Pediatrics Rotation Syllabus
Department of Physician Assistant Studies
Learning. Caring. Serving. Leading.
PAS 632 Pediatrics
3 Semester Hours
Course Director: Office Phone E-mail
Diane Duffy, MD FC 205 336-278-6848 dduffy2@elon.edu
Tracey Tonsor, PA-C FC 207 336-278-6852 ttonsor@elon.edu
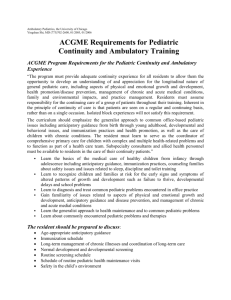
Course Description:
The Pediatric Medicine rotation is designed to give students exposure to the spectrum of pediatric practice, including care of infants, children and adolescents in routine well-child care and care of acute and chronic diseases. The student will recognize the role that understanding the developmental stage of a patient plays in the approach to, examination of and treatment of a pediatric patient.
Course Goals:
The educational goals of the Clinical: Pediatrics rotation include:
1.
To apply the medical content and principles that define the care of pediatric patients.
2.
To provide opportunities for each student to develop the core PA competencies in a supervised pediatric setting.
3.
To expose each student to an experienced and competent medical provider role model for the care of pediatric patients.
Learning Outcomes:
Upon completion of this course clinical phase PA students will:
1.
Clinical Skills: Demonstrate the clinical skills required to competently provide individualized care to pediatric patients.
2.
Health Supervision: Demonstrate the skills needed for thorough assessment and implementation of health supervision.
3.
Growth: Integrate pediatric patients’ growth pattern in the assessment of their overall health.
4.
Development: Assess the development of a child and make recommendations for follow up evaluation based on the screening tools commonly used in pediatric practice.
5.
Behavior: The student will provide anticipatory guidance to parents regarding behavior norms in children and be able to offer advice to parents regarding behavioral issues.
6.
Nutrition: Accurately assess patients’ nutritional status and needs through detailed nutritional history taking and observation.
7.
Adolescence: Interact with adolescent patients in an appropriate manner, recognizing the unique physical, cognitive and psychosocial changes that typically occur in this age group.
1 Revised 10/23/13
8.
Newborn: Understand the unique physiological changes that occur immediately after birth and through the first month of life and apply this understanding to the care of the infant and in communicating with parents the unique needs and vulnerabilities of this patient population.
9.
Common Acute Pediatric Illnesses: Use information obtained from the history and physical exam and when appropriate laboratory tests and/or imaging studies to develop a differential diagnosis and treatment plan for each of the problems identified. The student will demonstrate knowledge of disease etiology, pathophysiology and epidemiology and their relation to patient gender, age, ethnicity and prior health status.
10.
Common Chronic Illnesses and disability: Understand the long term medical implications and complications of chronic illnesses and apply that understanding to the decision making process in recommending treatment options to patients and their families.
11.
Therapeutics, Fluid and Electrolyte Management: Recommend therapeutic intervention based on an understanding of pharmacokinetics of medications and their knowledge of the influence of growth and physiologic maturation in addition to a child’s psychomotor development and behavior on the form of medication dispensed and the expectation for compliance. Assess fluid balance in a pediatric patient and correctly manage disorders of fluid or electrolyte balance.
12.
Child Abuse and Neglect: Understand, recognize and address the types of abuse seen in pediatric patients including physical, sexual and or emotional abuse in addition to neglect.
Teaching Methodologies:
The content of this module will be presented through a variety of methods that include observation and participation at the clinical site, independent reading and participation in online activities developed to guide experiential learning.
Accommodations:
Students requiring academic accommodations must follow the “Academic Support” policy in the Elon University DPAS Student Handbook.
Academic Honesty:
All Elon PA students acknowledged their commitment to abide by the Elon Honor
Code by signing the Honor Pledge during orientation. Students will sign an Honor Pledge (electronically or manually) each time an assignment is turned in or an examination is started to reaffirm their complete understanding of the Honor Code of Elon University and their affirmation that their work abides by that Code.
Required Textbooks:
1.
All first-year required textbooks.
2.
Current Pediatric Diagnosis & Treatment by Hay et. al., 15th Ed.
3.
Harriet Lane Handbook , 16th Ed., ISBN: 0-323-01486-0
Other Resources:
1.
*Moodle: Please check the course site frequently for new announcements, updated schedules, assignments and other course communication.
2.
Practicing physician assistants, physicians, allied health care providers and laboratory teaching
2 Revised 10/23/13
TOPICS aids.
