Differential Diagnosis for White Lesions
advertisement

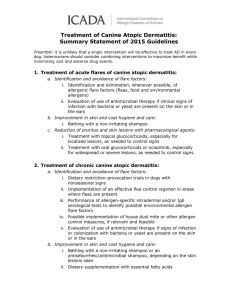
Everyday Encounters with Oral Pathology: Review, Refresh, Discover NCDHAAS Fall Meeting October 24, 2014 Hickory, North Carolina Presented by: Alice E. Curran, DMD, MS University of North Carolina School of Dentistry Division of Oral and Maxillofacial Pathology Chapel Hill, NC 27599 alice_curran@unc.edu Differential Diagnoses, Management Plans And Supplementary Material Differential Diagnosis for White Lesions Differential Diagnosis for Mixed Red-and-White Lesions Differential Diagnosis for Ulcerative Conditions Differential Diagnosis and Treatment for a Tongue Mass Differential Diagnosis and Treatment for a Palatal Mass Differential Diagnosis for Blue/Brown Oral Pigmented Lesions Differential Diagnosis for a Neck Mass Managing Xerostomia Managing Oral Candidiasis Performing an Oral Cytologic Smear Clinical Features of Recurrent Aphthous Ulcers versus Herpes Simplex In Immunocompetent Patients Managing Recurrent Aphthous Ulcers Managing Recurrent Herpes Simplex Infection Prescription Rx Recipes and Formulas Diseases Associated With Desquamative Gingivitis Drugs Associated With Osteonecrosis of the Jaws Syndromes Associated With Hereditary Gingival Overgrowth Oral Squamous Cell Carcinoma: 5-year Survival by Stage at Diagnosis Critical Evaluation of Diagnostic Aids for the Detection of Oral Cancer 2 NCDHAAS Fall Meeting October 24, 2014 Title: Everyday Encounters with Oral Pathology: Review, Refresh, Discover Course Description: Using a series of clinical and radiographic cases, this course will review and expand upon basic oral pathology what we all learned in school, to include updates on familiar concepts as well as discuss newlyevolving issues facing dental and dental hygiene practice today. Objectives: At the end of the course, the participant will be able to: 1) Recognize common oral lesions that are encountered in daily practice, using both clinical photos and radiographs. 2) Discuss variations of common lesions that affect the periodontium that are unrelated to plaque. 3) Discuss lesions associated with various forms of trauma or irritation. 4) Apply current management protocols for common and not-so-common oral lesions. 5) Discuss HPV-related oropharyngeal cancer; become prepared for changes as new information evolves in the coming years. 6) Discuss drug-associated osteonecrosis of the jaws and its management in general practice. About The Presenter Dr. Alice Curran is originally from Milford, Massachusetts. She began her dental career as a dental hygienist. She graduated from Cape Cod Community College with an AS in Dental Hygiene and the University of Rhode Island with a BS in Dental Hygiene. During dental hygiene school, histology and oral pathology were her favorite courses. She completed the Pathology Education Master’s Degree Program at Washington University School of Dental Medicine in St Louis, MO, where she was one of five dental hygienists who studied general and oral pathology for two years. Following graduation with an MS, she taught oral pathology, histology, periodontics and radiology at the University of Kentucky Community College System Mobile Dental Hygiene Program for 10 years, during which time she also practiced dental hygiene part-time. After that, she decided to pursue her DMD degree so that she could attain certification as an oral pathologist. She graduated from the University of Kentucky College of Dentistry and then completed the certificate program in Oral and Maxillofacial Pathology at Emory University School of Medicine in Atlanta, GA. Her first academic position as an oral pathologist was at the University of Mississippi where she taught dental and dental hygiene oral pathology courses for four years. She has been on the faculty at UNC for 12 years. She is a Fellow in the American Academy of Oral and Maxillofacial Pathology and a Diplomate of the American Board of Oral and Maxillofacial Pathology. In addition to teaching dental hygiene and dental graduate students, she treats patients with oral pathologic lesions, reads biopsies, conducts research and gives continuing education courses for dentists and dental hygienists on current topics in oral pathology. Along with her friend and oral pathology colleague, Dr. Sandra Myers of the University of Minnesota, she co-authored the new textbook General and Oral Pathology for Dental Hygiene Practice published by FA Davis. 