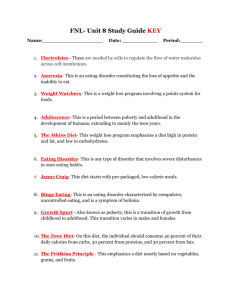
The Genetics of Obesity and Eating Disorders School
advertisement

THE GENETICS OF OBESITY AND EATING DISORDERS GENETICS OF NUTIRENT CONSUMPTION AND AN EVOLUTIONARY PERSPECTIVE OF EATING DISORDERS By ALEXANDRA JEAN MAYHEW, B.A.SC A Thesis submitted to the School of Graduate studies in partial fulfilment of the requirements for the degree Master of Science McMaster University © Copyright by Alexandra Jean Mayhew, July 2014 McMaster University MASTER OF SCIENCE (2014) Hamilton, Ontario (Health Research Methodology) TITLE: Genetics of Nutrient Consumption and an Evolutionary Perspective of Eating Disorders AUTHOR: Alexandra Jean Mayhew, B.A.Sc (University of Guelph) SUPERVISOR: Dr. David Meyre NUMBER OF PAGES: 146 ii ABSTRACT GENETICS OF NUTRIENT CONSUMPTION AND AN EVOLUTIONARY PERSPECTIVE OF EATING DISORDERS Alexandra Jean Mayhew McMaster University, 2014 Advisor: Dr. David Meyre Committee Member: Dr. Sonia Anand Committee Member: Dr. Andrew Mente Obesity prevalence continues to increase worldwide, yet few safe and effective treatment options are available suggesting there needs to be a greater emphasis on preventing rather than treating obesity. This research investigated the association of obesity predisposing SNPs and a gene score with nutrient consumption patterns including total energy intake and macronutrient distribution in a European ancestry population as well as discussing an evolutionary perspective on eating disorders using current epidemiological evidence to identify genes which may be involved. The association of two of the 14 obesity predisposing SNPs and the gene score with BMI was confirmed in the EpiDREAM population. Novel associations between two SNPs located in or near BDNF (rs6265 and rs1401635) were found with total fat, MUFA, and PUFA intake. Rs1401635 was also associated with total energy and trans fat intake. Novel associations of rs6235 (PCSK1) and the gene score were found with total energy intake. The novel associations found indicate that food related behaviours are one of the mechanisms of action through which obesity predisposing SNPs cause obesity and therefore warrant further investigation. The lack of association among all genes and the modest association of the gene score show that mechanisms other than food consumption are important. The investigation of the evolutionary history of eating disorders revealed that the adapted to flee famine hypothesis is a plausible theory explaining anorexia nervosa while the thrifty genotype hypothesis provides a possible explanation for bulimia nervosa and binge eating disorder. These evolutionary theories can be applied to identify new candidate genes as well as phenotypic traits to investigate to better understand the genetic architecture of eating disorders. Understanding genes associated with disordered eating patterns may highlight future areas for obesity prevention. Key words: obesity, polygenic obesity, BMI, SNP, gene score, energy intake, macronutrient, eating disorders, anorexia nervosa, bulimia nervosa, binge eating disorder, thrifty genotype hypothesis, adapted to flee famine hypothesis. iii ACKNOWLEDGEMENTS I would like to begin by thanking my advisor, Dr. David Meyre for his continued support and guidance throughout the duration of my Masters. His passion for understanding the genetics of obesity, dedication to his students, and willingness to teach made this thesis a reality. My research also benefited greatly from my committee members Drs. Sonia Anand and Andrew Mente who provided exceptional suggestions for improving this thesis. A special thank you goes out to my peers and additional mentors, Russell de Souza, Aihua Li, and Sébastien Robiou-du-Pont, who played important roles in developing my skills and understanding. I thank my parents, John and Rose Mayhew for encouraging me from day one to pursue a career in academia and providing support in countless ways over the many years of school. I thank my friends Lindsay Morris, Claudia Chan, Jill Patrick, Victor and Tori Da Silva Sa, Allison Davis, Chris Bonanno, Florence Wilson, Ray Flores, Matt and Julia Stoop, and Nicole Seymour for boosting my spirits when overwhelmed and for their continued friendship. Lastly, I thank my partner Alexander Jensen for providing the support necessary to push forward during the most challenging times through his endless patience and unwavering belief in my abilities. iv TABLE OF CONTENTS Title Page…………………………………………………………………………………..i Descriptive note…………………………………………………………………………...ii Abstract…………………………………………………………………………………...iii Acknowledgements……………………………………………………………………….iv Table of contents…………………………………………………………………………..v List of figures and tables………………………………………………………………..viii List of abbreviations……………………………………………………………………...xi Declaration of academic achievement…………………………………………………...xii 1.0 Introduction .............................................................................................................. 1 2.0 Literature Review..................................................................................................... 