor to the identity of the person performing the act. Authority: Misrepresentations as to the nature and quality of an action (e.g. claiming that it is for a medical purpose when it is not) do not invalidate consent to medical services. R v Naveed Tabassum [2000] 2 Cr App R 328 Facts: The appellant, Mr Tabassum, had asked several women to take part in what he said was a breast LAWS5126 Medical Law | Exam Notes 9 cancer survey to enable him to prepare a computer software package for sale to physicians. The three complainant women agreed to the appellant showing them how to carry out breast self-examination, which involved removing their clothes and allowing the defendant to feel their breasts. Each of the complainants said that they had only consented because they thought that the appellant had either medical qualifications or relevant training. The appellant had neither. There was no evidence of any sexual motive. The appellant was charged with three counts of indecent assault. The appellant appealed. Issue: Had the complainants provided valid consent to the appellant’s breast examination? Held: The appellant’s claims were dismissed at trial and on appeal. Reasoning: There was no genuine consent because the complainants had consent only to an act of a medical nature and not any other touching. The fundamental quality of the act performed by the appellant was so significantly different that it rendered any consent from the plaintiffs irrelevant. Authority: Deception as to the purpose of the touching (though not the nature) vitiates consent to medical services. Capacity In order to provide valid consent to medical services, the patient must have capacity. To have the capacity to consent to treatment, the patient must: 1. Have an actual understanding of the information provided by the physician; 2. Believe the information is correct; 3. Apply the information to his or her treatment choices. There is a legal presumption that adults are competent to consent to treatment. Emergency Emergency is a defence to battery except in cases where the patient has clearly not consented to the medical treatment. However, the medical treatment provided must be necessary and not merely convenient: A surgeon who removed a plaintiff’s diseased testicle during a hernia operation to prevent him from dying of septicaemia was held not liable in battery: Marshall v Curry (1933) 3 DLR 260. A surgeon who tied a patient’s Fallopian tubes and removed fibroid growth during a caesarean section was held liable in battery: Murray v McMurchy (1949) 2 DLR 422. Malette v Shulmann (1990) 67 DLR (4th) 321. Facts: Plaintiff, Ms Malette, was severely injured in a car crash and taken to emergency. Defendant Dr Shulmann determined it was necessary to administer a blood transfusion. Before this took place, a Jehovah’s Witness card was discovered on the plaintiff’s person and indicated that in no circumstances did she want to receive a transfusion. The physician continued with the blood transfusion on the basis that it was his conviction that it was his professional responsibility to administer the transfusion. Issue: The plaintiff sued the defendant in battery for administering a blood transfusion when she had refused consent. LAWS5126 Medical Law | Exam Notes 10 Held: The plaintiff’s claim was upheld. Reasoning: The patient’s right to bodily autonomy and the principle of informed consent extends to the patient’s right to reject a specific medical treatment or all medical services. ‘For the freedom [of patients to make choices concerning their medical care] to be meaningful, people must have the right to make choices that accord with their own values regardless of how unwise or foolish those choices may appear to others’. Just as the physician could not have disregarded a patient’s instructions given immediately prior to a procedure, the physician could not ignore a patient’s express wishes indicated in advance of the procedure. The plaintiff was awarded nominal costs and damages, as it was difficult for the court to calculate the position that she would have been in had the battery not occurred (she would have been dead). Authority: Emergency is not a defence to battery if the patient has clearly indicated that they do not consent to a medical treatment. Sharin Qumsieh v The Guardianship and Administration Board and Lance Pilgrim [1998] VSCA 45 Facts: The plaintiff, Q, was admitted to hospital for childbirth. Developed complications and Q required blood transfusion. Q was a JW and had an advance medical directive refusing a transfusion. Husband applied to have a guardian appointed for his wife, claiming she satisfied the criteria (e.g. had a disability and was unable to make decision herself). Defendant guardianship Board was not aware of the advance directive and granted the husband’s application. Plaintiff had the transfusion. Issue: Plaintiff sued Board in battery for appointing a guardian who authorised medical treatment contrary to express instructions. Decision: The plaintiff’s claim was dismissed at trial and on appeal. Reasoning: The Board’s function was to act on material provided at the date of application that the protected person satisfied the criteria for the appointment of a guardian. IN this case, the Board has reasonably been satisfied the criteria were met. QUESTION: 1. In what circumstances would a doctor find himself liable for committing an offence? 2. Consider the case of R v Patel (ex parte AG QLD) [2011] QCA 81 and Patel v R [2012] HCA 29. Queensland Criminal Code 1899 Section 288 ‘It is the duty of every person who, except in a case of necessity, undertakes to administer surgical or medical treatment to any other person or to do any other lawful act which is or may be dangerous to human life or health, to have reasonable skill and to use reasonable care in doing such act; and he is held to have caused any consequences which result to the life or health of any person by reason of any omission to observe or perform that duty’. Section 282 ‘A person is not criminally responsible for performing in good faith and with reasonable care and skill a surgical operation upon any person for his benefit, or upon an unborn child for the preservation of the mother’s life, if the performance of the operation is reasonable, having regard to the patient’s state at the time and to al the circumstances of the case.’ LAWS5126 Medical Law | Exam Notes 11 Bateman (1925) 19 Cr App R 8 at 13 (Hewart LCJ) – negligence for s 288 must go ‘beyond a mere matter of compensation between subjects and showed such disregard for the life and safety of others to amount to a crime against the State and conduct deserving punishment.’ R v Patel (ex parte AG Qld) [2011] QCA Facts: Patel was convicted on the basis of s 288. Prosecution submitted at trial, and judge accepted, argument that the failure of the duty was not the provision of management and care during the course of treatment, but rather the decision to recommend the procedures to victims at all. Issue: Was the trial judge’s construction correct? Held: The Court held that s288 encompasses “the whole management of the patient, to everything that is done in accordance with that management, and also to things which are not done as a result of a decision which is deliberately taken with regard to the management of the patient.” Patel v R [2012] HCA Issue: Was the QCA’s decision correct as a matter of interpretation of s 288? Appellant’s argument: Section 288 deals with the actual performance of surgery or the provision of medical treatment, it does not refer to a decision or recommendation to operate relies upon the words "or to do any other lawful act" and "in doing such act". The physical sense of the word "act" does not, in the appellant's submission, accommodate any anterior decision to operate. Held: Surgical treatment refers to all that is involved, from a recommendation that surgery should be performed, to its performance and the post-operative care which is necessary to be given or supervised by the person who conducted the surgery. The duty imposed by s 288 may be breached by a discrete act of gross negligence in carrying out the surgical procedure or if gross negligence attends the making of judgments about a patient's condition and the risks to the patient of the surgical procedure. Note: Appeal was granted on the basis of prejudicial evidence being led to make out grounds of offences later abandoned by the prosecution. Negligence – (Medical Law as Tort Law) The elements of negligence LAWS5126 Medical Law | Exam Notes 12 In the context of medical law, the three elements of negligence are: 1. The existence of a duty of care (the physician’s duty to take care towards/of the patient); 2. Breach of a duty of care in comparison to the ‘standard of care’ (the physician’s failure to meet the standard of care required of medical services in the circumstances); 3. Causation between the breach of the duty of care and the damage/’reasonable foreseeability’ (damage as a consequence of the physician’s breach of the duty of care to the patient). Duty of Care Does a doctor owe a duty of care? Bolam v Friern Hospital Management Committee [1957] 1 WLR 582 Facts: The plaintiff, Bolam, suffered severe depression and had voluntarily sought treatment at a psychiatric hospital administered by the defendant. P agreed to undergo electro-convulsive therapy. He was not given any muscle relaxant prior to the procedure, and his limbs were not restrained. Plaintiff convulsed and suffered fractured bones. Competing evidence put forward of hospital practice. Issue: The plaintiff sued the Committee in negligence for not issuing muscle relaxants, not restraining him, AND not warning him about the risks involved. Held: The plaintiff’s claim was dismissed at trial. Reasoning: A physician satisfied his or her duty of care to a patient ‘if he [or she] exercises the ordinary skill of an ordinary competent man exercising that particular art … in the case of a medical man, negligence means failure to act in accordance with the standards of a reasonably competent medical men at the time. That is a perfectly accurate statement, as long as it is remembered that there may be one or more perfectly proper standards; and if he conforms to one of those proper standards, then he is not negligent … A man is not negligent if he is acting in accordance with such a practice, merely because there is a body of opinion who would take a contrary view.’ (McNair J). Authority: The standard of care must be that at the date at which the negligence is alleged to have occurred. May be more than one reasonably accepted proper method but provided practitioner acts in accordance with ONE, then no negligence. PROVIDED it is not contrary to the substantial part of the whole informed medical opinion. Roe v Minister of Health [1954] 2 QB 66 Facts: The plaintiff, Roe, underwent surgery at a hospital managed by the defendant. Before entering the operating room, an anaesthetic was administered through a lumbar puncture. As was common practice at the time (1947), the anaesthetic was stored in glass ampoules placed in carbolic acid. Unknown to the staff, the glass had micro cracks which were invisible to the eye but allowed phenol to penetrate. When used, the contaminated anaesthetic caused permanent paraplegia. Medical practices had changed considerably by trial date. Issue: The plaintiff sued the defendant alleging negligence for not colouring the carbolic acid with de and in cracking the ampoules. Decision: Plaintiff’s case dismissed at trial LAWS5126 Medical Law | Exam Notes 13 Reasoning: ‘Every surgical operation is attended by risks. We cannot take the benefits without taking the risks. Every advance in technique is also attended by risks. Physicians have to learn by experience, and experience often teaches in a hard way. Something goes wrong and shows up a weakness, and then it is put right. That is just what happened here. The physician sought to escape the danger of infection by disinfecting the ampoule. In escaping that known danger, he unfortunately ran into another danger. He did not know that there could be undetectable cracks, but it was not negligent for him not to know at that time. We must not look at the 1947 accident with 1954 spectacles’ (Denning). Authority: The standard of care must be that at the date at which the negligence is alleged to have occurred. Application: Dwan v Farquhar [1988] 1 Qd R 234. Dwan v Farquhar [1988] 1 Qd R 234 Facts: Man had contracted AIDS undergoing procedure in 1983. As at the date of trial, it was well known that a medical practitioner would know the risks of transacting AIDS from a blood that had not been screened and tested. Authority: Need to judge the standard of care as available at the time of wrongdoing. Physician’s duties of care to strangers/non-patients Physicians may have duties of care to people that they have no previous physician-patient relationship with: Lowns v Woods (Unreported, NSWCA, 5 February 1996). o Departure from basic rule of no duties upon bystanders. Lowns v Woods (Unreported, NSWCA, 5 February 1996) Facts: Mrs Light mother of plaintiff Patrick Woods who suffered a seizure while out walking. Mrs Light sent son Harry for ambulance and Joanna to nearby doctor’s surgery about 300 metres away and arrived within 5 minutes. Joanna’s evidence was that she spoke to Dr Lowns and asked him to come up as her brother was fitting, but that the defendant repeatedly refused and advised her instead to call an ambulance (which her older brother already had done). Patrick was not a patient and Dr Lowns did not know anything about Patrick’s condition other than what Joanna told her. The ambulance was delayed and Patrick suffered brain damage. The defendant conceded that if the conversation had occurred, he would have breached his duty of care to Patrick – he claimed that it didn’t. Issue: Did the defendant owe a duty of care to Patrick? Held: The plaintiff’s claim was dismissed at trial but upheld on appeal. Reasoning: In general, the CL does not impose a duty on a person to assist another in need of help – even where damage is reasonably foreseeable. Something other than foreseeability of harm is required before the law imposes a duty to intervene. Further, a physician is not under a duty to attend to a person, even in an emergency, if the physician has no pre-existing relationship with that person. However, the physical proximity of Joanna and Patrick to Dr Lowns and the fact that Lowns was an adequate physician to whom a direct request for assistance was made, created as sufficiently proximate relationship that the defendant had a duty of care to attend to Patrick. Authority: A physician who is in a reasonably proximate relationship to a person in need of medical attention has a duty of care to that person. LAWS5126 Medical Law | Exam Notes 14 Note: This case was decided when proximity was still considered in ascertaining the existence of a duty of care. Proximity is no longer required for a duty to exist – could be decided differently today!! Move away occurred in Woolcock Stores Investments. Lowns has been recently applied in a WA Medical Tribunal case. Much clearer when patient presents for treatment at an emergency ward. Once a patient is ‘seen’ as a patient by attending staff, a duty of care clearly arises: Barnett v Chelsea and Kensington Hospital Management Committee. NOTE: Fleming detects an increasing trend away from the ‘laissez-faire approach of the common law’, which ‘shrank from converting the law into an agency for forcing them to help each other’, towards a sense of ‘heightened social obligation and other communitarian tendencies’. But still, the distinction between non-feasance and misfeasance endures, and there is no general duty of care in the former case. Duties of care are also owed to beyond patients – if a request for examination comes from employer/insurance company, the doctor owes a duty similarly to those requesting: Thomsen v Davison (1975) Qd R 93 Principle: Doctor who undertakes examination of a person merely in order to asses state of health has a duty of care not merely to his employer, but also to that person to conduct the examination competently and not do or omit anything in the course of performing the examination which is likely to cause the latter damage. Stokes v Guest, Keen and Nettleford (Bolts and Nuts) Ltd [1968] 1 WLR 1776 Principle: A factory medical officer was under a duty to institute six-monthly medical examination of certain employees, given his knowledge of the risk to those employees of contracting cancer from the work in which they were engaged. Lindsey County Council v Marshall [1937] AC 97 Principle: HL held defendants liable for negligently failing to warn the plaintiff of the risk of infection by puerperal fever when she was admitted to their maternity home, following a recent outbreak of the disease. Evans v Liverpool Corporation [1906] 1 KB 160 Similarly, if a doctor negligently discharged an infectious patient form a hospital and, as a result, a third party contracted the disease, the doctor would undoubtedly owe a duty of care to the third party. Extent of the duty to third parties? BT v Oei [1999] NSWSC 1082 Facts: AT diagnosed with Hep B following tests by GP, Dr Oei. AT advised Hep B could have been acquired via unprotected intercourse and he provided information to AT about safe sex. AT brushed it LAWS5126 Medical Law | Exam Notes 15 off as he would ‘have no energy for it’ and did not mention that he had a partner. Dr Oei never aware. AT presented intermittently over 12 months for viral illnesses and diagnosed with liver condition. AT saw another specialist who diagnosed HIV positive. AT dies of liver failure, plaintiff BT (partner) also diagnosed HIV positive and attributes that to interaction with AT. Issue: Plaintiff sues the defendant in negligence alleging failure to diagnose AT’s HIV infection and failing to give proper counselling and advice to AT of the need for HIV antibody testing. Decision: The plaintiff’s claims were upheld. Reasoning: There was no conflict between the duty owed by the defendant (e.g. of confidentiality) to AT and BT as the two were coincident; BT was a sexual partner of AT and it was reasonably foreseeable that AT, if HIV positive, would transmit the virus to a sexual partner; AT was unaware of his HIV status; the defendant’s specialist medical knowledge and training equipped him to identify the risk that AT had contracted HIV, and the failure to diagnose and adequately counsel AT to undertake an HIV antibody test exposed AT’s sexual partners to the real risk of contracting a fatal disease. Authority: A physician may have duties to third parties, particularly if the duty to the third party does not conflict with the physician’s duty to the patient. 2 ways in which this case can be understood: 1. Doctor owes a duty of care directly to a 3rd party and has breached it by failing to advise AT to take precautions. 