Correlation of virologincal and clinical profile of patients with chronic
advertisement

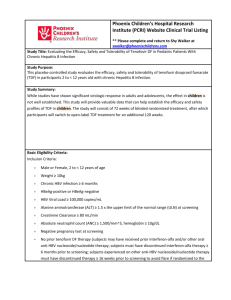
TITLE PAGE: Original Research Article CORRELATION OF VIROLOGICAL AND CLINICAL PROFILE IN PATIENTS WITH BC-COINFECTION IN OUR SET-UP JAVED IQBAL FAROOQI, RIAZMUHAMMAD, ZAFAR ALI, ABDURREHMAN, INTEKHABALAM, NOORULLAH KHAN, MOHAMMAD JAMSHED KHAN MUHAMMADASGHAR, FAROOQ AHMAD Department of Medicine, PGMI, LRH, Peshawar ABSTRACT OBJECTIVE:to find out and correlate the virological and clinical profile in our patients with chronic hepatitis B and C co-infection. MATERIAL AND METHODS:This observational, descriptive and cross-sectional study was conducted at Medical A Ward, PGMI, LRH Peshawar and Author’s Private Hepatology Clinic, Akber Medical Center, Peshawar, from July 2010 to June 2014. All patients with HBsAg and Anti-HCV Reactive by ELISA for more than 6 months were included in the study. Following investigations were carried out in these patients: Serum ALT, HBeAg, anti-HBe, HBV DNA PCR, HCV RNA PCR, and abdominal ultrasound. Data was entered and analyzed using SPSS version 16.0. RESULTS: A total of 130 patients were included in the analysis, out of which 81 (62.3%) were males. Mean age of patients was 40.52±14.27 years. Majority of patients belonged to age-group of 21-30 years. Mean serum ALT of patients was 83.69±60.48 U/L. Majority of patients belonged to ALT-Group of 41-80 U/L. Hepatitis C Virus was the dominant virus in 53% of patients. Chronic Hepatitis was the dominant clinical profile in 73% of patients. CONCLUSION:Hepatitis C Virus is the dominant virus in our patients with BC co-infection. There is no statistically significant association between virological and clinical profile of these patients. KEY WORDS:Hepatitis B Virus, Hepatitis C Virus, BC Co-infection, Chronic Hepatitis, Cirrhosis, Hepatocellular Carcinoma INTRODUCTION Hepatitis B and hepatitis C viruses are the most commoncauses of chronic liver disease worldwide. Approximately 350 million people are infected with HBV1and another 170 million people with HCV2.Both chronic Hepatitis B and Ccan progress to cirrhosis and later on hepatocellular carcinoma (HCC).Chronic hepatitis B leads to cirrhosis and HCC in 5-40% of patients3, with an annual death rate of an over a million people worldwide4,5. Similarly, chronic hepatitis C leads to cirrhosis and HCC in 32% of patients, with an annual death rate of half a million people worldwide6. As hepatitis B and C share same modes of transmission, co-infection with these viruses is possible7. Infection with multiple viruses leads to management problems with higher incidence ofmorbidity and mortality8. Therefore, BC Co-infection may potentially lead to moresevere liver disease, with an increased risk of progressionto cirrhosis and HCC9-12.HBV super-infection in patientswith chronic hepatitis C, and HCV super-infection inpatients with chronic hepatitis B have both been reported13-15. In Pakistan, overall national prevalence of HBsAg is 2.5%, antiHCV is 4.9%, and BC Co-infection is 0.1%16. Several studies have shown that the HBV and HCV interactwith each other and affect immune responses17-22. The present study was conducted to find out the virological and clinical profile in patients with chronic hepatitis B and C co-infection in our set-up. MATERIAL AND METHODS This observational, descriptive and cross-sectional study was conducted at Medical A Ward, PGMI, LRH Peshawar and author’s private practice setup, over4 years’ time period (from July 2010 to June 2014). All patients with HBsAg and Anti-HCV Reactive by ELISA for more than 6 months were included in the study by convenience sampling. Patients, who were currently receiving or had received in past antiviral therapy, were excluded from the study. As