4 2.1 Heritability of obesity ............................................................................................... 4 2.2 Heritability of eating characteristics ......................................................................... 7 2.2.1 Energy consumption and macronutrient distribution ......................................... 7 2.2.2 Food consumption patterns ................................................................................ 9 2.2.3 Food consumption behaviours ......................................................................... 10 2.2.4 Conclusions ...................................................................................................... 12 2.3 Current state of knowledge of the genetics of obesity ............................................ 13 2.3.1 Monogenic obesity ........................................................................................... 13 2.3.2 Polygenic forms of obesity .............................................................................. 16 2.4 Current state of knowledge of the genetics of eating behaviour ............................. 20 2.5 Background of eating disorders .............................................................................. 23 2.5.1 Diagnostic criteria ............................................................................................ 23 2.5.2 Symptoms, comorbidities, and mortality of eating disorders .......................... 24 2.5.3 Treatment ......................................................................................................... 25 2.5.4 Risk factors for eating disorders ...................................................................... 27 2.6 Heritability of eating disorders ............................................................................... 39 2.7 Genetics of eating disorders .................................................................................... 40 v 2.7.1 Serotonin .......................................................................................................... 41 2.7.2 Catecholamine pathway ................................................................................... 44 2.7.3 Norephinephrine .............................................................................................. 47 2.7.4 Neuropeptides and Feed Regulations............................................................... 48 2.7.5 Summary .......................................................................................................... 55 3.0 Justification and Objectives ........................................................................................ 56 4.0 The Association of Obesity SNPs with Food Consumption Patterns ......................... 59 4.1 Introduction ............................................................................................................. 59 4.2 Methods................................................................................................................... 62 4.2.1 Participants ....................................................................................................... 62 4.2.2 Phenotyping ..................................................................................................... 64 4.2.3 Genotyping ....................................................................................................... 64 4.2.4 Statistical methods ........................................................................................... 65 4.3 Results ..................................................................................................................... 68 4.3.1 Association of obesity predisposing SNPs and genotype score with BMI ...... 70 4.3.2 Association of obesity predisposing SNPs and genotype score with dietary intake parameters ...................................................................................................... 73 4.4 Discussion ........................................................................................................... 73 4.5 Conclusions ............................................................................................................. 78 5.0 An Evolutionary Perspective on Eating Disorders ..................................................... 79 5.1 Introduction ............................................................................................................. 79 5.2 Suppression of reproduction and sexual competition ............................................. 79 5.3 Adapted to flee famine hypothesis and rogue hibernation...................................... 81 5.4 Thrifty gene hypothesis........................................................................................... 84 5.5 Summary of evolutionary theories .......................................................................... 89 5.6 Coexistence of Anorexia Nervosa and Bulimia Nervosa in binge/purge subtype Anorexia Nervosa ......................................................................................................... 