- D-Scholarship@Pitt
advertisement

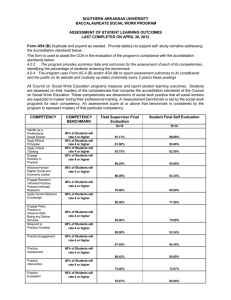
WORKFORCE DEVELOPMENT AT THE ALLEGHENY COUNTY HEALTH DEPARTMENT: IDENTIFYING TRAINING PRIORITIES THROUGH SELF-ASSESSMENT by Alyssa K. Landen BA, Franklin & Marshall College, 2012 Submitted to the Graduate Faculty of the Department of Health Policy & Management Graduate School of Public Health in partial fulfillment of the requirements for the degree of Master of Public Health University of Pittsburgh 2014 i UNIVERSITY OF PITTSBURGH GRADUATE SCHOOL OF PUBLIC HEALTH This essay is submitted by Alyssa K. Landen on December 4, 2014 and approved by Essay Advisor: Gerald M. Barron, MPH Associate Professor Department of Health Policy & Management Graduate School of Public Health University of Pittsburgh __________________________________ Essay Reader: Ronald Voorhees, MD MPH Professor of Public Health Practice Department of Epidemiology Associate Dean for Public Health Practice Director, Center of Public Health Practice Graduate School of Public Health University of Pittsburgh __________________________________ Essay Reader: Jamie Sokol, MPH __________________________________ Workforce Development and Training Administrator Allegheny County Health Department Allegheny County, Pennsylvania ii Copyright © by Alyssa K. Landen 2014 iii Gerald M. Barron, MPH WORKFORCE DEVELOPMENT AT THE ALLEGHENY COUNTY HEALTH DEPARTMENT: IDENTIFYING TRAINING PRIORITIES THROUGH SELF-ASSESSMENT Alyssa K. Landen, MPH University of Pittsburgh, 2014 ABSTRACT A competent and skilled public health workforce is crucial in delivering the ten essential services of public health. Recognizing this, the Public Health Accreditation Board has incorporated workforce development and training into its national accreditation standards for State, Local, and Tribal Health Departments. Currently, the Allegheny County Health Department is in the preapplication phase of accreditation. Achieving accreditation status will ensure that the health department maintains standards related to population health. In June 2014, the Allegheny County Health Department administered a self-assessment of the Core Competencies for Public Health Professionals to its entire workforce to identify the training needs of the staff. The results of the survey will provide important, baseline data upon which a workforce development and training plan can be developed in accordance with accreditation standards. Through initial analysis of the assessment, it is recommended that the Allegheny County Health Department focus its efforts on public health policy, cultural competency, and the identification of community stakeholders. In addition, deputy directors and department managers will review assessment data relevant to their staff and identify trainings that can support the achievement of program-specific goals. Developing a training plan that supports the diversity of programs at Allegheny County Health Department will be a challenge; however, utilizing this type of evidence-based approach will best prepare its workforce to address current and future public health issues. iv TABLE OF CONTENTS PREFACE ..................................................................................................................................... X 1.0 CASE SITE ................................................................................................................... 1 1.1 THE STRUCTURE OF PUBLIC HEALTH IN PENNSYLVANIA .............. 1 1.1.1 Act 315: Pennsylvania’s Local Health Administration Law ....................... 2 1.2 THE ALLEGHENY COUNTY HEALTH DEPARTMENT .......................... 3 1.3 POPULATION THE ALLEGHENY COUNTY HEALTH DEPARTMENT SERVES ............................................................................................................................... 7 2.0 ISSUE AT HAND ....................................................................................................... 10 2.1 DOMAIN 8 OF ACCREDITATION: MAINTAIN A COMPETENT PUBLIC HEALTH WORKFORCE ................................................................................. 11 2.2 ACCREDITATION AT THE ALLEGHENEY COUNTY HEALTH DEPARTMENT .................................................................................................................. 12 3.0 LITERATURE REVIEW.......................................................................................... 13 3.1 WORKFORCE DEVELOPMENT DEFINED ............................................... 13 3.2 WORKFORCE DEVELOPMENT IN THE UNITED STATES .................. 14 3.2.1 History of Workforce Development ............................................................. 15 3.2.2 Workforce Development and Accreditation ............................................... 16 3.2.3 Methods for Workforce Development ......................................................... 16 v 3.3 THE IMPORTANCE OF INVESTING IN THE PUBLIC HEALTH WORKFORCE ................................................................................................................... 17 4.0 METHODS ................................................................................................................. 19 4.1 DEVELOPMENT OF SURVEY ...................................................................... 19 4.2 DETERMINATION OF METHODS OF ANALYSIS .................................. 22 4.3 ADMINISTRATION OF SURVEY ................................................................. 22 4.4 ANALYSIS OF SURVEY RESPONSES ......................................................... 23 4.5 DETERMINATION OF TRAINING PRIORITIES...................................... 25 4.6 NEXT STEPS ..................................................................................................... 28 5.0 RECOMMENDATIONS ........................................................................................... 30 5.1 PUBLIC HEALTH POLICY............................................................................ 31 5.1.1 Reason to Address ......................................................................................... 31 5.1.2 Recommended Trainings .............................................................................. 32 5.2 CULTURAL COMPETENCY ......................................................................... 33 5.2.1 Reason to Address ......................................................................................... 33 5.2.2 Recommended Trainings .............................................................................. 34 5.3 6.0 IDENTIFICATION OF STAKEHOLDERS .................................................. 35 5.3.1 Reason to Address ......................................................................................... 35 5.3.2 Recommended Trainings .............................................................................. 36 CONCLUSION........................................................................................................... 38 APPENDIX A: ORGANIZATIONAL STRUCTURE OF ALLEGHENY COUNTY HEALTH DEPARTMENT ........................................................................................................ 39 vi APPENDIX B: ALLEGHENY COUNTY HEALTH DEPARTMENT TRAINING NEEDS ASSESSMENT SURVEY QUESTIONS .................................................................................. 41 APPENDIX C: ALLEGHENY COUNTY HEALTH DEPARTMENT TRAINING NEEDS ASSESSMENT SURVEY SUMMARY OF DATA ANALYSIS ............................................ 54 APPENDIX D: ALLEGHENY COUNTY HEALTH DEPARTMENT TRAINING NEEDS ASSESSMENT SURVEY AND THE TEN ESSENTIAL SERVICES OF PUBLIC HEALTH ..................................................................................................................................... 56 APPENDIX E: SCREENSHOT OF TRAIN TOOL................................................................ 60 BIBLIOGRAPHY ....................................................................................................................... 61 vii LIST OF TABLES Table 1: Allegheny County Health Department number of employees by years in current position ......................................................................................................................................................... 5 Table 2: Allegheny County Health Department number of employees by program ...................... 6 Table 3: Training needs assessment survey average domain response......................................... 24 Table 4: Training needs assessment survey question findings ..................................................... 25 viii LIST OF FIGURES Figure 1: State public health structure within the United States agency ........................................ 1 Figure 2: Allegheny County Health Department percent of employees by years in current position............................................................................................................................................ 