MD 803 – Obstetrics and Gynecology LIC Clerkship The
advertisement

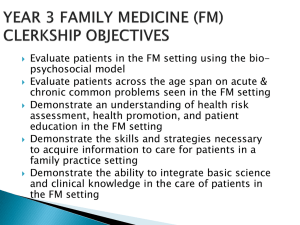
MD 803 – Obstetrics and Gynecology LIC Clerkship The Commonwealth Medical College Academic Year 2012-2013 Approved, Year 3-4 Subcommittee of the CAC: May 30, 2012 Approved (as modified), Curriculum Action Committee: June 4, 2012 Contact Information Education Director: Regional Education Coordinators: Brian D. Wilcox, M.D., Ph.D. Harold Davis, M.D. Scranton Physicians Health Alliance 401 Adams Avenue Scranton, PA, 18503 570-346-7338 570-650-2889 hdavis@tcmedc.org Physicians Health Alliance 748 Quincy Ave, Suite 2A Scranton, PA 18510 570-961-0855 570-309-7569 bwilcox@tcmedc.org Regional Clerkship Directors: 2 Lisa C. Thomas, M.D. Scranton Hematology/Oncology Associates of NEPA 1100 Meade Street Dunmore, PA 18512 570-342-3675 ext. 228 lthomas01@tcmedc.org Joseph P. Narins, M.D. Wilkes-Barre Wyoming Valley Family Practice Residency Program 2 Sharpe Street Kingston, PA 18704 570-552-8954 570-706-5522 jnarins@tcmedc.org Mary Beth Sokach, DO Wilkes-Barre Exeter Twp Medical Center RR 1, Box 301 Falls, PA 18615 570-388-6151 570-947-3680 msokach@tcmedc.org Janice L. Schifferli, DO Williamsport 699 Rural Avenue Williamsport, PA 17701 570-321-2339 570-329-5521 jschifferli@tcmedc.org Margrit Shoemaker, MD Williamsport 1100 Grampian Boulevard Williamsport, PA 17701 570-320-7848 570-419-0149 mshoemaker@tcmedc.org Charles D. Lamade, MD Williamsport Women’s Health Care Associates, PC 777 Rural Avenue, 6th Floor Williamsport, PA 17701 570-323-3671 clamade@tcmedc.org Purpose of the Course Syllabus: This syllabus is a guide for participation in the course; information is subject to change during the presentation of the course. Any changes in the course will be announced during the classroom or clinical sessions and will be noted in the course Blackboard website. Learning Objectives for MD 803: The Learning Objectives of the clerkship are based on the general MD Curriculum Program Objectives that have been established by TCMC. These include: 1. Medical Knowledge: Students must demonstrate understanding of established and evolving biomedical, clinical, epidemiological and social-behavioral sciences, and the application of this knowledge to the care of obstetric and gynecologic patients. Students must demonstrate depth of knowledge about the presentation and management of obstetric and gynecologic illness and evidence-based knowledge that is the foundation of well-woman care. 2. Practice-Based Learning and Improvement: Students must demonstrate an ability to locate, appraise and assimilate scientific evidence for improvement of OB/GYN patient care practices. 3. Interpersonal and Communication Skills: Students must demonstrate interpersonal and communication skills that result in effective information exchange, therapeutic, ethically-sound relationships and collaborative decision-making with patients, their families, and professional colleagues. 4. Patient Care: Students must demonstrate patient care that is compassionate, appropriate, and effective for the treatment of obstetric and gynecologic patients in the context of their families and communities. Students will demonstrate and advocate for appropriate treatment of illness and also the promotion of health maintenance, disease prevention and wellness as it pertains gynecology and obstetrics. 5. Professionalism: Students must demonstrate a commitment to carrying out professional responsibilities, adherence to ethical principles, and sensitivity to contextual issues in a diverse female patient population. This includes demonstration of a commitment to continuous learning, dedication to patient care, respect, compassion and integrity in all activities. 6. Systems-Based Practice: Students must demonstrate an awareness of, and responsiveness to, the larger context and system of health care, as well as the ability to call on other resources in the system to provide optimal health care to obstetric and gynecologic patients and their families. General Clerkship Description / Overview: The Obstetrics and Gynecology 803 clerkship is one of the six core components of the third year longitudinal integrated curriculum (LIC). Students will spend one half day weekly with an OB/GYN clinician in his/her office and will care for a group 3 of patients over the course of the year. Additional inpatient “bursts” and/or inpatient “on-call” experiences will also be scheduled. Students will follow obstetric patients and gynecologic patients. Obstetric patients will be followed through various settings including outpatient prenatal care visits, outpatient consultations, inpatient antepartum care, labor, birth, and postpartum care. Gynecologic patients will be followed through well-woman visits, gynecologic problem visits, emergency room visits, inpatients hospitalizations, preoperative care, surgery, postoperative care and outpatient consultations. Students will all have a TCMC extension/voice mail and are expected to discuss how they can be contacted by the supervising attending on any emerging issues. Students are expected to possess the ability to take an accurate history and physical and formulate an initial differential diagnosis from their clinical experiences in the first and second year courses “Profession of Medicine, ” “Art and Practice of Medicine, ” and “Systems II: Reproduction”. They are also expected to already possess professional attitudes and deportment in a clinical setting, appropriate to the third year student level. Clerkship Outcomes: During the Obstetrics and Gynecology clerkship, third year students will: Acquire basic medical knowledge about normal and abnormal pregnancy, gynecologic illness and wellwoman care. Attain clinical skills, clinical knowledge and professional behaviors required to evaluate and care for the gynecologic and obstetric problems of female patients and the health maintenance of female patients. Gain knowledge of the evaluation, diagnosis and management of obstetric and gynecologic patients encountered in the ambulatory setting, emergency department, operating room, and labor and delivery suite. Obtain the foundation for OB/GYN sub-specialty 4th year clerkships if desired. Clerkship Schedule/Schedule of Learning sessions: Students will be scheduled in an Obstetrics and Gynecology practice/office one half-day per week for the duration of the third year integrated clerkship. They will work on an ongoing basis with a primary supervising attending physician who will coordinate their activities and ensure adequate experience. Experiences with additional OB/GYN providers are anticipated for some students depending on the schedule and practice pattern of the supervising attending. Students will see patients in the office, at scheduled specialty consultations in other offices, and in inpatient settings depending on the needs of the patients. Gynecology experiences will include inpatient and outpatient surgery and appropriate preoperative, hospital and outpatient follow-up care. Obstetric experiences will require the longitudinal follow-up of at least three patients through the entirety of pregnancy, labor and birth, and postpartum. Students are expected to visit any hospitalized patients they are following on one of the two weekend days. In addition, students will attend regularly-scheduled formal didactic conferences during each week. Inpatient and “on-call” Experiences: All students will obtain additional inpatient experiences by participation in “bursts” of inpatient care in the Departments of Obstetrics and Gynecology at participating hospitals. In Scranton and Williamsport, students 4 will be scheduled for two, 5-day inpatient bursts. In Wilkes-Barre, students will perform three, 3-day bursts. Because of variations in patient volume and practice patterns at outlying hospitals, some students may be assigned alternative inpatient experiences under