Clinical Aspects of Tuberculosis
advertisement

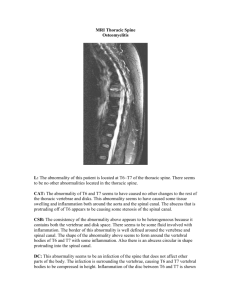
CARIES SPINE AND SPINAL STENOSIS DR. NADIR MEHMOOD ASSOCIATE PROFESSOR SURGERY IIMC-T, RLY HOSP CLINICAL ASPECTS OF TUBERCULOSIS • Pathogenesis of tuberculosis –Infection versus disease •Host factors •Pathogen factors PATHOGENESIS • Host factors include – Social e.g. • Poverty • alcoholism – Age e.g. • Newborn • Teenage girl • Old age – Immunity e.g. • HIV • Gamma interferon PATHOGENESIS • Organism factors e.g. –Virulence factors –[Drug resistance] PATHOGENESIS • Tuberculous disease is a consequence of: – Primary infection e.g. In a baby – Reactivation • ‘natural’ • Associated with immunosupression – Re infection PULMONARY TB TYPICALLY AFFECTS THE UPPER ZONES OF THE LUNG CLINICAL FEATURES • Clinical illness –Pulmonary –Extrapulmonary CLINICAL ILLNESS TB may affect any tissue of the body including: – Skin and soft tissue – Lymph nodes – Bones and joints – Intra abdominal structures including • • • • peritoneum Kidneys Adrenal glands Lymph nodes – Central nervous system • Tuberculoma • meningitis Clinical clues for TB • Clinical symptoms – usually ‘chronic’ rather than acute – – – – Fever Sweats Weight loss Focal symptoms • Epidemiology – History of TB, HIV – Country of origin, recent travel/work – Contact with TB • Investigations- CP ESR,URINE R/E, CXR, X-RAYS, C/S, SKIN TESTS,ELISA, CRP, PCR, CT, MRI TB – guidelines for the clinician • Great mimicker • Low index of suspicion • Pulmonary TB usually easy to consider • Non pulmonary often requires ‘lateral thinking’ What will happen if diagnosis or treatment for TB spinal osteomyelitis is delayed? MENINGES OF THE SPINAL CORD What will happen if treatment delayed? – gibbus formation (acute angulation of spine with or without neurological damage) The physical appearance – Potts disease of spine - gibbus • Progress – Increasing back pain and neurological symptoms – mild leg weakness • Treatment – Continue therapy – consider surgical decompression • Further progress • Weakness of legs • Neurosurgery and internal splinting • Other considerations - clinical • Has the patient got HIV? • Is vitamin D level normal? • Other considerations epidemiological • From where has the pt got infection? • To whom might the pt have given it? TREATMENT OF TB • BTS guidelines – 1999 Thorax 2000: 55; 210-218 • NICE guidelines – 2006 – Sensitive TB – 4 drugs for 2 months 2 drugs for 4 months – Resistant TB - 6 drugs for 24 months (second line drugs are not so effective) [Eng, Wales & NI 2004, 6.8% Isoniazid resistant, 1% MDR TB (R to Isoniazid and rifampicin)] Problems of TB therapy • • • • Toxicity e.g. liver Multiple therapy Prolonged treatment Drug interactions Compliance – Treatment will not work if not taken – DOTS (Directly Observed Therapy) if: • Likely poor compliance • MDRTB Public health - avoiding transmission • TB is statutorily notifiable disease • Multidisciplinary approach – medical, TB nurses, CCDC etc. • Identify and manage possible sources of infection and contacts • Considerations • • • • treat as OP where possible multi occupancy housing, social deprivation negative pressure rooms in hospitals (limited facility) beware transmission in OP setting e.g. waiting area WHY FAILURE? • Patient non compliance –Deliberate –Failure to understand e.g. language, culture –Social e.g. alcohol • Patient movement e.g. ‘lost to follow up’ • Lack of medical/nursing support • others Summary • TB is a challenging disease for the clinician • Must have microbiology before starting treatment – more rapid lab tests? • Need to encourage compliance • Need for multidisciplinary approach to diagnosis and management and control • Need shorter, better, cheap anti TB regimes SAMPLE MSQs • The starting pathogenesis in TB is; • • • • • Secondary TB Miliary TB Ghon focus CNS involvment GIT involvment • The advanced stage in Potts disease is • • • • • Paresis Lost urinary control Gibbus formation Paraplegia Death • Poor compliance to treatment, TB of any site becomes • • • • • Resistant to treat MDRTB XDRTB MILIARY TB TB ABSCESS