2. BT is a 3rd party, the Dr didn’t know of BT’s existence therefore wrong to owe a duty to someone who may not even exist. But Dr owes a duty of care to AT. If reasonable Dr would have ordered the HIV screen and breached duty of care and breach has caused damage to both AT and BT (who is not too remote). Harvey and Ors v PD [2004] NSWCA 97 Facts: The plaintiff, PD and future husband FH visited defendant GP Dr Harvey to have blood tests to confirm that neither of them were HIV-positive before marriage. PD was concerned that FH’s was at risk of having HIV because he was from Ghana. The blood tests were conducted: PD was HIV negative but FH was HIV positive. The defendant did not schedule any follow-up joint consultation, and when PD went to collect the results from the defendant’s receptionist, she was advised that she was only entitled to receive her own results. The defendant was legally prohibited from disclosing any information concerning the HIV/AIDS status of one patient to the other. In future consultations between FH and the other defendant GP Dr Chen, the defendant advised FH that HIV ‘kills’ but did not ask FH whether he intended to inform PD of his HIV positive status. PD then acquired HIV status from FH. Issue: The plaintiff sued the defendant in negligence, claiming that his management of the couple was inadequate. Held: The plaintiff’s claim was upheld at trial and on appeal. Reasoning: The defendants’ management of the couple was not in compliance with established practices. The defendants should have, in the course of the initial joint consultation, discussed the need for consent to disclose test results, the manner of disclosure, and the possibility of discordant test results. Authority: Although a physician has a duty of confidentiality, if patients come in for a joint LAWS5126 Medical Law | Exam Notes 16 consultation, the physician must discuss with them how to manage conflict of duties that could arise. Increasingly likely to see more liability owed to 3rd parties. Does standard of care very from city to country? – NO. Simpson J in Geissman v O’Keefe. Breach of Duty The standard of care: Pre 1992: Bolam v Friern Hospital Management Committee [1957] 1 WLR 582. In diagnosis, advice and treatment, the standard of care that a physician owes to a patient in medical services is the ordinary skill of an ordinary competent practitioner in that area. o Practitioner-centred test. 1992 – 2004: Rogers v Whitaker (1992) 175 CLR 479; Naxakis v Western General Hospital (1999) 197 CLR 269 In diagnosis and treatment, the standard of care that a physician owes to a patient in medical services is the ordinary skill of an ordinary competent practitioner in that area. In advice, the standard of care that a physician owes to a patient is to advise the patient of risks if a reasonable person in the patient’s situation would attach significant to that risk or side-effect, or if the physician is aware or ought to be aware that this particular patient would attach significance to the risk. What a ‘reasonably competent practitioner would have done’ does not bind the court. o Combination of practitioner and patient-centred tests. Post 2004 - Civil Liability Acts Restoration of the Bolam standard in all areas of medical practice except concerning the duty to advise of risks. (i) Failure to take a medical history Chin Keow v Government of Malaysia and Anor [1967] 1 WLR 813 Facts: Amah employed in KL hygiene clinic complained about ulcer on right ankle and swollen glands in thigh. Nurse took her to respondent, Dr Devadson who examined her and gave an injection of procaine penicillin, from which she died within an hour. It was admitted by Dr Devadson that he did LAWS5126 Medical Law | Exam Notes 17 not enquire into the deceased’s medical history. Evidence given of the possibility of developing hypersensitivity to penicillin. History would have revealed appellant’s prior adverse reactions. Held: Appellant succeeded, respondent liable in negligence. Authority: There is an ongoing duty for a health care practitioner to take a patient’s medical history and enquire as to the progress of medical treatment. Giurelli v Girgis (1980) 24 SASR 264 Facts: P went to see surgeon for treatment for broken leg. Plate was placed in the leg. P was a difficult patient and constantly complained about the quality of his treatment/hospital surroundings. Referred to physio about pain in his leg and complaints were not taken seriously. Day of discharge – was required to put weight on his leg. P refused as was in too much pain. His complaints were again ignored. P put leg on ground and waited for Dr. Eventually attempted and leg broke again in 3 places. Held: Dr liable in negligence for failing to listen and adjust to patient’s complaints of complications. Reasoning: Duty to undertake a medical history is ongoing. Duty to listen and consider a patient’s pain should have been an indication that the bone was not healing properly. Court also critical of amount of time Dr spent with each patient. Locher and Anor v Turner (Unreported, Qld SC, 22 Dec 1994) Facts: Plaintiff had complained to her GP of rectal bleeding when suffering of cancer. Complaints were ignored by the treating physician. Held: Plaintiff whose life expectancy reduced to 12 months awarded damages in negligence. Reasoning: GP should have listened to the complaint and ordered further tests, which would have revealed the presence of the cancer and would have allowed more successful treatment thereof. (ii) Causing an injury to patient during surgery Paton and Anor v Parker [1941] 65 CLR 187 Facts: P admitted to hospital for operation. Hospital was using ether for anaesthetic and operating theatre had a large radiator heater. Bottle was spilt and the exposed wires of the radiator ignited with spirit vapour. P sustained burns and sued in negligence. Held: Plaintiff succeeded in establishing negligence on the part of the anaesthetising surgeon. Reasoning: Legal duty on the part of the hospital authorities to exercise reasonable care to provide a suitable theatre and equipment. High standard of care owed to unconscious patient. Necessary therefore to take appropriate precautions to see that the patient was safe against explosion and fire in respect of the bottle falling on the floor and in the ether being administered. Duty to know of the danger of explosion if the ether became mixed with air. Leaving materials inside a patient not necessarily a case of res ipsa loquitur. LAWS5126 Medical Law | Exam Notes 18 Mahon v Osborne [1939] 2 KB 14 Facts: Mahon admitted to hospital for emergency surgery on a perforated duodenal ulcer. Shortly before, he had eaten lunch. During the operation, the defendant surgeon Dr Osborne used swabs to ‘pack off’ the adjacent organs in the patient’s abdomen. Theatre sister ‘flagged’ these swabs so that they could be more easily seen and counted the number of swabs used on a blackboard. The patient had a poor tolerance to the anaesthetic and anaesthetist was worried if the operation took too long the patient would die on the operating table. The defendant asked the sister if all the swabs had been removed. Told that they had, Dr felt the patient’s abdomen to check and asked assistant to do the same – none found so Dr closed up the patient. However, one swab was left in the abdomen, patient developed infection and died. Issue: P’s mother sued in negligence for failing to remove the swab (Lord Campbell claim). Held: Plaintiff’s claim upheld at trial but dismissed on appeal. Reasoning: ‘If a surgeon professes an art he must be reasonably skilled in it. There is no doubt the defendant surgeon was that. He must also be careful, but the standard of care that the law requires is not insurance against accidental slips. It is such a degree of care as a normally skilful member of the profession may reasonably be expected to exercise in the actual circumstances of the case in question. It is not every slip or mistake that imports negligence and, in applying the duty of care to the case of a surgeon, it is peculiarly necessary to have regard to the different kinds of circumstances that may present themselves for urgent attention … A few [circumstances] applicable to a major abdominal operation: The multiform difficulties presented by the particular circumstances of the operation; The condition of the patient and the whole set of problems arising out of the risks to which he is being exposed; The difficulty of the surgeon’s choice between risks; The paramount need of his discretion being unfettered if he thinks it right to take one risk to avoid a great; and At the penultimate stage (swab removal) he may, particularly where the patient has been taking the anaesthetic badly and is suffering from shock, be so anxious on surgical grounds to bring the operation to an end as rapidly as possible that, in the exercise of his discretion, perhaps unconsciously exercised, as soon as he has completed the removal of swabs of which he is at that moment aware he asks the sister for the count and forthwith starts to close the wound.’ – (Scott LJ). Authority: The standard of care is dependent on the context of the physician-patient relationship. Also, a physician who professes an art must be reasonably skilled at it. Compare: In Chasney v Anderson (1950) 4 DLR 223, a surgeon was found liable for the death of a child who died after choking on a sponge left at the base of his nostrils during a tonsillectomy. The surgeon did not use sponges with tapes attached, nor employed a nurse to count, but he and an assistant both did feel around for the sponge. Reconciling Chasney and Mahon? It is suggested that Chasney is the standard approach. In Mahon v Osborne, the Dr was presented with a case of exceptional circumstances – emergency procedures were done by a surgeon alone. Danger if they left it too long, plus risk mitigated by system of counting swabs and flags. Whereas in Chasney, a much more loose system was used with no flags/count. LAWS5126 Medical Law | Exam Notes o 19 view that Chasney is to be preferred reflected in later cases. Hocking v Bell o Part of a drainage pipe left in patient. Dr found liable. Gloning v Miller o Forceps left in patient. Dr found liable. Dryden v Surrey County Council and Stewart o Surgical gauze ‘plugging’ left in patient. Dr found liable. (iii) Errors in treatment Geissman v O’Keefe Facts: Woman slipped and twisted ankle in Wellington. Seen by GP who bandaged foot, rest and aspirin in August. In November, was a Dr in Mt Tambo who did x-rays. Diagnosed a torn ligament in the ankle with a spur (parts of bone attached to ligaments). Subsequently referred to ortho surgeon for assessment of the spur and applied plaster cast to ankle from 26 Dec – 11 Feb. Cast was removed – foot stank and was not healed – foot was stiff and defendant injected local anaesthetic and then cortisone. Later admitted to hospital for removal of the spur. Foot became more swollen and inflamed. Further operation found strange pus oozing from foot. Dr didn’t proceed with surgery because of infection risk. Prescribed anti-biotics, painkillers and discharged her. Condition became worse and P developed fever. Turned out anti-biotics ineffective as she actually had a very simple infection. Held: Judgment for the plaintiff Reasoning: There was no difficulty in identifying the errors in treatment – a reasonable Dr would have known to take a sample of the infection and have it typed to enable proper treatment. This did sound in negligence. Fouady v Marakboui v Western Sydney Area Health Facts: Woman rushed to hospital with spinal fracture and displacement of an arm and leg. Given an excessive dosage of opiate analgesics. This caused her breathing to become more shallow, and P subsequently developed pneumonia and heart problems Held: Dr was negligent. Reasoning: Court found Dr had failed to give appropriate treatment which fell below the standard expected of a reasonably competent medical practitioner. -------Not every failure in treatment is actionable in negligence!! Hancock v State of Queensland Facts: P went in for sterilisation procedure which failed, and P subsequently sued Dr in negligence. Held: Having carefully examined the facts, Court held that what happened was the miniscule risk of the rate of failure of that particular operation. This had occurred without negligence on the part of the surgeon. Authority: Failures in treatment sound in negligence only when the Dr has fallen below the standard of a reasonably competent medical practitioner. LAWS5126 Medical Law | Exam Notes 20 ------Sometimes the allegation is not that the Dr didn’t perform the operation negligently, but that it was totally competent. However, in the course of performance, a side-effect occurs without negligence. If that does happen, does the Dr have a duty to tell the patient that that side-effect has occurred? Should they therefore seek effective treatment to deal with that side-effect? Wighton v Arnot Facts: Surgeon practised in Inverell. Plaintiff developed a lump on right shoulder/neck and D operated on it three times. On the third occasion, D severed a nerve. Issue: Plaintiff sued Dr in negligence alleging that: 1. Surgeon failed to inform of suspicion of severed nerve; 2. Failed by appropriate examination to confirm that he had severed the nerve; 3. Failed to refer the plaintiff to remedial surgery. Held: Found surgeon liable. Reasoning: Defendant argued that he did submit the plaintiff for an appropriate test before she left the hospital and intended to check it again when she was supposed to return for a follow-up appointment. However, plaintiff never returned. Court nonetheless found the surgeon liable for failing to inform the plaintiff of his suspicion. By the time it came to light, it was too late to seek remedial treatment. Should there therefore actionable negligence even if the patient fails to show up for a subsequent appointment? (iv) Error in diagnosis The failure of a health care practitioner to diagnose a condition is not, per se, actionable. Patient also needs to prove that the failure to properly diagnose caused some loss to the patient. Causation therefore the necessary element – (e.g. where is the damage for failing to diagnose the flu?) Barnett v Chelsea and Kensington Hospital Management Committee [1969] 1 QB 427 Facts: A group of three night watchmen presented at the casualty department of a hospital managed by the defendant Kensington Hospital Management Committee, complaining of vomiting. The duty casualty officer declined to see them, advising them (via the duty nurse) to contact their general practitioners in the morning. However, one of the men died overnight of arsenic poisoning. Issue: The plaintiff (relatives of the deceased) sued the defendant in negligence for failing to attend to the three men. The defendants admitted that they had failed to attend, diagnose or treat the patient. However, on the basis of the evidence provided by a toxicologist, the defendants claimed that even if the physician had correctly diagnosed and treated the men, the deceased man would have died anyway. Held: The plaintiff’s claim was rejected. Reasoning: Even if the deceased had been attended, diagnosed and treated, the effective antidote to arsenic poisoning could not have been administered in time to save the patient’s life. LAWS5126 Medical Law | Exam Notes 21 Authority: An error in diagnosis is not causative of harm suffered by the patient if no effective treatment could have been administered anyway. Note: Following Lowns v Woods, here Drs employed in a hospital do have a duty to those whom aren’t current patients – hospital has its doors open to everyone and invite treatment. Content of the duty to attend and hopefully diagnose and potentially treat. Compare: Similarly, in Stacey v Chiddy (1993) 4 Med LR 345 and Smith and Another v Lennard (unrep, NSWSC, 7 Sep 1994), physicians who failed to correctly diagnose patients’ illnesses (breast cancer and stomach carcinoma respectively) were held not liable in negligence. Stacey v Chiddy Facts: Patient made allegations that if GP had made proper examination of her in an earlier diagnosis, her breast cancer could have been detected and avoided. Held: Trial judge found that the GP had been negligent in failing to make a proper examination of the woman’s breasts. He was also found negligent in failing to give the patient proper advice after she’d had a negative response to a mammogram and ultrasounds. TJ however went onto point out that malignancies that formed 15 months later were unrelated to the presence of earlier cysts which would have been detected by a competent examination and no causation was therefore established. Compare: - Stairmond v Baker – damages were awarded for a missed diagnosis of breast cancer. CA held that if the plaintiff had been early diagnosed, 7 more years of life and less pain and suffering and no chemotherapy. Smith v Lennard Facts: Patient presented with dysphagia. GP failed to request an endoscopy. That was in 1989. In 1993, an endoscopy of the patient revealed carcinoma of the stomach. Held: TJ determined that it was unlikely cancer would have detected by an endoscopy in 1989, even if the gastric reflux patient was experiencing could be attributed to carcinoma. COMPARE ABOVE AUTHORITY… Wood v Qld Medical Laboratories Facts: P visiting mother and stepfather in Brisbane. Became concerned about a mole on the left side of his back approximately midway of armpit and waist. Very small but boy noticed change in colour and went to see GP in Paddington. GP examined mole, excised it and sent it to the Defendants for pathology test. Path report came back saying no evidence of malignancy could be seen and excision was complete. This was in 1990. In mid-1993, boy moved to Mossman with grandmother and had for some time felt unwell – weight had fallen from 72kg to 65kg. Suffered from general tiredness and lack of energy. Not long after – noticed small lump in armpit. Saw GP in Mossman, gave him antibiotics but after 2 weeks, lump remained. Shortly after saw mother (nurse at Cairns Base). Saw Dr at that hospital on 13 August 1993. Admitted to hospital on 14 October 1993. Lymph node biopsy was performed revealing melanoma in 20/23 lymph nodes. Held: At trial it was held that if defendant pathologist correctly identified melanoma, the boy would LAWS5126 Medical Law | Exam Notes 22 have accepted surgery for which the prognosis was very good in 1990 but woeful in 1993. Laboratories were therefore liable in negligence. O’Shea v Sullivan Facts: Plaintiff in complained of having blood/bleeding after sex. Dr ordered pap smear and result came back, falsely, as negative. Pathologist was found liable and GP not found liable for not referring the patient, who had clearly indicated symptoms to a specialist. ------- What about a situation where performance is done competently, but in not informing of a side-effect, patient is deprived of ability to seek remedial treatment. Also looked at failure to diagnose. Flinders Medical Centre v Waller Facts: Woman experiencing numbness in legs and feet and back pain. She had decreased sensation below breasts and had ankle spasms. Seen by some specialists who decided she had MS. Turns out the diagnosis was incorrect and woman in fact had a spinal tumour. By the time the tumour was correctly diagnosed, it was too late to offer he effective treatment. Held: Found that the Dr fell below standard of a reasonable practitioner in diagnosis which denied the plaintiff a chance to seek efficacious treatment. (v) Failure to follow-up Medical practitioners have been found liable in negligence for not chasing up patients to advise them of adverse test results – Kite v Malycha, or failing to ensure that a patient is correctly entered onto a surgical list for medical treatment – Tai v Hatzistavrou. Kite v Malycha Facts: Plaintiff was referred to a surgeon after it was discovered she had a lump in her breast. Surgeon conducted a FNA (fine needle aspiration – insert small needle and drained liquid out). Surgeon did this and sent away liquid he had obtained to pathology lab for analysis. Told plaintiff to come back and see him. Was then some sort of mix up in terms of getting the results from the pathology lab back. Dr shared a common administrative area (one receptionist looking after other Drs) and surgeon never saw the pathology results. These indicated that the woman had a malignancy. Dr didn’t chase up or follow up what happened to the path results (no bring-up system). Plaintiff did not come back but went for surgery years later and found advanced cancer. Issue: P sued the Dr for failing to follow up the results. Held: Dr found negligent. Reasoning: Court established a duty of care. Necessary for a safe system of work for getting results back and needed a system of bring up. Needed a system of ensuring that there was a way of ensuring outcomes if he didn’t. Defendant sought that P was contributorily negligent. Court rejected this counter-claim: Patient is NOT REQUIRED to chase up a Dr or turn up for appointments. LAWS5126 Medical Law | Exam Notes 23 COMPARE… Tai v Hatzistavrou Facts: Defendant was a specialist gyno. Had rooms opposite hospital. He was consulted on a semiregular basis by the plaintiff who was concerned that she had heavy bleeding and pain. Concerned because a number of members of family had died of cancer. Referred for a procedure at the local hospital which involved examination of uterus and removal of some tissue for examination. Defendant specialist wrote out on a referral pad for the plaintiff. Plaintiff then took that form, crossed the road and gave it to the booking clerk. Plaintiff didn’t hear anymore from the hospital, and assumed that it was a public hospital and waiting lists were long. Defendant, having provided referral didn’t follow it up. Argued that it was P’s job to take it into hospital and chase up what was supposed to happen and supposed to be placed on specialist’s next list. Years later, the woman had bad cancer. Issue: Was the Dr negligent – should he have followed up and ensured she was placed on the booking list? Held: Dr was negligent for not following up. Reasoning: Woman would have had a better survival rate. Defendant argued that the plaintiff, having been given the form, had failed to lodge the form with the hospital and had done everything he could and woman’s responsibility to make sure she was on the surgical list. At trial it was revealed that the Hospital had lost the referral document and found