4 Figure 3: Allegheny County Health Department percent of employees by program ..................... 5 Figure 4: Location of Allegheny County Pennsylvania .................................................................. 8 Figure 5: Analysis of training needs assessment survey data breakdown .................................... 23 Figure 6: Training needs assessment survey average domain response ....................................... 26 Figure 7: Training needs assessment survey average domain response ....................................... 26 Figure 8: Ten Essential Services of Public Health........................................................................ 28 Figure 9. Allegheny County Health Department Organizational Structure .................................. 40 ix PREFACE I would like to take this opportunity to thank my advisor Gerald M. Barron, MPH for all of his support in identifying a case site for my essay and for his encouragement. I would like to thank Ronald Voorhees, MD MPH for his support through my practicum experience at the Allegheny County Health Department and for agreeing to be a reader of my essay. I would also like to thank the Allegheny County Health Department for providing me with the opportunity to participate in their accreditation and workforce development and training efforts. I would especially like to thank Jamie Sokol, MPH my mentor at the health department and to whom I owe much of my success in identification of an essay topic and writing this essay. x 1.0 1.1 CASE SITE THE STRUCTURE OF PUBLIC HEALTH IN PENNSYLVANIA Public health infrastructure varies from state to state. Local agency responsibility can be independent or shared with the state health agency (National Association of County and City Health Officials, 2014). Health departments within a state can be centralized (state governed), decentralized (locally governed), or a mix of the two agency (National Association of County and City Health Officials, 2014). As shown in Figure 1, Pennsylvania’s structure is mixed. (Source: National Association of County and City Health Officials, 2014) Figure 1: State public health structure within the United States agency 1 The financing of public health and public health staff within a state also vary among states. It is estimated that from 2008-2013, local health departments in the United States lost approximately 28,000 total employees, approximately a 12% decrease in FTEs (National Association of County and City Health Officials, 2014). Although the amount of funding a state receives depends on the economic status of the state, about 50% of the funding for states come from the federal government, through grants, cooperative agreements, and contracts (Salinsky, 2010). In 2009, 76% of state health departments and 55% of local health departments reported cuts within the past 12 months (Meyer and Weiselberg, 2009). In Pennsylvania, the median annual per capita local health expenditure is less than $20 (National Association of County and City Health Officials, 2014). Such losses in funding and staff have significantly reduced the number of initiatives and programs that a community can implement, and they must find ways to insure that the programs and interventions within the state are improving the health status of the community in which they serve. 1.1.1 Act 315: Pennsylvania’s Local Health Administration Law Act 315 and its amendments guide health departments within Pennsylvania. Since its establishment in 1951, provisions and amendments have been made to strengthen the act. These include (Pennsylvania Department of Health, 2013): Steps to establish a health department in Pennsylvania Act 12, which adds environmental health support Provisions to chapters 13, 15, 17, and 27 2 Additionally, Act 315 provides communities with (Pennsylvania Department of Health, 2013; Local Health Administration Law): The authority to establish local health departments to serve their residents The process of how to establish a local health department Financial administration guidance Documentation of powers and duties of local health departments, the director, and board of health Local health department jurisdiction State funding to recognized health departments to deliver public health services Health departments within Pennsylvania, under Act 315, are required to address administrative and supportive services, personal health services, and environmental health services (Pennsylvania Department of Health, 2013). 1.2 THE ALLEGHENY COUNTY HEALTH DEPARTMENT The Allegheny County Health Department was founded in 1957 (Allegheny County Health Department, 2014) and today serves the over 1.2 million residents of Allegheny County Pennsylvania. A Board of Health governs the Allegheny County Health Department, its nine members receiving their appointments from the County Chief Executive and approved by the County Council (Allegheny County Health Department, 2013). During their four-year appointment, these members advise the County Health Director (and appoint one if needed) and perform the following duties (Allegheny County Health Department, 2013): Formulate rules and regulations for the prevention of disease Formulate rules and regulations for the prevention and removal of conditions which constitute a menace to health Formulate rules and regulations for the promotion and preservation of the public health 3 The Allegheny County Health Department is one of only 6 county and 4 municipal health departments in Pennsylvania (Pennsylvania Department of Health, 2013). The mission of the Allegheny County Health Department is “to protect, promote, and preserve the health and wellbeing of all Allegheny County residents, particularly the most vulnerable” (Allegheny County Health Department, 2014). The workforce of the health department strives to fulfill the mission of the health department through programs and interventions aimed at improving health and well-being. The health department employs 349 individuals, not including contractors (as of September 30, 2014). Demographics of health department employees are not available because the health department is an equal opportunity employer. Based on a self-assessment, it is possible to determine the number of years individuals working at the health department have been in their current role (Figure 2 and Table 1) and distinguish which programs individuals work in (Figure 3 and Table 2). Appendix A provides a current organizational structure of the Allegheny County Health Department. Allegheny County Health Department Percent of Employees By Years In Current Position 14.8% 23.8% Less than 1 year 1-5 years 5-10 years 22.9% 7.2% 10-15 years 15-20 years Over 20 years 10.2% 21.1% Figure 2: Allegheny County Health Department percent of employees by years in current position 4 Table 1: Allegheny County Health Department number of employees by years in current position Allegheny County Health Department Number of Employees By Years In Current Position Less than 1 year 1-5 years 5-10 years 10-15 years 15-20 years Over 20 years Response Count Percent (%) 49 76 70 34 24 79 14.8 22.9 21.1 10.2 7.2 23.8 Administration Allegheny County Health Department Percent of Employees By Program Air Quality Chronic Disease and Injury Prevention Dental 14.2% 1.2% Directors Office/Leadership Team Epidemiology and Biostatistics 9.0% 4.2% 13.9% 0.6% 1.5% 9.9% 0.9% 3.0% 0.9% 2.4% 7.2% 9.3% 7.8% Food Safety Housing and Community Environment Infectious Diseases/STD Legal MIS Maternal Child Health Other 12.3% Preparedness 0.6% Public Drinking Water/Waste Management 0.9% Figure 3: Allegheny County Health Department percent of employees by program 5 Table 2: Allegheny County Health Department number of employees by program Allegheny County Health Department Number of Employees By Program Administration Air Quality Chronic Disease and Injury Prevention Dental Directors Office/Leadership Team Epidemiology and Biostatistics Food Safety Housing and Community Environment Infectious Diseases/STD Legal MIS Maternal Child Health Other Preparedness Public Drinking Water/Waste Management Public Health Laboratory Public Information, Health Information Publications WIC Response Count Percent (%) 30 46 2 5 3 8 24 26 41 3 2 31 10 3 33 14 9.0 13.9 0.6 1.5 0.90 2.4 7.2 7.8 12.3 0.9 0.6 9.3 3.0 0.9 9.9 4.2 1.2 and 4 47 14.2 It is important to note that most of the individuals working in the health department work in regulatory roles and very few provide administrative support. To better prepare employees to achieve the ten essential services of public health, the health department currently offers a limited set of trainings to employees. These trainings include: Required Preparedness Trainings o Incident Command System 100 and 700 o Points-of-Dispensing o American Heart Association CPR o American Heart Association First Aid o Hazmat Awareness (environmental health staff only) Non-Required Preparedness Trainings o Personal Preparedness o Swift Water Awareness o Incident Command System 300/400 (for certain staff only) 6 Health Department Wide Trainings o HIPAA o New Staff Orientation o Public Health 101 Additional trainings are needed to improve the competencies and capabilities of the workforce at the Allegheny County Health Department. 