3 Differential Diagnosis for White Lesions 1. Does the lesion wipe off? Yes : Pseudomembranous candidiasis (perform smear) Thermal or chemical burn including aspirin burn Cotton roll burn Toothpaste allergy No Frictional keratosis Premalignant epithelial dysplasia These lesions cannot be separated by any clinical means; they must be biopsied. Squamous cell carcinoma Hyperplastic candidiasis Verrucous carcinoma Others that may be have clinical differentiating features but must be biopsied for confirmation: -Reticular Lichen Planus-white lace-like pattern -Lichenoid mucositis-white lace-like pattern near dental metal or in patient on certain medications -Oral hairy leukoplakia-vertical folds; patient will be immunocompromised ie, HIV or transplant -White sponge nevus-generalized to most mucosal surface; thick heavy plaques; family members affected -Submucous fibrosis- seen in users of betel quid, a tobacco/areca nut concoction popular in Asia. -Papilloma: finger-like projections -Verruca vulgaris (common wart): raised with rough surface 4 Differential Diagnosis for Mixed Red-and-White Lesions Lesions with Characteristic Clinical Features -Geographic tongue-serpiginous/circinate white lesions with red atrophic centers; can occur in other mucosal locations other than tongue -Thermal burns-per patient history -Nicotine stomatitis-white background with red papules in smokers or hot tea drinkers -Cinnamon allergy-per patient history of use -Scarlet fever (strawberry tongue)-per medical history -Atrophic candidiasis-perform smear to confirm Lesions with No Characteristic Clinical Features Must be biopsied to establish diagnosis -Premalignant epithelial dysplasia -Carcinoma-in-situ -Squamous cell carcinoma -Histoplasmosis and blastomycosis infection (might have central ulcer) -Traumatic granuloma (might have central ulcer) -Erosive lichen planus-erosions with peripheral white striae may be seen 5 Differential Diagnosis for Ulcerative Conditions Ulcers are focal lesions with loss of epithelium covered by a necrotic membrane. They all appear as yellow/gray lesions with a red halo. Acute Short Duration -Traumatic ulcer including Anesthetic necrosis - per history -Recurrent aphthous ulcer: single ulcer on nonkeratinized tissue that does not overly bone with no prodrome -Herpes labialis or stomatitis: cluster of coalesced ruptured vesicles on keratinized bound tissue preceded by prodrome -Allergic reactions -Herpangina-usually on soft palate as a cluster of small ulcers; fever and pain -Herpes Zoster-looks like severe HSV but lasts longer and does not cross the midline -Erythema multiforme-large ulcerated areas and target lesions on the skin Chronic Long Duration -Squamous cell carcinoma- nonpainful ulcer with raised borders -Traumatic granuloma- nonpainful ulcer with raised borders -Erosive lichen planus -Tuberculosis -Histoplasmosis -Wegener’s granulomatosis -Cancers that have metastasized to the oral cavity from other parts of the body -Major aphthous ulcers: multiple large ulcers with prominent borders; very painful; few periods of remission; heal with scars; may be caused by Crohn’s disease or immunosuppression; some cases are idiopathic. 6 Differential Diagnosis and Treatment for a Tongue Mass Irritation fibroma: firm, dome-shaped mucosal-colored and the papilla on top become short; usually has a history of injury or you can see the irritating tooth or partial. Biopsy. Mucocele: we think of these on the lip but they can occur anywhere there are minor salivary glands. They are fluctuant and usually on the anterior ventral tongue. Usually has a history of injury to the area. Biopsy. Granular cell tumor: will look much like a fibroma on the dorsum, with short or absent papillae on the surface but there may not be a history or signs of trauma. You can feel it within the body of the tongue but it feels well-defined. Biopsy. Pyogenic granuloma: usually thought of on the gingiva of women but can occur on any mucosal surface in anyone; usually red and white with ulceration, sometimes a bleeding surface; can be tender; often a history of trauma. Biopsy. Lingual thyroid: mucosal-colored mass behind the circumvallate papillae. Surface will be intact with no ulcerations; mucosa may be thin and you might be able to see blood vessels through the thin mucosa. Refer to ENT for thyroid scan. DO NOT REMOVE. This may be the only functioning thyroid the patient has. Salivary gland tumor: can be benign or malignant, usually benign; can occur anywhere that there are minor salivary glands. Biopsy. Traumatic granuloma: painless lesion with raised red borders with yellow necrotic center; borders may be indurated; may be a history of repeated trauma to the area; most often interpreted as a squamous cell carcinoma. Biopsy. Squamous cell carcinoma: will have a variety of appearance from a flat white plaque to a raised ulcerated red and white painless mass. Biopsy. 