Low Tidal Volume Ventilation Form
advertisement
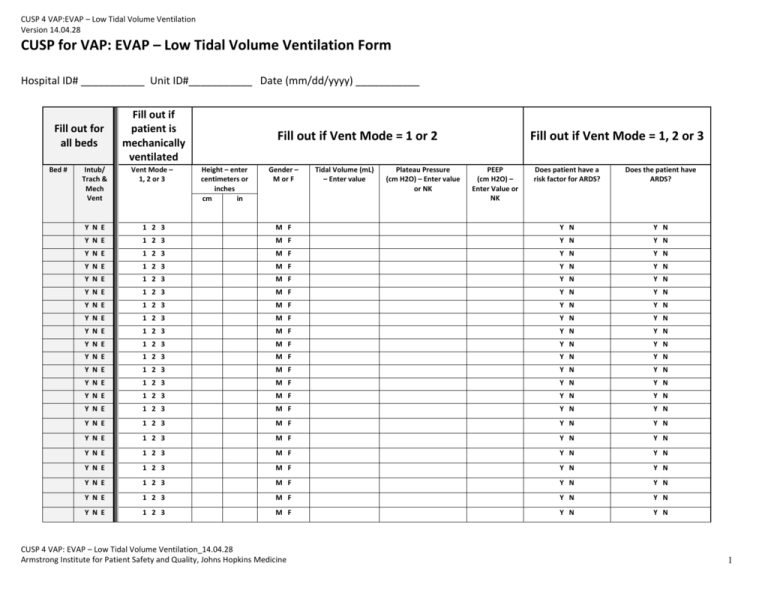
CUSP 4 VAP:EVAP – Low Tidal Volume Ventilation Version 14.04.28 CUSP for VAP: EVAP – Low Tidal Volume Ventilation Form Hospital ID# ___________ Unit ID#___________ Date (mm/dd/yyyy) ___________ Fill out for all beds Bed # Fill out if patient is mechanically ventilated Intub/ Trach & Mech Vent Vent Mode – 1, 2 or 3 Y N E 1 2 3 Y N E 1 2 3 Y N E Y N E Fill out if Vent Mode = 1 or 2 Height – enter centimeters or inches cm in Gender – M or F Does patient have a risk factor for ARDS? Does the patient have ARDS? M F Y N Y N M F Y N Y N 1 2 3 M F Y N Y N 1 2 3 M F Y N Y N Y N E 1 2 3 M F Y N Y N Y N E 1 2 3 M F Y N Y N Y N E 1 2 3 M F Y N Y N Y N E 1 2 3 M F Y N Y N Y N E 1 2 3 M F Y N Y N Y N E 1 2 3 M F Y N Y N Y N E 1 2 3 M F Y N Y N Y N E 1 2 3 M F Y N Y N Y N E 1 2 3 M F Y N Y N Y N E 1 2 3 M F Y N Y N Y N E 1 2 3 M F Y N Y N Y N E 1 2 3 M F Y N Y N Y N E 1 2 3 M F Y N Y N Y N E 1 2 3 M F Y N Y N Y N E 1 2 3 M F Y N Y N Y N E 1 2 3 M F Y N Y N Y N E 1 2 3 M F Y N Y N Y N E 1 2 3 M F Y N Y N CUSP 4 VAP: EVAP – Low Tidal Volume Ventilation_14.04.28 Armstrong Institute for Patient Safety and Quality, Johns Hopkins Medicine Tidal Volume (mL) – Enter value Plateau Pressure (cm H2O) – Enter value or NK Fill out if Vent Mode = 1, 2 or 3 PEEP (cm H2O) – Enter Value or NK 1 CUSP 4 VAP:EVAP – Low Tidal Volume Ventilation Version 14.04.28 Ventilator Modes: Enter 1 – if the patient’s vent is set to one of the following Volume Cycled Modes 1. Continuous Mandatory Ventilation (CMV) 2. Assist Control (AC) 3. Synchronized Intermittent Mandatory Ventilation (SIMV) 4. Volume Support (VS) 5. Pressure Regulated Volume Controlled (PRVC) Enter 2 – if the patient’s vent is set to one of the following Pressure Cycle Modes 1. Pressure Support (PS) 2. Continuous Positive Airway Pressure (CPAP) 3. Pressure Control (PC) 4. Airway Pressure Release Ventilation (APRV) 5. BiLevel Ventilation Enter 3 – if the patient’s vent is set to one of the following modes 1. Proportional Assist Ventilation (PAV) 2. Adaptive Support Ventilation (ASV) 3. Inverse Ratio Ventilation 4. High Frequency Oscillatory Ventilation (HFOV) 5. Extracorporeal Membrane Oxygenation (ECMO) 6. Other CUSP 4 VAP: EVAP – Low Tidal Volume Ventilation_14.04.28 Armstrong Institute for Patient Safety and Quality, Johns Hopkins Medicine 2 CUSP 4 VAP:EVAP – Low Tidal Volume Ventilation Version 14.04.28 Instructions for CUSP4MVP-VAP – Low Tidal Volume Ventilation Form Please complete this form once a day, every day. If possible, complete it around the same time each day, hopefully during patient rounds. Patients are considered to be mechanically ventilated on a specific day if they were mechanically ventilated at the time of observation. All of the vent modes are listed on the back of the data collection sheet. Please print the data collection sheet with the vent modes on the back of the sheet for ease of data collection. DATA FIELD DIRECTIONS Hospital: Enter the name of your hospital. ICU: Enter the name of your unit. Date: Enter today’s date as MM/DD/YYYY format (e.g. 01/31/2014). Bed #: Enter all the bed numbers on the form, whether the patient is on mechanical ventilation or not. Include empty beds. Intub/Trach & Mech Vent: Is the patient