it again – became clear that plaintiff had lodged the form with the hospital. In those circumstances, doctor was negligent for not following up, where his failure to do so posed serious consequences to the plaintiff. (vi) Failure to counsel patient who might be seriously ill, against leaving hospital Can you restrain a person when competent, and wants to leave emergency ward? Wang v Central Sydney Area Health Service & 2 Ors [2000] NSWSC 515 Facts: Plaintiff struck from behind while walking in Newtown. Taken to Royal Alfred Hospital at Camperdown. Plaintiff and mates waited and initially assessed but not seen by Dr. P didn’t speak good English and frustrated at what was happening at the hospital. At one point asked Nurse and was told a busy night have to wait but knew they were there. Hours passed and new nurse on duty – told again to wait. Got fed up and went to a local superclinic, was seen by Dr at clinic (private facility). Dr gave advice that it was in the plaintiff’s best interest to go to hospital for a scan. Friends got agitated and Dr then said to go home and get monitoring. If get symptoms, need to go to hospital. Plaintiff went home and was monitored and exhibited symptoms warned about (vomiting, dilation, slurring and unconsciousness). Ambulance was called and difficulties in communication between ambulance and his friends delayed return to hospital. Upon return – P had serious and irreversible brain damage. Issue: Was the hospital and superclinic respectively liable in negligence in respect of the way he was and was not treated? Should the hospital staff have attempted to dissuade the plaintiff from leaving? Held: Hospital liable in negligence and not the Superclinic. Reasoning: The primary duty which the hospital owed to the plaintiff was to assign him his appropriate priority through the triage system and to observe him in the waiting are in case his condition deteriorated. I am content to assume that no duty to provide him with medical services arose until he could be accommodated in the treatment area … In my view, that duty extended to furnishing the plaintiff with appropriate advice when it was intimated that he might leave the hospital. LAWS5126 Medical Law | Exam Notes 24 The hospital failed to discharge that duty, and the plaintiff’s present condition is attributable to that failure. Superclinics not liable as it was impractical for the Dr on duty to undertake the observations (only Dr on call and only a receptionist to do a nurse’s duty). Superclinics Dr gave appropriate advice of recommending hospital and giving head injury advice at home as only a fall back position. (vii) Failure to properly train reception to detect and prioritise patients with urgent need Alexander v Heise & Anor [2001] NSWSC 69 Facts: Man suffering from severe headaches and contrary to normal practice he took medication provided to him by his wife. Man’s wife told him he needed to go see a doctor, the man dismissed it, the man’s wife made an appointment to see the wife’s doctor. The earliest appointment that could be made was in a week’s time. In the time between when the appointment was made, and the time of the appointment, the husband died of an aneurism. Issue: Did the doctor have a duty of care towards Mr Alexander, who had not previously consulted a medical practitioner of the surgery? Did the receptionist? And were both duties breached? Held: Although both Dr and receptionist owe duties, causation could not be established. Insufficient information provided by wife to alert the receptionist to the possibility of a serious illness and receptionist therefore acted reasonably in setting a later appointment. Reasoning: Once Mr Alexander’s symptoms were described to the receptionist, albeit by his wife, and an appointment was made, Mr Alexander became a patient of the practice and a duty of care was owed at least by the first defendant, Dr Heise. Receptionist also under a duty of care to ensure that a patient presenting with a possible urgent medical condition, that the patient is seen in a timely manner … It is my view that the first defendant had properly instructed the second defendant on the proper management of patients who present with complaints that may warrant urgent treatment. The second defendant was aware that the severe headache had subsided the next morning … In these circumstances the second defendant’s index of concern would not have been heightened. A medical receptionist acting reasonably and prudently would not have appreciated that Mr Alexander could have a life-threatening condition on the information provided. The risk of him suffering a grade V aneurism or some other life-threatening illness on what she was told by the plaintiff was not foreseeable. The first and second defendants did not breach their duty of care that they owed to Mr Alexander. Authority: Separate duties. Adequate guidelines would be instruction on duties and would produce list of phone calls/messages and if issue – go through with Dr. Need receptionist to be aware of matters requiring urgent attention and where there was a doubt she was to consult the doctor. She was also aware of how to assess a patient and explore the duration of the problems and the severity of the symptom. Causation and Necessary Legal Principles Traditionally, the test used at common law for causation was the ‘but for’ test. The High Court’s decision of March v Stramare, the High Court preserved the ‘but for’ test but also added the ‘common sense test’. (This test has caused some problems). LAWS5126 Medical Law | Exam Notes 25 Therefore, two tests: 1. But for; 2. Common sense. Generally speaking, the plaintiff must prove the damage was caused by the negligence. In addition, there is a requirement that the damage must not be too remote. The type or kind of harm involved must be reasonably foreseeable – The Wagon Mound (No.2). Before plaintiff can pursue their claim – there is a duty to mitigate their loss. If a plaintiff fails to mitigate their loss, the court will not give the full value of the un-mitigated loss. CES v Superclinics Facts: Plaintiff was a young woman who went to see doctor complaining of malaise, nausea and breast tenderness. Dr diagnosed her as having an underlying viral condition. She didn’t get better, but symptoms got worse. Dr ran a pregnancy test, woman was advised to call with results. When she did so, she was wrongly advised she was not pregnant. P went on holidays and Qld doctor diagnosed her with a pregnancy. Woman devastated – not ready for children. Gave birth to healthy baby and suffered from post-natal depression. Issue: To what extent was Superclinics liable in negligence? Had the plaintiff been told of her condition, she would have sought an abortion (which was permissible under law at the time where health risks to life of mother or child). P was a healthy and fit woman who carried child with few complications. Could not be said pregnancy caused risk to her life or health. Superclinics admitted duty of care and breach, but it would have been illegal for P to have an abortion and therefore P was not deprived of anything lawful (should not be able to do an unlawful act) -- Argued that P therefore suffered no loss. To the extent that she did, mitigation required her to do something like give her child up for adoption. Held: Court rejected the mitigation principle. Reasoning: The gestation period is 40 weeks, the law on abortions looked at whether the pregnancy poses a risk to life and health of the mother. The court said why not stop at 40 weeks? Clear with benefit of hindsight that taking the child to term caused serious risk to woman’s mental health, accordingly she could have sought a lawful abortion, she has been denied that opportunity therefore damages will flow. Unanswered questions: How far after the birth of the child does the illness have to manifest? What if the child turns out to be a teenage dirtbag? (viii) Failure to advise of material risks Rogers v Whitaker (1992) 175 CLR 479 Facts: Plaintiff had suffered a childhood injury where a stick went through her eye. Her eye was grossly disfigured, she consulted with Dr Rogers, an ophthalmic surgeon. Dr told her he could improve the sight of the bad eye and the physical appearance. She asked lots of questions, and as she went into surgery they asked her to tape over her normal eye because she was concerned about the loss of sight/any potential damage that may happen to her good eye. Dr performed the operation competently. But Dr failed to warn her of the risk of sympathetic opthalmia, 1:14,000. So plaintiff suffered consequential damage in both eyes, and went completely blind. She sued the Dr in negligence. LAWS5126 Medical Law | Exam Notes 26 Issue: Was the Dr liable in negligence for failing to advise her of a material risk? Adduced evidence that other ophthalmic surgeons would not have advised a normal patient of this risk either. Held: Plaintiff’s claim was upheld at trial and on appeal to the HCA. Reasoning: The duty of care of a physician to a patient is ‘a single comprehensive duty covering all the ways in which a physician is called upon to exercise his skill and judgment: it extends to the examination, diagnosis and treatment and the provision of information in an appropriate case’ (Mason CJ, Brennan, Dawson, Toohey and McHugh JJ). In relation to diagnosis, examination and medical treatment, the standard of care is the Bolam test: what would an ordinarily competent physician in that area of practice have done? However, in relation to the provision of information, the standard of care is different, and the physician must advise of a side-effect if a reasonable person in the patient’s situation would attach significance to that risk of side-effect, or if the physician is aware or ought to be aware that this particular patient would attach significance to the risk or sideeffect. The plaintiff had indicated that she was very concerned about losing sight in her left eye, so the defendant was aware that this risk would have been very significant for her. Notes: Material risks is not a medical activity – risk is material if “in the circumstances of the particular case, a reasonable person would if warned, be likely to attach significance to it, or it the medical practitioner is or should be reasonably aware that this patient would attach significance to it.” This is subject to therapeutic privilege – if disclosure would cause more harm than good then there is no requirement. NEED TO PROVE: 1. Doctor owes a duty 2. Doctor has breached that duty a. Risk was material or you as an individual attach significant to it. 3. AND, if the risk was disclosed would not have undergone the procedure. THE COURTS have been sceptical to accept this fact. (REMEMBER -- a ‘material risk’ is a risk or side-effect that a reasonable person in the patient’s situation would attach significance to, or one that a particular patient would attach significance to: Rogers v Whitaker (1992) 175 CLR 479.) Berger v Mutton Facts: Plaintiff, Mrs Berger, was an experienced surgery, trauma and oncology nurse who was employed as director of a nursing home. Plaintiff had recurrent abdominal pain and vaginal/rectal bleeding for two years. The plaintiff consulted the defendant Dr Mutton with a ‘real fear’ that she may have cancer. The defendant Dr recommended an examination under anaesthetic with dilation and curettage, and a diagnostic laparoscopy. The defendant claimed he followed his usual practice of advising patients of the risk of bowel trauma and perforation, but the plaintiff contested this. During the course of the examination, the plaintiff’s bowel was perforated and she was hospitalised for six days and developed PTSD. Issue: The plaintiff sued the defendant in negligence for failure to inform her of the material risk of bowel perforation. LAWS5126 Medical Law | Exam Notes 27 Held: Plaintiff’s claim was dismissed at trial. Reasoning: The plaintiff did understand the risk of bowel perforation during the procedure: she had relevant professional knowledge and experience, and also had had a similar procedure performed previously. Further, even if the plaintiff had been advised of the risks, her fear of having cancer was such that she would have had the procedures anyway. Authority: A patient who would have had the treatment even if the material risk had been disclosed cannot recover against a defendant for failure to disclose the material risk if it occurs. Bustos v Hair Transplant Facts: Man was concerned about thinning hair, uncle had thinning hair and recommended juri-flap hair transplant. Defendant Hair Transplant Centre claimed that he would follow his normal practice and gave a detailed explanation of the operation and the possible complications to the plaintiff, although the plaintiff contested this. The defendant performed the operation on the plaintiff. Plaintiff claimed he experience extensive scarring, a droop and excess skin on one side of his scalp, headaches, a psychiatric disorder, the breakdown of his marriage, the collapse of his restaurant and an inability to work. Issue: The plaintiff sued the defendant in negligence for failure to inform him of the risks which occurred. Held: The plaintiff’s claim was dismissed at trial. Reasoning: Even if the plaintiff had been warned of the risks and side-effects of the operation, he was, by his own evidence, ‘keen, if not desperate’, to have the procedure. The only thing that would have stopped the plaintiff from proceeding with the operation was if it was conveyed to him that his appearance would be worse after the procedure, which was not a reasonable prognosis at the time that the operation was performed. Authority: A patient who would have had the treatment even if the material risk had been disclosed cannot recover for failure to disclose the material risk if it occurs. --------It is clear that, in order to prove causation, the patient needs to prove that if he or she had been informed of the risk, he or she would have avoided the risk. This is not to say the patient needs to prove that he or she would not have had the medical procedure performed. Chappel v Hart [1990] HCA 55 Facts: The plaintiff, Mrs Hart, had a consultation with the defendant ear, nose and throat surgeon Dr Chappel, concerning a progressive throat condition that would eventually leave her voiceless. The plaintiff informed the defendant that she did not want to ‘sound like Neville Wran’ (the then Premier of NSW, who had a raspy voice). The defendant performed the surgery competently. However, the defendant perforated the plaintiff’s oesophagus during the surgery and she developed a mediastenitis infection, leading to her developing a raspy voice (this was considered a random event). The plaintiff provided evidence that if she had known of this risk, she would have gone to a more experienced surgeon and hat she would have delayed having the operation. Issue: Plaintiff sued the defendant in negligence for failure to advise of a material risk. LAWS5126 Medical Law | Exam Notes 28 Held: The plaintiff’s claim was upheld. Reasoning: The defendant’s failure to advise the plaintiff of this risk meant that she was deprived of the loss of opportunity to go to a surgeon who was more experienced and to delay the operation. Although the event that occurred was random, causation is a matter of common sense, and a more experienced surgeon would be less likely to have risks occur. Gaudron, Gummow and Kirby JJ – one reason for this conclusion is that a more experienced surgeon will perform with fewer risks, as a matter of logic. Gaudron J made clear distinction between the nature of the risk (which would always be present) and the degree of the risk (which would be reduced had a more experienced surgeon been in charge). Kirby J also noted that evidence demonstrated that the chance of receiving such an injury in another operation was miniscule. Gummow J once causation was establish said – “It would have been for Dr Chappel to show that Mrs Hart’s damages were to be reduced to reflect that possibility … that Mrs Hart would have sustained at some later date the injuries she complained of” – Dr Chappel did not plead his case in this way and instead tried to deny all liability due to want of causation. Authority: A physician’s failure to advise of a material risk that could occur even without negligence is negligent. Damages for loss of a chance? To be successful in negligence, we need to prove that on the balance of probabilities that damage has been done to you caused by a breach of duty of care and that the damage is not too remote. We know from Green v Chenowyth that if you can only prove 41% deprived, you cannot get 41% of the damages. Need to show balance of probabilities you will get 100%. If you cannot, you get nothing. When looking at the different approaches in Tabet v Gett, try to work out what the HCA is saying with loss of a chance being not inconsistent with general principles of negligence and Chappel v Hart in particular. Then ask, is Chappel v Hart a medical negligence case or a loss of a chance case? If it is a loss of chance – decided in the same way as Tabet and if it isn’t, why not? Tabet v Gett [2010] HCA 12 Facts: Appellant, Tabet, was a six-year-old child suffering from headaches, nausea and vomiting and was admitted to hospital. Dr Gett made a provisional diagnosis of chickenpox. On Jan 14, the appellant had a seizure and was then diagnosed with a brain tumour. She suffered irreversible brain damage as a consequence of intra-cranial pressure. Trial judge held that Dr Gett had been negligent in failing to discover the tumour at an earlier stage, but did not find that the appellant would have had, on the balance of probabilities, treatment available which would have avoided deterioration. He awarded damages on the loss of a 40% chance that she could have avoided that deterioration. The NSWCA allowed an appeal by the respondent. Issue: Whether or not the appellant could claim damages for the loss of a chance of more successful treatment. Held: The High Court of Australia held that the common law of Australia has never recognised the compensability of a mere loss of a chance simply where a breach of duty is established but without the LAWS5126 Medical Law | Exam Notes 29 establishment of causation of actual, physical injury. Reasoning: Kiefel J: - There was insufficient expert evidence to support the appellant’s claim that the brain damage that the appellant suffered may have been avoided or reduced by the administration of steroids [114]. - Even if the evidence had adequately addressed the possible effect of the earlier administration of steroids, the appellant would still have been unsuccessful because the common law does not recognise the loss of a chance of a better outcome as actionable damage [109]-[112] o ‘Expressing what is said to be the loss or damage as a “chance” of a better outcome recognises that what is involved are mere possibilities and that the general standard of proof cannot be met’ [143]. - The adoption of possible, rather than probable, causation as a condition of liability would be a fundamental change that would require strong policy considerations which were not evident [148], [151], [152]. - The change proposed by the appellant “would suggest, if not require, a degree of precision in the assessment of probabilities which is not part of the more liberal, commonsense, approach presently undertaken” ([150]). Further, the general standard of proof required in negligence actions is flexible and did permit a level of uncertainty in proof of causation, and that the common law has shown itself able to adapt appropriately to the challenges faced in a number of cases involving difficulties of proof [148-9]. - While Australia already recognises a loss of a commercial opportunity as actionable damage, this does not support a finding by the court that a loss of a chance of a better medical outcome should also be considered actionable damage [122]. When a commercial opportunity has been lost, it will often be readily apparent that the opportunity lost was of value in itself so long as there was a substantial, rather than merely a speculative, prospect of acquiring a benefit [124]. However, a loss of a chance of a better medical outcome only has value in relation to the injury or loss ultimately suffered by the plaintiff [124]. Gummow ACJ: - Similar conclusion to Kiefel J on the insufficiency of expert evidence to support the appellant’s claim [43-45]. The appeal to the High Court should fail on this ground alone [45]. - The traditional legal approach to causation issues reflects a carefully considered compromise between the competing interests of parties and that allowing a loss of chance action