92 5.6.1 Binge eating as protection against Anorexia Nervosa ..................................... 92 5.6.2 Accumulation of independent genes leading to binge eating and Anorexia Nervosa ..................................................................................................................... 93 5.6.3 Mutations/structural gene variants with opposite effects in the same gene lead to AN or BN .............................................................................................................. 94 vi 5.6.4 Mutations in nearby genes result in partial linkage disequilibrium of Anorexia Nervosa and binge eating traits ................................................................................. 95 5.6.5 Summary of the role of genetics in the coexistence of Anorexia Nervosa and Bulimia Nervosa in binge/purge subtype Anorexia Nervosa ................................... 96 5.7 Conclusions ............................................................................................................. 97 6.0 Ethical Considerations .............................................................................................. 100 7.0 Conclusions and Future Work .................................................................................. 103 8.0 References ................................................................................................................. 109 vii LIST OF FIGURES AND TABLES FIGURES Figure 1. The role of monogenic obesity genes in the melanocortin pathway………….15 Figure 2. EpiDREAM participant flow chart……………………………………………63 Figure 3. Statistical power for detecting associations between individual SNPs and BMI according to allele frequency and beta-coefficients with a sample size of 1,850 participants……………………………………………………………………………….67 Figure 4. Framework for the risk of developing an eating disorder based on genotypic category and presence or absence of pressure to be thin………………………………...99 TABLES Table 1. Gene symbols and proteins coded……………………………………………...14 Table 2. Genotypic information for obesity predisposing SNPs………………………...65 Table 3. EpiDREAM Participant Characteristics………………………………………..68 Table 4. Pearson correlations for unadjusted nutrient intakes....………………………...69 Table 5. Association of energy and energy adjusted nutrients with BMI……………….69 Table 6. The association of obesity predisposing SNPs with BMI and energy adjusted nutrients…………………………………………………………………………..71 viii LIST OF ABBREVIATIONS AND SYMBOLS 5-HIAA – 5-hydroxyindoleacetic acid 5-HT – Serotonin 5-HT2A – 5-hydroxytryptamine receptor 2A 5-HTTLPR – Serotonin-transporter-linked polymorphic region AFFH – Adapted to flee famine hypothesis AGRP – Agouti related peptide AN – Anorexia Nervosa AN(BP) – Anorexia Nervosa binge/purge subtype AN(R) – Anorexia Nervosa restrictive subtype BDNF – Brain-derived neurotrophic factor BED – Binge eating disorder BMI – Body mass index (kg/m2) BN – Bulimia nervosa CBT – Cognitive behaviour therapy COMT – catecholamine-O-methyltransferase CSF – Cerebrospinal fluid CVD – Cardiovascular disease D2 – Dopamine receptor 2 D3 – Dopamine receptor 3 D4 – Dopamine receptor 4 DAT1 – Dopamine transporter 1 DNA – Deoxyribonucleic acid DRD2 – Dopamine receptor 2D DRD3 – Dopamine receptor 3D DRD4 – Dopamine receptor 4D DSM – Diagnostic and Statistical Manual of Mental Disorders ix DZ – Dizygotic twins FFQ – Food frequency questionnaire FTO – Fat mass and obesity associated gene GWAS – Genome wide association study HEW – Hardy-Weinberg equilibrium HOXB5 – homebox protein HVA – Homovanillic acid IBC – ITMAT Broad Care KCTD14 – Potassium channel tetramerization domain containing 14 LEP – Leptin LEPR – Leptin receptor LOD – Logarithm of odds MAOA – Monoamine oxidase A MC3R – Melanocortin 3 receptor MC4R – Melanocortin 4 receptor MISTRA – Minnesota Study of Twins Reared Apart MRAP2 – Melanocortin 2 receptor accessory protein 2 MUFA – Monounsaturated fatty acid MZ – Monozygotic twins NEGR1 – Neuronal growth regulator 1 NET – Norepinephrine transporter NHLBI – National Heart, Lung, and Blood Institute NIMH – National Institute of Mental Health NMDAr – Glutamate receptor NPL – Nonparametric linkage NPY – Neuropeptide Y NSAL – National Survey of American Life NTRK2 – Neurotrophic tyrosine kinase receptor type 2 gene x OGTT – Oral glucose tolerance test OLFM4 – Olfactomedin OPRD1 – Opioid delta receptor PCSK1 – Prohormone convertase 1 PET – Positron emission tomography POMC - Proopiomelanocortin PUFA – Polyunsaturated fatty acid PVN – Paraventricular nucleus PYY – Peptide YY RCT – Randomized controlled trial RNA – Ribonucleic acid SH2B1 – SH2B adaptor protein 1 SHARE – Study of Health Assessment and Risk Evaluation SIM1 – Single-minded homolog 1 SNPs – Single nucleotide polymorphisms SPSS – Statistical Package for the Social Sciences TPH – Tryptophan hydroxylase xi DECLARATION OF ACADEMIC ACHIEVEMENT My supervisor Dr. David Meyre and myself developed the plans of analysis for the association of obesity predisposing SNPs with dietary consumption patterns