Dermatology
Dermatitis- Diaper
Dermatitis –Perioral
Drug Eruptions
Lichen planus
Pityriasis rosea
Stevens-Johnson Syndrome
Toxic epidermal necrolysis
Erythema multiforme
Acne vulgaris
Lice
Scabies
Androgenetic alopecia
Exanthems
Verrucae
Burns
Urticaria
Contact dermatitis
Atopic dermatitis
Tinea
Impetigo
EENT
Conjunctivitis
Orbital cellulitis
Strabismus
Acute otitis media
Allergic rhinitis
Hearing impairment
Mastoiditis
Otitis externa
Inguinal hernia
Umbilical hernia
Niacin deficiencies
Vitamin A deficiency
Tympanic membrane perforation Vitamin D deficiency
Epistaxis Lactose intolerance
Acute pharyngotonsillitis Genitourinary
Epiglottitis
Oral candidiasis
Peritonsillar abscess
Cardiovascular
Atrial septal defect
Coarctation of the aorta
Patent ductus arteriosus
Tetralogy of Fallot
Ventricular septal defect
Acute rheumatic fever
Kawasaki disease
Hypertrophic cardiomyopathy
Cryptorchidism
Hydrocele
Paraphimosis
Phimosis
Testicular torsion
Enuresis
Hypospadias
Vesicourethral reflux
Glomerulonephritis
Cystitis
Cardiology (cont’d)
Syncope
Pulmonary
Acute bronchiolitis
Croup
Pneumonia-bacterial
Respiratory syncytial virus
Asthma
Foreign body
Hyaline membrane disease
Cystic fibrosis
Gastrointestinal/Nutritional
Gastroenteritis
Dehydration
Appendicitis
Colic
GERD
Constipation
Pyloric stenosis
Intussusception
Hirschprung disease
Foreign body
Encopresis
Hepatitis
Jaundice
Duodenal atresia
3
Hematology
Anemia
Bleeding disorders
Leukemia
Lymphoma
Neutropenia
Brain tumors
Hemophilia
Lead poisoning
Endocrinology
Short stature
Hypothyroidism
Hypercalcemia
Obesity
Diabetes mellitus
Musculoskeletal
Nursemaid’s elbow
Slipped capital femoral epiphysis
Osgood-Schlatter’s disease
Scoliosis
Congenital hip dysplasia
Avascular necrosis of the
proximal femur
Neoplasia of the musculoskeletal
System
Juvenile rheumatoid arthritis
Infectious Disease
Atypical mycobacterial diease
Pinworms
Epstein-Barr viral disease
Erythema infectiosum
Herpes simplex
Influenza
Mumps
Roseola
Rubella
Measles
Varicella
Hand-foot-and-mouth disease
Pertussis
Revised 10/23/13
Topics (cont’d)
Neurology/Developmental
Normal growth & development
Immunization guidelines
Anticipatory guidance
Teething
Febrile seizures
Epilepsy
Meningitis
Turner syndrome
Down syndrome
Assessment Activities:
Exams/quizzes (25%), Preceptor Evaluation (65%), Professionalism (10%).
Behavioral Medicine
Child abuse
ADHD
Autistic disorder
Eating disorders
Depression
Anxiety
Conduct disorders
Suicide
Grade Scale and Grade Points:
Percentage
89.50-100
85.50-89.49
79.50-85.49
75.50-79.49
69.50-75.49
Below 69.50
There is no rounding of grades.
Letter Grade
A
B+
B
C+
C
U
Grade points
4.0
3.3
3.0
2.3
2.0
0
Note: For further information regarding academic standing in the Department of Physician
Assistant Studies, please see the Student Handbook.
Grading Criteria:
1.
Demonstrate acquisition of a strong basic science and medical science knowledge base as demonstrated on the written examination/quizzes.
2.
Demonstrate satisfactory self-directed learning skills, clinical reasoning skills, commitment to patient-centered care and professionalism as evidenced by satisfactory performance on the preceptor evaluation.
3.
Demonstrate a commitment to learning and professionalism by actively participating in all clinical activities and exceeding the professional behavior standards and minimum requirements for clinical rotations available in the Elon PA Student Handbook.
Instructional Objectives:
1.
Clinical Skills: Possess the skills essential for competent pediatric care including the ability to: a.
Conduct an interview
4 Revised 10/23/13
b.
Perform a physical examination c.
Manage medical data d.
Communicate written and oral information e.
Integrate basic science knowledge f.
Search and read the literature critically.
2.
Health Supervision: Demonstrate the skills needed for thorough assessment and implementation of health supervision including. a.
Assessment of growth and development b.
Advisement on the prevention of disease by immunization c.