would shift the balance towards claimants [59]. Allowing such actions might increase the practice of defensive medicine in Australia and that this would involve costly testing procedures [59]. Loss of chance actions might remove analysis of the facts and law to a more abstract level, when the analysis should be focused on the actual harm suffered by the claimant and the possible causes of that harm [62]. - Rejected the argument that amending the law to recognise a loss of chance of a better medical outcome as actionable damage could be supported on the basis that the law already recognised that a loss of a commercial opportunity could be actionable damage [47]. Damage is essential in negligence actions, while an action for breach of contract exists at the moment the contract is breached [47]. Consequently, in a negligence action the issues of the existence and the causation of compensable loss cannot be established by reference to a breach of a previous promise to provide an opportunity [47]. Hayne and Bell JJ - The appellant did not demonstrate that the respondent’s negligence was a cause of her damage LAWS5126 Medical Law | Exam Notes 30 [65]. - Loss of chance actions should not be allowed as they would alter the balance struck between the competing interests of claimants and defendants [68]. o ‘The language of loss of chance should not be permitted to obscure the need to identify whether a plaintiff has proved that the defendant’s negligence was more probably than not a cause of damage ... The language of possibilities (language that underlies the notion of loss of chance) should not be permitted to obscure the need to consider whether the possible adverse outcome has in fact come home, or will more probably than not do so’ [69]. Heydon J - Similar conclusion to Kiefel J on the insufficiency of expert evidence to support the appellant’s claim. - It was significant that the trial judge assessed the loss of chance at 40% while the Court of Appeal assessed it at most at 15%; this significant difference in percentage figures suggested that the state of the evidence on this central issue permitted only speculative findings [96]. - Declined to consider the issue as to whether the law should permit a loss of chance action as such a resolution could not produce any consequences for the parties [98]. Crennan J: - Australian law should not permit recovery of damages where the breach of a duty of care results in the loss of a chance of a better medical outcome [100]. - Loss of chance actions might encourage defensive medicine,the increased practice of defensive medicine might adversely impact on the Medicare system and private medical insurance schemes, and that there might be a number of negative effects produced if there were to be a change to the basis of the liability of professional liability insurance of physicians [102]. - The change in the common law requested by the appellant was radical and was therefore the kind of change that should generally be made by Parliament [102]. Implications: It was noted by the Court that the claim was brought in negligence alone and not in contract. Had the claim also been brought in contract then damages, albeit only nominal damages, may have been available for the loss of the promised opportunity resulting from the breach. Therefore, on one view, contract should be pleaded, where possible, in a medical negligence claim. -------------------It had therefore been assumed that after Rogers v Whitaker, there were two tests in respect of the standard of care that applied for doctors. 1. Diagnosis and treatment was said to be the Bolam test: ‘breach if fall below the standard of the reasonably competent medical person’. 2. Advice of risks was the Rodgers v Whitaker standard. THEN CAME - Naxakis v Western General Hospital (1999) 197 CR 269 Naxakis v Western General Hospital (1999) 197 CLR 269 Facts: Mr Paraskevas Naxakis, the plaintiff, was a 12-year-old schoolboy who was involved in an altercation with a schoolmate and was struck twice on the head by the other boy’s vinyl school bag. He collapsed and was seen by a GP who referred him to the defendant Western General Hospital. The physician did not order a CT scan. The plaintiff was discharged. Subsequently, the plaintiff had a collapse at home and after being taken to a different hospital, it was found that he had a major intracranial bleed from a burst aneurysm. The aneurysm could have been diagnosed and treated if a LAWS5126 Medical Law | Exam Notes 31 CT scan had been ordered earlier. The plaintiff suffered brain damage. Issue: The plaintiff and his parents sued the defendant in negligence for failing to diagnose the aneurysm. Decision: The plaintiff’s claim was dismissed at trial but upheld on appeal. Reasoning: The standard of care is not necessarily what other competent physicians would have done in the circumstances; the ‘standard is not determined solely or even primarily by reference to the practice followed or supported by a responsible body of opinion in the relevant profession of trade’ – Gaudron J. It is ultimately for the court to determine, using common sense, what standard of care should be in medical diagnosis, advice and treatment. Authority: Rogers v Whitaker has been read the wrong way. While the Bolam test may often be influential in diagnosis and treatment, it is not binding on the court. It is up to the court to determine whether or not the practitioner has been negligent. Irrespective of what the profession says, it is a court-centred standard test. ------It is clear then that Naxakis extended the Rogers construction of a doctor’s duty consisting of a single duty of diagnosis, advice and treatment, and that Rogers standard would operate insofar as advice as to risks, whereas Bolam would continue to apply in respect of treatment and diagnosis (i.e. what would a reasonable general practitioner do?). In Naxakis, the court made the point that Bolam in no longer good law for diagnosis or treatment. HCA will be guided by advice of members of the profession in respect of diagnosis and treatment – however, they were not bound to follow that standard and it is up to the court to set the standard of what is reasonable. *** Pre – CLA at 1998 … DOES NOT MATTER WHETHER IT IS DIAGNOSIS, ADVICE OR TREATMENT. It is a matter for the Court to determine. ---Other cases on material risks: Karparti v Spira – preferable where possible that patient should be advised of risk in percentage terms if a known figure rather than “small risk” or “rare”. Vale v Ho – Doctor’s evidence preferred due to detailed notes. C.f. Locher v Turner where doctor had vague notes. ---- Cattanach v Melchior Appeal from the QCA to HCA Antecedent cases: CES v Superclinics o Court awarded damages, but not for the costs of maintaining child until it turned 18 Dahl v Purnell – p661 o Qld District Court allowed a claim for the birth of a child following a failed vasectomy. o Court awarded costs for birth of child and maintaining child until it hit the age of LAWS5126 Medical Law | Exam Notes 32 majority. o But allowed a set off for the benefits of having a child. Veivers v Connolly p662. o QSC awarded damages following the birth of a child who is severely disabled. The Dr had failed to diagnose that the patient was suffering from rubella when pregnant. MacFarlane – p662 o Denied damages until child hits age of majority. Facts: The plaintiff, Mrs Melchior, consulted the defendant gynaecologist, Dr Cattanach, concerning a sterilisation operation. The plaintiff informed the defendant that when she was 15, she had an appendectomy, in which the surgeon had also removed her right fallopian tube. The defendant performed a laparoscopic tubal ligation procedure on the plaintiff, involving the application of a Filshie clip to the plaintiff’s left fallopian tube. Four years after the procedure, the plaintiff became pregnant and gave birth to a healthy child. It transpired that the plaintiff had become pregnant because her right fallopian tube was intact, although it was convoluted and obscured by scar tissue. An ovum had transmigrated from her left ovary to her right fallopian tube, rendering her fertile. The plaintiff and her husband sued the defendant for breach of contract and negligence. The particulars of the negligence claim were that: the defendant had not warned the plaintiff of the risks of pregnancy after the operation; and/or that the defendant had not verified the removal of the plaintiff’s right fallopian tube by checking hospital records; and/or that the defendant failed to order a hysterosalpingogram (procedure that could have indicated the presence of two functioning tubes). At first instance, the plaintiff’s action for breach of contract was dismissed because the defendant had carried out the operation in the course of his duties at a public hospital. However, the plaintiff’s action for negligence, and specifically the third particular, was successful. The TJ held that the defendant should have advised the plaintiff to have a hystero-gram because the defendant could not be sure that her right fallopian tube had been removed, and if it had not, then her risk of becoming pregnant was 10 times higher than it would have been in a ‘normal’ sterilisation procedure. The TJ was also satisfied that the plaintiff had been advised of the increased risk of pregnancy, she would have had the hysterogram, the presence of her right fallopian tube would have been detected and appropriate precautions against conception would have been taken. The TJ awarded damages for birth and confinement and costs of raising the child to the age of 18. On appeal to the QCA, the court was divided as to the recoverability of the claim for the costs of raising the child to the age of 18. The majority held that although the plaintiff could recover damages for birth and confinement, she could not receive damages for the costs of raising the child to the age of 18. The defendants were granted leave to appeal to the High Court. Issue: Could the plaintiff recover the costs of maintaining the child to the age of 18? Held: Yes, the plaintiff could recover the costs of maintaining the child to the age of 18 – the defendants’ appeal was dismissed. Reasoning: The HCA referred to Dahl, Veivers and CES v Superclinics. The Court also referred to a Scottish case – Macfarlane v Tayside Health Board [2000] 2 AC 59, where damages were awarded for the birth of a child following a failed sterilisation procedure, but not for the costs of raising the child to the age of 18. That is, there were five possible findings for the court: LAWS5126 Medical Law | Exam Notes 33 1. No damages where a child is healthy and without disability or impairment (because a healthy child is a blessing); 2. Damages confined to the immediate damage to the mother (and loss of consortium to the father) plus any expenses and loss of earnings immediately consequential on the pregnancy and delivery, but excluding the costs of rearing the child; 3. Damages confined to the foregoing plus any additional costs of rearing a child born with a disability or to parents with a disability; 4. Damages in full for the reasonable costs of rearing an unplanned child to the age where the child might be expected to be economically self-reliant, whether the child is healthy or disabled or impaired, but with a deduction for the joys and benefits received, and potential economic support derived, from the child; and 5. Damages in full for the cost of rearing the child with no discounts for joys, benefits or support. The court chose the fifth option, with a 4:3 split: McHugh and Gummow JJ: o ‘[It is not] correct to say that the damage that the respondents suffered was the parentchild relationship or the coming into existence of the parent-child relationship … In the law of negligence damage is either physical injury to person or property or the suffering of a loss measurable in money terms or the incurring of expenditure as the result of the invasion of an interest recognised by the law … For the purpose of this appeal, the relevant damage suffered by the respondents is the expenditure that they have incurred or will incur in the future, not the creation or existence of the parentchild relationship’ [67]. o ‘The expression “wrongful birth” used in various authorities to which the Court was referred is misleading and directs attention away from the appropriate frame of legal discourse. What was wrongful in this case was not the birth of a third child to the respondents but the negligence of the appellants’ [68]. o ‘To suggest that the birth of a child is always a blessing, and that the benefits to be derived therefrom always outweigh the burdens … denies the widespread use of contraception by persons such as the respondents to avoid just an event. The perceived disruption to familial relationships by, for example, the respondent’s child later becoming aware of this litigation, is at best speculative. In the absence of clear and accepted understanding of such matters, the common law should not justify preclusion of recovery on speculation as to possible psychological harm to children’ [79]. Kirby J o ‘The notion that a child might be hurt emotionally following the later discovery that parents had sought sterilisation and had gone to court to recover damages for its failure to prevent the child’s birth is unconvincing. It is difficult to accept that children in today’s age learning such facts would not realise, if explained to them, that the claim was brought simply for the economic consequences of medical negligence and to burden the tortfeasor with (and spare the family of) such financial consequences. The experience of post-birth parental love will usually allay the hypothetical hurts attributed to hypersensitive children later learning that their births were originally unexpected’ [145]. o On the first option: ‘the “blessing” idea has a double aspect. First, it is said that the birth of a healthy child is a blessed event and cannot possibly constitute “harm”, “injury” or “damage” for which a person will be heard to claim in a court of law. To say otherwise, it is suggested, would require a court to postulate that it would have been better that the child concerned had not been born. That would be repugnant to the basic idea of the sanctity and value of each human life which every legal system … upholds. Secondly, if contrary to this proposition, there is harm, injury or damage of some kind, LAWS5126 Medical Law | Exam Notes o o o o 34 it cannot sound in monetary damages because the blessing of such a child will always overwhelm the burdens so as to expel any right of financial recovery. On this theory, “after the birth of a normal healthy child the injury is entirely healed” [147]. ‘These arguments are equally unconvincing. The notion that in every case, and for all purposes, the birth of a child is “blessing” represents a fiction [that] the law should not apply to a particular case without objective evidence that bears it out. In any event, it is not the birth of the child that constitutes the harm, injury or damage for which the parents sue. Instead, it is for the economic harm inflicted upon them by the injury they have suffered as a consequence of the negligence that they have proved’ [148]. On the second option: ‘The difficulty with this reasoning is that severing the causal link between various outcomes of the pregnancy is incontestably arbitrary. Both kinds of damage are equally foreseeable as a consequence of negligence. Each is directly caused. Neither is too remote’ [161]. On the third option: ‘This differentiation is also arbitrary and therefore unacceptable as a statement of the CL. In Aus, even the use of the description of such parents as “afflicted with a handicapped child” would be offensive to most such parents and contrary to their attitudes about themselves, their child and others’ [164]. ‘It reinforces views about disability and attitudes towards parents and children with physical or mental impairments that are contrary to contemporary Australian values reinforced by the law’ [166]. On the fourth option: ‘No-one until now has suggested that the damages of a negligently injured worker or pedestrian, totally incapacitated for work, should be reduced to allow for the fact that the injuries have resulted in a kind of benefit – having relieved the injured person from the obligation to answer the morning alarm or the necessity to travel to work on a cold day. Any such “benefits” and “joys” as a result from unplanned and undesired idleness are treated by the law as too remote or of a different character so that they are not offset but ignored’ [173]. On the fifth option: ‘The supposed reasons for departing from the general rule of the CL have been variously explained. In so far as they relate to a suggested disproportion between the original wrong and the cost burden imposed as a consequence, this is unconvincing and unprincipled, but least so far as legal analysis is concerned. In many cases, especially those involving vulnerable people, the damages recoverable may bear little relationship to the degree of the tortfeasor’s initial culpability’ [177]. Callinan J: o ‘The respondents are entitled to be compensated for the costs they are likely to incur in rearing the child until he is 18 years old which is all that they claim. IN this case, the claim as formulated was a reasonably simple one … The reciprocal joy and affection of parenthood can have no financial equivalence to the costs of rearing him. One is no substitute for the other. There is no reason to suppose in any event that the reciprocal bonds of obligation and affection will be any the less if the parents are compensated for the cost of bringing up the child’ [298]. o ‘The appellants were negligent. The respondents as a result have incurred and will continue to incur significant expense. That expense would not have been incurred had the first appellant not given negligent professional advice. All of the various touchstones for, and none of the relevant disqualifying conditions against, an award of damages for economic loss are present here … No identifiable, universal principle of public policy dictates any different result. The damages are not indeterminate. That they should be awarded is also consistent with the underlying notion that their availability in tort serves as a measure of deterrence of tortious conduct’ [299]. Gleeson CJ (in dissent): o ‘The CL has always attached fundamental value to human life; a value originally based upon religious ideas which, in a secular society, no longer command universal assent … However, in this context, the concept of value is ethical, not economic. It does not LAWS5126 Medical Law | Exam Notes o o o 35 depend upon the benefits, tangible or intangible, that some children bestow upon their parents. It may be assumed that most children enrich the lives of their parents. But, in the eyes of the law, the life of a troublesome child is as valuable as that of any other; and a sick child is of no less worth than one who is healthy and strong. The value of human life, which is universal and beyond measurement, is not to be confused with the joys of parenthood, which are distributed unevenly’ [6]. ‘To say that, as a result of the birth of an unintended child, the parents have an extra mouth to feed, is true. But it is a small part of the truth. Except for people who live at the most basic level of subsistence, it is an obviously incomplete description of the consequences of parenthood. It is incomplete even as a description of the financial consequences. IT is not difficult to think of cases in which the birth of a child, and the formation of a parent-child relationship, could have serious effects upon the future earning capacity of a mother, or a father. There are parents for whom the costs of feeding and maintaining an unintended child would be of minor importance compared to other financial consequences. Furthermore, the financial consequences of the birth of a child may extend beyond those which directly affect the parents. The child’s siblings, for example, might be affected; in some cases, substantially. Their prospects of inheritance may be diminished. Or their parents may have less money available to them for financial assistance. The incongruity is said to lie in selecting, out of the lifelong, and manifold, consequences of the birth of a child, a few particular financial incidents of the parent-child relationship’ [9]. ‘The claim focuses only one aspect of the existence of a child, namely, the child’s financial needs until adulthood, and involves a partial and selective approach to the results of the child’s birth and existence’ [9]. ‘It is a feature of affluent societies that children remain