7 Differential Diagnosis and Treatment for a Palatal Mass Anterior Palate Nasopalatine duct cyst: soft swelling between #8 and 9; will be seen radiographically. Biopsy. Palatal abscess: fluctuant swelling with fistulous tract; test for tooth vitality; can be associated with any tooth. Treat odontogenic infection. Odontogenic tumor: not common on the anterior palate but if present will be close to the teeth. Biopsy. Note: Salivary gland tumors and mucoceles DO NOT occur in the anterior hard palate. Posterior Hard Palate and Soft Palate Torus palatinus: hard bony bump in midline that appears radiopaque on an occlusal film; surface may be ulcerated if it is traumatized. No treatment. Salivary Gland Tumor: either benign or malignant; soft but firm painless usually slowgrowing mass usually to the right or left of the midline; mucosal colored or red if ulcerated; sometimes they are blue. Biopsy Necrotizing sialometaplasia: a reactive response to an injury usually caused by a dental injection or other injury that led to ischemia of the area; the anesthetic causes a mild ischemia that causes death of the minor salivary glands near the greater palatine foramen as well as the surface mucosa; appears as red ulcerated mass shortly after the injury. No treatment. Lymphoma: a malignancy that can be mucosal-colored and firm or red and white and ulcerated with a boggy texture; usually appear over a short period of time; can be mistaken for necrotizing sialometaplasia. Biopsy. Neurofibroma: firm mucosal-colored mass; can occur on any oral surface but likes the posterior hard palate near the greater palatine foramen. Biopsy. Kaposi’s sarcoma: usually seen in immunocompromised patients (HIV+ or transplants patients) as a well-defined or diffuse blue-purple mass, often in multiple locations. Biopsy. 8 Differential Diagnosis for Blue/Brown Oral Pigmented Lesions All pigmented lesions of the oral cavity must be biopsied! Exceptions: Ethnic Pigmentation and Amalgam Tattoo But how do you know it is an amalgam tattoo? Rule of Thumb for Managing an Amalgam Tattoo If you see what you interpret to be an amalgam tattoo, radiograph it. If you see small radiopaque bits of amalgam in the area of the oral lesion, then it is an amalgam tattoo. If you cannot see any amalgam fragments, then the lesion must be biopsied. Sometimes the amalgam has stained the tissue without leaving fragments. Only a biopsy can determine this. We are most concerned about melanoma in the oral cavity. It is rare. When it occurs, it favors the gingiva and hard palate, but can occur anywhere. The following lesions are benign but may have very close similarities to the appearance of an early melanoma: Melanotic macule Smoker’s melanosis Melanocytic nevus Melanoacanthoma Drug pigmentation (can be differentiated by doing a compete drug history) Café au lait pigmentation of neurofibromatosis or McCune-Albright syndrome (can be differentiated from medical history) 9 Blue Lesions Blue lesions are often confused with pigmented lesions because they are both dark. Blue lesions are most often vascular (come from blood vessels) and are not pigmented, per se, because they do not contain melanin pigment or pigment from foreign materials like amalgam. One way to differentiate a blue vascular lesion from a grey-brown pigmented lesion is to use DIASCOPY: this involves putting pressure on the lesion and observing it for BLANCHING (color fades and comes right back when pressure is released). If the lesion is DIASCOPY +, then it is vascular. If it is DIASCOPY-, it is most likely pigmented but some vascular lesions are Diascopy-. A biopsy can determine the difference. Vascular Blue Lesions: Varicosity (if there is a small clot in the vein, it may be diascopy+) Hemangioma (most hemangiomas are congenital. It is unusual for an adult to develop a true hemangioma.) Hematoma: a bruise caused by local injury, usually blunt trauma. Petechiae are usually red but will appear to contain blood. They are less than 1 mm in diameter and occur in clusters. Kaposi’s Sarcoma: malignant tumor made up of small blood vessels so it looks blue. Non-vascular blue lesions Mucoceles, ranulas and salivary gland duct cysts can occasionally be bluish in color. Never occur on gingiva or anterior hard palate Eruption cyst developing over an impacted tooth Gingival cyst of the adult will be located within the zone of attached gingiva 10 Differential Diagnosis for a Neck Mass Midline Upper Neck: Dermoid cyst Salivary gland obstruction Ranula Salivary gland neoplasm Thyroid area: Thyroglossal duct cyst Thyroid gland enlargement- goiter Thyroid gland neoplasm Lateral Neck Reactive lymph nodes (reacting to infection) Lymphoepithelial cyst (Branchial cleft cyst) Cystic hygroma (cervical lymphangioma in children) Metastasis of oral cancer to lymph nodes Lymphoma (cancer of lymph nodes) Lipoma (benign fat tumor) Salivary gland tumor (upper neck) 11 Managing Xerostomia Many OTC commercial saliva substitutes and commercial oral moisturizing gels are listed. Other hints such as avoiding caffeine and