per routine clinical practice protocol, following investigations were carried out in all of these patients: Serum ALT, HBeAg, anti-HBe, HBV DNA Qualitative PCR, HCV RNA Qualitative PCR, and abdominal ultrasound. According to virological profile, patients were divided in four groups: 1) Both Active: those patients in whom both HBV and HCV PCRs were detected; 2) HBV Active: those patients in whom HBV PCR was detected and HCV PCR was not-detected; 3) HCV Active: those patients in whom HCV PCR was detected and HBV PCR was not-detected; and 4) Both Inactive: those patients in whom both HBV and HCV PCRs were not-detected. Chronic hepatitis B patients were classified into: 1) CHB-ITP (Chronic Hepatitis B Immune Tolerant Phase): those patients, who were having HBV-DNA PCR detected, HBeAg Reactive, Anti-HBe Non-Reactive, with normal serum ALT; 2) CHB-IRP (Chronic Hepatitis B Immune Reactive Phase): those patients, who were having HBV-DNA PCR detected, HBeAg Reactive, Anti-HBe Non-Reactive, with raised serum ALT; 3) CHB-ICP (Chronic Hepatitis B Immune Control Phase): those patients, who were having HBV-DNA PCR not-detected, HBeAg Non-Reactive, Anti-HBe Reactive, with normal serum ALT; and 4) CHB-IEP (Chronic Hepatitis B Immune Escape Phase): those patients, who were having HBV-DNA PCR detected, HBeAg Non-Reactive, Anti-HBe Reactive, with raised serum ALT. According to clinical profile, patients were divided in three groups: 1) Chronic Hepatitis: those patients in whom ultrasound was showing normal liver with portal vein of normal size, spleen of normal size, and no evidence of ascites; 2) Cirrhosis: those patients in whom ultrasound was showing liver with coarse echogenic parenchyma to small nodular liver, increased portal vein diameter, enlarged spleen with or without ascites; and 3) Hepatocellular Carcinoma (HCC): those patients in whom ultrasound showing space occupying lesion, confirmed as hepatocellular carcinoma by triphasic CT liver with raised serum alpha fetoproteins (AFP). SPSS Version 16.0 was used to analyze the data. After entry, descriptive statistics was used to calculate Mean + SD (Standard Deviation) for numerical variables like age (in years) and ALT levels. Frequencies/Percentages were calculated for gender, virological and clinical profile of patients. Chi-square (in Crosstabs analysis) was used to identify significant association between virological and clinical profile of the patients. RESULTS A total of 130 patients with BC Co-infection were assessed during the study period. Among them 81(62.3%) were males and 49 (37.7%) were females. Mean age was 40.52±14.272 years. Their age range was from 10 to 85 years. Majority of patients belonged to age-group of 21-30 years, followed by age-group of 41-50 years (Table-1). Mean serum ALT was 83.69 ± 60.482 U/L. Their Serum ALT range was from 18 to 377 U/L. Majority of patients belonged to ALT-Group of 41-80 U/L, followed by ALT-Group of 81-120 U/L (Table-2). Among the four virological profile groups, majority of patients belonged to “C Active” group, followed by “Both Active” group (Table-3). Among the four HBV virological profile groups, majority of patients belonged to “CHB-ICP”-group, followed by “CHB-IRP”-group (Table-4). Among three clinical profile groups, majority of patients belonged to “Chronic Hepatitis”group, followed by “Cirrhosis”-group (Table-5). Majority of patients with “Chronic Hepatitis”was females and majority of patients with “Cirrhosis”was males (Table-6). Majority of patients with “Chronic Hepatitis” was in the age-group of 21-30 years whereas majority of patients with “Cirrhosis” was in the age-group of 41-50 years (Table-7). Majority of patients with “Chronic Hepatitis”as well as “Cirrhosis” was having ALT in the range of 41-80 U/ (Table-8). Pearson