Central Nervous System Infections
advertisement
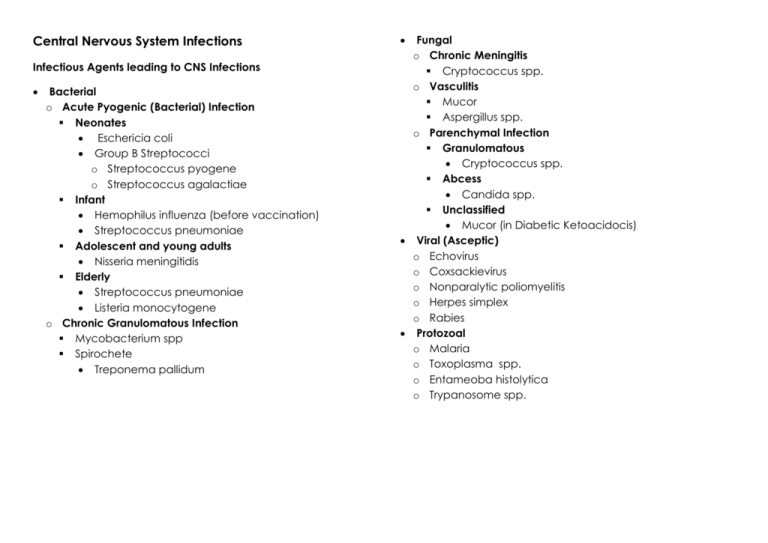
Central Nervous System Infections Infectious Agents leading to CNS Infections Bacterial o Acute Pyogenic (Bacterial) Infection Neonates Eschericia coli Group B Streptococci o Streptococcus pyogene o Streptococcus agalactiae Infant Hemophilus influenza (before vaccination) Streptococcus pneumoniae Adolescent and young adults Nisseria meningitidis Elderly Streptococcus pneumoniae Listeria monocytogene o Chronic Granulomatous Infection Mycobacterium spp Spirochete Treponema pallidum Fungal o Chronic Meningitis Cryptococcus spp. o Vasculitis Mucor Aspergillus spp. o Parenchymal Infection Granulomatous Cryptococcus spp. Abcess Candida spp. Unclassified Mucor (in Diabetic Ketoacidocis) Viral (Asceptic) o Echovirus o Coxsackievirus o Nonparalytic poliomyelitis o Herpes simplex o Rabies Protozoal o Malaria o Toxoplasma spp. o Entameoba histolytica o Trypanosome spp. Types of CNS Infections 1. Bacterial Infections a. Acute Pyogenic Meningitis b. Chronic Granulomatous Meningitis i. Tuberculous meningitis ii. Neurosyphilis iii. Neurborelliosis iv. Tabes dorsalis c. Abscess i. Epidural abscess ii. Subdural abscess iii. Brain abscess 2. Fungal Infections a. Chronic fungal meningitis 3. Viral Infections a. Acute asceptic meningitis b. Viral encephalitis c. Herpes simplex encephalitis 4. Protozoal Infection a. Toxoplasmosis 5. Prions Diseases a. Creutzfeldt-Jakob Disease (CJD) b. Gerstman-straussler Syndrome (GSS) c. Fatal familial insomnia d. Kuru Bacterial Infections Disease Acute Pyogenic Meningitis Bacterial infection of the o Arachnoid membrane o Subarachnoid space o CSF Morphology Macroscopic Microscopic Pathogenesis Heamatogenous spread (the most common) o The etiological agents spread from distant area of the body and lodged at the CNS Direct implantation of organisms o Trauma o Congenital malformation – ventricular septal defect o Iatrogenic Lumbar puncture Local extension o Sinusitis Mastoid sinus Frontal sinus o Infected tooth o Osteomyelitis of the Cranium Spine Pathophysiology Vasculitis of the leptomeningeal arteries lead to an ischemic attack of the brain o Hypoxic-Ischemic Encephalopathy (HIE) will then develop Infection hs led to disturbance in vascular permeability of the brain o This has led the to brain edema and leakage of protein into the CSF o Ultimately, increased in ICP Yellow-tan exudate o This purulent exudate covers the cerebral hemispheres o It usually settles at Along the base of the brain Around cranial nerves Openings to the 4th ventricle Meningeal arteries appeared engorged Neutrophilic exudate is seen involving the meninges Prominent dilated blood vessels especially the Leptomeningeal vessels Edema and focal inflammation extending into the superficial brain parenchyma (Virchow-Robin space) Complications 1. Cranial Nerves deficits and ischemic infarction a. During infection, veins may inflamed and lead to Phlebitis b. Phlebitis may disrupt blood flow, turbulance may lead to formation of blood clot c. Blood clot may ultimately occlude smaller vessels and lead to liquefactive necrosis of the brain 2. Hydrocephalus a. Purulent fibrinous exudate of infection may organize into fibrous tissue b. This fibrous tissue may block the exit of CSF at the 4th ventricle and lead to communicating hydrocephalus Complications take times to develop, sometimes it develops long after the disease subsides Clinical Manifestation Initial symptoms Fever Severe headache Stiff neck Progression of disease Confusion Coma Seizure o Due to ↑ICP HIE Toxic Metabolic Encephalop athy Later