currently receiving mechanical ventilation? Enter for all patients. Mechanical ventilation is defined as receiving ventilator support via an ETT or tracheostomy tube. Patients treated with non-invasive ventilation would be counted as ‘N’ Enter ‘Y’ if the patient is currently intubated/trached and mechanically ventilated. Enter ‘N’ if the patient is not currently intubated /trached and mechanically ventilated. Enter ‘E’ if there is no patient in the bed. For any specific patient, if the patient is not currently intubated/trached AND on mechanical ventilation, STOP. Do not enter any more information regarding that bed for this date. CUSP 4 VAP: EVAP – Low Tidal Volume Ventilation_14.04.28 Armstrong Institute for Patient Safety and Quality, Johns Hopkins Medicine 3 CUSP 4 VAP:EVAP – Low Tidal Volume Ventilation Version 14.04.28 Ventilator Mode DATA FIELD DIRECTIONS Enter for all patients receiving mechanical ventilation. Enter 1, 2, or 3 on the form depending on which type of vent mode is being used at the time of observation. Enter 1 – if the patient’s vent is set to one of the following Volume Cycled Modes 6. Continuous Mandatory Ventilation (CMV) 7. Assist Control (AC) 8. Synchronized Intermittent Mandatory Ventilation (SIMV) 9. Volume Support (VS) 10. Pressure Regulated Volume Controlled (PRVC) Vent Mode: What mode of ventilation is being used at the time of observation? Enter 2 – if the patient’s vent is set to one of the following Pressure Cycle Modes 6. Pressure Support (PS) 7. Continuous Positive Airway Pressure (CPAP) 8. Pressure Control (PC) 9. Airway Pressure Release Ventilation (APRV) 10. BiLevel Ventilation Enter 3 – if the patient’s vent is set to one of the following modes – If your answer is 3, skip to “Does patient have a risk factor for ARDS?” 7. Proportional Assist Ventilation (PAV) 8. Adaptive Support Ventilation (ASV) 9. Inverse Ratio Ventilation 10. High Frequency Oscillatory Ventilation (HFOV) 11. Extracorporeal Membrane Oxygenation (ECMO) 12. Other For any specific patient, if the numerical value equals 3, skip to “Does patient have a risk factor for ARDS?” AND “Does the patient have ARDS?” CUSP 4 VAP: EVAP – Low Tidal Volume Ventilation_14.04.28 Armstrong Institute for Patient Safety and Quality, Johns Hopkins Medicine 4 CUSP 4 VAP:EVAP – Low Tidal Volume Ventilation Version 14.04.28 Height FIELD DIRECTIONS Evaluate daily for patients receiving mechanical ventilation and whose vent mode equals 1 or 2. Don’t enter both centimeters and inches. Height: How tall is the patient? Enter the patient’s height in centimeters in the “cm”column if your unit uses centimeters. Enter the patient’s height in inches in the “in” column if your unit uses inches. Gender FIELD DIRECTIONS Evaluate daily for patients receiving mechanical ventilation and whose vent mode equals 1 or 2. Gender Enter “M”, if the patient is male. Enter “F”, if the patient is female. For transgender patients, please enter their birth gender. For transsexual patients, please enter their current gender. CUSP 4 VAP: EVAP – Low Tidal Volume Ventilation_14.04.28 Armstrong Institute for Patient Safety and Quality, Johns Hopkins Medicine 5 CUSP 4 VAP:EVAP – Low Tidal Volume Ventilation Version 14.04.28 Tidal Volume FIELD DIRECTIONS Evaluate daily for patients receiving mechanical