cola, avoiding alcohol containing products, avoiding tobacco, humidifying the area, and coating the lips are included. OTC: SalivaSure salivary stimulant. Available on-line Information: http://www.scandinavianformulas.com/salivasure.html Purchase: www.vitacost.com OTC: OraMoist Dissolvable Discs Information OTC: XyiMelts Mint and regular OTC: Biotene products from Laclede. Toothpaste and mouthwash feel gentle to irritated tissues. Lubricating gel and liquid help keep mouth moist. They do not medically treat xerostomia but provide great comfort for the tender mouth. They will send samples to your office. http://www.laclede.com/ Address: 2103 East University Drive, Rancho Dominguez, CA 90220 Customer Service Toll-Free: 1-800-922-5856 OTC MedOral Dry Mouth Spray. This was initially recommended by patients who were given it while in hospital, but it is available for purchase toll free 1-866-887-4867 or www.BHMLABS.com. RX: Aquoral spray, a plant lipid based product for dry mouth symptoms. RX: Aquoral protective oral spray, 40 ml, 2 sprays 3-4x daily. It has a mild citrus flavor. Information: http://www.aquoral.com/ No Longer Available RX: Caphosol artificial saliva, New product for dry mouth symptoms and to prevent damage to teeth (artificial saliva and remineralizing solution) 4 boxes (12-30 days supply @4-10x daily) Rinse as instructed 4x daily and increase as needed up to 10x daily. Refill one year. Information :http://www.caphosol.com/new/default.asp Prescribing information: http://www.caphosol.com/new/03_default.asp Note: This was developed for cancer patients, but it can be used by anyone with dry mouth and oral pain or mucositis. Mix solutions together in cup, swirl together, swish with mouthful for one minute and spit out. Repeat with remainder of the solution. If swallowed accidentally no adverse effects are anticipated. Do not eat or drink for at 30 minutes after use. No product-related adverse effects or drug interactions have been reported. It may taste salty to some. 12 CONDITION SHARED BY Managing Oral Candidiasis Angular cheilitis (perleche): Vytone cream applied 3-4 times per day or Information: http://products.sanofiaventis.us/Vytone/vytone.html Alcortin A Oral candidiasis: Selection of product depends on compliance issues and drug interactions for the particular patient. If Diflucan is contraindicated because of a possible drug interaction with another drug the patient is taking, then an oral rinse or lozenge is indicated. If the patient cannot follow instructions for swishing or sucking on a lozenge, then systemic medication may be the choice-- if there are no potential drug interactions. Topical Antifungals: -Nystatin oral suspension 100,000 units: Rinse 1 teaspoon for 2 minutes; spit; NPO 30 minutes. Repeat 4-5 times per day for 2 weeks. -Mycelex troches 10 mg: Dissolve one troche 4-5 times per day; NPO 30 minutes. NOTE: If patient wears a denture or RPD, it must be removed while using these medications because they work by direct contact to kill the fungal organisms. The prosthesis will block the drug from touching the tissue. Systemic Antifungals: Fluconazole 100mg tabs. Take 200 mg on Day 1 and 100 mg for each day thereafter for 2 weeks. Check for drug interactions before prescribing. There is no strong research evidence to support soaking a denture or partial in an antifungal soak to kill candida. However, if this step is desired, use chlorhexidine for any prosthesis that contains metal framework. For acrylic- based prostheses, use 1:20 solution of household bleach in a denture cup overnight. Scrub well in the morning. A stronger solution will bleach the acrylic. 13 PERFORMING A CYTOLOGIC SMEAR 1. Do NOT wipe or otherwise disturb the area you wish to sample. This may cause a false negative result. A smear is best taken at the beginning of an appointment. 2. Write the patient’s name in PENCIL NOT PEN on the frosted end of the glass slide. 3. IF THE PATIENT HAS A VERY DRY MOUTH, have them rinse gently with a little water without spitting before the specimen is collected. 4. Using a dental cement spatula OR a damp wooden tongue blade, firmly wipe the area. Use enough strokes to collect a visible accumulation of oral fluids. 5. Transfer the fluids to a clean dry glass slide. Smear the sample across the slide to make a thin coat. Hold the glass slide up to the light. If you can see the sample on the slide, you have enough. Do not overload the slide. Repeat in another area if necessary to obtain an adequate sample. 6. Spray Cytofix on the slide from a distance of about 8 inches. DO NOT spray too closely to prevent rinsing the cells off the slide. Do not overspray; one or two swipes should be enough. If you do not have CytoFIX, you can use any hairspray that contains alcohol. 7. Allow the slide to dry for a few minutes and place in the slide container. 