File - Elizabet Iankova
advertisement

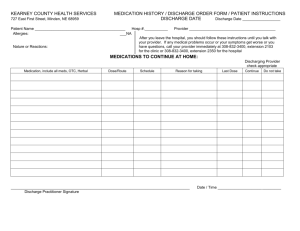
Running head : DISCHARGE PLANNING 1 Discharge Planning Project Elizabet Iankova University of South Florida DISCHARGE PLANNING 2 The patient is a 70 year old male who had came to the hospital for a scheduled coronary artery bypass graft times 2 because of his significant coronary artery disease. The patient complained of exertional chest pain over the last year that had gotten worse over the last couple weeks before his surgery. He had a cardiac catherization with a finding of a very high grade calcified aorta and was recommended to have bypass surgery. The patient has a past medical history of hypertension, hyperlipedemia, diabetes and anemia. His family medical history revealed that both his mother and father had passed away from cardiac problems such as heart failure and myocardial infarction. The patient drinks alcoholic beverages daily, such as beer and could have up to nine a day. In addition, he was a former smoker for the majority of his life and used to eat a lot of restaurant style fried foods. The patient also reported periods of mild depression and fatigue. Currently, the patient is well aware of his hospitalization. He understands the need for surgery and reasons that lead to his coronary artery disease. Diabetes management, medication regimen , low fat diet and daily exercise are all very important teaching topics to be considered with his disease process. Prior to discharge, the SCIP core measure had been met. SCIP core/quality measure refers to surgical site infection education. The patient was given education on safely cleaning the site, applying the dressing and signs and symptoms of an impending infection. Medication education is an important piece in discharge planning. The patient should go home with a new medication list that includes name of medications, next expected dose and possible side and adverse effects associated with each drug. The patient has received information on the following medications : ALPRAZolam ( Xanax 0.25 mg oral tablet ) 3 times a day as needed for anxiety. Xanax can cause dizziness, drowsiness and lethargy. The patient should avoid driving and other activities that require alertness and also avoid drinking grapefruit juice during therapy. aspirin ( aspirin 81 mg oral delayed release tablet ) next dose at 9 am for clot prevention. aspirin can cause GI bleeding, dyspepsia, 2 DISCHARGE PLANNING 3 epigastric distress and nausea. The patient should be instructed to take salicylates with a full glass of water and to remain in the upright position for 15-30 minutes after administration. In addition, alcoholic beverages should be avoided to minimize possible gastric irritation. clopidogrel ( Plavix 75 mg oral tablet ) next dose at 9 am for reduction of atherosclerotic events. Plavix can cause GI bleeding, rash and thrombocytopenic purpura. Bleeding time should also be monitored with therapy. Patient should notify health care professional if fever, chills, sore throat , rash or unusual bleeding occurs. furosemide ( Lasix 40 mg oral tablet ) next dose at 9 am for decreasing blood pressure. Lasix can cause aplastic anemia, Steven-Johnsons syndrome and Agranulocytosis. Patient should monitor daily weights, intake and output ratios and location of any edema. lisinopril ( lisinopril 20 mg oral tablet ) next dose at 9 am for decreasing blood pressure. lisinopril may cause dizziness, hypotension and angioedema. Patient should take medication as directed at the same time each day, take caution when doing activities that require alertness and monitor for signs of allergic reaction. metFORMIN (500 mg oral tablet ) twice daily , next dose at 9 pm for management of diabetes. metFORMIN may cause abdominal bloating, diarrhea and nausea. Patient should take the medication as directed same time each day, monitor for signs of hypoglycemia and instruct patient to properly test blood sugar. metoprolol ( Lopresor 50 mg oral tablet ) twice daily, next dose at 9 pm for management of hypertension. metoprolol may cause fatigue, weakness, bradycardia, heart failure, pulmonary edema and erectile dysfunction. Patient should monitor their blood pressure, and pulse frequently. Also, monitor intake and output rations and adverse lung sounds. omeprazole ( PriLOSEC 20 mg oral delayed release capsule ) daily, next dose at 9 am for reflux. omeprazole may cause abdominal pain and psuedomembranous collitis. Patient should monitor bowel function, fever, bloody stools and abdominal cramping. Potassium chloride ( 10 mEq oral tablet ) 2 tablets, next dose at 9 am for potassium replacement. Potassium chloride can cause arrythmias, abdominal pain , diarrhea, nausea and vomiting. Patient should monitor for signs of hypokalemia such as weakness, fatigue, polyuria and polydipsia. Patient should also be cautious of overdosing which can lead 3 DISCHARGE PLANNING 4 to hyperkalemia. Lastly, simvastatin ( Zocor 20 mg oral tablet) take next dose at 9 pm and all doses at bedtime for high chloesterol. simvastatin may cause abdominal cramps, constipation, diarrhea, flatus and heartburn. Patient should monitor for muscle tenderness, and advise the patient that this medication should be used in conjunction with diet restrictions and cessation of smoking. This information is in his discharge packet and it has a page for each medication explaining in detail side effects and adverse effects. The patient must bring his list of medications to all appointments, follow up visits, and hospital visits. The patient has a relatively safe living situation. He lives with his wife of 38 years and his small dog in a mobile home. The patient needs to be most careful with his dog and not let the dog jump on him, as the dog can cause damage to his wound site or allow infection to develop. His wife will help him with his medications, food, and transportation to his follow up appointments. The patient states that he does not need any financial assistance for his medications or required care. A follow up appointment with Dr. Mellor is scheduled for him within the next two to five weeks. Furthermore, he has follow ups scheduled with Dr. Tabesh, Dr. Koshy and Dr. Balakumar within one to two weeks. He is required to bring his chest x-ray films when he attends his appointment. The patient is to resume activities as tolerated and follow a cardiac diet. The most important considerations to prevent readmission for this patient are life style modifications and infection prevention. Given that the patient suffers from diabetes and cardiac problems, diet and exercise teaching is paramount. The patient needs to follow his low fat, count carb diet in order to maintain a healthy blood sugar, as well as normal ranges for hemoglobin A1C. When talking to the patient , he mentioned he ate fried foods for the majority of his life. He also stated that he understood that his past diet was a contributing risk factor for his coronary artery disease. Along with diet, the patient should not drink alcoholic beverages. He mention he drank up to nine beers a day, so 4 DISCHARGE PLANNING 5 cutting down his alcoholic intake is an important consideration to prevent readmission or worsening disease process. In addition, he needs to be timely with his oral antidiabetic drug and insulin before or after eating. The patient should check his blood sugars regularly during the day, and get coverage if he needs it. The patient should try and exercise as much as he can tolerate and try to do it on a regular basis. Lastly, infection prevention should be addressed to prevent readmission as this issue can occur rapidly. The patient has a surgical site on his chest from his cardiac bypass. The site needs to be cleaned with proper solution and have a clean dressing on it. The patient should be able to recognize signs of infection such as redness, drainage and/ or fever. As mentioned above, surgical site infection prevention is a core measure. If any of these signs occur, the patient should notify his physician immediately. Overall, the patient is ready and eager for discharge. If the patient follows his discharge instructions as directed, he will prevent his chances for readmission. 5