financially dependent upon their parents for longer periods. Many children are supported by their parents well beyond the age of 18. The claim in the present case did not cut out at the age when attendance at school was no longer compulsory … Why it did not continue into a period of tertiary education is not clear. It was not restricted to items which [the plaintiffs] were legally obliged to provide. It included items of reasonable discretionary expenditure’ [20]. ‘The claim under consideration displays all the features that have contributed to the law’s reluctance to impose a duty of care to avoid causing economic loss. The liability sought to be imposed is indeterminate. It is difficult to relate coherently to other rules of common law and statute. IT is based upon a concept of financial harm that is imprecise; an imprecision that cannot be concealed by an arbitrary limitation of a particular claim in subject matter or time. It is incapable of rational or fair assessment. Furthermore, it involves treating, as actionable damage, and as a matter to be regarded in exclusively financial terms, the creation of a human relationship that is socially fundamental’ [29]. Hayne J (in dissent): o ‘The chief criticism of the blessing argument can be put in different ways … it imposes upon parties a paradigm of family life which may or may not be apt in the circumstances … there will be cases in which the birth of an unwanted child does put one or both of the parents of that child in circumstances which, whatever measure is applied, are worset than the circumstances in which that prent, or those parents, would have been but for the negligence of which the complain is made. The parent or parents are worse off economically, emotionally, socially and spiritually’ [169]. o ‘It is not self-evident that the feared consequences of harm to the child are likely, let alone inevitable. Much would turn on what was said on the subject, when and how, and on the nature of the relationship that had been established between parent and child both before and after these revelations were made … Recovery of damages which include the costs of maintaining the child may, in at lease some cases, make a considerable difference to the material well-being of the child. But for their recovery LAWS5126 Medical Law | Exam Notes o 36 the child may have faced the consequences of the parents’ financial hardship’ [203]. ‘The recompense obtainable by the parent should be confined to those matters which affect the parent alone: the pain and suffering of pregnancy and childbirth, and those costs of the failed procedure that have been thrown away. By adopting this rule, the law would refuse to regard a normal, healthy baby as more trouble and expense than it is worth. No less importantly, the law would refuse to allow a parent to seek to demonstrate the contrary’ [262]. Heydon J (in dissent): o ‘If parents are entitled to recover for the costs of rearing an unplanned child until 18 on the ground that they are legally obliged to maintain the child until that age, why are the not entitled to recover for the costs of maintaining the child after the age if it was the practice of that family to do so? Does the ambit of the damages extend to cover “everything that can reasonably be described as necessary for the upbringing of the child until the end of school, university, independence, maturity?” Parents often do maintain their children until well after the age of 18 – occasionally until death’ [309]. o ‘The various assumptions underlying the law relating to children and the duties on parents created by the law would be negated if parents could sue to recover the costs of rearing unplanned children. That possibility would tend to damage the natural love and mutual confidence which the law seeks to foster between parent and child. It would permit conduct inconsistent with a parental duty to treat the child with the utmost affection, with infinite tenderness, and with unstinting forgiveness sin all circumstances, because these goals are contradicted by legal proceedings based on the premise that the child’s birth was a painful and highly inconvenient mistake. It would permit conduct inconsistent with the duty to nurture children’ [404]. Summary of the Three Elements and Causes of Action 1. Contract a) – not ruled out entirely! It will be relevant where there is an action in negligence (and corresponding breach of an implied term). Difficulty due to implied terms not including ‘being cured’ unless expressly guaranteed by practitioner. Also limitations where public hospitals are involved. 2. Battery a) – Limited by the fact that once a patient is informed in broad terms of the nature of the procedure and gives consent, that consent it real and the failure to advise of risks relates to negligence and not battery. b) – Battery will be relevant where (i) the patient is not capable of giving consent (i.e. due to capacity); or (ii) where the patient gave consent to one procedure but a different one was ultimately performed. 3. Negligence a) – 3 elements: Duty, Breach and Causation of damage (which is not too remote) I. Duty: Clearly duty of care between doctor and patient but two difficult questions – when does that duty commence and to whom is that duty owed? LAWS5126 Medical Law | Exam Notes 37 II. Breach: Numerous categories of breach (e.g. failing to take medical history) focussing especially on diagnosis and treatment – failure to advise of material risks changed from Bolam to Rogers standard which was extended by Naxakis to apply beyond advice to diagnosis and treatment. III. Patient in a case regarding failure to advise of material risk must show that they wouldn’t have had the procedure anyway – BUT important gloss put on this by Chappel v Hart – only needed to show wouldn’t have undergone at that time. Four stages of negligence: 1. Pre-1992 – Bolam; Roe v Minister of Health (Dwan v Farqhuar) for diagnosis, advice and treatment. Causation is ‘but for’ and commonsense – March v Stramare. Remoteness of damage is Wagon Mound (No 2). 2. Post-1996 – Bolam for diagnosis and treatment; Rogers v Whitaker for advice. Causation is ‘but for’ and commonsense – March v Stramare Remoteness of damage is Wagon Mound (No 2). 3. Post-1998 – Naxakis Rogers v Whitaker applies to diagnosis, treatment and advice. Court centred test but medical profession’s advice is relevant. Causation is ‘but for’ and commonsense – March v Stramare Remoteness of damage is Wagon Mound (No 2). Damages claimable for wrongful birth (from failed sterilisations/pregnancy misdiagnosis) – Cattanach v Melchior; no duty to mitigate loss – CES v Superclinics. Don’t need to have undergone the procedure for material risks – just have it done by someone better or delay. Can make statements on this – Chappel v Hart 4. Post 1 December 2002 – CLA modified Bolam standard for diagnosis and treatment in s 22. Rogers for advice – s21. Causation is s 11(1)(a) ‘necessary condition’ and (2) relevant things Remoteness of damage is reasonable foreseeability (aka same as Wagon Mound (No 2). Perhaps wider though in s 11(4) – court have wide discretion to determine. No damages for wrongful birth (unless disabled or not ordinary expenses). 49A(2) CLA No ability to make statements vis-à-vis Chappel v Hart – s 11(3)(b) CLA LAWS5126 Medical Law | Exam Notes 38 The Civil Liability Acts Introduction Ipp Committee led by Justice David Ipp in response to perception that Australia had become too litigious. Cases considered by Ipp J included Chevron (drunk man walking across a road suing the bar); Allegation of woman in cinema seat not being warned about folding seat; Man suing after breaking neck diving into a sandbar. (1) CLA operates prospectively The CLA does not operate retrospectively. Civil Liability Act 2003 (Qld) in force from 2 December 2002. (per s 2). For incidents prior – the Common Law will remain authoritative. (2) CLA not entirely comprehensive For example – s 5 – excludes WorkCover from ambit of the Act. (3) CLA is not a codification of the law of negligence Section 7(5). The CLA makes modifications to part of the common law of negligence, but to the extent that they are unmodified, common law principles still apply. Duty of care under the CLA LAWS5126 Medical Law | Exam Notes Section 7(1) and 5: CLA does not create or confer any cause of civil action for the recovery of damages (2 exceptions to this in the section – N/A). o 39 CLA therefore doesn’t determine whether a duty exists – still need to look at Rogers and other case law to determine whether one does. Scope of the duty, however, is altered by the CLA. o s 20, s 21, s22 – etc. Breach under the CLA Separate provisions dealing with breach – either follow the s 9 path or the s 20/21/22 path. Section 9: establishing a breach is generally a three step process (three aspects of breach). 1. Work out ‘reasonable foreseeability’ – two sub-steps a. Section 9(1)(a): in order for there to be a breach, the risk must be something that the defendant was aware of or ought reasonably to have been aware of b. Section 9(1)(b): the risk has to be ‘not insignificant’ i. This is a change to the common law – under common law, Wyong v Shirt – the risk must not be ‘far-fetched or fanciful’ (Mason J). ii. The cases and the explanatory memorandum suggest that the test ‘not significant’ is a higher threshold (harder to satisfy) than not ‘far-fetched or fanciful’. 2. Standard of care a. Arises under s9(1)(c): requires that for there to be a breach of taking precautions against a risk of harm, a reasonable person in the position of the defendant would have taken precautions. i. This does not alter the common law position – CAN USE any common law cases about taking reasonable precautions for determining standard of care under s9(1)(c). 3. Factors indicating a breach – calculus of negligence a. Section 9(2) – four factors (court required to consider these factors in deciding whether a reasonable person would have taken precautions against a risk of harm): i. ii. iii. iv. Probability of harm; Seriousness of harm; Burden of avoiding harm; Social utility of the harmful activity. b. Statutory reflection of the calculus of negligence from Wyong. i. e.g. Tram example: 1. ¼ chance person over 80 has heart attack. Could install Dead Man’s Switch which is $1 per tram (total = $1000). LAWS5126 Medical Law | Exam Notes 40 2. 85 yo has heart attack. DMH has not been installed and tram runs over two pedestrians. 3. Probability = high; risk = high; burden of avoiding ($1000) = low; social utility = low. Causation under the CLA Two tests under the common law – ‘but for’ and ‘common sense’ after March v Stramare. Once prove causation – move to reasonable foreseeability of harm. CLA changes: o Section 12 – plaintiff has burden to prove on balance of probabilities, any fact relevant to causation. o Causation under s11(1)(a) = ‘factual causation’. Remoteness under 11(1)(b) now = ‘scope of liability’ – Wagon Mound (No 2) will still apply. s 11(1)(a) really the same as ‘but for’, just words change to ‘necessary condition’. o but exception to that in 11(2), which appears to bring in the commonsense approach (not entirely clear): “In deciding in an exceptional case, in accordance with established principles, whether a breach of duty—being a breach of duty that is established but which can not be established as satisfying subsection (1)(a)—should be accepted as satisfying subsection (1)(a), the court is to consider (among other relevant things) whether or not and why responsibility for the harm should be imposed on the party in breach.” o s11(3)(b)*** Deals with the circumstances of what the defendant would have done had he/she been warned. Says that in deciding it is to be determined ‘subjectively in light of relevant circumstances’. Statements made by the patient are inadmissible = major change to Chappel v Hart. o Courts trying to get around by saying ‘surrounding circumstances might lead you to those conclusions’. But patient cannot make statements about how they would change behaviour. o s11(4) – appears to widen the discretion of courts to determine whether the damage suffered was too remote: “among other relevant thing”. Doctors’ duties under the CLA Section 21 – Doctor does not breach duty of a patient to warn of a risk before P undergoes medical treatment, unless the doctor fails to give or arrange to be given to P the following information about the risk: o (a) – information that a reasonable person in the patient’s position would, in the circumstances, require to enable the person to make a reasonably informed decision about whether to undergo the treatment or follow the advice; o (b) – information that the doctor knows or ought reasonably to know the patient LAWS5126 Medical Law | Exam Notes 41 wants to be given before making the decision about whether to undergo the treatment or follow the advice. Restates, in a slightly modified form, the duty to warn from Rogers. Recall that Naxakis stated that diagnosis, treatment and advice were governed by court-centred standard, not just advice (as previously thought). Section 21 reverses the effect of Naxakis – only advice is governed by the modified Rogers standard. Everything OTHER than advice is governed by the modified Bolam standard: Section 22: o (1) A professional does not breach a duty arising form the provision of a professional service if it is established that the professional acted in a way that (at the time the service was provided) was widely accepted by peer professional opinion by a significant number of respected practitioners in the field as competent professional advice -- note subtle reference to Roe v Ministry of Health. o (2) ** However, peer professional opinion cannot be relied on for the purposes of this section if the court considers that the opinion is irrational or contrary to a written law. o (3) The fact that there are differing peer professional opinions widely accepted by a significant number of respected practitioners in the field concerning a matter does not prevent any one or more (or all) of the opinions being relied on for the purposes of this section. o (4) Peer professional opinion does not have to be universally accepted to be considered widely accepted. o (5) This section does not apply to liability arising in connection with the giving of (or the failure to give) a warning, advice or other information, in relation to the risk of harm to a person, that is associated with the provision by a professional of a professional service. Reversal of Cattanach v Melchior Section 49A(2): o Court cannot award damages for economic loss out of the costs of rearing a child. Section 49B: o Deals with failed contraception procedure or contraceptive advice. Note – ‘costs ordinarily associated’ = leaves open the ability to sue for additional costs in respect of a disabled child. LAWS5126 Medical Law | Exam Notes 42 Competency Capacity, Autonomy and Beneficence In order to provide valid consent to medical services, the patient must have capacity. Here, we refer to competence to consent to treatment (which would otherwise be a battery). There is a presumption that adults are competent to consent to their own medical treatment, but cases concerning patients who are children, mentally handicapped or mentally ill, are more complicated. The principle of patient autonomy (allowing patients to make their own medical decisions, even if those decisions contradict medical best practice) can conflict with the principle of physician beneficence (requiring physicians to maximize the health of patients, or at least, not to cause them harm). Competency assists in resolving the conflict between those principles; in cases of competent patients, physicians should respect patient’s autonomy, but in cases of incompetent patients, physicians should prioritise beneficence. The Definitions of Capacity The definition of capacity to consent to medical treatment is contested. LAWS5126 Medical Law | Exam Notes 43 Approaches to the definition of capacity to consent to medical treatment include: o the status approach: A patient who has a certain status (e.g. an adult) has capacity to consent to medical treatment. In Australia, this approach is now considered outdated because children’s ability to consent to medical treatment increases as they approach adulthood. NOTE: this approach has largely been abandoned o the functional approach: A patient who can evidence certain functions (e.g. expresses a choice; makes a reasonable choice; provides rational reasons for the choice; is able to understand information as complex as that required to make the choice at hand; or actually comprehends the information required to make the choice) has capacity to consent to medical treatment. In Australia, the actual comprehension functional approach has been adopted. Therefore the last of Roth, Meisel and Lidz’s five tests of competency is used = actual understanding. This is because there is a disjunct between an ability to understand information as complex at that at hand or actual understanding. But what is understanding? o 3 senses of understanding: ‘understanding how’; ‘understanding that’; ‘understanding what’. Understanding ‘that’ is the essential element – it is reducible to the knowledge of the truth of the matter and belief in it: ‘I understand that you are Catholic’. vis-à-vis understanding ‘what’ – a person doesn’t have to believe what they are told in order to understand what they are being told: ‘Made sense of the information but don’t believe it to be true – Sky falling on head’. Courts have applied ‘understanding that’ as the relevant standard for judging understanding. Australian courts have held that once patients are informed in broad terms about the nature of the medical procedure and provide consent, they have sufficient understanding and cannot complain that a battery has occurred: Chatterton v Gerson [1981] QB 432, affirmed in Rogers v Whitaker (1992) 175 CLR 479. An Application of the Understanding Approach Re C (Refusal of Medical Treatment) – Lord Thorpe Facts: Case concerned a 68 year-old man who was suffering from chronic schizophrenia. The man refused to have a clinically indicated amputation of his leg. Held: Decision-making analysis can be reduced to three stages: 1. Comprehending and retaining treatment information; 2. Believing it; 3. Weighing it in the balance to arrive at a choice. Further to which, there is arguably: 4. being able to communicate that decision (in some form). What is required to be understood to be competent? LAWS5126 Medical Law | Exam Notes 44 Courts both in Australia and England have followed Chatterson v Gerson. Bristow J: Once a patient was informed in broad terms of the nature of the procedure and gave her consent then the patient could not complain that a battery had been committed. That is the general test of competency – NOTE – it is higher for children. Further, there is a general presumption that every adult is of sound mind and has the capacity to refuse consent – Cardozo J in Schloendorff v Society of New York Hospital. Factors that impair competency? 1. Permanent factors; 2. Temporary factors. Temporary factors In Re T (Adult: Refusal of Medical Treatment) [1992] 4 All ER 649 Facts: Plaintiff, Ms T, was 34 weeks pregnant and admitted to hospital following an accident. The plaintiff had been raised by her mother (a Jehovah’s Witness) and although the plaintiff had never been a member of that religion, she was sympathetic to its beliefs. The plaintiff was diagnosed as suffering from pneumonia and was administered antibiotics, oxygen and pethidine. The plaintiff subsequently went into labour. After a period spent alone in the ambulance with her mother, the plaintiff advised the physician and the nurse that she did not want to receive a blood transfusion. The plaintiff was informed (incorrectly) that there were other medical procedures available and that a blood transfusion was often not necessary with a caesarean section. The plaintiff’s child was stillborn the following day, and the plaintiff was sedated and placed on a ventilator after the birth. A blood transfusion was clinically indicated, so the plaintiff’s partner sought a declaration that it would not be unlawful for the hospital to administer a blood transfusion. Issue: Had the plaintiff validly refused consent to the blood transfusion? Held: No, the plaintiff had not validly refused consent to the blood transfusion. Reasoning: The plaintiff had not been provided with correct information, so she had not been able to consider the true situation she was facing. Further, there were doubts as to her competency at the time she made the decision, due to the short-term effects of fatigue, shock, pain and drugs. ‘Prima facie, every adult has the right and capacity to decide whether or not he will accept medical treatment, even if a refusal may risk permanent injury to his health or even lead to premature death. Furthermore, it matters not whether the reasons for the refusal were rational or irrational, known or even non-existent. This is so notwithstanding the very strong public interest in preserving the life and health of all citizens. However, the presumption of capacity to decide, which stems from the fact that the patient is an adult, is rebuttable. An adult patient may be deprived of his capacity to decide either by long-term mental incapacity or retarded development or by temporary factors such as unconsciousness or confusion or the effects of fatigue, shock, pain or drugs’ (653) – Lord Donaldson MR. LAWS5126 Medical Law | Exam Notes 45 Authority: A plaintiff may not have provided valid consent to medical treatment if they are under the effects of fatigue, shock, pain or drugs at the time they make decisions. Re MB (Medical Treatment) [1997] 2 FLR 426 Note: Butler-Sloss LJ commented on Re T: ‘the temporary factors mentioned by Donaldson MR in Re T … may completely erode capacity but those concerned must be satisfied that such factors are operating to such a degree that the ability to decide is absent. Another such factor may be panic induced by fear. Again, careful scrutiny of the evidence is necessary because fear of an operation may be a rational reason for refusal to undergo it. Fear may also, however, paralyse the will and thus destroy the capacity to make a decision.’ Facts: Concerned a woman who was needle-phobic. Consented to performance of a caesarean but refused the procedure because the caesarean section would involve the use of a needle. Held: Court of Appeal noted that at MB’s moment of panic ‘her fear dominated all … at the actual point she was not capable of making a decision at all. She was at that moment suffering an impairment of her mental functioning which disabled her. She was temporarily incompetent’. Re L (An Adult: Non-consensual Treatment) [1997] 1 FCR 609 Facts: Same as Re MB Held: Kirkwood J applying the test of Thorpe J in Re C, noted that L’s extreme needle phobia amounted to an involuntary compulsion that disabled L from weighing treatment information in the balance to make a choice. Indeed, it was an affliction of a psychological nature that compelled L against medical advice with such force that her own life would be in serious peril. While there is no principle that just because a patient is suffering from a mental illness then he or she is incompetent, many of the recent cases have focused on patients suffering from mental illnesses. A patient with a mental illness or an intellectual disability which affects one of the capacities in Re C, may not be competent. Norfolk v W Facts: W arrived at hospital in an advanced state of labour. She dienied, however, that she was pregnant. An obstetrician recommended that either a forceps delivery or a caesarean setion should be performed. W was examined by a psychiatirist who was undecided whether W was capable of understanding and retaining information about the treatment. He note dtht she continued to deny that she was pregnant. The psychiatrist was equally unsure if she believed the information about the proposed treatments. The psychiatrist suggested W was unable to weigh in the balance the information provided to her. Reasoning: The trial judge noted that W ‘… lacked the mental competence to make a decision about the treatment was proposed because she was incapable of weighing up the considerations that were involved. She was called upon to make the decision at a time of acute emotional stress and physical pain in the ordinary course of labour, made even more difficult for her because of her own particular mental history’. LAWS5126 Medical Law | Exam Notes 46 But just because a patient has a mental illness doesn’t mean they are incapable of withholding consent. Secretary of State v Robb Facts: Respondent was a prisoner who suffered from an anti-social personality disorder. Despite the existence of this psychiatric disorder, the court established that he was competent to make his own decisions about medical treatment (including the provision of food and hydration) and that, therefore, his wish to engage in a hunger strike and starve himself to death had to be respected. Authority: A competent patient could refuse medical treatment extended to food and water. R v Collins; ex parte S (1998) ** Facts: Applicant was a 29 year-old woman who was 36 weeks pregnant. She suffered from preeclampsia. Medical advice was provided to her that she should be admitted to hospital and undergo a caesarean section. S refused to attend hospital. The local authority had her compulsorily admitted under s2 of the Mental Health Act 1983 (UK) and a declaration from the court was obtained to carry out ‘all necessary treatment’ on S. S’s baby was delivered by caesarean. Issue: S sough a review of her admission to hospital and of the declaration made in respect of her treatment. Held: Court of Appeal struck down the order Reasoning: Court of Appeal was scathing of the fact that a declaration had been made, and the use of the mental health legislation to detain someone whose views were thought to be bizarre or irrational. Approved the earlier statement of Butler-Sloss LJ in Re MB: ‘Every person is presumed to have the capacity to consent to or to refuse medical treatment unless and until the presumption is rebutted. A competent woman who has the capacity to decide may for religious reasons, other reasons, for rational or irrational reasons, or for no reason at all, choose not to have medical intervention, even though the consequence may be the death or serious handicap of the child she bears, or her own death. In that event, the courts do not have the jurisdiction to declare medical intervention lawful’. Note – Guardianship Boards are used in Australia instead of courts to address matters of competency. Permanent Factors These, as the name suggests, are ongoing. They are matters that affect, on an ongoing basis, someone’s ability to give consent to treatment. In a sense, that is a misnomer. Because the major group that they effect are children. One of the difficulties in this area of law is working out the test that applies to adults in terms of their actual understanding and protecting children from themselves. Unpalatable to allow children to make decisions that could to themselves harm. Uncomfortable balance putting lip service to principle of bodily autonomy but also providing detailed supervision. Court is saying: children in some circumstances can consent but Court retains supervisory jurisdiction. There are some things that parents nor children can consent to and Court must make a decision. For those reasons, the Chatterton test is NOT THE TEST THE COURTS USE WHEN LAWS5126 Medical Law | Exam Notes 47 DEALING WITH CHILDREN. Children Traditional view = no child could consent to medical treatment – entirely a matter for the parents. Changed in Gillick v West Norfolk Area Health Authority Gillick v West Norfolk Area Health Authority Facts: Department of Health/SS in UK issued guidance to its doctors on family planning services. Most doctors in the UK work for the NHS and therefore employees of the Government. NHS guidance stated that in exceptional circumstances, a Dr could lawfully proscribe contraception for a girl under 16 without parental consent. Gillick had 5 daughters below 16, wrote to DHSS and sought assurance that none of her daughters would be given contraception without consent. Held: Gillick’s claims were rejected. First Issue: Gillick sought declaration that the guidance was unlawful by virtue of facilitating unlawful conduct (underage sex). Reasoning: House of Lords held that the guidance was not the same as giving someone a gun. Child has already decided to have sex – merely ameliorating the side-effects. As if someone were shot and Dr arrived on scene to tend to the wounded criminal. Merely avoiding some of the negative consequences of unlawful activity. Second Issue (tort) – if we could say children could consent in some circumstances, what capacities must the child have? It was argued that the same approach b taken to children as adults – if child can understand in broad terms the nature of the procedure and apply it in his/her circumstances, then the child is competent – this was rejected by the House of Lords. Court stated that there were 3 possible decision makers – parent, child and court. Significance: The parental right to consent to treatment gradually dwindles over time as the child matures. Gillick Competency: Once a child has obtained sufficient maturity and intelligence to understand fully what is proposed, then that child is competent – until that time the parent retains the capacity in exceptional circumstances (emergency, parental neglect, abandonment of child or inability to find the parent). o Having regard to the reality that a child became increasingly independent as it grew older and that parental authority dwindled correspondingly, the law did not recognise any rule of absolute parental authority until a fixed age. Instead, parental rights were recognised by the law only for as long as they were needed for the protection of the child and such rights yielded to the child’s right to make his own decisions when he reached a sufficient understanding and intelligence to be capable of making up his own mind. Accordingly, a girl under 16 did not, merely by reason of her age, lack legal capacity to consent to contraceptive advice and treatment by a doctor. C.f. ‘understand fully’ (per Lord Scarman) with ‘in broad terms, the nature of the procedure’ from Chatterson v Gerson. LAWS5126 Medical Law | Exam Notes 48 Third Issue – Did the capacity to consent also include competency to refuse? Logically, the competency to consent to do something must also include competency to refuse. The House of Lords did not accept this logic. Competency to consent to treatment doesn’t necessarily mean that the child has capacity necessary to refuse treatment. Fallout from Gillick considered and applied in a number of cases… In Re R Facts: R = teenage woman, placed in care of local authority. Suffered from episodic mental illness that was controlled by drugs. Had an episode and told social worker that she didn’t like the drugs and didn’t want to take them any more. Issue: Was the woman Gillick competent to refuse treatment? Held: Court of Appeal decided that the capacity to consent to something did not necessarily include the capacity to refuse. Reasoning: CA described capacity as a flak-jacket to protect doctors from immunity from suit. Just because woman was competent to decide, didn’t mean she was competent to refuse. If she did, any one of parent, social worker could step in. This view was again taken in In Re W In Re W Facts: W was a woman with anorexia and unsubstantiated theories about what had happened to this woman to bring about her condition. Was going to be taken to a facility to be force fed which she didn’t want to happen. Issue: Was W Gillick competent? Held: Court of Appeal repeated the heresy – capacity to consent did not necessarily mean capacity to refuse. Reasoning: Consent is like a ‘key to a lock’. Only to unlock unlawful treatment. Initially, only a court/parent had the key to open. When the child became Gillick competent, she too was given the key. but even if she decided not to use it, it didn’t mean the court/local authority couldn’t use their own key to give consent. This was the state of English law and was to be critiqued in Marion’s Case. Secretary for Department of Health and Community Services v JWB (Re Marion) Facts: Marion suffered from severe mental retardation, deafness and epilepsy and at the date of appeal was 14 years old. Had severe behavioural problems and was totally unable to care for herself. Parents brought an application for the Court to authorise sterilisation procedures on Marion, or alternatively, LAWS5126 Medical Law | Exam Notes 49 that it was lawful for them as parents to consent to such a procedure for their child. Issue: Could parents consent to sterilisation of their child when it is not necessary for the purposes of saving life or protection from serious harm? Held: Court took a broader view of what children can consent to by way of medical treatment. Distinction between therapeutic and non-therapeutic treatment. Reasoning: Court made several important findings: First: Even in the case of parental consent … a parent may only consent to procedures that are in the best interests of the child. o Example – it would not be acceptable to maim a child to maker her a more efficient beggar. Second: Court explicitly adopted Gillick as good law for Australia. o Gave it a theoretical underpinning – which is to say that the Gillick test accorded from what we know about the growing abilities of children in developmental psychology. The Court therefore put an important gloss on the ability of either a child or a parent to consent: There are some procedures that are so serious that no child/parent competent could properly consent to. Court approval is therefore mandatory in these situations. Following factors are relevant: 1. Invasive, irreversible and major surgery; 2. Significant risk of making the wrong decision, either as to a child’s present or future capacity, or about what the best interests of the child are. 3. Whether the consequences of a wrong decision are particularly grave. Examples of procedures of Marion-level seriousness: Cardiac surgery on an 11 year old boy: Re Michael Harvest of bone marrow cells from a healthy 10 year old boy, to transplant into the child’s heart (to cure leukaemia): Re GWW and CMW Sex change surgery for a person under 18 years old: Re Alex Parlett and Weston-Scheuber, ‘Consent to Treatment for Transgender and Intersex Children’, (2004) 9(2) Deakin Law Review 375. There are a number of issues that arise form a consideration of the principles of child consent in the context of transgender and intersex children … o 1. Despite the Court’s endorsement of Gillick, are there in fact some types of treatment which are so serious in nature that a minor can never consent to them? Would gender reassignment and irreversible hormonal therapy fall into this distinction? o 2. Should a distinction be drawn between the capacity of a minor to consent to medical treatment on the one hand and her or his capacity to refuse consent to medical treatment on the other? o 3. How should the principles of child consent be applied in the special context of treatment for the transgender or intersex child, given the particular consequences which may result both from administering treatment and withholding it? LAWS5126 Medical Law | Exam Notes 50 In both Re A and Re Alex, the Court found that although the children possessed a general understanding of the kinds of treatment that were being proposed, they did not possess the requisite intelligence and maturity to give them the capacity to consent to treatment … if it truly is the case that some treatment is of such a serious nature, or the refusal of treatment would have such serious consequences, that a competent child’s right of consent or refusal should not be absolute, then that should be enunciated clearly as a matter of legal principle … The suggestion here is that there are some types of medical treatment which are so serious that even a child who has sufficient understanding and maturity to understand fully the nature of the treatment and the consequences of her or his decision, should not be allowed an absolute right to consent to that treatment. The English cases considered above appear to reflect the idea that although competent adults are entitled to consent to or refuse treatment as they see fit, regardless of the consequences, there should be some overarching protection of a Gillick competent child to shield her or him from the consequences of an unfettered right to decide whether or not to accept medical treatment. The language of s 67ZC fo the Act would appear to support the existence of similar unlimited parens patriae jurisdiction in Australia. In Marion’s Case, the majority stated that ‘more contemporary descriptions of the parens patriae jurisdiction over infants invariably accept that in theory there is no limitation upon the jurisdiction’. But given that the jurisdiction springs from the direct responsibility of the Crown for those who cannot look after themselves, it would seem illogical for it to extend to overriding the wishes of a competent minor. o Question of whether child has the requisite capacity needs to be clarified. Role of the court to determine and verify capacity or to ensure that the best interests are served regardless of the child’s competent wishes? It is potentially more significant to allow a child an absolute right to refuse medical treatment than it is to allow the child to consent to medical treatment, as the consent to treatment will only have effect if there is a doctor who is willing to administer the treatment or perform the procedure. o Best not to follow UK distinction. Despite the distinction between consent and refusal and the added protection that medical ethics provides to the patient in the case of the former, it still should not be presumed that the best interests of the child will always favour administration of treatment rather than absence – particularly relevant where the treatment is to deal with congenital adrenal hyperplasia and transgender children. o Ultimately, the procedures of the kinds addressed in Re A and Re Alex are special in that they are not simply for the purpose of curing an illness or improving health, but are inextricably associated with the patient’s self-identity. The consequence of not allowing treatment where that is sought or alternatively, of carrying out treatment where that is not wanted, can be terrible … Unresolved Issues 1. Situation where a woman under 18 presents at a Doctor’s surgery with her own child. LAWS5126 Medical Law | Exam Notes 51 a. Normal situation would be to ask parent for consent… i. but what if that parent is below the age of capacity? 1. Option of appointing a guardian under – Director of Community Services, or applying for parens patriae jurisdiction. a. not really satisfactory 2. Approach of Court of Appeal in In Re R and In Re W. a. McHugh held that they were probably decided wrongly in Marion’s Case. b. Balance of HCA silent. 3. Test from Gillick is woolly. a. What is the situation where Dr forms view that child is Gillick competent, but with hindsight that the child is actually not? b. Would liability flow in these circumstances? Information and Medical Practice Part 1 - Confidentiality Why keep information confidential? In society’s interests to ensure patients are comfortable talking to doctor, especially in cases of serious and communicable disease. Patient wants to feel comfortable in respect of highly sensitive information. Encourages people to seek treatment. Three sources of the right to a patient’s confidentiality: 1. Health care practitioner’s ethical obligations; 2. The contract between the patient and health care practitioner; 3. Implications of equitable principles. Equity Courts in Australia, New Zealand and the United Kingdom have recognised that a court of equity has an original, inherent and independent jurisdiction to prevent violation of a confidence. Therefore, equity will grant relief against an actual or threatened abuse of confidential information. – Dal Pont and Chalmers. Coco v AN Clark (Engineers) Ltd [1969] RPC 41, 47 Megarry J: Elements of the equitable duty of confidence are – (apart from a contract) 1. Information must ‘have a necessary quality of confidence about it’ LAWS5126 Medical Law | Exam Notes 52 2. Information must have been imparted in circumstance importing an obligation of confidence 3. There must be unauthorised use of that information. First Element – uncontroversial that medical information has necessary qualities of confidence. Second Element: Imparting information that is confidential o Mense v Milenkovic [1973] VR 784, McInerney J held that the test is objective: ‘any reasonable man standing in the shoes of the recipient of the information would have realised that this information was being given in confidence’. Hunter v Mann [1974] QB 767, Boreham J o Doctor is under a duty not to voluntarily disclose without consent, information gained in his professional capacity. o Here there was a statutory duty under the Road Traffic Act. Two qualifications: 1. Where the doctor is compelled by law to disclose the information; 2. Where patient gives consent to the publication of the information. Two amplifications of this general rule: 1. Gurry F, Breach of Confidence (1984, Ox) suggests this duty extends to information acquired not only directly, but also to information acquired from other persons in the practitioner’s capacity as health care provider. 