complications Cranial nerve deficits Ischemic infarction Hydrocephalus Laboratory Findings Lumbar puncture o Increased in ICP o Abundant neutrophils o Elevated proteins o Reduced glucose Lumbar puncture is only indicated in pts without sign of Papiloedema Bacterial Infections Disease Brain Abscess Morphology Macroscopic Microscopic Pathogenesis Local extension o Sinusitis Mastoid sinus Frontal sinus o Infected tooth o Osteomyelitis of the Cranium Spine Heamatogenous spread (the most common) o The etiological agents spread from distant area of the body and lodged at the CNS Direct implantation of organisms o Trauma Post meningitis Descrete lesion with liquefactive necrosis Edema o Presented with expanded white matter adjacent to the abscess Dense aggregates of neutrophils Necrotic area surrounded with granulation tissue Neovascularization Outside the capsule of abscess is the zone of gliosis o With numerous Gemistocytic Astrocytes Disease Pathogenesis Subdural Abscess Evolution of the Abscess 1. The brain undergoes acute inflammatory response after come into contact with foreign agents, characterized with a. Neutrophilic infiltration b. Cerebritis 2. When the brain tries to heal the lesion, granulation tissue forms at the peripheral of the lesion; middle zone undergoes liquefactive necrosis 3. Sattellite abscess has a very poor capsulation at the medial side; therefore it is easily rupture and the pus may enter the ventricle Epidural Abscess Clinical Manifestation Ussually occurs due to complication of vertebral osteomyelitis Sometimes due to complications of o Spinal surgery o Trauma o Spinal anesthesia Extension of bacterial or fungal infection of the o Cranium o Sinuses o Middle ear Etiological agents Staphylococcus aureus (most cases) Gram negative rods o Bacteroides Streptococci spp. Mycobacterium tuberculosis Most commonly affected area o Frontal lobe o Parietal lobe o Cerebellum Features o Progressive focal deficit Loss of neurological function due to destruction of the brain tissue o Subsequent increased in ICP o Progrssive herniation If the abscess ruptures, it will lead to o Ventriculitis o Meningitis o Venous sinous thrombosis Clinical Manifestation Initially presented with o Fever o Back pain Progression o Weakness of the lower extremities o Impaired Bowel function Bladder function Ends up with paralysis Headache Fever Neck stiffness Signs and symptoms of origin infection Ultimately will lead to mass effect if the pus is massive Bacterial Infections Disease Tuberculous Infection of CNS Pathogenesis Spreaded through heamatogenous route and usually comes about from disseminated pulmonary tuberculosis o o o o 1. 2. Morphology Microscopic Macroscopic Mixture of Subarachnoid Lymphocytes space contains Plasma cells o Gelatinous Macrophages o Fibrinous exudate Florid cases show This exudate most well-formed often finds at the granulomas base of brain, Often presented with obliterating caseating necrosis o Cisterns and giant cells o Encasing cranial Mimicking the nerves morphology of May present with pulmonary descrete white tuberculosis granules scattered Obliterative over the endarteritis of artery Leptomeninges running through Tuberculoma may subarachnoid space have a bigger Same appearance lesion for Tuberculoma Complications Hydrocephalus a. Exudate may organize and form arachnoid fibrosis which may occlude the arachnoid granulation leading to communicating hydrocephalus Obliterative Endarteritis a. Artery may become occluded during healing and subsequently leads to cerebral infarction Clinical Manifestation Generalized Headache Malaise Mental confusion Vomiting