1.3 POPULATION THE ALLEGHENY COUNTY HEALTH DEPARTMENT SERVES Allegheny County is located in Southwestern Pennsylvania (Figure 4). Historically, Allegheny County and the City of Pittsburgh were major players in manufacturing and soon became a major port city due to the strategic location of rivers and location of the early towns on the riverbanks (Allegheny County Pennsylvania, n.d). In 1852, the Pennsylvania Railroad opened up Allegheny County and Pittsburgh to continued trade and Allegheny County soon became known for its steel and iron industries (Allegheny County Pennsylvania, n.d). 7 (Source: Pennsylvania Department of Transportation , 2014) Figure 4: Location of Allegheny County Pennsylvania As of 2013, the estimated population of Allegheny County Pennsylvania is 1,231,527 (United States Census Bureau, 2014). Of these individuals, 81.3% identify as white (79.9% identify as white not Hispanic or Latino), 13.3% identify as black, 0.2% identity as American Indian and Alaska Native, 3.2% identify as Asian, 1.9% identify as two or more races, and 1.8% identity as Hispanic or Latino (United States Census Bureau, 2014). In Allegheny County, the median household income from 2008-2012 was $50,644, with 12.7% of the population living below poverty level (United States Census Bureau, 2014). In Allegheny County, 5.2% of the individuals are under the age of 5, 19.2% are under the age of 18, 17.1% are 65 years of age or older, 51.9% of individuals are female, and 48.1% individuals are male (United States Census Bureau, 2014). Educational attainment estimates from 2008-2012 are listed below (United States Census Bureau: American FactFinder, 2014): 8 Less than 9th grade: 2.1% 9-12 grade, no diploma: 5.3% High school graduate: 31.5% Some college, no diploma: 17.2% Associate’s degree: 8.8% Bachelor’s degree: 20.8% Graduate or professional degree: 14.3% 9 2.0 ISSUE AT HAND The Public Health Accreditation Board (PHAB) notes “accreditation using the PHAB standards and measures can help a health department achieve performance excellence” (Public Health Accreditation Board, 2013b). The PHAB began working with health departments towards accreditation in September of 2011, with accreditation beginning in 2013 (Centers for Disease Control and Prevention, 2013). Accreditation of health departments is a voluntary program and signifies a health department is meeting national standards (Centers for Disease Control and Prevention , 2013). According to the PHAB, as of September 16, 2014, 54 health departments in the United States have received national accreditation (Public Health Accreditation Board, 2013a). National accreditation of health departments, although spearheaded by the PHAB, is supported by the Centers for Disease Control and Prevention and the Robert Wood Johnson Foundation (Centers for Disease Control and Prevention, 2014a). Benefits and impacts of accreditation include (Centers for Disease Control and Prevention , 2010): Improvement of health departments and infrastructure Valuable and measurable feedback on strengths and areas for improvement Improvements to delivery of public health services and programs Quality and performance improvement within all public health programs to better respond to health challenges Increasing accountability and credibility There are seven steps of accreditation (Public Health Accreditation Board, 2014): 1. Pre-application 2. Application 3. Documentation Selection and Submission 10 4. 5. 6. 7. Site Visit Accreditation Decision Reports Reaccreditation There are 12 domains of accreditation (Public Health Accreditation Board, 2013c): 2.1 Domain 1: Conduct and Disseminate Assessments Focused on Population Health Status And Public Health Issues Facing the Community Domain 2: Investigate Health Problems and Environmental Public Health Hazards to Protect the Community Domain 3: Inform and Educate about Public Health Issues and Functions Domain 4: Engage with the Community to Identify and Address Health Problems Domain 5: Develop Public Health Policies and Plans Domain 6: Enforce Public Health Laws Domain 7: Promote Strategies to Improve Access to Health Care Domain 8: Maintain a Competent Public Health Workforce Domain 9: Evaluate and Continuously Improve Processes, Programs, and Interventions Domain 10: Contribute to and Apply the Evidence Base of Public Health Domain 11: Maintain Administrative and Management Capacity Domain 12: Maintain Capacity to Engage the Public Health Governing Entity DOMAIN 8 OF ACCREDITATION: MAINTAIN A COMPETENT PUBLIC HEALTH WORKFORCE Domain 8 of the accreditation process focuses on building a competent workforce that is better prepared to deliver the ten essential services of public health. Domain 8 has two standards that are required of health departments (Public Health Accreditation Board, 2013c): Encourage the Development of a Sufficient Number of Qualified Public Health Workers Assess Staff Competencies and Address Gaps by Enabling Organizational and Individual Training and Development Under these standards, the health department must provide documentation of the following to measure each standard (Public Health Accreditation Board, 2013c): 11 Relationships and/or collaborations that promote the development of future public health workers Workforce development strategies A competent health department workforce Professional and career development for all staff Work environment that is supportive to the workforce 2.2 ACCREDITATION AT THE ALLEGHENEY COUNTY HEALTH DEPARTMENT Currently, the Allegheny County Health Department is in the pre-application phase of the accreditation process. This requires collaboration among staff members within different bureaus of the health department. Although there are many domains that must be addressed to become accredited, this essay looks at the second bullet above and addresses the process of determining the training needs of staff based on a self-assessment of core competencies. The documentation required for the measure “workforce development strategies” must include a workforce development plan and demonstrate that the health department implemented workforce development strategies (Public Health Accreditation Board, 2013c). An interdisciplinary working group, comprised of roughly twenty staff across all bureaus, has been developed to identify appropriate documentation for accreditation measures. The Allegheny County Health Department aims to submit an application for accreditation prior to December of 2015 and submit necessary documentation prior to December of 2016. 12 3.0 3.1 LITERATURE REVIEW WORKFORCE DEVELOPMENT DEFINED It is challenging to define workforce development within the context of public health due to the difficulties in even determining who is considered a public health professional. A public health worker can be interpreted to include those who are drivers within a health agency, transporting lab samples, or to include doctors who provide guidance to individuals on their health and behaviors that impact their health. A public health worker can be defined as an individual who “provide[s] essential public health services, regardless of the nature of the employing agency” (Beck et al, 2012), including those at public, private, and voluntary organizations (Turnock, 2003). This includes “all those engaged during a significant part of time in work that creates the conditions within which people can be healthy” (Tilson and Gebbie, 2004). Interviews with leaders in public health indicated that (Miner and Allan, 2014): “The public health workforce needs to be up-to-date in the practice of public health at the federal, state, and local levels There are organizations, personnel, and strategies in place to make this happen Public health academia should be more engaged in educating and training for public health practice with this increase practice engagement also benefitting academia There is a sense of ‘now is the time’ for public health to be as an essential player in the health care system” 13 Workforce development in public health “reflects the multiple disciplines constituting the field of public health” (Kaufman et al, 2014). Workforce development is thought to be a solution to gaps in competencies for public health workers who do not have a public health degree, a group that makes up a large portion of public health workers in the United States (Miner and Allan, 2014). However, not having a degree in public health or a lack of formal public health training does not mean that the current public health workforce is unprepared (Turnock, 2003). A systematic review of public health workforce literature, published in 2012, noted four themes and also indicated few articles were empirically based, peer reviewed, or provided evidencebased findings (Beck et al., 2012): 1. 