the discretion of the Regional Education Coordinator for OB/GYN. All students should obtain at least 9 days of inpatient experience. Continuity Patients: In the 3rd Year Longitudinal Integrated Clerkship, each student will develop a panel of at least 10 patients per discipline as “continuity patients”. For the Obstetrics and Gynecology Clerkship, this will require at least 5 Obstetric continuity patients and at least 5 Gynecology continuity patients. Students are required to follow these patients as they access the health care system. These patients are to be seen in the inpatient and outpatient setting. They are to be followed through consultations and procedures. Following the cohort of continuity patients is the PRIMARY ROLE of the M3 student. This longitudinal experience with patients and their families is the central learning experience of the LIC. Students, with the assistance of their preceptors, will develop a cohort of patients to follow throughout the year. Students should not have all patients selected in the first few weeks of the year-long clerkship, but they should have their cohort of patients selected no later than December, 2012. The characteristics of a continuity patient will be different depending on the discipline. Here are some general guidelines for the selection of these patients: Internal Medicine: a patient with chronic medical problems or a newly diagnosed problem who will be followed in the office, the hospital, and other locations over the year. Family Medicine: a patient who will be followed-up during the year, and at least one of these patients are to be seen in a home visit. Obstetrics and Gynecology: a patient who will be followed through the course of her pregnancy (and ideally for whom the student will be present for the delivery) or a non-pregnant patient who the student will follow throughout the treatment and follow-up of a gynecologic problem or an operative and peri-operative course. Surgery: a patient who the student will see preoperatively, in the operating room, and postoperatively. Pediatrics: a well patient who the student will see at least more than once during the year or a child with a chronic illness you will follow throughout the year. Psychiatry: a patient who the student will participate in on-going care, including counseling sessions or a patient with a newly diagnosed condition that will be followed throughout the year. Patient Encounter Log: The following patient encounter types and procedure requirements may be filled at any time during your yearlong experience in any clinical setting. The required obstetrics and gynecology patient encounters to be logged are derived from the “APGO Medical Student Objectives, 9th Edition,” 2009, Association of Professors of Gynecology and Obstetrics (APGO). Because this is a Longitudinal Integrated Clerkship in which you work and learn simultaneously in the six core disciplines, the patient encounter types and procedure requirements listed in 5 tables 1,2, and 3 may be filled at any time during your year-long experience in any clinical setting unless otherwise specified in the specific encounter type. Logging encounters is MANDATORY. Student logs are reviewed at 2 weeks, 1 month, 2 months, 3 months, 6 months, 9 months, and 12 months during the Longitudinal Integrated Clerkship. Students MUST complete all required patient encounter types by seeing a patient with that designation in one of the six core disciplines (IM—Internal Medicine, FM—Family Medicine, PED—Pediatrics, SURG—Surgery, OB—Obstetrics and Gynecology, PSY—Psychiatry) or in alternative learning environment (ALT) such as the simulation center, during educational sessions, on-line modules, or other learning methods. Experiences occurring in the Emergency setting are to be logged under the core discipline that is most appropriate. Tables 1,2 and 3 outline the requirements for all six disciplines. ALL encounters must be logged into the One45 system. The table below is a master list of all encounters. The first column is the specific encounter type; the second column is the MINIMAL number of encounters required (remember ALL encounters MUST be logged). Students must participate in at least this number of encounters to pass the clerkship. The next column designated “L” means that these encounters are “logged only” unlike certain procedures and encounter types which require “L/F”, “logging and feedback”. Students must choose (from a drop-down menu in One 45) one of the following seven clerkships or alternative educational experiences appropriate to the encounter. Just as busy clinicians must finish patient records to be in compliance with standards of practice, M3 students are expected to be in compliance with logging. It is recommended that students will log their encounters at least daily to maintain their record. Students who fail to log encounters or who fall behind in logging will be referred to their Regional Clerkship Director (RCD) who may ultimately decide to make a referral to the Committee on Academic and Professional Standards for a breach of professionalism. Required Encounters / Procedures: Table 3 is a summary of encounters/procedures that require faculty feedback. ALL of these encounters are to be logged into One45 and MUST be entered into the Preceptor Feedback Book which you will receive. Students will only receive credit for encounters that are either done under the direction of a faculty member or done under direct observation (the first two columns are for student recordkeeping. EACH encounter/procedure must have a check in either the “done with direction” or “does while observed” column and then certified with the supervising faculty initials in the last column. Certifying faculty may include preceptors, advanced practitioners, residents, nurses, or technicians (depending on the procedure). If an encounter does not have a faculty initial next to it, it will not be counted for credit. ALL encounters/procedures MUST be completed and certified by a faculty member to pass the clerkship. Logging is MANDATORY. Student logs are reviewed at 2 weeks, 1 month, 2 months, 3 months, 6 months, 9 months, and 12 months during the Longitudinal Integrated Clerkship. . It is recommended that students log their encounters at least daily to maintain their record. Students who fail to log encounters or who fall behind in logging will be referred to their Regional Clerkship Director (RCD) who may ultimately decide to make a referral to the Committee on Academic and Professional Standards for a breach of professionalism. Whitespace: An LIC requires initiative on the part of all medical students. While an LIC gives students the most true-to-life experience of patient care, it also demands a high degree of responsibility. Most students feel somewhat 6 disoriented for the first few months; this is expected. Many students express confusion with the concept of whitespace. Some guidelines to how to use this protected educational time are provided below. 1. Whitespace is not vacation or “free-time”. It is time in which you are to follow your patients who are hospitalized, having a procedure, or a consultation. It is time to make a home visit. It is time to make rounds on patients. The first use of whitespace is to follow your patients. 2. The second use of whitespace is to fulfill the requirements of the clerkship. It is a time to seek out encounters or procedures that are required. This does not need to be done during the first two months. The LIC is not a race to complete encounter charts, but it is a method to learn the practice of medicine over time. In fact, students will experience better educational outcomes if required encounters are completed over time. 3. Whitespace CAN be used to pursue areas of interest, however, it is not just to be used observing procedures or being a “fly on the wall”. Students should seek out active learning opportunities whenever possible. 