Chi-Square test showed that there is no statistically significant association between virological and clinical profile of these patients, and similarly Phi and Cramer’s V systemic measures showed that the strength of association between virological and clinical profile is very weak (Table-9). DISCUSSION In our study, male to female ratio was 1.6:1 among 130 patients studied. Results of the current study revealed that 74% of chronic liver disease patients were in 3rd to 5th decade oflife. Chronic hepatitis patients were a decade younger than cirrhotic patients, whereas HCCpatient was a decade older at an average. Increasing age is a higher risk to have thedisease, probably due to longer exposure to multiple risk factors23-29. In our study, 62% of chronic liver disease caseswere younger than 50-years of age, out of which 31% younger than 30 years of age; the percentage gradually decreased in the later decades. The reason could be an earlychildhood infection with the hepatitis viruses. The chronic infection with hepatitis virusesleads to slow progressive liver disease. It may end up in cirrhosis, chronic liver failure,and hepatocellular carcinoma (HCC) over a period of up to 30 years30,31.Since the route of transmission for these viruses are similar, so patientscould have co-infection with one or two viruses. Co-infection with HBV and HCV has been reported from Pakistan32,33. Studies have shown that the HBV and HCV interact with each other and affect immune responses. Four virological profiles have been described: Active HCV, Active HBV, Dual Active BC, and Inactive BC. In our study, HCV was active in more than half of the patients (53%) with inactive HBV. Many studies have shown the same trend in BC Co-infected17-19. Chronic hepatitis B patients who become superinfected with HCV can undergo seroconversion of HBeAg and HBsAg to respective antibodies20-22. Longitudinal studies have found 2.08% annual incidence of HBsAg seroconversion in BC Co-infected patients as compared to 0.43% in patients with HBV monoinfection34,35. Several authors have reported that HBV can reciprocally inhibit HCV replication as well36-38. In our study, only 11% of patients were having active HBV and inactive HCV. An Italian study reported 71% HCV RNA clearance in BC Co-infected patients as compared to 14% in HCVmonoinfection39. Furthermore, mutual suppression of each other in BCCo-infected patients hasalso been reported40. In our study, 14% of patients were having both inactive HBV and HCV. Chronic hepatitis BC coinfected patients can present in three possible clinical phases: Chronic Hepatitis, Cirrhosis, and Hepatocellular carcinoma. In our study, 73% patients belonged to chronic hepatitis stage. Majority of them was females, in the age-group of 21-40 years, and having ALT in the range of 41-80 U/L. In majority of these HCV was active alone or in combination of active HBV (dual active infection). These patients are at highest risk of progressionto cirrhosis and decompensated liver disease, and therefore,should be considered for treatment.In our study, Cirrhosis was found in 26% of BC-coinfected patients irrespective of their virological profile. Majority of patients were males and in the age-group of 31-50 years. No specific trend was seen regarding ALT levels.Studies have reported higher rates of cirrhosis in BC-coinfected patients as compared to mono-infected patients17, 38, 41, but we our study did not reveal statistically significant association between virological and clinical profile of BCcoinfected patients.We found only one case of HCC, a male patient over 70 years of age. BCcoinfected patients have an increased risk ofdeveloping HCC9,10,12,41,42. Because of thelikely increased risk of developing HCC, coinfectedpatients should receive regular 6-month