Advisement on the prevention of injury d.
Screening for treatable conditions e.
Promoting a healthy environment and healthy lifestyle.
3.
Growth: a.
Understand the influences genetic and environmental factors have on a child’s growth pattern. b.
Accurately obtain the growth parameters of a child and plot them on a standardized growth curve. c.
Interpret the data in relation to the child’s overall health.
4.
Development: Describe normal patterns of development in order to detect deviations that might be the first sign of a medical or psychosocial problem.
5.
Behavior: Discuss the normative and expected behaviors in children and be able to recognize abnormal behavior and counsel parents.
6.
Nutrition: a.
Demonstrate an understanding of pediatric nutritional requirements of healthy children and those with acute and chronic illness. b.
Counsel patients and/or parents on the proper nutritional interventions required for healthy children and those with special nutritional requirements.
7.
Issues Unique to Adolescence: a.
Describe the unique features of the physician assistant-patient relationship during adolescence including confidentiality and consent. b.
Identify and describe the sequence of the physical changes of puberty (e.g. Tanner scale). c.
List the components of health supervision for an adolescent, such as personal habits, pubertal development, immunizations, acne, scoliosis, sports participation, and indications for pelvic exam. d.
Describe the common risk-taking behaviors of adolescents, such as alcohol and other drug use, sexual activity and violence. e.
Describe the contributions of unintentional injuries, homicide, suicide and HIV/AIDS to the morbidity and mortality of adolescents. f.
Describe the features of common mental health problems in adolescence, including school failure, attention deficit, body image, eating disorders, depression and suicide. g.
Describe an approach to counseling an adolescent regarding sexual activity, substance abuse, and personal safety. h.
Describe the unique difficulties encountered by adolescents with chronic diseases, including adherence and issues of autonomy vs. dependence. i.
Discuss the characteristics of early, mid and late adolescence in the terms of cognitive and psychosocial development.
5 Revised 10/23/13
j.
Interview an adolescent patient, using the HEADSS method, to ask sensitive questions about lifestyle choices that affect health and safety (e.g. sexuality, drug, tobacco and alcohol use) and give appropriate counseling k.
Conduct a physical examination of an adolescent that demonstrates respect for privacy and modesty, employing a chaperone when appropriate. l.
Conduct a pre-participation sports examination and demonstrate the key components of that examination necessary to clear an individual for participation in strenuous exercise (special senses, cardiac, pulmonary, neurological, and musculo-skeletal). m.
Conduct a health supervision visit for a healthy adolescent, incorporating a psychosocial interview, developmental assessment and appropriate screening and preventive measures.
8.
Issues Unique to the Newborn: a.
Describe the transition from the intrauterine to the extrauterine environment, including temperature regulation, cardiovascular/respiratory adjustment, glucose regulation, and initiation of feeding. b.
List the information from the history of pregnancy, labor, and delivery obtained from the parents or medical record that has implications for the health of the newborn. c.
Describe how gestational age can be assessed with an instrument such as the Ballard scale and identify key indications of gestational maturity. d.
Describe the challenges for parents adjusting to a new infant in the home. e.
List the differential diagnosis and complications for the following common problems that may occur in the newborn. i.
Jaundice ii.
Respiratory distress iii.
Poor feeding iv.
Large and small for gestation infants v.
"State" abnormalities which includes tremulousness, irritability, lethargy from causes such as drug withdrawal, hypoglycemia, sepsis vi.
Prematurity f.
Describe how gestational age affects risks of morbidity or mortality in the newborn period (for example lung disease, hypothermia, and glucose homeostasis) g.
Perform a complete physical examination of the newborn infant. h.
Give parents of a newborn anticipatory guidance for the following issues: i.
The benefits of breast-feeding vs. formula for the newborn and mother ii.
Normal bowel and urinary elimination patterns iii.
Normal neonatal sleep patterns iv.
Newborn screening tests to include screens for metabolic and infectious conditions and hearing loss v.
Appropriate car seat use vi.
Prevention of SIDS ("back to sleep"): vii.
Immunizations (e.g. HBV) viii.
Medications (e.g. eye prophylaxis and vitamin K) ix.
The role of circumcision
9.
Common Acute Pediatric Illnesses: a.
Describe the etiology, pathophysiology, epidemiology, clinical presentation, diagnostic criteria and therapeutic management pertinent to the age appropriate differential
6 Revised 10/23/13
diagnosis for pediatric patients presenting with each of the following symptoms, physical abnormalities or laboratory findings.
1.
Abdominal pain
2.
Cough and/or wheeze
3.
Diarrhea
4.