Laboratory Findings Lumbar puncture Elevated protein Glucose may be o Moderately reduced o Normal Bacterial Infections Disease Neurosyphilis Types 1. Meningovascular neurosyphilis 2. Paretic neurosyphilis 3. Tabes dorsalis Morphology Pathogenesis Happens during the tertiary syphilis This occurs in about 10% of syphilitic patients who didn’t have proper treatment It is caused by spirochete o Treponema pallidum Microscopic Macroscopic Meningovascular Neurosyphilis (Meninges) Lymphocytes and plasma cells appeared at the peripheral to blood vessels Heubner Arteritis o Marked endothelial thickening, thickened Tunica media Tunica adventitia Primarily involved the meninges of the o Base of the brain o Subarachnoid space o Blood vessels Paretic Neurosyphilis (Brain Parenchyma) Loss of neurons with microglial (rod cells) proliferation Gliosis Loss of Ependymal lining with subependymal gliosis o Granular ependymitis Brain appeared o Shrunken o Firm Frontal lobe is atrophic Leptomeninges is thickened With or wihout hydrocephalus Tabes Dorsalis (Spinal Cord) Loss of axons and myelin sheath at the Dorsal Column Pallor and atrophy of the Dorsal Column Clinical Manifestation Meningovascular Neurosyphilis Apathy Seizures General paresis with dementia Paretic Neurosyphilis Insidious loss of mental and physical function Mood alteration o Delusion of grandeur Terminating with severe dementia Tabes Dorsalis Impaired joint position sense Locomotor ataxia Loss of pain sensation Charcot’s joint o Skin and joint damage Lightning pains Loss of deep tendon reflex Fungal Infections Primarily happens in Immunocompromised patients o HIV patients o Debilitated patients o Patients undergoing chemo Disease Pathogenesis Chronic Fungal Meningitis Characterized by 3 patterns o Parenchymal Invasion o Chronic fungal meningitis Abscess forming lesion Cryptococcus spp. Candida spp o Vasculitis Granulomatous lesion Mucor Cryptococcus Aspergillus spp. Invasion of the blood vessel leading to o Heamorrhage o Thrombosis Branching of hyphae can be seen invading the cerebral vessels Morphology Clinical Laboratory Manifestation Findings Microscopic Macroscopic Usually well-formed Tubercle like nodule The infections CSF findings granuloma is hardly on the can be o High protein seen Leptomeninges at o Fulminant concentrati Infiltration of chronic the base of the and fatal on inflammatory cells brain within 2 o Few cells including weeks Presence of o Fibroblasts o Indolent and mucoid o Mononuclear evolving up encapsulated giant cells to months or yeast in Indian o With presence of years Ink Cryptococci spp. Usually caused by Cryptococcus spp. Brain usually one of the latest organs to infected after disseminated fungal infection Spreaded through heamatogenous route Viral Infections Disease Acute Aseptic Meningitis Generally viral in origin Echovirus Coxsackievirus Nonparalytic poliomyelitis Sometimes can be non-viral in origin (drug-induced) o NSAIDs o Antibiotics Nervous system tropism Certain virus affects certain cells o Others have preference towards particular area of the brain Temporal lobe/ limbic system Herpes simplex Capacity of latency o Varicella-zoster may remain dormant at the dorsal root ganglia It may also follow an immune mediated disease pathway o This has no evidence of direct viral invasion o For example Acute Disseminated Encephalitis Intrauterine infection o May lead to congenital malformation May follow a slowly degenerating disease o Postencephalitic Parkinsonism General characteristics Perivascular and parenchymal mononuclear cells infiltration o Lymphocytes o Plasma cells o Macrophages Gliosis