2. Enforcement of the duty may lead to not only damages for the breach of confidence per se, but also liability for any consequential losses which might flow. Furness v Fitchett [1958] NZLR 396 Facts: Dr gave patient a certificate about certain matters involving his wife. Certificate in opened envelope which was not marked confidential. No restrictions put on use of the certificate by Dr at the time. Man disclosed certificate during family law proceedings. Issue: Was the Dr liable for mental illness incurred by the wife due to disclosure of the certificate. Held: Yes, Court found the Dr should have treated the information carefully due to its sensitivity and put limits on the ability of its use. Significance: Case indicates that a Dr’s duty of care extends to preventing harm to people within foreseeable limits. This includes by way of release of confidential information. Legislation in every State and Territory places limits on ability of Drs to disclose information. In Snell v Pryce, Angel J considered that the NT’s provision (s222 NTCC) doesn’t extend to information already in the public domain – e.g. names, addresses and telephone numbers. Exceptions to Confidentiality 1. Where the doctor is compelled: a. by court order b. by statute – e.g. Public Health Act (notifiable communicable diseases) – Hunter v Mann. Hunter v Mann [1974] QB 767 LAWS5126 Medical Law | Exam Notes 53 Facts: Section 186 Road Traffic Act stated that where a driver is alleged to be guilty of an offence, driver has to provide information as to identity or ‘any other person’ shall if required give information within his power to assist driver ID. Dr was asked for information and refused to give it to police. Issue: Did ‘within power’ mean the Dr had to breach confidentiality and reveal patient? Held: Yes it did, and Dr was convicted under the Act and conviction upheld on appeal. Note – no issue of ‘privileged communication’ for medical documents which prohibit disclosure during litigation. 2. Patient’s express or implied consent: This situation is simple when viewed from the positive angle: a positive consent to release of information elides any obligation to secrecy owed by the person receiving that consent. Equally, an explicit request that information should not be disclosed is binding on the doctor save in the most exceptional circumstances. From the negative aspect, this is trickier though. What is there is another person in the room? Would the patient have consented were they informed about that presences? The example used in the textbook is having trainee doctors in a teaching hospital – in practice, a modern hospital could not function … the return for a technical loss of patient autonomy (i.e. difficult for patient’s refuse to let young doctors stand in) is having access to the best therapeutic and diagnostic aid available. 3. Public interest reasons for disclosing: W v Edgell a. Most controversial permissible exception to confidentiality. i. Rests of subjective definitions – Dr doesn’t need to assist police in enquiries by answering questions, merely cannot give misleading info – Rice v Connolly. W v Edgell [1990] 1 Ch 359 Facts: Plaintiff was detained in a secure hospital following killing of five people. The plaintiff attempted to have himself transferred to a regional secure unit and thereby release into community. Commissioned defendant to compile report on mental state. Defendant psychiatrist’s report was unfavourable, so W withdrew application and refused consent of report’s release. Defendant then released the report and W sought injunction. Issue: Could the defendant psychiatrist lawfully release the report on public interest grounds? Held: The law recognises (1) an important public interest in maintaining professional duties of confidence but (2) that the law treats such duties not as absolute but as liable to be overridden where there is held to be a stronger public interest in disclosure. The report in this case could be disclosed. Debate is therefore about two competing public interests. Reasoning: Principle 1: Edgell redefined conflict between duty of confidence and duty to public as a conflict between two public duties (rather than private and public) – Court stated there was a public interest in maintaining confidentiality (otherwise people would be unwilling to see doctors). Principle 2: It is permissible to breach duty of confidence in circumstances where there is a (1) LAWS5126 Medical Law | Exam Notes 54 serious identifiable risk to public provided disclosure is made to the (2) appropriate authority and done in (3) no greater way than is necessary. Duncan v Medical Practitioners Society (Unrep) Facts: Dr consulted a man who was a bus driver experiencing serious medical condition which made him unfit to drive buses. Dr counselled him to give up job or advise someone of his condition. Patient failed to do so and Dr ran off to the media. Held: Dr was subsequently disciplined by medical board. Board noted that the disclosure was justified but that it had to be a limited disclosure to someone who could deal appropriately with the issue, and not a broad, public one to newspapers. Is there a duty of disclosure? Although following Edgell, a doctor has permission to divulge confidential information, is he under any kind of legal duty to do so? This question has received judicial attention in the United States. Potential existence in Australia? Tarasoff v Regents of University of California Facts: Psychologist employed by University of California had patient who made direct and vivid threats about victim – Tatiana Tarasoff. Dr reported matter to campus police who had him detained but was subsequently released. Upon release, killed Tarasoff and relative sued the University. Issue: As there was public interest in information of murderer’s intentions, relatives claimed failure to advised Tatiana and family amounted to a breach of duty of care. Held: Tobringer J held (1) the general rule that people are under no obligation to control others’ conduct, but that (2) an exception exists where there is a special relationship. Here, the protection of confidentiality “ends where the public protection begins” and the doctor will be under an affirmative duty towards a third party. (The special relationship can include the person’s whose conduct is in question or the foreseeable victim). ‘If the exercise of reasonable care to protect the threatened victim requires the therapist to warn … we see no sufficient societal interest that would protect and justify concealment.’ Tarasoff was immediately subjected to criticism – there is a degree of latitude for professional judgement when a therapist determines, or pursuant to standards of the profession should determine, that his patient represents a serious danger. At what time, therefore, does the danger of violence from a patient towards a third party become apparent? Brady v Hopper o District Court in Colorado limited duty to warn only when there was a specific, identifiable victim. LAWS5126 Medical Law | Exam Notes 55 c.f. Lipari v Sears, Roebuck & Co o Federal District Court gave expansive interpretation – holding that a psychotherapist has a duty to warn when he or she could ‘reasonable foresee that the risk engendered by the patient would endanger others’. identity of the victim therefore irrelevant. Thompson v County of Alameda o Supreme Court of California favoured limited interpretation on a ‘readily identifiable victim’. c.f. Hedlund v Superior Court of Orange County o Same court then held that ‘readily identifiable victim’ included family members and possible that could include all bystanders who might be injured. Academic work has focused on concept of whether there would be proximity between injured party and therapist but the concept of proximity is now rejected in Aus. In absence of unifying concept of when duty of care will arise, better view appears to be that we should resort to the general common law – Under Home Office v Dorset Yacht Company, there is no duty to assist a third party. Confirmed in Australia in Sutherland Shire Council v Heyman. Third party is someone with whom therapist has no previous relationship – what if there had been a relationship in the past – for example, if the threat was made to injure another patient of the therapist or a family member of the therapist? A: law is unclear. Abadee notes that in England and Australia, at most, a doctor will have a discretion to breach confidentiality but would not be mandatory and have to be justified as in the public’s interest. Part 2 - Access to Records Who owns medical records? Can a patient force a Dr to divulge them? Breen v Williams (1996) 186 CLR 71 Facts: Plaintiff had breast implants which were defective. Wanted to join a class action in the United States. Needed defendant’s medical records. Defendant refused to release the records unless P agreed to give him indemnity from any law suit. Breen argued that she was entitled to the records and brought an action. Issue: Were the records the property of the patient or the doctor? Even if the doctor owned them, could he still refuse to release them? Breen ran five arguments: (1) common law gave her a proprietary right and interest in the actual information contained within the records; (2) common law implied a term in the contract to the effect that she had a right of access to the records; (3) there was an innominate common law right of access to medical records; (4) the common law recognised a patient’s ‘right to know’ all necessary information concerning treatment and gave rights for access because of that; (5) law imposed on Dr Williams a fiduciary duty, enforceable in a court of equity , to give her access. Held: LAWS5126 Medical Law | Exam Notes 56 (1) Court noted that she didn’t say she owned the pieces of paper. Documents prepared by an agent usually the property of the principal? Court held this wasn’t agent/principal relationship – notes prepared by him as a professional to assist his duties. Right of ownership good against world except for statute/contract. Premise of this argument was that no one owned the records, Court said it was Dr who owned them. (2) Breen argued by implication of law, contract between Dr and patient requires Dr to ‘act in best interests’ = this includes giving up records on request. Court held Dr/patient requires only reasonable care and skill, not to always act in best interests. Further, Court held that ‘best interests’ term lacks certainty to be implied within contract, therefore fails the Moorcock test as not so obvious that the parties would have agreed on outcome had they turned their minds to it. (3) Court rejected UK decision on innominate right of access as not part of Australian law. (4) Fiduciary argument. Court held that Dr/patient relationship not a broad based fiduciary relationship like trustee and beneficiary. Some aspects of the relationship are fiduciary in nature, e.g. undue influence. Court said no pre-existing duty on Dr to give patient records, Dr is not representative of the patient or acts for him/her (Mason J in Hospital Products). If Dr Williams owed a fiduciary duty, the duties and obligations could only come from aspects of the relationship that included trust, confidence and vulnerability – only in matters of diagnosis, advice and treatment. This meant, even if the Dr was a fiduciary, there was no conflict of interest, no unauthorised profit and no loss resulting from the breach. (5) The ‘right to know’. Breen’s counsel suggested law in Australia moving towards ‘right to know’. Reflected in Rogers v Whitaker: (1) acceptance of personal inviolability of patient; (2) rejection of paternalistic approach; (3) rejection of a notion that patient’s interests fixed by medical profession; (4) imposition of judicially imposed standards; (5) acceptance of patient autonomy. HCA held that it would require a quantum leap to hold that the above gave relief claimed by Breen. Court held that it cannot invent a legal doctrine and that change would have to come from the legislature. Aftermath of Breen 1. All States and Territories have enacted FOI legislation (RTI) a. allows a person to apply to State Gov agency for info (e.g. public hospitals). 2. Federal level – important changes to Privacy Act a. EU trade restrictions required alignment of our domestic law b. unfettered patient access now to medical records…. CTH passed amendments to the Privacy Act 1988 (Cth) (Privacy Amendment (Private Sector) Act 2000). Under amendment, subject to certain exceptions, patients are now able to access their own medical information and there is an obligation on people holding that information to alter it if it is inaccurate c. Privacy Act requires individuals/organisations comply with the National Privacy principles, set out in schedule III of the Act – Principle 6 requires access be granted to people about whom the information is written (subject to some exceptions) LAWS5126 Medical Law | Exam Notes 57 Constitutional Limitations on Health Care No ‘health’ power in s 51 of the Constitution. On what basis can the Federal Government fund programs? Relevant heads of power Section 51: o (9) – quarantine o (14) – insurance o (23) – invalid and old-age pensions o (23A) o Referral power First PBS attempt Despite the absence of a clear head of authority as at 1901, in 1943, Cth attempted to introduce a scheme of pharmaceutical benefits. Act provided for the gratuitous provision of certain medicines prescribed in a formulary and imposed duties on medical practitioners and chemists in relation to prescriptions and supply of medicines. Cth relied on s81 – appropriations ‘for the purposes of the Commonwealth’. Was subsequently challenged in the Pharmaceutical Benefits Case. Pharmaceutical Benefits Case (1945) Held: No broad grant of power for laws to be made ‘for the welfare of’ the people – c.f. United States Constitution. Starke J held Cth can only make laws under a head of s51 and then such purposes as necessary for existence of Cth and running Federal Gov (e.g. paying public servants). Dixon J agreed. Williams J had strident criticism: ‘The Act contains provisions affecting relationships under the laws of the States between practitioners and patients and customers and chemists and many other matters which can only be described as legislation upon the subject matter of public health. There is no express power in the Constitution for the Parliament to legislate upon this subject matter except to make laws LAWS5126 Medical Law | Exam Notes 58 with respect to quarantine and as incidental to the execution of any powers vested in the Cth by the Constitution’. Second PBS attempt: The Commonwealth responded by way of a Constitutional Referendum in 1946. New s 51(xxiiiA) gave the Commonwealth Parliament power to legislate with respect to: - ‘provision of maternity allowances, widow’s pensions, child endowment, unemployment, pharmaceutical, sickness and hospital benefits, medical and dental services (but not so as to authorise any form of civil conscription), benefits to students and family allowances’. New Pharmaceutical Benefits Act 1947-9. Included prostheses in the addendum and destructively, included in s 7A a requirement that a medical practitioner use medicines or appliances in the formulary using a form prescribed by the Cth. A penalty was charged for non-compliance. British Medical Association in Australia challenged Act on the basis that it amounted to civil conscription. BMAA v Cth (1949) 79 CLR 201 Held: Act was invalid. Williams J held civil conscription as forcing people to work for Government’s interests (e.g. forcing people to work in mills). Cth argued that they weren’t compelled to use the forms at all, only if they wanted something for free, within Drs discretion to proceed under the Act’s scheme. Williams J rejected this >> true effect of the section was to make provision of pharmaceutical benefit conditional of Dr prescribing particular treatment. In doing so – Dr is providing service to Cth and certifying to Cth that the patient requires a pharmaceutical benefit. He or she is compelled to render that service in the course of performing contract between Dr and patient. But it is not an implied term of that contract – it is a compulsory service to the Cth for the purpose of an Act which is superimposed on the parties. Was therefore compulsory service whether the obligation was absolute or not. His H said that to decide otherwise would be compelled in the course of their practice to perform all sorts of medical duties (e.g. giving certificates, keeping records and giving info about health of patients). Third attempt: New legislation – Health Insurance Act 1973. Set up a scheme of Medicare, amended in 1977 and placed conditions on entitlement of Dr to claim benefits in respect of pathology services performed. General Practitioners Society of Australia objected to this as civil conscription. General Practitioners Society v Cth (1980) Held: Gibbs J disagreed with earlier constructions of ‘civil conscription’. Plain and natural meaning meant any sort of compulsion to engage in practices as a doctor or dentist or to perform medical or dental services. HH said it does not refer to compulsion in a particular way, some act in the course of carrying out in a profession when there is no compulsion in the first place to provide that service or to carry out that practice. HH pointed out would be an abuse of language to say that a soldier who voluntarily enlisted becomes a conscript because he is now obliged to follow orders. HH held scheme was admissible. More recent constitutional challenges set up to in light of Cths attempts to control administration of nursing homes – Alexandra Private Geriatric Hospital v Cth (1987) LAWS5126 Medical Law | Exam Notes 59 Seems relatively clear what Cth can and cannot do. But what if the Federal Government introduces a scheme requiring newly admitted doctors, before being assigned a Medicare number to: 1. Undertake two years military service as a doctor; 2. Undertake two years service in remote or rural Australia; 3. Provide 24 hour coverage for patients registered in their surgery – ‘on call’ at all times? How does the Cth legislate in respect of health? s96 – allows Cth to make grants to the states on such terms as the Cth sees fit. Cth funds a lot of health service on conditions that vary on the basis of agreements entered into with the states. o e.g. complaints schemes o Medicare scheme and a lot of treatment provided in hospitals Cth also legislates over private health insurance. o scheme of health insurance is very different to most other countries System mandated by the Health Insurance Act is a system of ‘community rating’ – what that means is that the premium is the same (if young, healthy/old, sick). Those premiums are adjusted by agreement between the Gov and various health insurance organisations. The one exception is lifetime health cover. If you haven’t signed up for insurance by a prescribed date, yours will be higher than everyone else and will stay that way for the rest of your life. Also, it is not possible for you to get higher premiums on the basis of increased sickness. NO health insurer can refuse you service once you have the insurance. Insurance market operates very differently! As a consequence: drift in the way health insurance has worked If the premium charged to everyone in the scheme remains the same, then the premiums are going to be set higher to spread the load. That means young, fit and healthy people are dropping out – means more sick people there and premiums rise again (downward spiral) – Fed Gov then introduces lifetime premiums. What do the States legislate? Anything to do with health can be legislated on at any time. Registration of practitioners (but agreement with Cth establishes a national authority). If the State wants to build/fund a hospital or do an inquiry, set up a complaints mechanism – entirely up to their competence (subject to agreements with the Federal Government). LAWS5126 Medical Law | Exam Notes 60 Conjoined Twins Concepts What is a conjoined twin? – Two eggs fertilised that have split, vis-à-vis two fertilised eggs implanted at same time. Conjoined twin: two children born at same time, but fused together. Share common organs = enormous strain on future life. Usually can separate and keep one alive but difficult for both to survive. Is it lawful to separate conjoined twins to preserve one life at the cost of the other? Dudley v Stephens Held: Could they rely on necessity in the common variety (swerve to avoid child and destroy fence)? Court made it clear that there were limits to the doctrine of necessity. Subject to the law of selfdefence, it is not permissible to take one life to preserve your own. If Dudley is still good law, how can it be permissible to effect separation of twins? In Re A [2001] 2 WLR 480 Facts: Twins named Gracie and Rosie Attard. Referred in media as Jodie and Mary. Fused at pelvis and shared lower abdomens. Shared bladder and aorta and inferior vera carva. Mary would not survive separation and surgery. Evidence led that if Mary had not been connected – would not have survived after birth, heart was abnormal and relied on Jodie’s heart to pump blood properly. Mary also had no functioning lung tissue. Neurological problems but were unclear – Mary had never breathed unaided. LAWS5126 Medical Law | Exam Notes 61 Issue: Given the parents were devout Catholics, could Drs obtain a declaration that it was lawful to separate without consent? Held: Trial Judge gave the declaration exercising parens patriae. TJ equated the operation with withdrawal of life support. Parents appealed, which was rejected. (1) HL had to consider first whether there was ever a reasonable creature in being? Are there two persons capable of being killed? Ward LJ – it would be contrary to common-sense and to everyone’s sensibilities to say that Mary is not alive or that there are not two separate persons … The fact that Mary is dependent upon Jodie, or the fact that twins may be interdependent if they share heart and lungs, should not lead the law to fly in the face of the clinical judgment that each child is alive and separate for purposes of criminal and civil law. (rejection of Coke’s ‘monstrous birth’). Brooke LJ – accepted submission that criminal law’s protection of life should be as wide as possible. Robert Walker LJ – expressions such as “monster” were redolent and no place in legal discourse. All three Lord Justices held that Mary and Jodie were alive and separate persons. Walker LJ and Ward LJ held that separation from mother satisfied this. How then to get around Dudley v Stephens? All three Lord Justices held that it was lawful to effect separation. What were the justifications in their Lordships reasoning? 