with feedback from my committee members, Dr. Sonia Anand and Dr. Andrew Mente. The data used had previously been collected for the EpiDREAM study and the principle investigator, Dr. Hertzel Gerstein provided comments on the proposal. I performed the data cleaning and all statistical analysis for the project. Dr. Meyre and I conceptualized the paper on the evolutionary history of eating disorders together with all data collection and writing being performed by myself. xii M.Sc. Thesis – A. Mayhew; McMaster University – Health Research Methodology 1.0 Introduction Obesity is caused by a positive energy balance in which more calories are consumed than expended per day, leading to excessive fat accumulation in adipose tissue. Body mass index (BMI) is typically used to determine obesity at a population level. Using predetermined BMI categories, individuals under 18.5kg/m2 are underweight, 18.5 to 24.9 kg/m2 are normal weight, 25.0 to 29.9 kg/m2 are overweight and anyone over 30 kg/m2 is obese (World Health Organization). The studies used to determine the current cut off points for weight categories were conducted in European populations. Recent evidence from a multiethnic study showed that the cut-off point for obesity should be approximately 6kg/m2 lower in non-European populations to more accurately reflect the metabolic risk associated with weight such as blood pressure, glucose metabolism, and lipid metabolism (Razak et al. 2007), supporting the need for the development and use of ethnic specific BMI categories. Additionally, the prevalence of obesity has been increasing globally. In 2008, it was estimated that 1.46 billion adults worldwide were overweight or obese with average BMI increasing by 0.4 to 0.5kg/m2 per decade from the 1980s (Finucane et al. 2011). The greatest burden of disease is in Western countries. The United States has the highest percentage of obese adults (Finucane et al. 2011). However, developing countries are experiencing the greatest increases in incidence of obesity and in the future will be the greatest contributors to the obesity epidemic (Finucane et al. 2011). Obesity is associated with many health complications including type 2 diabetes, cardiovascular disease (CVD), fatty liver disease, cancer, obstructive sleep apnea, breathing difficulties, and musculoskeletal disability and pain (Schelbert 2009). These complications contribute to severe forms of obesity decreasing life expectancy by 5 to 20 1 M.Sc. Thesis – A. Mayhew; McMaster University – Health Research Methodology years (Fontaine et al. 2003). In addition to affecting health, obesity is also an economic burden. In the United States, the annual healthcare cost of obesity is estimated to be $56 billion with a positive association between BMI and per capita expenditure. Though difficult to measure, this number is much higher when considering the indirect costs of obesity, such as absenteeism, disability, and premature death (Lehnert et al. 2013). The treatments available for obese patients vary based on the degree of obesity and associated co-morbidities as well as the potential side effects of the therapeutic options. Interventions range from lifestyle modifications involving food restriction and increased energy expenditure through physical activity for those with mild obesity, to pharmacotherapy options for moderate obesity, and surgical interventions for those with the most extreme forms of obesity (Gray et al. 2012; Wyatt 2013). Despite the availability of diverse treatment options the effect of lifestyle interventions is modest and the more effective pharmacotherapy and surgical options are associated with serious complications. The lack of adequate treatments indicates that prevention may be the best strategy for curbing the obesity epidemic (Gortmaker et al. 2011). One of the barriers to obesity prevention is the abundance of contributing causes of the disease. The availability of low cost, calorically dense foods and less physical activity demands are often cited as the two biggest contributors to the rising prevalence of obesity (McAllister et al. 2009), particularly in developing countries which are increasingly influenced by Western culture through globalization (Malik et al. 2013). While energy balance is the most cited cause of obesity, other risk factors such as infections, epigenetic effects, maternal age, assortative mating, reproductive fitness, sleep debt, endocrine disruptors, pharmaceutical side effects, ambient temperature, and intrauterine and 2 M.Sc. Thesis – A. Mayhew; McMaster University – Health Research Methodology intergenerational effects have at minimum epidemiological evidence supporting their association with obesity (McAllister et al. 2009). Obesity risk is also partially attributable to genetic factors. Family and twin studies have established that 50 to 80% of the interindividual variation in predisposition to obesity is because of genetic factors (Choquet and Meyre 2011b). In an effort to determine how to better prevent obesity, genome wide association studies (GWAS) and