4. Whitespace CAN be used to read, study, or attend local educational sessions. This is probably the least effective use of time. While students must set up a reading and study schedule, this is better done during evenings and weekends. Clinical Education Days (CED): 1. On Friday afternoons from 1:00 to 4:30 PM students are REQUIRED to participate in a Clinical Education Day (CED). This is held at the regional campus and is sponsored by the Year 3 educational team. Please refer to the schedule posted on the portal. 2. Attendance is MANDATORY. Students may have no more than 2 unexcused absences during the year. This is to maximize the learning experience for each student. Students missing any activity for any reason must report this to the appropriate faculty and their Regional Educational Specialist (REC). 3. Any student having more than 2 unexcused absences during the year will be referred to the Committee on Academic and Professional Standards (CAPS) by his/her Regional Clerkship Director. Inpatient Experiences for the third year: “Bursts” and Emergency Medicine Shifts: 1. There will be seven one-week experiences during the third year in which students are relieved of duties in the ambulatory setting and work in inpatient settings. The purpose of these “bursts” is for students to gain a deeper understanding of the fields of inpatient medicine, surgery, anesthesia, and obstetrics and 7 2. 3. 4. 5. 6. gynecology. These bursts serve as the foundation of sub-internships in the fourth year and allow exposure to the field of anesthesiology. Inpatient Medicine x 2 weeks Inpatient Surgery x 2 weeks Anesthesia x 1 week Obstetrics/Gynecologic Surgery x 2 weeks Students are assigned to16 “shifts” in the emergency department during the year. Learning Objectives for INPATIENT BURSTS in Obstetrics and Gynecology: 1. Students will understand the process of normal labor and delivery. They will obtain the medical knowledge to provide optimal care and reassurance for the woman in normal labor and the timely recognition and treatment of abnormal events. This includes, but is not limited to: a) Understanding the signs and symptoms of true and false labor b) Performing the initial assessment of the laboring patient c) Performing and documenting an adequate admission history and physical d) Understanding the stages of labor and recognizing common labor abnormalities e) Understanding approaches to pain management in labor f) Understanding the methods of monitoring of the mother and fetus g) Performing, with supervision, normal vaginal delivery h) Observing operative vaginal delivery and understanding the indications i) Observing cesarean section and understanding its indications, risks and recovery 2. Students will demonstrate knowledge of, and the provision of normal postpartum care, reassurance of the normal postpartum patient, and recognition of abnormal events. This includes but is not limited to: a) Understanding the normal maternal physiologic changes of the postpartum period b) The components of normal postpartum care including postpartum rounds and care notes c) Understanding and providing appropriate postpartum patient counseling 3. Students will understand and demonstrate knowledge of medical and surgical conditions that may alter the course of pregnancy, labor and delivery and the postpartum period. This includes an understanding of the diagnosis, evaluation, and management of the following conditions: a) Ectopic pregnancy b) Spontaneous abortion c) Medical and surgical comorbidities and their affect on pregnancy d) Medical and surgical comorbidities and the effect of pregnancy on these conditions e) Preeclampsia-eclampsia f) Alloimmunization g) Multi-fetal gestation h) Fetal death i) Abnormal labor j) Third trimester bleeding k) Preterm labor l) Preterm rupture of membranes m) Postpartum hemorrhage n) Postpartum infection o) Postpartum depression and anxiety p) Post term pregnancy q) Fetal growth abnormalities 8 4. Students will demonstrate knowledge of obstetric procedures basic to the management and counseling of the pregnant patient. This includes but is not limited to: a) Preoperative evaluation, planning, history, physical exam and informed consent b) Measures for the prevention of infection, deep venous thrombosis and other perioperative complications c) Essential components of postoperative care d) Common postoperative complications e) Communication of operative findings to the patient and family f) Understanding indications, mechanisms and possible complications of obstetric procedures including: i. Ultrasound ii. Amniocentesis iii. Intrapartum fetal surveillance iv. Induction and augmentation of labor v. Vaginal birth after cesarean delivery vi. Breech delivery vii. Cesarean delivery viii. Postpartum tubal ligation ix. Newborn circumcision 5. The student will demonstrate knowledge of the evaluation and management of gynecologic problems that frequently require diagnostic and therapeutic surgical procedures. This includes but is not limited to: 1. Preoperative evaluation, planning, history, physical examination and informed consent 2. Common measures for the prevention of surgical infections, deep venous thrombosis and other perioperative complications 3. Essential components of post operative care 4. Common postoperative complications and management 5. Effective communication of operative findings and complications to the patient and family 6. Understanding common outpatient and inpatient gynecologic surgical procedures, their indications and possible complications including: i. Foley catheter insertion ii. Electrosurgical excision of the cervix iii. Dilation and curettage iv. Hysteroscopy v. Gynecologic laparoscopy vi. Tubal sterilization vii. Hysterectomy and bilateral salpingo-oophorectomy Reading List: There is an integrated reading list as part of the Clinical Education Day schedule on the portal. There are assignments directly related to the material covered that day as well as a list to round out the reading list for the year. Core weeks: Attendance at ALL activities during core weeks is MANDATORY. Any student with an unexcused absence will be referred to the Committee for Academic and Professional Standards (CAPS). Students with excused absences 9 are REQUIRED to make-up any material missed during their absence. The core weeks for the 2012-2013 academic year are: 1. Monday, October 22, 2012 to Friday, October 26 2. Monday, April 1, 2013 to Friday, April 5, 2013 3. Monday, June 17, 2013 to Friday, June 21, 2013 Required / Recommended Texts Title Link to Resource Required : Obstetrics and Gynecology, 6th edition, (2010) Charles RB Beckmann, Frank W Ling, et.al. (Wolters / Lippicott /ACOG) http://www.amazon.com/Obstetrics-GynecologyBeckman/dp/0781788072/ref=sr_1_5? Case Files: Obstetrics and Gynecology, 2nd edition (2006)Eugene Toy, Benton Baker III, et.al. (Lange) http://www.netlibrary.com.ezproxy.tcmedc.net/ListContent. aspx?cc=Ebook Recommended / Optional Learning Materials: Blueprints: Obstetrics and Gynecology (2008)Tamara L Callahan, Aaron B Caughey. (Blackwell) Obstetrics, Gynecology and Infertility: Handbook for Clinicians, 6th edition John D Gordon, Jan Rydfors, et.al., (Scrub Hill Press) Managing Contraception: (2010-2012) Mimi Zieman, Robert A Hatcher, et.al., Obstetrics and Gynecology Recall (2007) F John Bourgeois, Megan J Bray, Catherine H Matthews (Wolters / Lippincott) Blackboard Site: OR http://www.amazon.com/Case-Files-Obstetrics-EugeneToy/dp/0071402845/ref=sr_1_19? http://www.amazon.com/Blueprints-Obstetrics-GynecologyTamarahttp://www.amazon.com/Obstetrics-Gynecology-InfertilityHandbookClinicians/dp/0964546779/ref=ntt_at_ep_dpi_1#_ http://www.amazon.com/Managing-Contraception-20072009-MimiZieman/dp/0979439507/ref=sr_1_1?s=books&ie=UTF8&qi d=1280183138&sr=1-1 http://www.amazon.com/Obstetrics-Gynecology-RecallJohnBourgeois/dp/0781770696/ref=sr_1_1?s=books&ie=UTF8 &qid=1280183392&sr=1-1 http://my.tcmedc.net/ Agencies used in this clerkship include, but are not limited to: 1. Local health departments 2. Social service agencies 3. Area agencies 10 4. Indigent care clinics 5. Visiting nurse organizations 6. Hospice organizations Teaching & Learning Methods to be used in this course: 1. Direct Patient Care under Supervision – Students will work in clinical settings closely supervised by attending faculty. Attendance at these sessions is MANDATORY. Any student with more than 2 unexcused absences will be referred to the Committee for Academic and Professional Standards (CAPS). 