with/out nodules Neurophagia Nuclear/cytoplasmic inclusion bodies can be found Herpex Simplex Encephalitis Large eosinophilic intranuclear inclusion Rabies Negri bodies o Round to oval in shape o Eosinophilic cytoplasmic inclusion o Found in Neurons in Hippocampus Pyramidal cells of the Cerebellum CMV Owl eyes o Intranuclear and cytoplasmic inclusion Measles Warthin Finkeldey Bodies in Subacute Sclerosing Panencephalitis (SSPE) JC Virus Progressive Multifocal Leucoencephalopathy (PML) o o o o Viral Encephalitis Morphology Microscopic Macroscopic Pathogenesis Usually no abnormalities can be found Sometimes mild to moderate lymphocytic infiltration of the Leptomeninges No distinctive changes can be seen on the brain Sometimes, brain appears edematous General characteristics Almost invariably with meningeal inflammation o Meningoence phalitis Sometimes with the involvement of the spinal cord o Encephalomy elitis Herpex Simplex Encephalitis Petechiae are seen on the Temporal lobe Rabies Intense edematous brain Vascular congestion Clinical Manifestation Less fulminant, and usually self-limiting Laboratory Findings CSF findings Increased in pressure Clear color Increased numbers of Lymphocytes o Slightly increased protein o Normal glucose level Smear and culture appear negative for bacteria o o o Protozoal Infections Disease Pathogenesis Cerebral Toxoplasmosis can be either o Acquired Toxoplasmosis o Congenital Toxoplasmosis Ingestion of the cysts will lead to infection The initial infection takes place at the intestion and regional lymph nodes The cysts formation occurs at the o CNS o Eyes o Cardiac muscle o Skeletal muscle Toxoplasmic Encephalitis Morphology Microscopic Macroscopic Toxoplasma Abscess pseudocyst formation with Often present bradyzoites with multiple foci With/out of calcification granuloma Clinical Manifestation During an acute infection, patients usually appear assymptomatic But when the cysts forms in the CNS, patients will develop o Fever o Headache o Lethargy o Altered mental status o Focal neurological deficits o Convulsions May end with fatality Single or multiple lesions can be seen at the o Basal Ganglia o Junction between the white and gray matter Prions Diseases Disease Prions Diseases a. CreutzfeldtJakob Disease (CJD) b. Gerstmanstraussler Syndrome (GSS) c. Fatal familial insomnia d. Kuru Pathogenesis Groups of diseases with abnormal form of a specific protein, Prion Protein (PrP) o It is itself transmissable particles o Can be directly inoculated PrP undergoes conformational change from Normal α-helix-containing isoform (PrPc) Abnormal β-helix-pleated sheet isoform (PrPsc) PrPsc is located at the Chromosome 20 Accumulation of PrPsc in the neurons appear to be the cause of pathology Largely how does this happens, remains unknown Morphology Microscopic Macroscopic Spongiform Brain atrophy cerebral cortex The progression of o Small disease can be either vacoules in o Very slow dendritic o Rapid cytoplasm o Grape-like cluster Astrocytocis Neuronal loss Clinical Manifestation Most patients develop Dementia Cause Appearance Polymorphonuclear cell Lymphocyte Protein Glucose Pyogenic bacterial meningitis Yellowish, turbid Markedly increased Slightly increased or Normal Markedly increased Decreased Viral meningitis Clear fluid Slightly increased or Normal Markedly increased Slightly increased or Normal Normal Tuberculous meningitis Yellowish and viscous Slightly increased or Normal Markedly increased Increased Decreased Fungal meningitis Yellowish and viscous Slightly increased or Normal Markedly increased Slightly increased or Normal Normal or decreased