1. Doctrine of double-effect Provision of pain relief to a terminally ill patient to alleviate pain may also result in death. Law excuses practitioner from such consequences. Ward and Brooke LJJ held that there was no place for double-effect in the separation of conjoined twins. Robert Walker LJ held that it could justify the separation. 2. Quasi-self defence Ward LJ considered doctrine of necessity insufficient to justify separation. Relied upon a theory of quasi-self defence. His Lordship recognised the dilemma posed to be able to preserve both lives. Looked at several factors and decided appropriate method was to choose the lesser of the two evils and so find the least detrimental alternative. 3. Quasi-necessity/necessity Brooke LJ used ‘quasi-necessity’ and distinguished Dudley v Stephens to hold that the rule is inapplicable to a case of conjoined twins. Robert Walker LJ prepared to accept necessity should be extended to conjoined twins. LAWS5126 Medical Law | Exam Notes 62 How is the House of Lords’ judgment to be applied in Queensland? What role does the Criminal Code play? State of Queensland v Nolan & Anor [2001] QSC 174 Facts: Alyssa and Bethany born conjoined at the head. Surgery to separate extremely complicated and survival rate for either is low. Alyssa has one kidney and Bethany no kidneys or bladder. Bethany has underlying brain damage and share cranial draining veins and thus one blood flow (Alyssa’s kidney keeps Bethany alive). Bethany suffered a pulmonary and should have died but for Alyssa’s connection. Medical evidence led showed had Bethany died, Alyssa would also die within minutes. Surgery gave Alyssa 60-80% chance. Parents gave permission to separate and State of Queensland applied for order of separation. Issue: Would the surgery which leading to Bethany’s certain death be unlawful? Held: (Chesterman J) 1. Two lives in being. Applying In Re A and s292 QCC. 2. Surgery unlawful? a. HH decided surgery was lawful as it was an attempt to save Alyssa’s life. b. Strict application of the QCC might lead to the Drs being liable for Bethany’s death. c. s 291 QCC provides that it is unlawful to kill anyone without excuse, authorisation or justification by law. d. Necessity of very limited application therefore under the Code. e. Chesterman J then referred to the judgment of Ward LJ in In Re A, concerning the problem faced by doctors in conflicting duties. i. this duty is imposed on the Drs in the case by s 286 QCC requiring provision of necessaries of life for the child. f. Obligation of s 286 would extend towards a duty to save Alyssa’s life. Chesterman J noted that the obligation would discharge in performance, the death of Bethany. i. HH: the operation which is compelled by law is authorisation for the act which has that result. The killing is therefore not unlawful. ii. his Honour relied on s282 to establish the abnegation of criminal responsibility for a surgeon who performs an operation in good faith and reasonable skill. Significance: Suggested by Colleen Davis that His Honour ignored that Bethany was also owed an equally important duty, which was ultimately breached. It is also difficult to see how Chesterman J gets around s 296 of the Code: ‘person who does any act, or makes any omission, which hastens the death of another, who when the act is done or the omission is made, is labouring under some disorder or disease arising from another cause, is deemed to have killed that other person’. Other Issues – what if the twins are adults? 2 scenarios: 1. When ailing twin refuses to consent to the procedure? a. what is the legal position? i. only individual has right to consent 2. Where ailing twin agrees to sacrifice? LAWS5126 Medical Law | Exam Notes 63 a. is that lawful? i. no – cannot consent to own death: s 284 QCC. Difficulty – why should we do something to non-competent people under the protection of the state when that would be impermissible for competent people. Remember ‘factors to be considered’ – In Re A – Brooke and Ward thought about asking guidance from Parliament as to what is legally permissible and what is not. Conference Paper by De Jersey CJ – Legal Ethics ‘Public Interest and Public Policy, Unruly Horses’. CJ points out that when the legislature allows law remain silent, judges may extend principle to cover the gap. In an age of racing medical and scientific development, Parliament is challenged to keep up to date and to date Parliament has not chosen to give that guidance. Third thing – In Re A. Remember that one child born without functioning lungs and without the other twins, would not be able to breathe unaided. Since the classic definition refers to being able to ‘breathe unaided’ from mother, does this mean the Courts in In Re A have impliedly change the meaning of what it means to proceed in a living state from one’s mother? Difficult decisions and courts made correct decisions. But question is whether the law and the coherency of the law can be stretched to so accommodate? Property Rights in Human Body Parts Are there property rights in human body parts? Controversial area. Some people have cell lines that can be used for cancer therapy – example where someone whose cell lines are used to produce lifesaving technology worth millions of dollars could recover part of revenue? Basic principle: common law has historically refuse to recognise the existence of property rights in the human body. Prior to the Judicature Acts – different courts exercised different jurisdictions. Ecclesiastical Court’s position was that once someone died – soul was said to proceed to next world. CL and Equitable Courts had no jurisdiction over the body after death. Doodeward v Spence (1908) 6 CLR 406 Facts: Concerned ownership of a stillborn child. Plaintiff was a showman who exhibited the child, the infant having two heads. Upon prosecution for indecent exhibition of a corpse, the defendant police officer took the child and upon the plaintiff claiming return of the exhibit, the police gave back the bottle and preserving fluid. Held: HCA held 2-1 that the plaintiff was entitled to the return of the exhibit. Sued in detinue (conversion and trespass only permit damages). Reasoning: Higgins J followed old rule in Haynes’s Case and Exelby v Handyside that there were no property rights in the human body. Barton J agreed no rights in a human body, but that is only applied to an unburied corpse. HH distinguished the child from that situation as the child had never been born alive and therefore not a normal child awaiting burial. Griffith CJ held that when a person has by the lawful exercise of work or skill so dealt with a human body or part of a human body in his lawful LAWS5126 Medical Law | Exam Notes 64 possession that it has acquired some attributes differentiating it to a mere corpse awaiting burial, he acquires a right to retain possession of it, at least as against any person not entitled to have it delivered to him for the purpose of burial. Moore v Regents of University of California Facts: Plaintiff being treated at UCal for cancer and as part of treatment, cells were typically taken from him. On one occasion, plaintiff was asked to sign a consent form and became suspicious. Discovered treating Dr had developed a new cell line from his spleen which had been patented by his Dr. The cell line was unique and profits could run into the billions. Issue: Plaintiff sued University regents (as Drs employers), alleging the had interfered with his property rights. Argued breach of fiduciary obligations (remember in Breen – unlikely to fly in Australia). Held: Both California Court of Appeal and Supreme Court recognised patients have some rights over their body tissues. Majority of CA found that property rights were therefore founded in human body parts. Doctor’s usage therefore amounted to conversion. On appeal, majority of the Supreme Court rejected the analysis and found no precedent for arguing there were property rights in the body. Instead found that a patient’s rights were best protected via fiduciary obligations. Result was that the surgically removed tissues could not be used without patient’s consent. NOTE: 1. By legislation in all States and Territories, illegal to sell body parts, but can be compensated for reasonable expenses (e.g. sperm donation). 2. Can we apply Griffith CJ’s reasoning to facts of Moore? a. HH as of the view that using skill to turn the body part into something other than that awaiting burial is permissible. b. Does that mean that Moore had turned the cells into something else? c. ‘Right to bury’ – does that mean that Moore has a property right that is good against everyone in the world but himself 3. Tomato soup paradox a. empty a can of soup that is yours into the ocean … is the ocean now materially different and therefore capable of having ownership rights expressed over it? b. Question of degree – where do we draw the line? Completely different or slight modification of the original? Note also the decision in Rank Hovis McDougall’s Application (1974) that property rights could exist in living things. There a patent was successfully obtained for the process of isolating a micro-organism. Section 18(2) of the Patent Act 1990 (Cth) that human beings cannot be patented. US Supreme Court in Diamond v Chakrabarty (1980) accepted that an invention may be subject of patent protection even though it consists of living matter. Applying Doodeward… Dobson v Tyneside Health Authority [1996] 4 All ER 474 Facts: Deceased died in hospital of a brain tumour. Brain was removed and stored in paraffin wax. LAWS5126 Medical Law | Exam Notes 65 Two years later, next of kin commenced an action against the hospital in negligence for causing the deceased’s death by failing to identify the tumours properly at an early stage. Key to determining this was examination of the brain which had been disposed of the hospital at an earlier stage. Issue: Could the next of kin obtain damages against the hospital for the loss of the brain? Held: Plaintiff’s claim was struck out by the Court of Appeal. No action in conversion because the deceased had died with no executors or administrators appointed. No one in actual possession of the body or with an immediate right to possession. A subsequent grant of administration did not occur until after burial. In any event, executor’s rights to custody of the corpse limited to interring the body. Court did accept from Doodeward that with skill can have a body part capable of being property. But Court rejected that preservation in paraffin wax was enough to convert an item into property capable of possession. Pecar v National Australia Trustees (Unrep, 27 November 1996 NSWSC) Facts: Plaintiff commenced action requesting access to tissue for purposes of a paternity test to prove relation to the deceased, as deceased was intestate, plaintiff possible entitled to share of estate. Pathology company agreed to release if Supreme Court of NSW ordered. Issue: Supreme Court rules can make an order against a party not in litigation for purposes of obtaining samples in relation to any property. Were the samples property under the Rules of Court? Held: Bryson J accepted principle in Doodeward and contrasting Dobson, held that the samples storage in paraffin wax meant the item was sufficient to be said to be susceptible to ownership. Roche v Douglas as Administrator of the Estate of Rowan (Unrep 7 June 2000, WA) Facts: Same as Pecar. Held: Tissue samples were property on the basis of the Supreme Court rules and could be the subject of orders. Didn’t follow Doodeward, stated that the finding was not because the tissue was preserved in wax but on the basis of ‘reason and good sense’. LAWS5126 Medical Law | Exam Notes 66 Bio-Ethics Four Principles of Bio Ethics Jurisprudence of medical practice. It is the underlying ethical principles which are there to guide medical practitioners. From a legal point of view, it is important when we run out of legal answers and have to argue from first principles. 1. Autonomy (or respect for autonomy) Two classical notions of what amounts to autonomy expressed by Emmanuel Kant and John Stuart Mill Kant and Mill’s writings are important because they not only explain what autonomy is but why people should respect each other’s autonomy 2. Kant was obsessed with the concept of ‘the will’ a. ‘To will’ something was to decide on a particular course of action; b. Such a decision would only be ‘morally good’ where the underlying reason for action was not only to act in accordance with duty but for the sake of duty c. States that rational nature exists as an end in itself – since man possesses a rational nature, he is thus an end in himself i. It follows that there is a fundamental law that a person should act in a way that he treats each man as an end in himself and not as a means to an end – this principle is binding on every rational will LAWS5126 Medical Law | Exam Notes 67 1. Respect for treating a person as an end in himself is described by Kant as “autonomy” 2. Kant contrasted autonomy with heteronomy (‘the rule of self by others’ which Kant said was a bad thing) ii. Bottom line from Kant: (1) respect individuals as ends in themselves; and (2) respect people as being able to rationally govern themselves 3. Mill did not refer to the idea of autonomy directly a. Instead, his concern was with ‘liberty’ – the focus to Mill was on a person’s thoughts or actions – restrictions upon a person’s freedom of action were to be tolerated only where the limitations were to prevent one person’s freedom impinging upon another b. Consistent with Mill’s utilitarianism views, it was felt that allowing every person the freedom to pursue his or her own goals, would maximise the benefits to all c. To Mill, the autonomous person was the person with true character (someone without character was controlled by other influences such as family or the State) – Mill said the concept of autonomy was only valuable or worthwhile to the extent that people respect one another’s autonomy 1. Mill said this respect flows implicitly from the idea that there are separate persons 2. To acknowledge another, is to acknowledge the possibility of other centres of choice and intention Autonomy becomes crucial in the area of healthcare – health, by definition, means freedom from mental or physical illness and good health allows an individual to plan present and future affairs. Achieving full health or making the best of poor health can therefore have other flow on effects in respect of a person’s other plans. Bottom line: Respect for autonomy means people are entitled to make their own decisions about their own selves 2. Beneficence (countervailing principle to autonomy) 1. The countervailing principle to autonomy is often beneficence. – Beneficence requires that medical practitioners act so as to produce the best medical result for their patient –it is said that beneficence is the Raison D’etre of the medical profession – A medical practitioner is trained to treat and to attempt to cure Bromberger: the trend to beneficence has now gone so far that the medical practitioner no longer administers to the sick, but rather treats the sickness 2. a. 2 versions of beneficence – see pg 6 and 7 of textbook – (1) Hippocrates designed a series of principles for medical people designed to set them apart from and above others in society – one of those moral purposes was to produce the best medical outcome – (2) More modern version has come from Scottish physician called Gregory – art of medicine is LAWS5126 Medical Law | Exam Notes 68 the art of preserving health, prolonging life and curing diseases. Drawing on earlier writings of David Hume, Gregory said moral judgements do not rest ultimately on reason, but rather on sympathy – Gregory’s theory rests on a moral view of medicine and using the medium of sympathy generates specific instances of beneficence – b. Beneficence is in a list of goods to be striven for and harms to be avoided – outlined in a book by 2 American philosophers, Beauchamp and McCulloch Interplay between autonomy and beneficence – The 2 can go hand in hand – e.g. if person is sick and goes to see medical practitioner – states that person has chest infection, gives course of anti-biotics and asks to take for 7-14 days; respect for autonomy means there needs to be some respect for the decision as to whether to decline or accept the treatment and beneficence means the best medical outcome has to be achieved – If the patient accepts the treatment, this means both autonomy and beneficence are achieved 3. Non-maleficence The flipside of ippocrates principle of beneficence In a work called ‘Epidemics’, Hippocrates states “as to disease, make a habit of two things: two help, or at least do no harm” – the ‘help’ part is beneficence (trying to achieve best medical outcome) and the ‘do no harm’ is non-maleficence (moral duty not to cause additional harm or suffering to a patient) 4. Justice Different versions of justice – on intuitive level, understood as being far between different groups of people (equality before the law) How do four bio-ethical principles help develop the law? What if patient chooses not to accept treatment (conflict between autonomy and beneficence)?– e.g. terminally ill patient offered chance to prolong life in a way which would increase pain/suffering and chooses not to take that option – recall competency cases where people stated they did not want to have certain procedures performed The concept of competency helps us decide between a conflict between beneficence and autonomy If a patient is competent, his/her autonomy must be respected. If a patient is not competent, beneficence will prevail and there are procedures at common law and under legislation where the patient’s will can be overborne What about implications of justice? Strong example in ‘QALY’ (Quality Adjusted Life Years) principle – a measure a group of Americans came up with to try and find a rational way of rationing healthcare resources o Thought by determining how many years a person has of quality life left, you could ration healthcare between different groups of people LAWS5126 Medical Law | Exam Notes Cross-reference later lecture on separation of conjoined twins – consider which principles are operating and whether they assist the court in reaching a determination OR whether it is a straightforward application of established legal principles 69