2 Interprofessional Learning: Students will function in clinical settings as a part of an interdisciplinary team, including physicians, nurses, office staff, cross-disciplinary hospital staff, and staff at community agencies. 3. Case-Based Learning: Students will participate in conferences where OB/GYN topics are covered in a case-based format. 4. Independent Learning: Students are allocated time during the schedule for independent learning focused on patient encounters. This includes uWISE (Undergraduate, Web-based, Interactive Self-Assessment, www.APGO.org) assignments as alternative learning for less-common patient encounter types. Required Clerkship Assignments: Student Led Tutorial: Each student will lead two tutorial sessions. Topics will be assigned at the beginning of the year. Course Evaluation: Thoughtful student feedback is vital to assuring a high quality curriculum and educational experience. All students will be given an opportunity to provide constructive feedback to the clerkship coordinators, Regional Campus Dean(s), and Clerkship Director(s) for the Obstetrics and Gynecology clerkship. Numerical ratings by all students will be solicited at the end of the course through the Office of Evaluation & Assessment using the student feedback evaluation form specifically designed for the TCMC Obstetrics and Gynecology Clerkship. Medical Knowledge Competency and Course Narratives: Medical Knowledge competency is assessed at multiple points in the MD Curriculum based upon students’ performance on graded items defined in each course (such as examinations, practicals, standardized patients, etc.). Unsatisfactory and satisfactory performance is determined based on the pass mark established at 70%. The course narrative is prepared by the clerkship grading committee. The Education Director for the discipline and the Regional Education Coordinators comprise this committee. This qualitative and quantitiative assessment of the student’s progress toward Professional competency will be maintained as part of the student’s academic record and will be sent to each student for review after the clerkship is completed. Students who have recurring difficulties in Medical Knowledge or professionalism competencies will be referred to the Office of Academic Affairs and/or CAPS for progress review. This referral can occur at any time in any 11 course in the first 2 years of the program (MS1 and MS2) or during the clinical years (MS3 and MS4). Issues in professionalism during the clinical years are usually addressed by the appropriate Regional Clerkship Director Evaluation Methods: Learner Evaluation: Each student will receive a 60-day, a mid-clerkship, and final evaluation from the Regional Education Coordinator. The final grade will be based on the College’s Standards and Procedures for the Evaluation of Students and will utilize evaluations from the student’s faculty supervisor, and the Obstetrics and Gynecology faculty leading case conferences and didactic activities. Students will complete the NBME Shelf examinations during the last third of the rotation. In addition to the formulation of specific grades, narrative evaluations will be prepared by the Regional Education Coordinator and the Education Director for Obstetrics and Gynecology and provided to the Office of the Registrar, the student’s advisor, and reviewed by the Committee on Academic and Professional Standards (CAPS). Final clerkship grades are assigned by the discipline-specific Grading Committee. NBME Practice Examinations: All students will take two NBME practice examinations. The Clinical Science Exam will cover all of the six core disciplines. Students will also choose a subject-specific exam to take. The results of these examinations will be reviewed by the Year 3 educational team. Friday, December 14, 2012: Clinical Science Exam Friday, February 1, 2013: Student-Selected Subject Exam NBME Shelf Exam Dates for the 2012-2013 Academic Year: As outlined above, the results of the NBME shelf exams are a component of the student’s final grade for a specific clerkship. The dates for the exams for the 2012-2013 academic year are as follows: Wednesday, May 15, 2013: Family Medicine and Pediatrics Thursday, May 30,2013: Surgery and Psychiatry Friday, June 14, 2013: Internal Medicine and OB/GYN To be announced: Make-up exam date Students may only use the make-up exam date for an excused absence. Students may miss no more than two scheduled exams, and may take no more than two shelf exams on a single day. Grading: All clerkship grades are determined by the discipline-specific grading committee. The Education Director and the Regional Education Coordinators from each region comprise the committee. The committee will review all of the materials that pertain to the specific clerkship and assign a specific grade. 12 Clerkship grades may be Honors (H), Satisfactory (S), or Unsatisfactory (U). Honors will be given to those students performing in the top 15%. Grades will be determined in the following manner: Clinical Preceptor Evaluation – 40% Performance in Case Conferences, Tutorials, Reflection and Inpatient Bursts – 20% Performance on NBME “Shelf” Exam – 20% Performance on OSCE’s-20% (done during the call back weeks) A SATISFACTORY grade requires that students have a passing score on the NBME exam which is defined as a score greater than two standard deviations below the national mean for the prior year. It also requires a mean score of “4” or more on their faculty evaluation. Passing OSCE and TBL scores are also required. Students MUST complete all of their clinical encounters/procedures as outlined. Any student not meeting these requirements will receive the grade of UNSATISFACTORY. A clinical preceptor may recommend a student for the grade of INCOMPLETE based on his/her assessment of the student’s performance over the year. Students receiving a grade of UNSATISFACTORY or INCOMPLETE will be notified by the Education Director for the clerkship and the student will be referred to the Committee on Academic and Professional Standards (CAPS). For clerkships with inpatient burst experiences, the grading committee will solicit feedback from the faculty involved in the burst(s) and will take this into account when assigning a final clerkship grade. The grading committee may choose to contact clinical preceptors to discuss a student’s performance over the year. The committee may use this information to help in the assignment of a final clerkship grade. The individual clinical preceptor may recommend a student for honors, but only the grading committee may assign a grade of HONORS. An HONORS grade will be given to the top 15% of students in that discipline for that year. Students will be considered as a class and not by region for this distinction. The rationale for the top 15% of students receiving honors is to identify those students who have truly excelled in a specific discipline. The grading schema for clinical clerkships is included in the TCMC Medical Student Performance Evaluation (MSPE) letter sent to residency programs. The grading committee will also finalize the clerkship narrative which will be included in the MSPE. Work Hour Policy: TCMC agrees with the AMA-MSS statement on medical student work hours, and believes that periods of rest optimize learning. In keeping with the ACGME work hour restrictions for residents, TCMC’s policy is as follows: TCMC does not permit students to work greater than 80 hours in a week. Call periods are limited to 16 hours. 