My thoughts re rehab programme pilot
advertisement

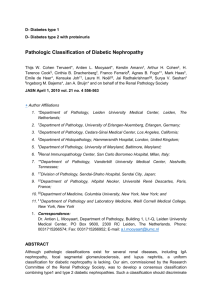
O50 RESTORATION OF ENDOTHELIAL GLYCOCALYX AND IMPROVED OUTCOMES IN DIABETIC NEPHROPATHY Y Qiu, M Stevens, C Neal, S Oltean, A Salmon Physiology and Pharmacology, University of Bristol INTRODUCTION: Diabetic nephropathy (DN) is the leading cause of end-stage renal failure in the western world. Increased urinary albumin excretion is a characteristic early feature in many patients with diabetic nephropathy, and is considered to represent dysfunction of the glomerular capillary wall. Current treatments for diabetic nephropathy include agents that target glomerular capillary hypertension (such as renin-angiotensin system blockade), as well as control of systemic parameters such as glycaemia, hyperlipidaemia and platelet aggregation. There are no therapies directly targeted to improve the function of the glomerular capillary wall. We have previously shown that the VEGF-A isoform VEGF-A165b modifies glomerular capillary wall permeability and improves functional and histological outcomes in diabetic nephropathy. The endothelial glycocalyx is a hydrated glycosaminoglycan- and proteoglycan-rich matrix covering the surface of all endothelial cells. In the glomerulus, the endothelial glycocalyx forms the innermost layer of the glomerular filtration barrier. Initial studies indicate a reduction in whole-body and systemic capillary endothelial glycocalyx in patients with diabetes and microalbuminuria (Nieuwdorp et al, Diabetes, 2006), but the endothelial glycocalyx covering the glomerular capillary wall has not previously been examined in diabetes. The mechanism of action of VEGF-A165b is also uncertain. We hypothesised that a reduction in glomerular endothelial glycocalyx would occur in diabetes, and that improved outcomes in diabetic nephropathy following VEGF-A165b treatment would be associated with long-term restoration of the endothelial glycocalyx in diabetes. METHODS: Adult male DBA2/J mice were rendered diabetic with streptozotocin; nondiabetic control animals received sodium citrate buffer alone. Following confirmation of hyperglycaemia (>15mmol/L) in diabetic animals, diabetic mice either received bi-weekly intraperitoneal injections of recombinant human VEGF-A165b (with non-diabetic animals receiving bi-weekly intraperitoneal injections of phosphate-buffered saline (PBS: vehicle) alone), or were exposed to high local concentrations of VEGF-A165b through podocyte-specific overexpression under control of the nephrin promoter. At the end of the study, animals were sacrificed by schedule 1 methods, including by cardiac perfusion with gluteraldehyde and alcian blue for transmission electron microscopy. All studies were conducted in accordance with UK Home Office Legislation. RESULTS: Both podocyte-specific VEGF-A165b over-expression and systemic VEGF-A165b injections reduced albuminuria and improved histology in diabetic mice. Glomerular VEGFR2 was upregulated in VEGF-A165b-treated mice, and this upregulation co-localised with the endothelial cell marker PECAM-1. In diabetic mice, glomerular endothelial fenestral density was reduced by half in vehicle-treated mice, but was unaltered by VEGF-A165b treatment. In diabetic mice, the depth of the glomerular endothelial glycocalyx was also reduced by half, but VEGF-A165b treatment of diabetic mice restored the endothelial glycocalyx to normal levels. CONCLUSION: The glomerular endothelial glycocalyx is damaged in diabetic nephropathy, consistent with the observed alterations in albuminuria and glomerular water permeability. VEGF-A165b improves outcomes in diabetic nephropathy, and acts on the glomerular endothelium. Long-term restoration of the endothelial glycocalyx in diabetes is feasible, in this case with improved outcomes following systemic treatment with VEGF-A165b. Restoration of the endothelial glycocalyx may be a novel approach to improve microvascular function in diabetic nephropathy.