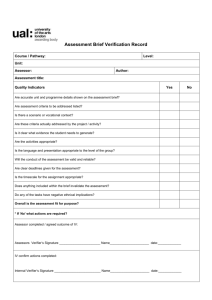
Professional Practice - monitoring maternal & fetal wellbeing
advertisement

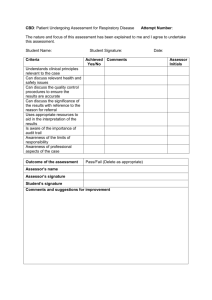
Proficiency: Professional practice – Monitoring maternal and fetal wellbeing Proficiency Outcome as a practising midwife: ‘Prioritising people: You put the interests of people using or needed nursing or midwifery services first. You make their care and safety your main concern and make sure that their dignity is preserved and their needs are recognised, assessed and responded to. You make sure that those receiving care are treated with respect, that their rights are upheld and that any discriminatory attitudes and behaviours towards those receiving care are challenged (NMC 2015) The Code: Professional standards of practice and behaviour for nurses and midwives, page 4. Practise‘ effectively: You assess need and deliver or advise on treatment or give help (including preventative or rehabilitative care) without too much delay and to the best of your abilities, on the basis of the best evidence and best practice. You communicate effectively, keeping clear and accurate records and sharing skills, knowledge and experience where appropriate. You reflect and act on any feedback you receive to improve your practice NMC (2015) page 7 Preserve safety: You make sure that patient and public safety, is protected. You work within the limits of your competence, exercising your professional ‘duty of candour’ and raising concerns immediately whenever you come across situations that put patients or public safety at risk. You take necessary action to deal with any concerns where appropriate NMC (2015) page 11. Midwife at the point of registration - can perform the activity satisfactorily without supervision, assistance and/or guidance; with acceptable speed and quality or work with understanding and appropriate application, identify the problem, relevant information and uncertainties (Competent and able to account for their actions) Refer to: Benner (1984) Assessment Level 3 (Appendix 1 LSA Guidance for Clinical Mentors and Academic assessors supporting a midwife undertaking an LSA practice programme 2013 Page 7) This is linked to: NMC (2015) The Code: Professional standards of practice and behaviour for nurses and midwives. NMC (2009) Pre registration standards for midwifery education, Standard 17, p31 NMC (2011) The PREP handbook NMC(2012) Midwives rules and standards, Rule 5; Scope of practice NMC (2013) Raising concerns: Guidelines for nurses and midwives. AKJuly2105 NB Competencies listed are to be modified or removed in light of the outcomes of the supervisory investigation. Clinical Proficiency Assessment Criteria used is (Benner, P. (1984). From novice to expert, excellence and power in clinical nursing practice. Menlo Park, CA: Addison-Wesley Publishing Company, 307 pp. Evidence Verifier/ signature can be: No Benchmark Statements 1 As a practising midwife is responsible for providing midwifery care to a woman and baby during the antenatal, intra-natal and postnatal periods, you must be able to demonstrate that you are familiar with the necessity to: Promote normal birth Facilitate women’s choice Act as an advocate Verifier signature/designation : AKJuly2105 Lead investigating Supervisor of Midwives, Academic Assessor, Risk/Governance midwife or Sign off mentor 1.1. 1.2 Documented discussion and structured questioning to demonstrate in-depth of physiology of labour and how this may be enhanced during birth. Demonstrate insight by writing a reflective essay which identifies and applies key principles and evidence to promoting normal and normalising complex birth and the outcomes of the supervisory investigation. Evidence of achievement Evidence Verifier/ signature can be: No Benchmark Statements 2 Lead investigating Supervisor of Midwives, Academic Assessor, Risk/Governance midwife or Sign off mentor Date Pass/Fail Assessment of maternal wellbeing, interpreting findings accurately and shares information with women, discussing any further action/consequences as necessary to include: 2.1 Assessment of clinical competence in an area relevant to supervisory investigation recommendations and related identified practice gap. Monitoring maternal well being Follow evidenced based care pathways, justifying any deviations Identification and management of risk Timely action and referral to appropriate professionals. Verifier signature/designation : AKJuly2105 2.2 Documented discussion and structured questioning 2.3 Critically appraise own practice demonstrating insight in reflective essay. 2.4 Attendance at a ‘normal birth’ workshop/MLU clinical practice and relate practice to the relevant physiology to facilitate low risk birth Evidence of achievement Evidence Verifier/ signature can be: No Benchmark Statements 3 Lead investigating Supervisor of Midwives, Academic Assessor, Risk/Governance midwife or Sign off mentor Date Pass/Fail Assessment of fetal wellbeing. 3.1. Assessment of clinical competence in an area relevant to supervisory investigation recommendations. 3.2. Successfully complete CTG training package. 3.3. Complete ‘fresh eyes’ reviews with delivery suite/DAU coordinators and review findings and follow up action. Care for, monitor and support women during labour and monitor the condition of the fetus, supporting spontaneous birth. Participates in monitoring fetal wellbeing using appropriate use of 3.4. Pinard, intermittent auscultation or by technical means. 