candidate gene studies have identified close to 70 loci associated with obesity-related traits. Despite the identification of obesity predisposing single nucleotide polymorphisms (SNPs), the underlying mechanisms are poorly understood. Food behaviors such as energy consumption, macronutrient consumption distribution, food preferences, and satiety responsiveness have been investigated as possible mechanisms with some evidence of association with obesity promoting genes (Breen et al. 2006; Hasselbalch et al. 2008; Llewellyn et al. 2012; Cornelis et al. 2014). In addition to exploring the association of already known obesity promoting genes with food consumption parameters, examining the evolutionary history of obesity and other disordered eating patterns may also shed light on possible mechanisms. 3 M.Sc. Thesis – A. Mayhew; McMaster University – Health Research Methodology 2.0 Literature Review 2.1 Heritability of obesity To determine the heritability of traits or diseases, including obesity, four contributing factors that lead to the development of the phenotype are quantified (Boomsma et al. 2002). These factors and their symbols include (Rijsdijk and Sham 2002): A: Additive genetic influences which are calculated as the sum of the effect of each allele at all loci which influence the phenotype C: Shared environmental factors which are influences that would be common to members of a family such as socioeconomic status D: Non-additive genetic influences which include the interaction between alleles at the same locus (dominance) or at different loci (epistasis) E: Unique environmental influences such as differences in parental treatment, prenatal environmental, and life events Twin studies are a frequently used method to determine heritability taking advantage of the nearly 100% shared genetic data for monozygotic (MZ) twins. Theoretically, MZ pairs do not differ from one another genetically (A and D) and also have the same shared environmental factors (C), therefore the difference in phenotypic traits can be attributed to unique environmental influences (E) (Rijsdijk & Sham, 2002). Like other sibling pairs dizygotic twins (DZ) only share 50% of their genetic data, however are assumed to have the same shared environment (C) and for the individual environment (E) to vary to the same extent as is observed in MZ pairs (Rijsdijk & Sham, 2002). Using the assumption that the unique environment (E) contributes to the development of the phentoype of interest 4 M.Sc. Thesis – A. Mayhew; McMaster University – Health Research Methodology equally in MZ and DZ pairs, comparing the correlation of a phenotype in MZ pairs versus DZ pairs allows for an estimate of heritability as the difference in correlation should be attributable to genetics, both additive and non-additive effects (Boomsma et al. 2002). The most straightforward method of calculating heritability is Falconer’s formula which subtracts the phenotypic correlation in DZ pairs from the phenotypic correlation in MZ pairs and multiplies the result by two [H2= 2(rMZ – 2DZ)] (Rijsdijk & Sham, 2002). Family studies are also used to determine the heritability of phenotypes. Genotypic data can be collected using either genetic marker data or estimates of the expected genetic relatedness based upon the relationship between the two individuals. Creating a regression model of the genetic relatedness and the phenotypic trait of interest allows for an estimate of heritability (Vinkhuyzen et al. 2014). Modelling can also be used in twin studies, however models are poorly equipped to determine the non-additive genetic component (D) because non-additive genetic factors are confounded with shared environment and therefore cannot be estimated in the same model (Elks et al. 2012). Classic twin studies also have some limitations. The assumptions that gene-environment correlations and interactions are minimal as well as assuming that the amount of variance explained by environmental factors is identical in MZ and DZ pairs are questioned (Rijsdijk and Sham 2002). Making these assumptions increases the risk that heritability estimates are artificially inflated by incorrectly attributing the contribution of these factors to genetics (Manolio et al. 2009). The study design can have a substantial impact on heritability estimates. A recent metaanalysis of studies investigating BMI heritability found that in 88 independent twin studies (n=140,525), heritability estimates ranged from 0.47 to 0.90 while the estimates from 27 family studies (n=42,968) were lower, ranging from 0.24 to 0.81 (Elks et al. 2012). Another 5 M.Sc. Thesis – A. Mayhew; McMaster University – Health Research Methodology meta-analysis estimated the heritability to be 0.20 to 0.80 using data from family studies and 0.20 to 0.60 from adoption studies (Maes et al. 1997). Though the assumption that the amount of variance explained by environmental factors is the same in MZ and DZ pairs has been criticized for inflating heritability estimates (Rijsdijk and Sham 2002), a study conducted in 93 MZ pairs raised separately