13 Call is limited to no more than once every three nights. Duty free periods between on-call should be at least 8 hours long. Students should have at least 24 consecutive hours free of all assigned duty every seven days. The on-duty time medical students spend delivering patient care services of marginal or no educational value should be minimized. Students will submit a monthly “hours on duty” form to their Regional Educational Specialist. Absences: There are no unexcused absences during the 3rd year. Students may take up to 7 days in excused absence time (if a student is ill, he or she must obtain a written clearance from a health-care provider to return to clinical duties). All absences must be reported to the Regional Educational Specialist and it is the student’s responsibility to inform clinical preceptors of this time and to use whitespace as make-up time. Any student failing to notify his/her clinical preceptor AND Regional Educational Specialist of an absence will be considered in breach of professionalism, and will be referred to his/her Regional Clerkship Director and ultimately to the Committee for Professional and Academic Standards (CAPS). Any other time off requested during the third year is covered by the College’s Leave of Absence Policy. Educational Conference Time: TCMC encourages 3rd and 4th year students to attend and participate in educational conferences of medical and scientific organizations and societies. Attendance at these meetings should follow the guidelines listed below: 1. Students may be absent from 3rd or 4th year clinical/educational responsibilities for a maximum of 3 days during each academic year. 2. Any absence greater than 3 days will be used against the student’s 1 week of personal time. 3. Students must apply to the Office of Academic Affairs, in writing, 30 days prior to the meeting. This is required even if the student is not seeking funds to attend the meeting. 4. The Education Director for the discipline must approve of the absence. 5. Students must inform all preceptors and arrange for any makeup time at the discretion of the preceptor. 6. Students must prepare a brief (10-15 minute) oral presentation and present at the next Friday CED session (between 1-1:30 PM) reviewing important topics learned at the meeting/conference. If the student is presenting data at the conference, it is desirable that the oral presentation focus on feedback received or new ideas learned regarding the research. 7. The TCMC Office of Academic Affairs has limited funds to defray the costs of attending such meetings. Priority is given to students presenting data or co-authoring presentations. See the policy on Scholarships to Attend Professional meetings. Faculty Roles and Responsibilities: 14 Education Director – The Education Director (ED) is ultimately responsible for all content and activities associated with the clerkship, including establishing the educational goals for the clerkship, organizing clinical and didactic activities, and ensuring that these activities meet stated goals. The ED works in conjunction with Clinical Chairs, Regional Deans, Regional Clerkship Directors, Regional Education Coordinators, and Clinical Faculty to develop and deliver the educational content of the clerkship. In addition, the ED works to ensure comparability for the clerkship at all sites and has responsibility for ongoing review and revision of the clerkship experience. The ED serves as the chair of his/her respective grading committee and works with the Regional Education Coordinators in assigning student grades for the clerkship. Regional Education Coordinator: The Regional Education Coordinator (REC) is responsible for the coordination of all local activities at his/her respective clinical regional campus, including the implementation of the curricular goals and ensuring that all activities are fulfilling these goals. The REC is responsible for the recruitment and evaluation of faculty in the region for the clerkship. The REC serves as a primary regional contact for students in a specific clerkship. All RECs serve as members of their respective grading committees. Regional Clerkship Director: The Regional Clerkship Director (RCD) works with the Regional Dean and Education Directors to ensure that all clinical activities in the region are functioning in a coordinated fashion. This individual is responsible for working with Regional Education Coordinators across the disciplines to ensure that each student fulfills educational goals. The RCD serves as a primary contact for students assigned to a specific region. The RCD mentors and motivates students, monitors their progress, and assists students requiring remediation or counseling. The RCD has no role in assigning grades for any clerkship, but may intervene in global student performance issues such as in the domain of professionalism. Regional Education Specialist: The Regional Education Specialist (RES) is the primary, initial point of contact for students to clarify scheduling issues, or address educational or logistical concerns. In addition, the RES will interface with the individual disciplines to help ensure that objectives are being met, and in addition, will act as an interface for Student Affairs functions. The RES, with the assistance of the Regional Campus Manager, will produce schedules for each student’s activities. Clinical Preceptor: The faculty for the clerkship will work with the student on a daily basis to collaborate with the student in the care of the students’ patients. The faculty is the initial point of contact for the students, and is responsible for reporting any issues a student may be having with meeting the learning objectives to the Regional Clerkship Director. The faculty is responsible for ensuring a welcoming and supportive learning environment for the student, identifying gaps the students may have, and helping to direct the student towards resources for self-directed learning to fill these gaps. He/she is also responsible for setting the highest example of professionalism and life-long learning for TCMC students. Students: The student is responsible for attending all clinical sessions and didactic learning experiences as part of the rotation as well as completing self-directed learning experiences and activities. The student is responsible for notifying both the RES and the supervising attending if illness or a personal emergency prevents attendance. Attendance at didactics and conferences is mandatory. Clerkship/Faculty Evaluation: Thoughtful student feedback is vital to assuring a high quality curriculum and educational experience. All students will be given an opportunity to provide constructive feedback to the clerkship coordinators, Regional 15 Campus Dean(s), and Clerkship Director(s) for the Family Medicine clerkship. Numerical ratings by all students will be solicited at the end of the course through the Office of Evaluation & Assessment using the student feedback evaluation form specifically designed for the TCMC OB/GYN Clerkship. Attendance Policy: Students will be accountable and personably responsible for attending all clerkship activities. Attendance is MANDATORY for all clerkship related activities (as outlined in the previous pages), Portfolio assignments, and presentation delivered at the conclusion of the clerkship. Excused absence from scheduled learning activity requires prior notification and approval of the agency clerkship coordinator and the Regional Campus Dean and should be requested only for extenuating circumstances. Absences because of illness or family emergency will be addressed on an individual basis by the Regional Campus Dean or Clerkship Director. Unexcused absences from any