2. 3. 4. Size and composition Effectiveness and health impact Demand Policy 3.2 WORKFORCE DEVELOPMENT IN THE UNITED STATES In 2000, the Public Health Functions Steering Committee published a report estimating there were approximately 500,000 public health professionals within government organizations and noted that there was a decrease in the public health workforce in comparison to a report they published in 1980 (Gebbie and Turnock, 2006). In acknowledgement of a decline in the public health workforce and gaps in competencies in the workforce, the federal government developed grant funded programs addressing training and preparedness (Gebbie and Turnock, 2006). Public health training centers were established to 14 “provide competency-based trainings and practice-based opportunities to advance the current and future public heath workforces” (Freedman et al., 2014). There are five steps in training module development in the public health training centers model (Millery et al., 2014): 1. 2. 3. 4. 5. Assess needs and identify priority competencies Define learning objectives and identify educational challenges Pose hypotheses and explore innovative technology based solutions Develop and deploy the educational experience Collect feedback and evaluate to inform continued cycles of revision and improvement For a short period of time, it appeared that the number of public health workers was increasing, peaking in 2003; however, a reverse in this trend appeared in 2004 (Gebbie and Turnock, 2006). The decline in the workforce of public health professionals can potentially be attributed to improvements in technology and changes in political and bureaucratics within government organizations (Gebbie and Turnock, 2006). 3.2.1 History of Workforce Development In 1988, the Institutes of Medicine noted the public health system as being in disarray (Beck et al., 2012) and “called for broad, crosscutting skills and competencies for public health practitioners” (Kaufman et al, 2014). In 2003, the Institutes of Medicine called for “continuous, lifelong training for the public health workforce” (Kenefick et al, 2014). In 2000, HealthyPeople2010 noted that improving the infrastructure of public health through investing in the workforce was a priority (Gebbie and Turnock, 2006), as concerns existed regarding the “composition, distribution, skills, and performance of the public health workforce” (Gebbie and Turnock, 2006). Today, HealthyPeople2020 still considers workforce development a priority for the nations public health officials. 15 3.2.2 Workforce Development and Accreditation In theory, addressing the competencies of a workforce through workforce development and training appears to be a simple and reasonable solution. Although it is acknowledged that additional training is needed, it was unclear for some time on how to determine baseline competencies of public health workers and what suggested workforce competencies should be. This lead to a project, that took a decade, by the Council on Linkages to develop a list of such competencies and how to assess for them in the workplace (Gebbie and Turnock, 2006). These established competencies “are critical for defining the desired outcomes of an educational activity, thus [provide] metrics useful for evaluating the effectiveness of skills acquisition” (Koo and Miner, 2010) and are “critical for public transparency and accountability” (Koo and Miner, 2010). Workforce development plays an important role in accreditation of health departments. Accreditation of health departments can serve as a method for monitoring the public health workforce. 3.2.3 Methods for Workforce Development A struggle exists between investing in training for the public health workforce and budget constraints. Recent studies have suggested using methods such as distance and online trainings. This method is possible due to advances in technology. These trainings are relatively inexpensive and this method removes the need for traveling to training centers, remove limits on the number 16 of individuals trained, and remove constraints due to time of training (Millery et al., 2014). It is recommended that training is active and that trainings include activities incorporating casestudies, problem solving, and bring learning into the workplace (Millery et al., 2014; Koo and Miner, 2010). When training adults, it is necessary to keep in mind adults (Koo and Miner, 2010; Kenefick et al., 2014): Are active learners Are reflective learners Need to know why they are learning Need to know what the goal is Need to know whether they can achieve the goal or not Generally favor short, self-paced, asynchronous, non-degree continuing education programs Are less confident using online chat rooms, discussion boards, or video technology These learning modules can be program specific or offered to an entire agency. Improvements in performance based on trainings can be monitored through employee performance reviews and achievement of yearly goals and objectives (Turnock, 2003). However, it is important to note that a gap in competencies may be concerning technology and individuals my need to be trained in using technology to advance knowledge and skills before computers and web-based courses can serve as training methods for public health workers. 3.3 THE IMPORTANCE OF INVESTING IN THE PUBLIC HEALTH WORKFORCE Workforce development mostly focuses on investing in the current public health workforce, but it is also important to discuss how future public health professionals are trained and prepared for their future careers. Today schools of public health have the ability to become accredited, by the 17 Council on Education for Public Health. Students at accredited schools of public health receive an education that meets a certain number of established standards. Students who have attended an accredited school have the opportunity to become certified in public health. Since the first exam in 2008, students can become certified to demonstrate they are competent and have mastered the public health skills necessary to improve the health and well-being of the community in which they serve (National Board of Public Health Examiners , 2014). However, until the establishment of the certification, standards were not available to assess the competencies of the public health workforce, including those who have masters in public health. Investing in the workforce, through training and professional development, must become accepted by all public health professionals, and must be incorporated into budgets and strategic directions of not only health departments, but all public health agencies. The public health workforce “is the backbone of the public health infrastructure, critical to the success of public health programs, and requires immediate intervention to improve capacity to deliver essential public health services” (Beck et al, 2012). It is essential that trainings are evaluated to determine if the trainings provided are sufficiently improving the knowledge and skills of the public health workforce (Freedman et al., 2014). 18 4.0 METHODS The Allegheny County Health Department set out to develop a self-assessment for employees of the health department. This process consisted of 5 steps: (1) development of survey, (2) determination of methods of analysis, (3) administration of survey, (4) analysis of survey responses, and (5) determination of health department priorities. 