3.5. Documented discussion and structured questioning Critically appraise own practice demonstrating insight in reflective essay. Recognises deviation from the normal wellbeing of the fetus Take appropriate action in response including appropriate referral Verifier signature/designation : AKJuly2105 Evidence of achievement Evidence Verifier/ signature can be: No Benchmark Statements 4 Lead investigating Supervisor of Midwives, Academic Assessor, Risk/Governance midwife or Sign off mentor Date Pass/Fail Support the creation and maintenance of environments that promote health, safety and wellbeing of women, babies and others, including; 4.4. Undertake mandatory training and apply learning to the identified practice gaps 4.2. Documented discussion and structured questioning in relation to effectively promoting healthy lifestyle choices and ‘Making every contact Count’ http://www.nhslocal.nhs.uk/story/every-contact-counts Prevention and control of infection Promoting health Safety and security in the environment in which they work whether within the home, community, clinic or hospital. Appropriate use of equipment/technology Verifier signature/designation : AKJuly2105 Evidence of achievement Evidence Verifier/ signature can be: No Benchmark Statements 5 Lead investigating Supervisor of Midwives, Academic Assessor, Risk/Governance midwife or Sign off mentor Date Pass/Fail Measure, assess and facilitate wellbeing during antenatal/postnatal periods. 5.1. Assessment of clinical competence in an area relevant to supervisory investigation recommendations. 5.2. Documented discussion and structured questioning 5.3. Critically appraise own practice demonstrating insight in reflective essay with application of relevant physiology and evidenced based guidelines. 5.4. Review with their clinical mentor 5 – 10 sets of their own records demonstrating evidence of justification of actions taken. Follow evidenced based care pathways, justifying any deviations. Assessment and interpretation of progress to include; observation, screening, abdominal, vaginal examinations as required; providing feedback to women. Social needs and assessment vulnerability. Timely referral to appropriate professionals Verifier signature/designation : AKJuly2105 Evidence of achievement Evidence Verifier/ signature can be: No Benchmark Statements 6 Lead investigating Supervisor of Midwives, Academic Assessor, Risk/Governance midwife or Sign off mentor Date Pass/Fail Measure, assess and facilitate the progress of labour. 6.1. Assessment of clinical competence in an area relevant to supervisory investigation recommendations and identified practice gaps. 6.2. Undertake the review of an existing guideline and benchmark against National guidance and if necessary update applying new research findings relevant to the guideline. Critically appraise and justify the use of any intervention, in order to facilitate birth Seeks informed consent prior to undertaking any procedure. Recognises deviation from the normal progress of labour or the well-being of the woman and fetus and discuss any further action/consequences as necessary. Verifier signature/designation : Evidence of achievement AKJuly2105 Evidence Verifier/ signature can be: No Benchmark Statements 7 Lead investigating Supervisor of Midwives, Academic Assessor, Risk/Governance midwife or Sign off mentor Date Pass/Fail Assesses accurately the health and wellbeing of the mother and baby at birth 7.1.Assessment of clinical competence in an area relevant to supervisory investigation recommendations and identified practice gaps Initiates and maintains emergency 7.2.Attend and pass NALS training/update measures if required 7.3.Attend and pass BLS training/update 7.4 Attend and pass Skills/drills training/update Add amend/add as required Verifier signature/designation : AKJuly2105 Evidence of achievement Evidence Verifier/ signature can be: No Benchmark Statements 8 Lead investigating Supervisor of Midwives, Academic Assessor, Risk/Governance midwife or Sign off mentor Date Pass/Fail The midwife must demonstrate accountability by demonstrating on-going development, education and practice experience to maintain registration. 8.1. Identify learning needs through the development of a professional portfolio. 8.2. Discussion regarding PREP/Revalidation requirements. 8.3. Present an individual learning plan to detailing learning needs and SMART goals to plans for how these will be achieved for the next year. Verifier signature/designation : Evidence of achievement Date Pass/Fail If Evidence, for example a study day, or attendance at a particular activity has not yet happened by either the 150 or 300 hour review please enter NYF (Not Yet Facilitated). At each of these reviews, if particular activities have not yet been facilitated , reassurance will be sought that, for example dates, times, venues, etc,, have been arranged to ensure evidence is completed and in place for the final 450 hour end review. At the final 450 hour review, if level 3 is not achieved, reasons for the failure must be clearly evidenced to justify the failure of the supervised practice programme. Named mentor must meet the sign off mentor requirements (NMC (2008) Standards to support learning and assessment in practice) The named supervisor can provide all the information in one document if appropriate. You may use the same five to ten sets of records if they provide all the evidence required You are only expected to prepare one presentation for student midwives ensuring that all areas identified are covered AKJuly2105