clerkship activity will be reported to the Regional Campus Dean’s office where attendance records will be maintained for review and appropriate action. Attendance at all clinical and educational sessions is required. The only exception to this is if there are conflicting patient care learning opportunities; in this case the student must prioritize the conflict and report in to the affected faculty member. Punctuality is of extreme importance; appearing late to clinical experiences and/or conferences is not acceptable and will affect the students’ grade. Dress Code: Attire should not detract from the educational atmosphere. Students are expected to dress professionally to show respect to yourself and others. This includes patient encounters in the hospital or clinic. Neat, clean and professional attire and a name tag are minimal requirements. Avoid dress or attire that could be potentially offensive to the public, your peers, patients, and faculty. General Standards: TCMC ID badges are worn at all times. Good personal hygiene is to be maintained at all times. This includes regular bathing, use of deodorants/antiperspirants, and regular dental hygiene. Scrubs may not be worn in ambulatory settings. They should only be worn in the Emergency Room and Operating Room. Check with your course or Clinical supervisor to learn of any other dress code requirements when you begin each rotation. Confidentiality: Students are required to maintain standards of confidentiality in accordance with HIPAA. Patient Care Responsibility: In order to enhance educational outcomes, it is important that students ‘take ownership’ of their patients. This means that students should feel that their contributions as a member of the health care team are meaningful and important. Students should communicate frequently with their faculty preceptors and the patients they are following; students should of course not be making medical decisions independently without guidance and 16 approval of faculty, but at this same time should see themselves as important contributors and completely engaged as a member of the team. This will necessitate regular communication with the office and physician; preferred modes of communication should be established at the outset of the year. Students should adhere to important ethical guidelines on the care of patients, including boundary setting and the avoidance of inappropriate relationships with patients. Remediation Policy for Students Who Fail a Course or Clerkship: If a student fails a clerkship, that student will be contacted by the appropriate Education Director prior to the posting of grades to be informed of the need to remediate. The Education Director will refer the student to the Senior Associate Dean for Academic Affairs, the Committee for Academic and Professional Standards (CAPS), and the Center for Learning Excellence (CLE). The Education Director will notify the student in writing of these referrals. The Education Director will notify the student in writing of these referrals. If the student is determined to be eligible for remediation by CAPS, the Education Director will determine the appropriate remediation and set the timeline for this remediation. Social Justice Statement: The Commonwealth Medical College is committed to social justice. The course director concurs with that commitment and expects to foster a nurturing learning environment based upon open communication, mutual respect, and non-discrimination. Our College does not discriminate on the basis of race, sex, age, disability, veteran status, religion, sexual orientation, color or national origin. Any suggestions as to how to further such a positive and open environment in this class will be appreciated and given serious consideration. Disability Support Services: If you are a person with a disability and anticipate needing any type of accommodation in order to participate in this class, please advise the course director and The Director of the Center for Learning Excellence prior to the commencement of the course. The Center for Learning Excellence coordinates all disability services and requires three days notification in order to proctor and provide all testing accommodations. Failure to notify the course director and Center for Learning Excellence 1 week before an exam that you will need accommodation for your disability implies acceptance of conditions for that examination. Code of Conduct and Professional Behavior: All activities in this course are conducted under The Commonwealth Medical College Student Code of Academic and Professional Integrity for the MD Degree Program. You signed and received a copy of this Student Code when you enrolled at The Commonwealth Medical College. The full policy is in the Student Handbook. The college, which includes the faculty and staff, expect students to behave appropriately and to fulfill their academic and professional responsibilities. Table 1: Continuity Patient Panels (Logging and Preceptor Certification) REQUIRED CONTINUITY PATIENTS Continuity Patient 1 -- Internal Medicine Description/Diagnoses Date of Initial Encounter Patient Initials Faculty Initials 17 Continuity Patient 2 -- Internal Medicine Continuity Patient 3 -- Internal Medicine Continuity Patient 4 -- Internal Medicine Continuity Patient 5 -- Internal Medicine Continuity Patient 6 -- Internal Medicine Continuity Patient 7 -- Internal Medicine Continuity Patient 8 -- Internal Medicine Continuity Patient 9 -- Internal Medicine Continuity Patient 10 -- Internal Medicine OTHER Continuity Patient(s) -- Internal Medicine Continuity Patient 1 -- Family Medicine Continuity Patient 2 -- Family Medicine Continuity Patient 3 -- Family Medicine Continuity Patient 4 -- Family Medicine Continuity Patient 5 -- Family Medicine Continuity Patient 6 -- Family Medicine Continuity Patient 7 -- Family Medicine Continuity Patient 8 -- Family Medicine Continuity Patient 9 -- Family Medicine Continuity Patient 10 -- Family Medicine OTHER Continuity Patient(s) -- Family Medicine Continuity Patient 1 -- Pediatrics Continuity Patient 2 -- Pediatrics Continuity Patient 3 -- Pediatrics Continuity Patient 4 -- Pediatrics Continuity Patient 5 -- Pediatrics Continuity Patient 6 -- Pediatrics Continuity Patient 7 -- Pediatrics Continuity Patient 8 -- Pediatrics Continuity Patient 9 -- Pediatrics Continuity Patient 10 -- Pediatrics OTHER Continuity Patient(s) -- Pediatrics Continuity Patient 1 -- Surgery Continuity Patient 2 -- Surgery Continuity Patient 3 -- Surgery Continuity Patient 4 -- Surgery Continuity Patient 5 -- Surgery Continuity Patient 6 -- Surgery Continuity Patient 7 -- Surgery Continuity Patient 8 -- Surgery Continuity Patient 9 -- Surgery 18 Continuity Patient 10 -- Surgery OTHER Continuity Patient(s) -- Surgery Continuity Patient 1 -- OB/GYN Continuity Patient 2 -- OB/GYN Continuity Patient 3 -- OB/GYN Continuity Patient 4 -- OB/GYN Continuity Patient 5 -- OB/GYN Continuity Patient 6 -- OB/GYN Continuity Patient 7 -- OB/GYN Continuity Patient 8 -- OB/GYN Continuity Patient 9 -- OB/GYN Continuity Patient 10 -- OB/GYN OTHER Continuity Patient(s) -- OB/GYN Continuity Patient 1 -- Psychiatry Continuity Patient 2 -- Psychiatry Continuity Patient 3 -- Psychiatry Continuity Patient 4 -- Psychiatry Continuity Patient 5 -- Psychiatry Continuity Patient 6 -- Psychiatry Continuity Patient 7 -- Psychiatry Continuity Patient 8 -- Psychiatry Continuity Patient 9 -- Psychiatry Continuity Patient 10 -- Psychiatry OTHER Continuity Patient(s) -- Psychiatry Table 2: Required Patient Encounters (Logging only) Longitudinal Integrated Clerkship Requirements REQUIRED PATIENT TYPES Abdominal Aortic Aneurysm Abdominal Pain Abnormal labor Abnormal Pap Smear Abnormal uterine bleeding Abrasion Acute injury -- in a child Acute Kidney Injury Adenexal mass/cyst Alloimmunization during pregnancy Amenorrhea 1 3 1 2 2 1 1 1 1 1 1 log IM FM PED SURG OB PSY ALT L L L L