4.1 DEVELOPMENT OF SURVEY The Allegheny County Health Department sought guidance from the Public Health Foundation (PHF) in the determination of survey questions. The PHF is “a private, non-profit, 501(c)3 organization based in Washington, DC, improves the public’s health by strengthening the quality and performance of public health practice” (Public Health Foundation, 2014a). The PHF has worked with community partners to develop tools for workforce development and training needs of local and state health departments. The PHF has recommended assessing the workforce at three tier levels (Public Health Foundation, 2014d): “Tier 1 – Front Line Staff/Entry Level. Tier 1 competencies apply to public health professionals who carry out the day-to-day tasks of public health organizations and are not in management positions. Responsibilities of 19 these professionals may include data collection and analysis, fieldwork, program planning, outreach, communications, customer service, and program support. Tier 2 – Program Management/Supervisory Level. Tier 2 competencies apply to public health professionals in program management or supervisory roles. Responsibilities of these professionals may include developing, implementing, and evaluating programs; supervising staff; establishing and maintaining community partnerships; managing timelines and work plans; making policy recommendations; and providing technical expertise. Tier 3 – Senior Management/Executive Level. Tier 3 competencies apply to public health professionals at a senior management level and to leaders of public health organizations. These professionals typically have staff who report to them and may be responsible for overseeing major programs or operations of the organization, setting a strategy and vision for the organization, creating a culture of quality within the organization, and working with the community to improve health.” In collaboration with University of North Carolina and their already existing set of competencies, the PHF developed a 74-question survey that assesses competencies of health department staff (Public Health Foundation, 2012). The survey assesses eight domains and approximately 68 competencies. According to the PHF, the core competencies “represent a set of skills desirable 20 for the broad practice of public health that professionals may want to possess as they work to protect and improve the nation's health” (Public Health Foundation, 2014b). The eight domains addressed in the survey are (Public Health Foundation, 2014c): 1. 2. 3. 4. 5. 6. 7. 8. Analytical/Assessment Skills Policy Development/Program Planning Skills Communication Skills Cultural Competency Skills Community Dimensions of Practice Skills Public Health Sciences Skills Financial Planning and Management Skills Leadership and Systems Thinking Skills Questions from the PHF were adapted to better meet the needs of the health department, a practice that is encouraged by the PHF. Questions were simplified and combined to shorten the survey and to make the survey more relevant to the job duties of health department employees. The final survey addressed all eight competencies and consisted of 36 questions (32 of which addressed the sub-competencies). The questions can be reviewed in Appendix B. This essay addresses the Tier 1 assessment only. Tier 1 assessment is inclusive of all employees in the health department. After completion of training determination for Tier 1, Tier 2, and Tier 3 questions will be developed. The Allegheny County Health Department used the 2012 version of the core competencies questions. An updated version was published in 2014 after the start of the project. 21 4.2 DETERMINATION OF METHODS OF ANALYSIS The Allegheny County Health Department contacted the PHF to determine the best methods of analysis for the survey. It was determined that the health department would base the analysis on the 3-Step Competency Prioritization Sequence (Public Health Foundation, n.d.). Excel was determined to be the best method for sorting data and determining averages of competencies. 4.3 ADMINISTRATION OF SURVEY Survey Monkey was determined to be the platform to administer the survey. The survey was sent via email to the 348 employees of the health department on June 30, 2014. Follow up emails were sent as reminders to complete the survey. 39 individuals at the health department do not have email addresses or access to the internet during their workday and were provided with a paper copy of the survey. The initial deadline for completion was July 18, 2014. The survey was kept open until August 1, 2014, at which time data were exported for analysis. Employees completed 32 questions of the self-assessment using the following sale. 1= None (I am unaware, or have very little knowledge of the item) 2= Aware (I have heard of it; limited knowledge and/or ability to apply the skill) 3= Knowledgeable (I am comfortable with knowledge or ability to apply the skill) 4= Proficient (I am very comfortable, an expert; could teach this to others) 22 4.4 ANALYSIS OF SURVEY RESPONSES 332 (95.4%) employees responded (5 incomplete responses, 39 manual entries, 293 online responses). 16 employees did not respond to the survey at the time of analysis. Data were exported into excel using the Survey Monkey analysis tool. The data exported included overall question responses and unidentifiable individual responses. Survey Monkey provided averages for each question and for the data broken out by program and duty. Data were manually analyzed to determine bureau averages. This process included sorting data by program and then each program to its respective bureau. Overall domain averages were also completed by hand through a process recommended by the PHF. The following figure outlines how the data were analyzed. Figure 5: Analysis of training needs assessment survey data breakdown 23 Table 3 indicates the average responses for each of the 8 domains. These data were then used to help determine priorities, discussed later in this section. Table 3: Training needs assessment survey average domain response Data were analyzed overall (Appendix C), as well as by program, by bureau, and by job duty for a comprehensive understanding of the competencies of the health department. Individual question averages were analyzed for contradicting answers and notable responses. Table 4 below describes these findings. 24 Table 4: Training needs assessment survey question findings 4.5 DETERMINATION OF TRAINING PRIORITIES Data were presented to the Director of the health department (Dr. Karen Hacker, MD MPH) and the four Deputy Directors: LuAnn Brink, PhD Roderick Harris DrPH., James Thompson, and Ronald Sugar Esq. Data provided a snapshot of the competencies of each bureau and program within the bureau. Deputy Directors were asked to determine their top three priorities for the health department based on the self-assessment data and the health department’s strategic direction. The Allegheny County Health Department used the general guidelines from the 3-Step 25 Competency Prioritization Sequence from the PHF (Public Health Foundation, n.d.) but adapted it to fit the needs of the health department. Figures 6 and 7 show the current gaps. Domain Averages: Analytical/Assessment Skills: 2.54 Policy Development/Program Planning Skills: 2.73 Communication Skills: 2.72 Cultural Competency Skills: 2.77 Community Dimensions of Practice Skills: 2.48 Public Health Science Skills: 2.41 Financial Planning and Management Skills: 2.50 Leadership and Systems Thinking Skills: 2.62 Figure 6: Training needs assessment survey average domain response Figure 7: Training needs assessment survey average domain response 26 The deputy directors are working to determine priorities for the upcoming year. These priorities will be based on the results of the self-assessment, the health department’s strategic plan, and gaps the deputy’s identified within their department. Some trainings will be offered department wide, while others may only be offered to those programs that have a particular training need. Addressing the gaps and priorities, the Allegheny County Health Department will be able to better achieve the Ten Essential Public Health Services. The Ten Essential Services of Public Health, listed below, aim to achieve the core functions of public health: assessment, assurance, and policy development (Centers for Disease Control and Prevention, 2014b). 1. 2. 3. 4. 5. 6. 7. Monitor health status to identify and solve community health problems. Diagnose and investigate health problems and health hazards in the community. Inform, educate, and empower people about health issues. Mobilize community partnerships and action to identify and solve health problems. Develop policies and plans that support individual and community health efforts. Enforce laws and regulations that protect health and ensure safety. Link people to needed personal health services and assure the provision of health care when otherwise unavailable. 8. Assure competent public and personal health care workforce. 9. Evaluate effectiveness, accessibility, and quality of personal and population-based health services. 10. Research for new insights and innovative solutions to health problems. The Centers for Disease Control and Prevention, to better illustrate these functions, has created a wheel depicting the ten essential services, see Figure 8. 27 (Source: The Centers for Disease Control and Prevention, 2014b) Figure 8: Ten Essential Services of Public Health The idea is that through addressing the gaps in competencies of the public health workforce at Allegheny County Health Department, the health department is better prepared to deliver these essential services to the community in which it serves. See Appendix D for an overview of how the core competency self-assessment addresses all Ten of the Essential Services of Public Health. 