found that the intra-pair correlation for BMI in MZ pairs reared apart was 0.70 for men and 0.66 for females. For MZ pairs reared apart, there is no shared environment (C) and the variance explained by unique environmental influences can be correctly assumed to be appropriately equal in the separated twins. In this unique situation, the intra-pair correlations are estimates of the amount of the variance explained by only genetic factors. The same study used a classical twin design with MZ (n=154) and DZ (n=208) pairs to provide a heritability estimate of 0.82 for males and 0.78 for females (Stunkard et al. 1990). The difference in heritability estimates indicates that the classic twin design may have provided inflated heritability estimates due to confounding from gene-environment correlations and interactions (Rijsdijk and Sham 2002). The study supplemented their results by using maximum-likelihood model fitting analyses yielding heritability estimates of 0.74 for males and 0.69 for females. The similarities between these estimates and those provided through the twins reared apart support the use of modeling techniques for estimated heritability. The study was also the first to show that shared environment has a very modest effect on the variation in BMI (Stunkard et al. 1990). The broad range of heritability estimates for BMI can in part be explained by different study methodologies including family studies and twin studies, different statistical procedures such as using Falconer’s formula versus various modeling techniques, errors in 6 M.Sc. Thesis – A. Mayhew; McMaster University – Health Research Methodology phenotyping, or the incorrect classification of MZ and DZ pairs. From the most recent meta-analysis, the median heritability estimate from twin studies was 0.75 and 0.46 for family studies (Elks et al. 2012) indicating that that genes explain a moderate to high degree of the variability in obesity. Heritability estimates for BMI are also age-dependent, increasing with age and reaching a plateau at young adulthood (Silventoinen and Kaprio 2009; Silventoinen et al. 2010; Elks et al. 2012). Based on this information, exploration into the specific genes that may be contributing to obesity risk is warranted. 2.2 Heritability of eating characteristics Increased total energy intake is a well-established risk factor for obesity (McAllister et al. 2009), however many other eating behaviours are similarly found to be associated with body weight or increased caloric consumption. Strong epidemiological evidence supports a positive association between dietary fat consumption and weight (Bray et al. 2004) and a negative association between dietary carbohydrate consumption and weight (Gaesser 2007). In both adult and adolescent populations there is a growing body of evidence that food responsiveness including liking of food and satiety responsiveness, eating in the absence of hunger, disinhibition, and impulsivity/self-control are associated with BMI and overall food/energy intake (French et al. 2012). Because of the association of these eating characteristics with weight the same techniques used to determine the heritability of obesity have also been used to determine the hereditably of food consumption behaviour. 2.2.1 Energy consumption and macronutrient distribution 7 M.Sc. Thesis – A. Mayhew; McMaster University – Health Research Methodology A strong positive association between energy intake and weight as well as the difference in energy density of macronutrients have led researchers to investigate if consumption levels are a heritable trait. A study conducted in twin pairs from the Quebec Newborn Twin Study (n=379) (Dubois et al. 2013) found that the heritability of mean energy intake measured in kilocalories (kcal) is 0.42 (95% confidence interval 0.31 to 0.53), while the heritability of intake in grams of protein, fat, and carbohydrates is 0.35 (0.24 to 0.47), 0.34 (0.22 to 0.46), and 0.42 (0.31 to 0.53) respectively. The study also investigated the percentage of total daily calories from each macronutrient with only the percentage of calories from fat having significant heritability with an estimate of 0.28 (0.16 to 0.40). Studies conducted in adult populations including twin pairs (n=600) from the Danish Twin Registry, (Hasselbalch et al. 2008), twins and non-related individuals from the Minnesota Study of Twins Reared Apart (MISTRA) (n=335) (Hur et al. 1998), and families from the San Antonio Family Heart Study (n=1431) (Mitchell et al. 2003; Cai et al. 2004) have come to similar conclusions. The Danish Twin Registry (Hasselbalch et al. 2008) produced heritability estimates for the additive genetic effect of 0.38 (0.24 to 0.51) in males and 0.32 (0.12 to 0.48) in females for total energy consumption, 0.28 (0.12 to 0.43) in males and 0.01 (0.00 to 0.39) in females for percentage of calories from protein, 0.36 (0.22 to 0.49) in males and 0.49 (0.35 to 0.61) in females for percentage of calories from carbohydrates, and 0.01 (0.00 to 0.45) in males and 0.01 (0.00 to 0.57) from percentage of