8. Fill out the patient history and submission form. 9. Send to the Oral Pathology Laboratory of your choice. You may obtain cytology kits from: Oral Pathology Laboratory University of North Carolina School of Dentistry 5603 Oral Health Sciences Building CB 7455 Chapel Hill, NC 27599 919 537-3155 14 Clinical Features of Recurrent Aphthous Ulcers versus Herpes Simplex In Immunocompetent Patients Feature Minor RAU Etiology Localized immune defect No Prodrome Herpetiform RAU Major RAU Herpes Localized immune Systemic immune Herpes simplex defect disorder virus No No Yes Intraoral location Preceding vesicle Ulcer appearance Nonkeratinized mucosa No Nonkeratinized mucosa No Nonkeratinized mucosa No Keratinized mucosa Yes Single; less than 5 mm Cluster less than 5 mm Cluster that coalesces into large ulcers Remission period Extraoral sites Yes Yes 1 - single, large deep, irregular rolled border 2 - cluster No No No No Yes Diagnosis Clinical features Clinical features Systemic disease consultations Treatment Topical antiinflammatory drugs Topical antiinflammatory drugs Yes Clinical features; cytologic smear Systemic Topical management of antiviral drugs underlying during disease; prodrome Systemic only; immunomodulary Systemic drugs for antiviral drugs idiopathic for severe etiology recurrent cases 15 Managing Recurrent Aphthous Ulcers Minor recurrent aphthous ulcers are a self-limiting disease. They resolve 7-10 days without treatment and in 7-10 days with treatment. The key to successful treatment is to avoid the trigger in the first place! Many over-the-counter medications are available. Most are either analgesics that reduce the pain or they are anti-inflammatory agents that reduce the healing time by about 1 day. Products are too numerous to list. The all work very much the same. New Product: Avamin Melts Cauterizing agents “burn” the affected tissue; this reduces pain and speed the healing. The theory is that a regular “burn” will heal faster than an aphthous ulcer. These agents CANNOT be given to patients. They must be used in the office by the dentist. Available agents: Debacterol: http://www.debacterol.com/ Silver nitrate sticks: http://www.aafp.org/afp/20010901/letters.html Hold the solution directly on the ulcer UNTIL IT TURNS WHITE. THEN STOP IMMEDIATELY. Use these with CAUTION as overuse may actually cause more tissue damage, more pain and longer healing times. 16 Managing Recurrent Herpes Simplex Infection Recurrent herpes simplex infection is a self-limiting disease. Lesions heal in 10-14 days without treatment and 10-14 days with treatment. The key to successful treatment is to avoid the trigger in the first place! The key to reducing healing time of the ulcers is to treat skin or mucosa during the PRODROME. This is the period of itching or tingling that occurs BEFORE there is actual clinical evidence of a lesion (a small blister also called a vesicle. In herpes, these form in small clusters, then coalesce to form one or two larger blisters.). This period may last hours or minutes, so the window of opportunity to treat them is VERY SMALL. NOTHING WORKS AFTER THE LESION APPEARS! Any treatment after that is palliative only. Any of the several OTC products available only work in the prodrome. Several prescription topical agents also are available but do not speed healing by more than 1-2 days and are most effective during the prodrome. One is Denavir: http://www.denavir.com/ If the patient has frequent serious outbreaks of recurrent herpes labial or herpes stomatitis, then consider prophylactic antiviral therapy with Valtrex. The recommended dose for VALTREX is 2 grams taken at the first sign of a cold sore prodrome, and then again about 12 hours later. (One day therapy ONLY) It’s important to start treatment with VALTREX at the first sign of a cold sore (such as tingling, itching, or burning). There are no studies that show if VALTREX works when used after the appearance of a cold sore. http://www.valtrex.com/coldsores/whatis_coldsore.html 17 Magic Mouthwash Prescription Rx Recipes and Formulas There is no standard formula for Magic Mouthwash. You will find many! When the pharmacy gets a prescription for Magic Mouthwash, the pharmacist compounds according to the prescribing physician's instructions or recipe. Many health care providers assume there is ONE formulation and don't know the exact ingredients or proportions. When a prescription for Magic Mouthwash is given to a patient, it must contain specific ingredients and amounts, so the pharmacist knows which one to make. Here are some of the more common adult formulations Keep in mind that most of these are low potency. Adding Nystatin to an elixir for a patient with no evidence of candidiasis may help promote resistance. Patients generally DO NOT LIKE viscous lidocaine. Avoid it!! Swallowing is not recommended. Most ingredients are inactivated in the stomach so there is no systemic benefit. Besides, they may cause gastric irritation. These formulations are not potent enough for vesiculoerosive disorders such as erosive lichen planus and pemphigoid. Magic Mouthwash Recipe 1 Use: Minor erosive or ulcerated lesions in patient with or with history of candidiasis Rx: 80 ml viscous lidocaine 2% (only with severe pain) 80 ml Mylanta 80 ml diphenhydramine 12.5 mg per 5 ml elixir 100 ml nystatin 100,000U suspension 120 ml prednisolone 15mg per 5ml solution 80 ml distilled water Sig: Swish, gargle, and spit one teaspoonful every 3-4 hours as needed. 