4.6 NEXT STEPS Based on the priorities determined by the deputy directors, the health department will use the PHF TRAIN tool to provide online trainings to health department employees. The Allegheny County Health Department has become a Course Provider, and will upload trainings and use existing training to improve workforce competencies. See Appendix E for a screen shot of the TRAIN tool. Upon determination of the training recommendations for the workforce, Tiers 2 and 28 3 will be surveyed to determine additional training needs for higher-level staff. A workforce development plan will then be completed for the accreditation process. 29 5.0 RECOMMENDATIONS The self-assessment helped to determine the staff’s competencies and training needs. This section provides guidance on potential trainings for Allegheny County Health Department employees. However, training recommendations are not solely based on the wants and needs of the staff, but also dependent on the strategic direction of the health department. The deputy directors have their own opinions and recommendations for trainings. In this section, recommendations will be provided solely based on the self-assessment. The eight domains were ranked from one to eight based on the average self-assessment score. 1. Public Health Science Skills: 2.41 2. Community Dimensions of Practice Skills: 2.48 3. Financial Planning and Management Skills: 2.50 4. Analytical/Assessment Skills: 2.54 5. Leadership and Systems Thinking Skills: 2.62 6. Communication Skills: 2.72 7. Policy Development/Program Planning Skills: 2.73 8. Cultural Competency Skills: 2.77 The narrow range of average scores indicates that individual questions should be analyzed to determine priorities. Determination of priorities were based on the following findings when data were analyzed (Table 4): 1. While staff have an awareness of how policy can influence public health, their ability to apply it to their work is limited. 2. Overall the department has a limited ability to describe the role of governmental and nongovernmental organizations in the delivery of public health services. 3. As a department we are aware of the importance of communicating clearly and with cultural understanding, but we report limited ability to apply this skill. 30 4. There is awareness of the importance of identifying stakeholders and assets; the ability to incorporate them into their work is limited. Although there are eight domains that the training needs assessment addressed, the three priorities recommended for training are: 1. Public Health Policy (both within government organizations and non-government organizations) 2. Cultural Competency (both within the organization and when working with the community) 3. Identification of Stakeholders These three priorities can be addressed and offered department wide and are not trainings specific to a bureau or program, although examples may vary depending on audience of training. 5.1 PUBLIC HEALTH POLICY 5.1.1 Reason to Address The Centers for Disease Control and Prevention define a policy “as a law, regulation, procedure, administrative action, incentive, or voluntary practice of governments and other institutions” (The Centers for Disease Control and Prevention , 2013). According to the World Health Organization, health policy “refers to decisions, plans, and actions that are undertaken to achieve specific health care goals within a society (World Health Organization, 2014).” Policies within the context of public health aim to: “define a vision for the future which in turn helps to establish targets and points of reference for the short and medium term” (World Health Organization , 2014) improve health, through limiting unhealthy behaviors and promoting healthy behaviors create sustainable change 31 It is important that individuals within a health department not only understand organization policy, but also public health policy within the county, state, and at the federal level. This includes an understanding of public health law and the precedents that allow the staff to perform their everyday duties. In addition to understanding how policy impacts their jobs, it is necessary that employees understand how implementing policy within the county can improve the health of its residents. With budget constraints and limits to program resources available to health department employees, policy change (if feasible) to promote health and behavior change is viewed as an intervention that will not only be sustainable, but impact a large number of individuals. 5.1.2 Recommended Trainings The following trainings are currently available on the TRAIN website as options for staff of the health department to participate in (under the search term “policy”) (Public Health Foundation, n.d.b): Public Health Policy and Advocacy Applying Performance Measurement to Policy Activities Engaging Communities in Public Health Research, Practice and Policy The Intersections of Cultural Diversity, Health Policy Development and Policy Analysis Making Data, Policy and Politics Work for Public Health The Role and Use of Evidence in Policy Using Evidence-Based Health Framework to Move Policy Forward 32 5.2 CULTURAL COMPETENCY 5.2.1 Reason to Address The goal of cultural competence is “to create a health care system and workforce that are capable of delivering the highest-quality care to every patient regardless of race, ethnicity, culture, or language proficiency” (Betancourt et al., 2005). According to the National Institutes of Health, “cultural competency is critical to reducing health disparities and improving access to highquality health care, health care that is respectful of and responsive to the needs of diverse patients” (National Institutes of Health, 2014). Understanding cultural competency is important because individuals have a broad range of knowledge and opinions regarding health, which is influenced “by their social or cultural backgrounds (Betancourt et al., 2005). Through trainings in cultural competency, staff are able to better understand their co-workers as well as the needs of the population they serve. Understanding differences among a diverse set of community members, the health department will better serve the community and more effectively implement programs. The Commonwealth Fund identify the following as barriers to culturally competent care (Betancourt, 2002): “Lack of diversity in health care’s leadership and workforce. Systems of care poorly designed to meet the needs of diverse patient populations. Poor communication between providers and patients of different racial, ethnic, or cultural backgrounds.” Current programs that address diverse populations include: Women, Infants, and Children Maternal Child Health Dental TB 33 Infectious Disease STD Housing Preparedness AmeriCorps 5.2.2 Recommended Trainings The following trainings are currently available on the TRAIN website as options for staff of the health department to participate in (under the search term “cultural competency”) (Public Health Foundation, n.d.a): Cultural Competency and Disaster Mental Health Introduction to Cultural Competency and Title VI Cultural Competency for Community Management of Special Needs Patients in Disaster Diversity and Cultural Competency in Public Health Settings- Basic Level Cultural Diversity, Health Disparities and Public Health Exploring Cross Cultural Communication Practicing Cross Cultural Communication- Community Health Worker Program Public Health Accreditation & Competency Based Learning: A Model Based on the TRAIN Learning Management System Alternatives to a required online module for health department staff is an in person cultural competency training during a staff meeting. An expert within the field of cultural competency from the county, The University of Pittsburgh, or another organization within Allegheny County, can be contracted to provide cultural competency training and workshops to help staff better understand and work with diverse populations within Allegheny County. Supplemental cultural competency trainings can be offered to staff in individual programs that work with specific populations on a regular basis, such as WIC or maternal child health program staff. 