Fever and rash
5.
Fever without a source
6.
Headache
7.
Lethargy or irritability
8.
Limp or extremity pain
9.
Otalgia
10.
Rash
11.
Rhinorrhea
12.
Seizures
13.
Sore throat
14.
Vomiting
15.
Abdominal mass
16.
Bruising
17.
Heart murmur
18.
Hepatomegaly
19.
Lymphadenopathy
20.
Splenomegaly
21.
Petechiae and/or purpura
22.
Red or wandering eye
23.
White pupillary reflex
24.
Anemia
25.
Hematuria
26.
Proteinuria
27.
Positive Mantoux skin test (PPD) b.
Explain how the physical manifestations of disease and the evaluation and management may vary with the age of the patient. c.
Discuss the characteristics of the patient and the illness that must be considered when making the decision to manage the patient in the hospital or in the outpatient setting.
10.
Common Chronic Illnesses and disability: a.
Describe the clinical features of chronic medical conditions seen in children such as: i.
Asthma ii.
Atopic dermatitis iii.
Cerebral palsy iv.
Cystic fibrosis v.
Diabetes mellitus vi.
Epilepsy vii.
Malignancy (e.g. acute lymphocytic leukemia and Wilms tumor) viii.
Obesity ix.
Seasonal allergies x.
Sickle cell disease xi.
HIV/AIDS xii.
Sensory impairment
7 Revised 10/23/13
b.
Describe how chronic illness can influence a child's growth and development, educational achievement, and psychosocial functioning. c.
Describe the impact that chronic illness has on the family's emotional, economic and psychosocial functioning. d.
Describe the impact of a patient's culture on the understanding, reaction to, and management of a chronic illness e.
Describe the contributions of each member of a multidisciplinary health care team in caring for children with a chronic illness. f.
Identify the key components of delivering "Bad News" in relation to chronic illness. g.
Explain the management strategies for common chronic illnesses seen in children such as asthma, seasonal allergies, diabetes, and atopic dermatitis. h.
Perform a medical interview and a physical examination in a child with a chronic illness that includes: i.
The effects of the chronic illness on growth and development. ii.
The emotional, economic and psychosocial functioning of the patient and family. iii.
The treatments used, including "complementary and alternative therapies.
11.
Therapeutics, Fluid and Electrolyte Management:. a.
Describe how to assess whether a drug is excreted in the breastmilk and is safe to use by a breast-feeding mother. b.
List medications such as aspirin, tetracycline, and oral retinoic acid that are contraindicated or must be used with extreme caution in specific pediatric populations. c.
Describe the appropriate use of the following common medications in the outpatient setting, including when it is NOT appropriate to treat with a medication: i.
Analgesics / antipyretics ii.
Antibiotics iii.
Bronchodilators iv.
Corticosteroids v.
Cough and cold preparations vi.
Ophthalmic preparations vii.
Otic preparations viii.
Vitamin / mineral supplements d.
Select generally accepted pharmacologic therapy for common or life-threatening conditions in pediatric patients. e.
Describe the ways medication errors are systemically prevented. f.
Calculate a drug dose for a child based on body weight. g.
Write a prescription e.g. for a common medication such as an antibiotic. h.
Negotiate a therapeutic plan with the patient and family to maximize adherence with the agreed upon treatment regimens and assess the family's understanding of the plan. i.
Describe the conditions in which fluid administration may need to be restricted (such as the syndrome of inappropriate ADH secretion, congestive heart failure, or renal failure) or increased (e.g. fever). j.
Describe the physical findings in hypovolemic shock and the approach to restoration of circulating fluid volume (i.e. "rescue" fluid infusion). k.
Describe the causes and consequences of fluid imbalances and electrolyte disturbances leading to dehydration and such conditions as hypernatremia, hyponatremia, hyperkalemia, hypokalemia, and severe acidosis.
8 Revised 10/23/13
l.
Obtain historical and physical finding information necessary to assess the hydration status of a child. m.
Calculate and write orders for intravenous maintenance fluids for a child considering daily water and electrolyte requirements. n.
Calculate and write orders for the fluid therapy for a child with severe dehydration caused by gastroenteritis to include "rescue" fluid to replenish circulating volume, deficit fluid, and ongoing maintenance. o.
Explain to parents how to use oral rehydration therapy for mild to moderate dehydration.
12.
Child Abuse and Neglect: a.
Students will understand the medical, legal, and social implications of suspected abuse and recognize the role of the medical provider in preventing child abuse and family violence, through routine assessment of family dynamics, early identification of children at risk and cooperation with community services that support families.
9 Revised 10/23/13