18 Magic Mouthwash Recipe 2 Use: Symptomatic geographic tongue Rx: 1 Part viscous lidocaine 2% (only with severe pain, otherwise leave it out) 1 Part Maalox (do not substitute Kaopectate) 1 Part diphenhydramine (12.5 mg per 5 ml elixir) Quantity: 120 ml Sig: Swish, gargle, and spit one teaspoon every 3-4 hours as needed. Magic Mouthwash Recipe 3 Use: Minor erosive or ulcerated lesions in patient without candidiasis Rx: 30 ml viscous lidocaine 2% (only with severe pain) 60 ml Maalox (do not substitute Kaopectate) 30 ml diphenhydramine 12.5 mg per 5 ml elixir 40 ml Carafate 1 gm per 10 ml Sig: Swish, gargle, and spit one teaspoon every 3-4 hours as needed. Magic Mouthwash Recipe 4 Use in conjunction with topical corticosteroid application for mild erosive lichen planus in patient with history of candidiasis Rx: 120 ml dexamethasone (0.5 mg per 5 ml elixir) 60 ml nystatin 100,000U suspension 100 ml diphenhydramine (12.5 mg per 5 ml elixir) 1000 mg tetracycline (contents of 2 capsules tetracycline 500 mg) Sig: Swish, gargle, and spit one teaspoonful every 3-4 hours as needed. 19 Patients with erosive lichen planus or other autoimmune vesiculoerosive disorder should be referred to an oral pathologist for management. Once the disease is under control, they can be maintained in the general dental office. 20 Diseases Associated With Desquamative Gingivitis DISEASE CLASSIC INTRAORAL FEATURES EXTRAORAL SIGNS Erosive lichen planus Wickham’s striae at border of ulcer or erosion Mucous membrane pemphigoid Vesicles that rupture; Purple polygonal pruritic plaques on skin of extremities Symblepharon; Positive Nikolsky’s sign Tense bullae on skin Pemphigus vulgaris Additional intraoral sites, rarely gingiva alone; Flaccid bullae on skin Desmosomes Erosive skin lesions Basement membrane zone Rare Nuclei of basal and lower spinous cells Scaly skin patches; “butterfly rash”; altered pigmentation Basement membrane zone Linear IgA disease Chronic ulcerative stomatitis Discoid lupus Positive Nikolsky’s sign Lesions heal with scarring; Occasional “blood” blisters Similar to erosive lichen planus but does not respond to steroids; No Nikolsky’s sign White plaques with papular rimming TARGET OF AUTOANTIBODIES* *Target of T-cells is bsal cells Hemidesmosomes 21 Traumatic Ulcerations of the Oral Mucosa Traumatic ulcer Traumatic ulcerative granuloma Denture ulcer Anesthetic necrosis Thermal burn Electrical burn Chemical burn Etiology Physical injury such as biting the tongue or contact with sharp object Traumatic ulcer that receives persistent mild chronic trauma New denture with illadapted flange; prolonged denture wearing Ischemia from epinephrine in local anesthetic or trauma during injection Contact with hot foods such as pizza Contact with live electrical cord or extension cord Contact with caustic medications, dental materials, improper use of analgesics, mouth rinses Clinical Features Usually single, well-defined area of erythema surrounding yellow fibrinopurulent membrane; slightly raised border; tender/painful; resolves in 7 to 10 days with removal of etiology Long duration; raised rolled border; crater with yellow fibrinopurulent membrane; nonpainful or mildly tender; slow to resolve with removal of etiology; often requires surgical excision and healing by primary intention Ovoid erythematous area with yellow necrotic center; contacts irregular area of denture; resolves with denture adjustment Usually on hard palate at injection site; painful welldefined intense red area with central necrosis; heals without treatment in 10 to 14 days Painful yellow to white zone of necrosis of surface mucosa of palate or buccal mucosa; tissue sloughs; patient reports etiologic event; resolve with no treatment Yellow to black painless area that gradually becomes edematous; sloughs and bleeds; usually on lips of children Superficial white corrugated or “cracked” appearance; epithelium sloughs leaving red painful surface; resolves without treatment in 10 to 14 days 22 Drugs Associated With Osteonecrosis of the Jaws Drug Intravenous Bisphosphonates Pamidronate Zoledronic acid