34 5.3 IDENTIFICATION OF STAKEHOLDERS 5.3.1 Reason to Address Public health agencies do not have the resources or the expertise to provide public health services to the community on their own. For this reason it is necessary to engage with stakeholders. A stakeholder is a group or individuals who have an interest in a public health decision or program, and has a unique perspective or opinion regarding this decision or program. According to Longest and Rohrer, communication with stakeholders assists in carrying out the health department’s mission and provides resources that allow for programs and efforts to be sustainable within the county (Longest and Rohrer, 2005). Stakeholders will vary based on intervention or program the health department is focusing on. It is essential that individuals at the Allegheny County Health Department be able to identify organizations within Allegheny County and the region to assist in their public health efforts. Program heads may have an idea or concept for an intervention that will improve the population’s health but it may not be successfully implemented without the assistance of others within the community. The Centers for Disease Control and Prevention indicate that stakeholders fall into three categories: those affected by the intervention, those involved in the operation of the intervention, and those involved in the evaluation of the intervention (Centers for Disease Control and Prevention, n.d.). They list the following as potential stakeholders in public health efforts(Centers for Disease Control and Prevention, n.d.): 35 Program managers and staff Local, state, and regional coalitions interested in the public health issue Local grantees of your funds Local and national advocacy partners Other funding agencies, such as national and state governments State or local health departments and health commissioners State education agencies, schools, and other educational groups Universities and educational institutions Local government, state legislators, and state governors Privately owned businesses and business associations Health care systems and the medical community Religious organizations Community organizations Private citizens Program critics Representatives of populations disproportionately affected by the problem Law enforcement representatives 5.3.2 Recommended Trainings The following trainings are currently available on the TRAIN website as options for staff of the health department to participate in (under the search term “stakeholders”) (Public Health Foundation, n.d.c): Introduction to Program Monitoring and Evaluation in Maternal and Child Health: Session One- Monitoring & Evaluation: What? When? Who? Community Toolbox Module 1: Assuring Engagement in Community Health Improvement Efforts Effective Leadership for Healthy Communities: Concepts, Collaborations and Case Studies Beyond the Affordable Care Act: The Next Frontiers for US Health Reform Some of these trainings are general, while others are specific to a program or intervention. These trainings can be used as is or adapted by health department staff to better meet the training needs of employees. It is recommended that trainings also provide examples of stakeholders within the county and current organizations with in which the health department already collaborates. It is 36 recommended that all staff within the health department receive a general training on engaging stakeholders and receive additional program specific training, if necessary. The goal of training the health department staff on the importance of community stakeholders and potential stakeholders within the county is to better achieve the ten essential services of public health. If a workforce at the health department understands the importance of stakeholder involvement and understands how successes of programs depend on involvement of stakeholders, they may be more willing to engage them. With cuts in funding to public health, it is important now more than ever to involve stakeholders that can provide resources to the health department for successful implementation of programs and provide guidance on the most effective allocation of limited resources. The health department alone cannot achieve improvements in the public’s health. 37 6.0 CONCLUSION Local health departments within the United States function to achieve the ten essential services of public health. With cuts in funding and a reduction in health department staff, a competent and efficient workforce is needed to provide the services necessary for population health. Accreditation attempts to hold health departments to standards necessary for optimal performance. Through addressing domain 8 of accreditation, maintain a competent public health workforce, Allegheny County Health Department is working to better prepare its workforce for current and future public health issues. Few current employees have formal public health training and through self-assessment have determined that there is room for improvement in their public health competencies. It is necessary that the Allegheny County Health Department better prepare its workforce to address public health issues and should focus on training staff in public health policy, cultural competency, and identification of stakeholders. These trainings will align with the health department’s strategic direction and will ensure that the health of the 1.2 million individuals the Allegheny County Health Department serves improves not only now but for future years to come. 38 APPENDIX A: ORGANIZATIONAL STRUCTURE OF ALLEGHENY COUNTY HEALTH DEPARTMENT 39 Figure 9. Allegheny County Health Department Organizational Structure 40 APPENDIX B: ALLEGHENY COUNTY HEALTH DEPARTMENT TRAINING NEEDS ASSESSMENT SURVEY QUESTIONS 41 42 43 44 45 46 47 48 49 50 51 52 53 APPENDIX C: ALLEGHENY COUNTY HEALTH DEPARTMENT TRAINING NEEDS ASSESSMENT SURVEY SUMMARY OF DATA ANALYSIS Domain 1: Analytical/Assessment Skills Question Describe a community's overall level of health and the factors that affect community health (e.g. quality, availability of health services, economic circumstances, environment) Identify sources of reliable public health data and information Use information technology (e.g. computers, data bases) and other appropriate tools to collect, store, and use data and information Describe the use of data that measure public health conditions Collect, use, and share data and information in an ethical manner Overall 2.40 2.43 2.84 2.28 2.74 Domain 2: Policy Development/Program Planning Skills Question Gather information that can be used for policy decisions in your program (e.g. health information, fiscal information) Understand laws, regulations, and policies relevant to your work at the health department (e.g. HIPAA) Describe how policy can influence public health programs (e.g. funding, legal regulations) Identify ways to improve the quality and effectiveness of your work Overall 2.57 3.01 2.42 2.92 Domain 3: Communication Skills Question Identify the health literacy (understanding of health-related terms) of the populations your program serves Communicate clearly and with cultural understanding in writing, speaking, and through other formats (e.g. community presentations, webinars) Use good communication skills with individuals and within groups (e.g conflict resolution, active listening, risk communication) 54 Overall 2.55 2.64 2.96 Domain 4: Cultural Competency Skills Question Recognize that cultural, social, and behavioral factors impact how people access and use public health services Describe the need for a diverse public health workforce Work to interact effectively with persons from diverse backgrounds (e.g. cultural, socioeconomic, educational, racial, gender, age, ethnic, sexual orientation, professional, religious affiliation, mental and physical capabilities) Respond to the diverse needs that might result from cultural differences Overall 2.76 2.67 2.94 2.70 Domain 5: Community Dimensions of Practice Skills Question Identify stakeholders (people or organizations) and community assets that can help your program Collaborate with the community and encourage community involvement within your program Describe the role of governmental and non-governmental organizations in the delivery of public health services Inform the population your program serves about policies, programs, and resources Overall 2.36 2.46 2.34 2.76 Domain 6: Public Health Science Skills Question Explain the role each of the following play in the field of public: Biostatistics Epidemiology Environmental health Health services administration Social and behavioral health sciences Recognize the Core Public Health Functions and the Ten Essential Services of Public Health Follow laws and procedures for the ethical conduct of research (e.g. HIPAA) Overall 2.15 2.29 2.63 2.37 2.31 2.29 2.83 Domain 7: Financial Planning and Management Skills Question Describe the roles of local, state, and federal public health agencies Follow all Allegheny County Health Department policies Identify potential funding sources (e.g. grants) that can help your program deliver services Prioritize tasks in order to operate within your program's budget Use feedback (individual and program) to improve performance Report program performance Overall 2.42 2.95 2.02 2.45 2.71 2.43 Domain 8: Leadership and Systems Thinking Skills Question Recognize factors (both within and outside the health department) that affect the delivery of the Ten Essential Services of Public Health Interact in a professional manner with organizations, communities, and individuals Describe how public health operates within a larger social, political, and economic environment Participate in trainings and educational opportunities for personal and professional development 55 Overall 2.15 3.09 2.38 2.88 APPENDIX D: ALLEGHENY COUNTY HEALTH DEPARTMENT TRAINING NEEDS ASSESSMENT SURVEY AND THE TEN ESSENTIAL SERVICES OF PUBLIC HEALTH Adapted from the Indiana Public Health Workforce Development Education & Training Toolkit (Indiana Public Health , n.d.). 