ventilation and whose vent mode equals 1 or 2. Enter the Tidal Volume in milliliters (mL). Use the Preset tidal (prescribed) volume if the mode is one of the Volume Cycled Modes (from Vent Mode question above). Tidal Volume: What is the Tidal Volume at the time of observation? If the modes is one of the Pressure Cycle Modes (from Vent Mode question, above), enter the approximate expired tidal volume. If the vent mode for the patient is in the third group of vent modes (from Vent Mode question, above), you should not be collecting this data. (Please read instructions for Vent Mode, above.) Plateau Pressure FIELD DIRECTIONS Evaluate daily for patients receiving mechanical ventilation and whose vent mode equals 1 or 2. Enter the Plateau Pressure at or nearest to the time of observation. Plateau Pressure: What is the Plateau Pressure at or nearest to the time of observation? If it is not available or unknown, please enter “NK”. For APRV/BiLevel modes, this is the Plow value. If the vent mode for the patient is in the third group of vent modes (from Vent Mode question, above), you should not be collecting this data. (Please read instructions for Vent Mode, above.) CUSP 4 VAP: EVAP – Low Tidal Volume Ventilation_14.04.28 Armstrong Institute for Patient Safety and Quality, Johns Hopkins Medicine 6 CUSP 4 VAP:EVAP – Low Tidal Volume Ventilation Version 14.04.28 PEEP (Positive End-Expiratory Pressure) FIELD DIRECTIONS Evaluate daily for patients receiving mechanical ventilation and whose vent mode equals 1 or 2. Enter the PEEP value at or nearest to the time of observation. PEEP: What is the PEEP (Positive EndExpiratory Pressure at or nearest to the time of observation? If it is not available or unknown, please enter “NK”. For APRV/BiLevel modes, this is the Plow value. If the vent mode for the patient is in the third group of vent modes (from Vent Mode question, above), you should not be collecting this data. (Please read instructions for Vent Mode, above.) ARDS FIELD DIRECTIONS Evaluate daily for patients receiving mechanical ventilation and whose vent mode equals 1, 2 AND 3. ARDS Risk Factors: Does the patient have a Risk Factor for ARDS? If the patient has one or more of the following, enter “Y”, otherwise enter “N”. 1. Pneumonia 2. Sepsis, Severe Sepsis or Septic Shock, not secondary to pneumonia 3. Aspiration 4. Trauma Remember to answer this question even if your Vent Mode = 3. (Please read instructions for Vent Mode, above.) CUSP 4 VAP: EVAP – Low Tidal Volume Ventilation_14.04.28 Armstrong Institute for Patient Safety and Quality, Johns Hopkins Medicine 7 CUSP 4 VAP:EVAP – Low Tidal Volume Ventilation Version 14.04.28 Evaluate daily for patients receiving mechanical ventilation and whose vent mode equals 1, 2 AND 3. ARDS: Does the patient of the diagnosis of ARDS at the time of the observation? If the patient has a diagnosis of ARDS at the time of observation, enter “Y”, otherwise enter “N”. Remember to answer this question even if your Vent Mode = 3. (Please read instructions for Vent Mode, above.) Please enter data from this paper-based data collection form in the CECity web-based reporting system at least once per week. CUSP 4 VAP: EVAP – Low Tidal Volume Ventilation_14.04.28 Armstrong Institute for Patient Safety and Quality, Johns Hopkins Medicine 8