Trade Name Aredia Use Indications Metastasis of cancer to bone; multiple myeloma Zometa Metastasis of cancer to bone Zoledronic acid Reclast (once annually) Osteoporosis Boniva (every 3 months) Osteoporosis Oral Bisphosphonates Alendronate Fosamax Osteoporosis Ibandronate Boniva Osteoporosis Risedronate Monoclonal Antibodies Denosumab Actonel Osteoporosis Prolia Metastasis of cancer to bone; multiple myeloma; osteoporosis Bevacizumab Avastin Breast cancer relapse; prostate cancer metastasis Ibandronate 23 Syndromes Associated With Hereditary Gingival Overgrowth SYNDROME OROFACIAL CHARACTERISTICS OTHER FEATURES Rutherford Delayed eruption; dentigerous Mental retardation; corneal cysts opacities Defects of ears, nose Hepatosplenomegaly; defects of Zimmerman-Laband fingers Cowden Papillomatosis of gingival, oral Hamartomas; neoplasms mucosa, and face Goltz-Gorlin Gingival, oral papillomatosis; Poikiloderma; adactyly; lip and tooth defects syndactyly; 90% female Murray-Puretic- Fibromas of head, trunk, and Suppuration of skin and Dresher extremities mucosa; mental retardation; flexion contractures Cross Ramon Microphthalmia; White hair; mental retardation; hypopigmentation athetosis; corneal clouding Hypertrichosis; cherubism Juvenile rheumatoid arthritis; mental retardation; epilepsy 24 Oral Squamous Cell Carcinoma: 5-year Survival by Stage at Diagnosis Stage I Stage II Stage III Stage IV Posterior tongue <t>60% 50% 20% 20% Anterior tongue 71% 59% 47% 37% Floor of mouth 73% 60% 36% 30% Gingiva 90% 90% 90% 35% Retromolar area 90% 90% 90% 60% Soft palate 90% 80% 50% 50% Buccal mucosa 90% 90% 70% 60% Lip 96% 83% 57% 48% Tonsil 70% 50% 30% 14% Maxillary sinus 70% 60% 30% 18% Site Retrieved August 2012 from www.cancer.org/.../oral-cavity-and-oropharyngeal-cancer-survivalrates 25 Critical evaluation of diagnostic aids for the detection of oral cancer. Lingen MW1, Kalmar JR, Karrison T, Speight PM. 1 Oral Oncology. 2008 Jan;44(1):10-22 Abstract Historically, the screening of patients for signs of oral cancer and precancerous lesions has relied upon the conventional oral examination. A variety of commercial diagnostic aids and adjunctive techniques are available to potentially assist in the screening of healthy patients for evidence of otherwise occult cancerous change or to assess the biologic potential of clinically abnormal mucosal lesions. This manuscript systematically and critically examines the literature associated with current oral cancer screening and case-finding aids or adjuncts such as toluidine blue, brush cytology, tissue reflectance and autofluorescence. The characteristics of an ideal screening test are outlined and the authors pose several questions for clinicians and scientists to consider in the evaluation of current and future studies of oral cancer detection and diagnosis. Although the increased public awareness of oral cancer made possible by the marketing of recently-introduced screening adjuncts is commendable, the tantalizing implication that such technologies may improve detection of oral cancers and precancers beyond conventional oral examination alone has yet to be rigorously confirmed. Am Dent Assoc. 2010 May;141(5):509-20. Evidence-based clinical recommendations regarding screening for oral squamous cell carcinomas. Rethman MP1, Carpenter W, Cohen EE, Epstein J, Evans CA, Flaitz CM, Graham FJ, Hujoel PP, Kalmar JR, Koch WM, Lambert PM, Lingen MW, Oettmeier BW Jr, Patton LL, Perkins D, Reid BC, Sciubba JJ, Tomar SL, Wyatt AD Jr, Aravamudhan K, Frantsve-Hawley J, Cleveland JL, Meyer DM; American Dental Association Council on Scientific Affairs Expert Panel on Screening for Oral Squamous Cell Carcinomas. Abstract BACKGROUND: This article presents evidence-based clinical recommendations developed by a panel convened by the American Dental Association Council on Scientific Affairs. This report addresses the potential benefits and potential risks of screening for oral squamous cell carcinomas and the use of adjunctive screening aids to visualize and detect potentially malignant and malignant oral lesions. TYPES OF STUDIES REVIEWED: The panel members conducted a systematic search of MEDLINE, identifying 332 systematic reviews and 1,499 recent clinical studies. They selected five systematic reviews and four clinical studies to use as a basis for developing recommendations. RESULTS: 26 The panel concluded that screening by means of visual and tactile examination to detect potentially malignant and malignant lesions may result in detection of oral cancers at early stages of development, but that there is insufficient evidence to determine if screening alters disease-specific mortality in asymptomatic people seeking dental care. CLINICAL IMPLICATIONS: The panel suggested that clinicians remain alert for signs of potentially malignant lesions or early-stage cancers while performing routine visual and tactile examinations in all patients, but particularly in those who use tobacco or who consume alcohol heavily. Additional research regarding oral cancer screening and the use of adjuncts is needed. 