L L L L L L L 19 Anemia Anorectal disease Anxiety disorder Appendicitis -- acute Arrythmia Asthma -- in a child Autism screening Back pain -- acute Behavioral disorder Biliary disease Bipolar disorder Bleeding Disorder Bowel incontinence Bowel obstruction Breast Mass Breast Pain CABG -- patient management Cancer Diagnosis Cerumen impaction Chest pain Child sexual abuse Chromosomal abnormality Chronic back pain Chronic Kidney Disease Colorectal cancer Colposcopy -- observe Congestive Heart Failure Conjunctivitis Contraception counseling COPD Cough evaluation Dehydration -- in a child Delirium Dementia Dental disease Dental review -- in a child Depression -- follow-up Depression -- geriatric patient Depression -- initial diagnosis Developmental delay Diabetes Diabetes -- initial diagnosis Diabetes and pregnancy Diabetes mellitus -- in a child 20 2 1 1 1 3 2 2 2 1 4 2 1 2 2 3 1 2 1 1 3 1 1 3 1 2 1 5 1 2 2 3 1 2 3 3 2 2 1 2 1 2 3 1 1 L L L L L L L L L L L L L L L L L L L L L L L L L L L L L L L L L L L L L L L L L L L L Diabetic foot ulcer Diarrhea Diet/Exercise counseling Digestive Malignancy Diverticular disease Dizziness Dysmenorrhea Dyspnea Evaluation Ear pain -- in a child Eating disorder Ectopic Pregnancy Edema -- lower extremity Electrolyte abnormality -- in a child Endometriosis Eye problem Failure to thrive -- in a child Fall risk evaluation Family and Social Support Discussion Fatigue Fetal Death Fetal Growth Abnormalities Fever Evaluation -- in a child Fever Evaluation -- in an adult Fibroids First Trimester Bleeding Fracture or dislocation Gastroenteritis -- in a child GERD GERD -- surgical evaluation Geriatric patient in community Geriatric patient in long-term care Gestational Trophoblastic disease GI bleed -- upper Grief Growth abnormality -- in a child Gynecologic Malignancies Headache -- in a child Headache -- in an adult Hearing screening -- in a child Hernia HIV/AIDS Hospice patient Hyperlipidemia Hyperlipidemia -- initial diagnosis 1 3 2 2 1 3 1 3 2 1 1 3 1 1 2 1 2 2 3 1 1 3 3 1 1 3 2 3 1 1 1 1 2 1 1 1 2 3 2 3 1 3 1 3 L L L L L L L L L L L L L L L L L L L L L L L L L L L L L L L L L L L L L L L L L L L L 21 Hypertension Hypertension -- initial diagnosis Immunizations Infection, peripartum Infertility patient Injury prevention -- in a child Intimate Partner Violence Screening Ischemic heart disease Kidney stones Labor, normal Lacerations Lactation Consult, observation Lead Exposure -- in a child Leg pain -- in a child Liver Disease Lung Mass Menopause/Perimenopause Multifetal gestation Multiple chronic illnesses Neck mass evaluation Neck pain -- acute New diagnosis -- adult patients Nutrition Obesity -- in a child Obesity -- in an adult Obstructive uropathy Osteoarthritis Osteoporosis 1 3 10 1 1 2 5 2 1 3 1 1 2 1 1 1 2 1 3 1 2 3 2 2 3 1 1 2 L L L L L L L L L L L L L L L L L L L L L L L L L L L L Panic disorder Pelvic floor dysfunction/prolapse Pelvic pain, acute Pelvic pain, chronic Peripheral vascular disease Pneumonia Pospartum depression Postmenopausal bleeding Postpartum care -- routine Postpartum hemorrhage Postterm Pregnancy Preconception care Pre-eclampsia/eclampsia Pregnancy -- advanced maternal age Pregnancy -- First trimester care Pregnancy -- Second trimester care 1 1 2 2 1 1 1 1 3 1 1 1 1 2 2 2 L L L L L L L L L L L L L L L L 22 Pregnancy -- Third Trimester care Pregnancy termination Premature infant Premature rupture of membranes (PROM) Premenstrual Syndrome/PMDD Preterm labor (PTL) Prostate disease -- surgical evaluation Psychosis, acute Rash -- in a child Rash -- in an adult Rheumatoid Arthritis Salivary gland malignancy Schizophrenia Seizure Disorder Seizure disorder -- in a child Severely disabled child Sexual Assault Sexually Transmitted Infection Sore throat -- in a child Spontaneous abortion Sterlization counseling Stroke, acute Substance use/dependence Suicide attempt, acute Teen Pregnancy Third trimester bleeding Thyroid disorder Thyroid disorder -- in a child Traumatic injury -- management Tuberculosis screening Upper respiratory tract infection Urinalysis interpretation Urinary incontinence -- female Urinary incontinence -- male Urinary tract infection Vaginal discharge Vertigo Vision screening -- in a child Vomiting Vulvar disease OTHER ENCOUNTERS 2 1 2 1 1 1 1 2 2 3 1 1 2 1 1 1 1 3 2 1 2 1 2 1 1 1 1 1 1 2 2 3 1 2 1 3 1 2 3 1 L L L L L L L L L L L L L L L L L L L L L L L L L L L L L L L L L L L L L L L L 23 Table 3: Required Encounters and Procedures (Logging and Preceptor Feedback) REQUIRED ENCOUNTERS/PROCEDURES -feedback Annual, well woman exam -- gynecology Arterial Blood Gas Sampling Breast examination Cervical Culture Cesarean Section Observation Delivery Note Disability Evaluation EKG Interpretation Fern and Nitrazine test Foley catheter insert -- female Foley catheter insert -- male Follow-up Acute Problem - adult/pediatric patient Follow-up Chronic Care -- adult patients Gynecology Operative Note Gynecology Preoperative Note Gyneology Postoperative Progress Note History and Physical -- Gynecology (complete) History and Physical -- Obstetrics (complete) History and Physical -- Psychiatry (complete) History and Physical Inpatient -- Adult (complete) History and Physical Inpatient -- Peds (complete) History and Physicial -- Adult Outpatient (focused) History and Physicial -- Surgical Eval (complete) Home Visit Hospital discharge -- of a child Hospital discharge -- of an adult Hysterectomy Observation IV catheter (peripheral) insertion Labor -- cervical check for dilation Laparoscopic Gynecologic Surgery Observation Nasogastric tube placement Nutrition Evaluation (surgery patient) Operative Vaginal Delivery Observation Pelvic examination (speculum and bimanual) Phlebotomy (diagnostic, peripheral) Postpartum note -- operative delivery Postpartum note -- vaginal delivery Rectal Examination School physical 24 obs only 6 2 1 1 1 3 2 5 1 1 1 10 15 2 1 2 6 6 3 6 6 10 6 2 1 5 1 6 1 1 2 1 1 6 6 1 1 3 2 L/F L/F L/F L/F L/F L/F L/F L/F L/F L/F L/F L/F L/F L/F L/F L/F L/F L/F L/F L/F L/F L/F L/F L/F L/F L/F L/F L/F L/F L/F L/F L/F L/F L/F L/F L/F L/F L/F L/F understand/explain done w/direction does while observed Faculty Initials Screening -- breast cancer Screening -- cervical cancer Screening -- colon cancer Screening -- intimate partner violence Screening -- prostate Skin excision Sports physical Suturing (simple) Suturing of vagina/perineal lac post vag delivery Tubal ligation -- observe Vaginal delivery with supervision Vaginitis exam with KOH and wet prep Well adult visit -- female Well adult visit -- male Well child visit -- 10-20 years Well child visit -- 1-4 years Well child visit -- 5-10 years Well child visit -- birth to 1 year OTHER PROCEDURES 6 3 3 3 3 3 3 3 3 3 3 3 3 3 3 3 3 3 L/F L/F L/F L/F L/F L/F L/F L/F L/F L/F L/F L/F L/F L/F L/F L/F L/F L/F L/F 25 Program Outcomes The Commonwealth Medical College (TCMC) will educate aspiring physicians and scientists to serve society using a community based, patient centered, interprofessional and evidence based model of education that is committed to inclusion, promotes discovery and utilizes innovative techniques. Competency & Student Learning Objectives and Examples of Outcome Measures: The following are the general MD Curriculum Program Outcomes that have been organized by competency domain established by TCMC and addressed in this course: Students will develop basic knowledge of the pathophysiology, presentation, and treatment of commonly encountered obstetric and gynecologic illnesses, prenatal care and well-woman care. The observable student learning performance of knowledge, skills and behaviors achieved by the end of the course are as follows: Clerkship Objectives General Objectives Medical Knowledge Knowledge & Skills Objectives Demonstration of the ability to apply a comprehensive basic science knowledge foundation to clinical medicine. Demonstrates an investigatory and analytic approach to patient care