56 57 58 59 APPENDIX E: SCREENSHOT OF TRAIN TOOL 60 BIBLIOGRAPHY Allegheny County Health Department. (2013). Board of Health. Retrieved from http://www.achd.net/board/index.html Allegheny County Health Department. (2014). Welcome to the Allegheny County Health Department Website! Retrieved from http://www.achd.net/admin/dir-office.html Allegheny County Pennsylvania. (n.d.). Inception of Allegheny County. Retrieved from http://www.alleghenycounty.us/about/inception.aspx Beck, A.J., et al. (2012). Building an Effective Workforce: A Systematic Review of Public Health Workforce Literature. American Journal of Preventive Medicine, 42(5s1): s6-s16. Betancourt, J.R. (2002). Cultural Competence In Health Care: Emerging Frameworks And Practical Approaches. Retrieved from http://www.commonwealthfund.org/usr_doc/betancourt_culturalcompetence_576.pdf Betancourt, J.R. et al. (2005). Cultural Competence and Health Care Disparities: Key Perspectives and Trends. Health Affairs, 24(2): 499-505. Centers for Disease Control and Prevention. (2010). National Voluntary Accreditation for Public Health Departments: Benefits & Impacts of Accreditation. Retrieved from http://www.cdc.gov/stltpublichealth/accreditation/benefits.html Centers for Disease Control and Prevention. (2013). National Voluntary Accreditation for Public Health Departments. Retrieved from http://www.cdc.gov/stltpublichealth/hop/pdfs/NVAPH_Factsheet.pdf Centers for Disease Control and Prevention. (2013). Public Health Policy. Retrieved from http://www.cdc.gov/stltpublichealth/policy/ Centers for Disease Control and Prevention. (2014a). National Voluntary Accreditation for Public Health Departments. Retrieved from http://www.cdc.gov/stltpublichealth/accreditation/ 61 Centers for Disease Control and Prevention. (2014b). The Public Health System and the Ten Essential Public Health Services. Retrieved from http://www.cdc.gov/nphpsp/essentialservices.html Centers for Disease Control and Prevention. (n.d.). Introduction to Evaluation for Public Health Programs. Retrieved from http://www.cdc.gov/getsmart/program-planner/step1.pdf Freedman, A.M. et al. (2014). Public Health Training Center Evaluation: A Framework for Using Logic Models to Improve Practice and Educate the Public Health Workforce. Health Promotion Practice, 15: 80s-88s. Gebbie, K.M., Turnock, B.J. (2006). The Public Health Workforce, 2006: New Challenges. Health Affairs, 25 (4): 923-933. Indiana Public Health. (n.d.). Indiana Public Health Workforce Development Education & Training Toolkit. Retrieved from http://www.in.gov/isdh/files/24_Appendix1.pdf Kaufman, N.J., et al. (2014). Thinking Beyond Silos: Emerging Priorities in Workforce Development for State and Local Government Public Health Agencies. Journal of Public Health Management Practice, 00:1-9. Kenefick, H.W., et al. (2014). On Your Time: Online Training for the Public Health Workforce. Health Promotion Practice, 15: 48s-55s. Koo, D., Miner, K. (2010). Outcome-Based Workforce Development and Education in Public Health. Annual Review of Public Health, 31: 253-269. Local Health Administration Law, Act 315. 16 P.S. § 12001 et seq (1995) Longest, B.B. & Rohrer, W.M. (2005). Communication Between Public Health Agencies and Their External Stakeholders. Journal of Health and Human Services Administration, 28(2): 189-217. Meyer, J., & Weiselberg, L. (prepared by). (2009). County and City Health Departments: The Need for Sustainable Funding and the Potential Effect of Health Care Reform on their Operations. Health Management Associates, 1-29. Miner, K., Allan, S. (2014). Future of Public Workforce Training: Thought Leaders’ Perspectives. Health Promotion Practice, 15: 10s-13s. Millery, M., et al. (2014). Using Innovative Instructional Technology to Meet Training Needs in Public Health: A Design Process. Health Promotion Practice, 15: 39s-47s. National Association of County and City Health Officials. (2014). 2013 National Profile of Local Health Departments. Retrieved from http://www.naccho.org/topics/infrastructure/profile/upload/2013-National-Profile-ofLocal-Health-Departments-report.pdf 62 National Board of Public Health Examiners. (2014). About the CPH. Retrieved from https://www.nbphe.org/aboutthecph.cfm National Institutes of Health. (2014). Cultural Competency. Retrieved from http://www.nih.gov/clearcommunication/culturalcompetency.html Pennsylvania Department of Health. (2013). County Municipal Health Departments & Act 315/Act 12. Retrieved from http://www.portal.state.pa.us/portal/server.pt/community/communities/14133/cmhd___act _315_page/556748 Pennsylvania Department of Transportation. (2014). Pennsylvania County Type 10 Maps in PDF Format. Retrieved from http://www.dot.state.pa.us/Internet/Bureaus/pdPlanRes.nsf/infoBPRCartoCountyType10 Public Health Accreditation Board. (2013a). Accredited Health Departments. Retrieved from http://www.phaboard.org/news-room/accredited-health-departments/ Public Health Accreditation Board. (2013b). Accreditation Overview. http://www.phaboard.org/accreditation-overview/ Public Health Accreditation Board. (2013c). Public Health Accreditation Board Standards & Measures. Retrieved from http://www.phaboard.org/wp-content/uploads/SM-Version-1.5Board-adopted-FINAL-01-24-2014.docx.pdf Public Health Accreditation Board. (2014). The Seven Steps of Public Health Department Accreditation. Retrieved from http://www.phaboard.org/accreditation-process/sevensteps-of-public-healthaccreditation/ Public Health Foundation. (2012). Competency Assessment: Tier 3 Public Health Professionals. Retrieved from http://www.phf.org/resourcestools/Documents/Competency_Assessment_Tier3_2012Jan.p df Public Health Foundation. (2014a) About PHF. Retrieved from http://www.phf.org/AboutUs/Pages/default.aspx Public Health Foundation. (2014b). Competency Assessments for Public Health Professionals. Retrieved from http://www.phf.org/resourcestools/Pages/Competency_Assessments_For_Public_Health_ Professionals.aspx 63 Public Health Foundation. (2014c). Core Competencies for Public Health Professionals: Domains. Retrieved from http://www.phf.org/programs/corecompetencies/Pages/Core_Competencies_Domains.asp x Public Health Foundation. (2014d) Core Competencies for Public Health Professionals: Tiers. Retrieved from http://www.phf.org/programs/corecompetencies/Pages/COL_CorePublicHealthCompetenc ies_Guidance_Definitions.aspx Public Health Foundation. (n.d.). 3-Step Competency Prioritization Sequence. Retrieved from http://www.phf.org/resourcestools/Documents/3Step_Competency_Prioritization_Sequence.pdf Public Health Foundation. (n.d.a). TRAIN National. Retrieved from https://www.train.org/DesktopShell.aspx?tabId=62&goto=browse&browse=keyword&ke yword=cultural+competency&keyoption=Both&clinical=Both&local=All&ByCost=0 Public Health Foundation. (n.d.b). TRAIN National. Retrieved from https://www.train.org/DesktopShell.aspx?tabId=62&goto=browse&browse=keyword&ke yword=policy&keyoption=Both&clinical=Both&local=All&ByCost=0 Public Health Foundation. (n.d.c). TRAIN National. Retrieved from https://www.train.org/DesktopShell.aspx?tabId=62&goto=browse&browse=keyword&ke yword=stakeholders&keyoption=Both&clinical=Both&local=All&ByCost=0 Salinsky, E. (consultant). (2010). Governmental Public Health: An Overview of State and Local Public Health Agencies. Retrieved from http://www.nhpf.org/library/backgroundpapers/BP77_GovPublicHealth_08-18-2010.pdf Turnock, B.J. (2003). Roadmap for Public Health Workforce Preparedness. Journal of Public Health Management and Practice, 9(6): 471-480. Tilson, H., Gebbie, K.M. (2004). The Public Health Workforce. Annual Review of Public Health, 25: 341-356. United States Census Bureau. (2014). State & County Quick Facts: Allegheny County, Pennsylvania. Retrieved from http://quickfacts.census.gov/qfd/states/42/42003.html United States Census Bureau: American FactFinder. (2014). Community Facts. Retrieved from http://factfinder2.census.gov/faces/nav/jsf/pages/community_facts.xhtml World Health Organization. (2014). Health Policy. Retrieved from http://www.who.int/topics/health_policy/en/ 64