27 HPV-Linked Oral Cancers May Not Be 'Contagious' Kissing doesn't seem to raise rate of viral infection between committed partners, study finds WebMD News from HealthDay By Dennis Thompson HealthDay Reporter TUESDAY, April 29, 2014 (HealthDay News) -- Romantic intimacy in long-term relationships often suffers when one partner gets a diagnosis of mouth or throat cancer caused by HPV, the sexually transmitted human papillomavirus. But new research suggests these couples can kiss as much and as deeply as they ever have, without worry. Spouses and long-term partners of patients with HPV-related oral cancers appear to have no increased risk of oral HPV infections, according to the results of a new study led by Johns Hopkins investigators. Saliva samples taken from the partners of oral cancer patients did not contain elevated levels of HPV DNA, the researchers reported online April 28 in the Journal of Clinical Oncology. The prevalence of HPV among spouses and partners -- about 1.2 percent -- is comparable to the 1.3 percent prevalence of HPV among the general population of the same age, the researchers found. Experts welcomed the findings. "This study does put the risk in perspective. It's not something you need to freak out about, or substantially alter your lifestyle. You can still smooch your sweetie," said Fred Wyand, spokesman for the American Sexual Health Association. HPV-related oral cancers are increasing among white men in the United States, with the virus now associated with nearly three out of four cases of oropharyngeal cancer, according to a 2011 report in the Journal of Clinical Oncology. These include cancers of the base of the tongue, tonsils, soft palate and pharynx. Although sexual behavior is associated with oral HPV infection, it's not fully clear how the cancer-causing virus is transmitted or progresses, according to background information in the new report. Once diagnosed, fear of HPV transmission can lead to anxiety, divorce and curtailing of sex and intimacy among couples, said the study's lead author, Gypsyamber D'Souza, associate professor of epidemiology at the Johns Hopkins Bloomberg School of Public Health. New York City oncologist Dr. Dennis Kraus said it's normal for older couples in long-term relationships to become unsettled by the news that one of them has mouth and throat cancer caused by a sexually transmitted virus. "They think, 'What kind of a relationship am I involved in? Who is this person?' Many of them have grandchildren and even great-grandchildren and now they have to be worried about their progeny being exposed to this disease," said Kraus, director of the Center for Head and Neck Oncology at Lenox Hill Hospital. To confront these concerns, researchers took mouth-rinse samples from 164 patients with HPV-related oropharyngeal cancer and 93 partners. They then ran DNA tests for 36 strains of HPV. Nine out of 10 of the oral cancer patients were men, and nearly all had performed oral sex in the past. They were in their 50s and early 60s. More than half of the cancer patients had detectable HPV in their saliva at the time of the test, but the virus showed up in only 1.2 percent of the partners tested. "While oral HPV DNA was common in people with cancer, their spouses did not have an elevated prevalence," D'Souza said. "That suggests either oral HPV is not being transmitted in the saliva when the partners kiss, or they have effectively cleared the infections they've been exposed to." 28 D'Souza said that most people clear HPV infections within a year or two, and persistent infections can take many years to lead to cancer. "Partners who have been together for many years have already shared any infections they are going to share," she said. However, new romantic partners should know that they stand a chance of being infected with oral HPV, even though the infection may not be long-lasting, said Dr. Snehal Bhoola, a gynecologic oncologist with Arizona Oncology, a US Oncology Network affiliate in Phoenix. "It is possible that HPV may be transmitted to new partners, but this appears to be cleared within one to two years in the majority of patients," Bhoola said. Female partners of HPV-positive patients should continue routine cervical cancer screening per recommended guidelines, he added. While most people acquire an oral HPV infection by performing oral sex, researchers have not yet tackled whether it can work the other way -- a person with oral HPV transmitting the virus to their partner's genitals during oral sex, D'Souza said. 29