practices. Demonstrates good analytic skills and sound judgment when making medical decisions Obtain the necessary clinical skills to address health maintenance needs on the female patient. Demonstrate a comprehensive knowledge foundation of the clinically supportive cognitive sciences Obtain the necessary clinical skills to diagnose and manage the health needs of populations and communities. Practice-Based Learning and Improvement 26 Demonstrates good knowledge of medical interviewing techniques and understands significance of physical examination findings. Locate, appraise and assimilate evidence from scientific studies related to their patients’ health problems; apply knowledge of epidemiologic principles, appropriate use of statistical methods, and proper study design to appraise information on diagnostic and therapeutic effectiveness Instructional Strategies Evaluation Methods Direct patient care under supervision, case conferences, tutorials, clinical rounds Direct patient care under supervision, case conferences, tutorials, clinical rounds Direct patient care under supervision, case conferences, tutorials, clinical rounds Direct patient care under supervision, case conferences, tutorials, clinical rounds Faculty evaluations NBME shelf examinations, OSCEs Faculty evaluations NBME shelf examinations, OSCEs Faculty evaluations NBME shelf examinations, OSCEs Faculty evaluation NBME shelf exams, OSCEs E-portfolio, Course narrative Case conferences, tutorials, clinical rounds Faculty evaluations NBME shelf exams, OSCEs Faculty evaluations NBME shelf exams, OSCEs E-portfolio, course narrative Faculty evaluations NBME shelf examinations, OSCEs Faculty evaluations, OSCEs E-portfolio, course narrative Direct patient care under supervision, case conferences, clinical rounds Direct patient care under supervision, case conferences, tutorials, clinical rounds Tutorials, clinical rounds, case conferences Documentation E-portfolio, course narrative E-portfolio, course narrative E-portfolio, course narrative E-portfolio, course narrative E-portfolio, course narrative General Objectives Interpersonal Skills and Communication Professionalism Patient Care Instructional Strategies Evaluation Methods Use information technology to manage information, access on-line information, and support self-education. Tutorials Faculty evaluations, OSCEs E-portfolio Use information technology to manage information, access on-line information, and support self-education Analyze clinical experiences and reflect on personal practice patterns to initiate practice-based improvement activities using a systematic methodology Facilitates the learning of students and other health care professionals. Clinical rounds, case conferences Faculty evaluations, OSCEs E-portfolio Patient panel audit Faculty evaluations E-portfolio Tutorials, clinical rounds, case conferences Clinical care under supervision Faculty evaluations, OSCEs E-portfolio, course narrative Faculty evaluations, patient evaluations E-portfolio Create and sustain a therapeutic and ethically sound relationship with patients. Clinical care under supervision Faculty evaluations, patient evaluations E-portfolio Work effectively with others as a member or leader of a healthcare team. Clinical care under supervision Faculty evaluations, patient evaluations E-portfolio Recognize that the need to learn and develop professionally is continuous. Conferences; faculty role modeling E-portfolio Demonstrate a commitment to ethical principles pertaining to provision or withholding of clinical care, confidentiality of patient information, informed consent, and business practices. Conferences Health care team and faculty evaluations Faculty evaluations Demonstrate sensitivity and responsiveness to patients and colleague’s culture, age, gender, race, religion, and sexual preferences. Supervised clinical experiences, tutorials Faculty evaluations E-portfolio Demonstrate respect, compassion and integrity; a responsiveness to the needs of patients and society that supersedes selfinterest; accountability to patients, society and the profession; and a commitment to excellence and ongoing professional development. Clinical rounds, supervised clinical care OSCEs, faculty evaluations E-portfolio, course narrative Demonstrate caring, respectful and effective communication skills when interacting with patients and families. Supervised clinical experiences Faculty and patient evaluations, OSCEs E-portfolio Gather essential and accurate patient information through history and physical examination and collection of pertinent data. Supervised clinical experiences, rounds Faculty evaluations E-portfolio Formulate appropriate diagnostic and therapeutic management strategies for patients with common health problems including emergent, acute or chronic across the spectrum of disciplines based on patient Supervised clinical experiences, rounds, case conferences Faculty evaluations, OSCEs, NBME exams E-portfolio Knowledge & Skills Objectives Use effective listening skills and elicit and provide information using effective nonverbal, explanatory, questioning and writing skills. Documentation E-portfolio 27 General Objectives Instructional Strategies Evaluation Methods Develops and implements patient management plans that actively engage the patient and caretakers. Use information technology to optimize patient care. Supervised clinical experiences, rounds, case conferences Supervised clinical care Faculty evaluations, OSCEs, NBME exams Faculty evaluations E-portfolio Perform competently appropriate medical and invasive procedures considered essential for entering any area of graduate medical education. Supervised clinical care Faculty evaluations E-portfolio Promote standard health maintenance and disease prevention. Supervised clinical care, conferences NBME exams E-portfolio Work with other health professionals to provide patient focused care. Supervised clinical care Faculty evaluations E-portfolio Understand how their patient care and other professional practices affect other healthcare professionals, the healthcare organization and the larger society. Clinical conferences, reflective writing Faculty evaluations E-portfolio Advocate for quality patient care and assist patients in dealing with system complexities. Clinical conferences, supervised clinical care Faculty and patient evaluations E-portfolio Act as advocates for better health for patients and the community by partnering with health care managers and providers to assess, coordinate and improve health outcomes. Supervised clinical care Health care team evaluations E-portfolio Know how types of medical practice and delivery systems differ from one another, including methods of controlling health care costs and allocating resources Practice cost-effective healthcare and resource allocation that does not compromise quality of care. Supervised clinical care, conferences Faculty evaluations E-portfolio Supervised clinical care, conferences Faculty evaluations E-portfolio Knowledge & Skills Objectives Documentation information and preferences, current evidence and clinical judgment, while considering costs for the patient and the system. Systems-Based Practice E-portfolio Every student will receive an MD Program Outcomes Evaluation (often referred to as Competency Evaluation) that is based upon the established overall MD Program Outcomes for the MD Curriculum at TCMC. This is a quantitative assessment that uses a scale of 1-9 for each competency item. The “Meets Expectations Criteria” has a scale of 4-6 and the expectation is that third year MD students will attain a mean score of 6.0 or greater in MS 3 and MS 4. This score is for MD program evaluation purposes only and is not calculated into the students’ final grade given for the course or used for any other student based evaluation purposes. It is reported in aggregate for program review purposes only. 28