and possiblemore frequent screening with ultrasound of the liver andserum alfa-fetoprotein levels. CONCLUSION Co-infection with HBV and HCV is not uncommon, especiallywithin areas of high prevalence of hepatitis B. We could not find any statistically significant association between virological and clinical profile of these patients, rather the strength of association between virological and clinical profile was very weak. Dualinfections present unique management challenges giventhe complex interaction of HBV and HCV, and the propensityfor developing more severe liver disease. Treatment decisions should bemade based upon the determination of the "dominant"hepatitis virus. Caution must be exercised in treatingcoinfected patients, as flares of the untreated virus mayoccur. No standard of care has been established for treatmentof coinfected patients, and larger randomized, controlledtrials are needed to clarify the optimal treatmentfor such patients and the role of newer antiviral agents. Table-1: Age-wise distribution of patients Age group (years) No of Patients 1-10 1 11-20 4 21-30 37 31-40 26 41-50 33 51-60 21 61-70 6 71-80 1 81-90 1 Total 130 Percent 0.8 3.1 28.5 20.0 25.4 16.2 4.6 0.8 0.8 100 Table-2: ALT Levels of patients ALT Levels (U/L) No of Patients <40 23 41-80 60 81-120 28 121-160 5 161-200 7 >200 7 Total 130 Percent 17.7 46.2 21.5 3.8 5.4 5.4 100 Table-3: Virological Profile of Patients Virological Profile No of Patients Both Active 28 HBV Active 15 HCV Active 69 Both Inactive 18 Total 130 Percent 21.5 11.5 53.1 13.8 100 Table-4: HBV Virological Profile of patients HBV Virological Profile No of Patients CHB-ITP 1 CHB-IRP 31 CHB-ICP 87 CHB-IEP 11 Total 130 Table-5: Clinical Profile of Patients Clinical Picture No of Patients Chronic Hepatitis 95 Cirrhosis 34 Percent 0.8 23.8 66.9 8.5 100 Percent 73.0 26.2 HCC 1 0.8 Total 130 100 Table-6: Gender-wise distribution of Clinical Profile of patients Age group Clinical Status of Patients Chronic Hepatitis Cirrhosis No of pts Percent No of pts Percent Male (n=81) 52 64.2 28 34.6 Female (n=49) 43 87.8 6 12.2 Total 95 73.0 34 26.2 HCC No of pts 1 0 1 Percent 1.2 0 0.8 Table-7: Age-wise distribution of Clinical Profile of patients Age Group Clinical Status of Patients Chronic Hepatitis Cirrhosis No of pts Percent No of pts Percent 1-10 1 0.77 0 0 11-20 4 3.07 0 0 21-30 35 26.93 2 1.54 31-40 20 15.38 6 4.62 41-50 21 16.15 12 9.23 51-60 12 9.23 9 6.92 61-70 2 1.54 4 3.08 71-80 0 0 0 0 81-90 0 0 1 0.77 Total 95 73.0 34 26.2 HCC No of pts 0 0 0 0 0 0 0 1 0 1 Percent 0 0 0 0 0 0 0 0.77 0 0.8 Table-8: ALT levels regarding Clinical Profile of patients ALT Levels Clinical Status of Patients (U/L) Chronic Hepatitis Cirrhosis No of pts Percent No of pts Percent <40 17 13.07 6 4.61 41-80 46 35.37 14 10.77 81-120 22 16.91 6 4.61 121-160 2 1.54 3 2.31 161-200 4 3.08 2 1.54 >200 4 3.08 3 2.31 Total 95 73.0 34 26.2 HCC No of pts 0 0 0 0 1 0 1 Percent 0 0 0 0 0.8 0 0.8 Table-9: Correlation of Virological and Clinical Profiles of patients Virological Clinical Status of Patients Profile Chronic Hepatitis Cirrhosis†‼* No of pts Percent No of pts Percent Both Active† 20 15.36 8 6.15 HBV active‼ 13 10.00 2 1.54 HCV Active* 47 36.13 21 16.15 Both Inactive 15 11.51 3 2.31 HCC No of pts 0 1 0 0 Percent 0 0.8 0 0 Total 95 73.0 34 26.2 1 0.8 *Both-Active vs Rest = Pearson Chi-square p value = 0.552, Phi & Cramer’s V p value = 0.552 ‼HBV-Active vs Rest = Pearson Chi-square p value = 0.186, Phi & Cramer’s V p value = 0.186 †HCV-Active vs Rest = Pearson Chi-square p value = 0.966, Phi & Cramer’s V p value = 0.966 Correspondence: Javed Iqbal Farooqi FCPS (Medicine), FCPS (Gastroenterology) Associate Professor of Medicine Medical A Unit, PGMI, LRH, Peshawar E-mail: dr_farooqi@hotmail.com Phone: 0333-9123818