calories in fat. For the variables in which low heritability was found for additive genetic effects, there was a moderate to strong contribution of non-additive genetic effects (Hasselbalch et al. 2008). In MISTRA (Hur et al. 1998) the additive effects of genetics accounted for an average of 0.22 of the variability of nutrients investigated 8 M.Sc. Thesis – A. Mayhew; McMaster University – Health Research Methodology including 0.32 (0.10 to 0.51) for caloric consumption, 0.40 (0.20 to 0.57) for calories/kg consumed, 0.16 (0.00 to 0.37) for protein in grams, 0.35 (0.14 to 0.52) for fat in grams, and 0.25 (0.03 to 0.45) of carbohydrates in grams. In the San Antonio Family Heart Study (Mitchell et al. 2003; Cai et al. 2004), the heritability estimates were considerably lower, ranging from 0.09 to 0.21 (Cai et al. 2004) for total energy intake and grams of nutrients consumed per day, and between 0.13 to 0.26 for the percentage of total calories coming from macronutrients (Mitchell et al. 2003). A potential cause of the lower heritability estimates from the San Antonio Family Heart Study compared to the other studies is that they used related individuals opposed to twins requiring different statistical methods to be employed to estimate heritability. Dietary estimation methods used in these studies such as food frequency questionnaires (FFQs) and 24 hour recalls also have a significant amount of error associated with them which could also lead to different estimates. 2.2.2 Food consumption patterns In addition to assessing the heritability of the consumption of energy and macronutrients, studies have also investigated if certain dietary pattern types, for example diets high in fruits and vegetables, are heritable. In children, there is evidence that the types of food most commonly consumed are heritable. The MacArthur Longitudinal Study of Twins (n=792) found that using a 24 hour dietary recall, seven food categories investigated had significant heritability estimates, including an estimate of 0.79 for the consumption of peanut butter and jelly in males and 0.56 for the consumption of fish and lemons in females (Faith et al. 2008). Using factor analysis on 77 food items, Breen et al (2006) found four categories, dessert foods, moderate for vegetables, moderate for fruits, and high liking for protein foods with heritability estimates of 0.20 (0.04 to 0.38), 0.37 (0.20 to 0.58), 0.51 9 M.Sc. Thesis – A. Mayhew; McMaster University – Health Research Methodology (0.37 to 0.68), and 0.78 (0.63 to 0.92) respectively. In adult female twins from the United Kingdom (n=3262), five diet patterns, high fruit and vegetable, high alcohol, traditional English, dieting, and low meat accounted for 22% of the variance in dietary patterns with heritability estimates ranging from 0.41 to 0.48 (Teucher et al. 2007). In adult Finnish twin pairs (n=2009) factor analysis revealed four dietary patterns, healthy foods, high-fat foods, sweet foods, and meat with heritability estimates of 0.49 (0.40 to 0.56), 0.44 (0.34 to 0.53), 0.42 (0.32 to 0.51), and 0.39 (0.30 to 0.48) in males, and 0.54 (0.47 to 0.60), 0.47 (0.39 to 0.53), 0.43 (0.36 to 0.50), and 0.44 (0.36 to 0.51) in females respectively (Keskitalo et al. 2008a). Results from 4640 male and female twins in the United States aged 50 and over found two dietary patterns, items high in fat, salt, and sugar, and the other which was described as a healthy diet. The heritability estimate for the unhealthy diet pattern was 0.30 and 0.40 for the healthy diet pattern (van den Bree et al. 1999). The results from these studies indicate that in both children and adults, a moderate to high amount of the variance in food types consumed can be attributed to genetics. 2.2.3 Food consumption behaviours The heritability of other food consumption behaviours thought to be associated with obesity have also been investigated. Neophobia, a fear of trying new foods, has been studied in children and adults. It is proposed that previously, neophobia motivated humans to eat familiar foods to avoid consuming new items which may not be safe. Between 20 and 30% of children are estimated to be neophobic with the trait being associated with decreased consumption of fruits, vegetables, and protein foods (Wardle and Cooke 2008). In two independent twin studies conducted in pediatric populations using modeling techniques, heritability estimates of 0.72 and 0.78 were produced (Cooke et al. 2007; Faith 10 M.Sc. Thesis – A. Mayhew; McMaster University – Health Research Methodology et al. 2013). Similar estimates were found in young adults, 0.61 in females, (Knaapila et al. 2011) and in adult Finnish and British twins, 0.66 (Knaapila et al. 2007). Shared environment did not account for any of the variability in neophobia in any study except for males from the study by Knaapila et al. (2011), in which shared environment was estimated to account for 45% of the variability. Studies have also found that in twin adolescents (n=254), the number of bites taken per minute is associated with BMI as well as hereditable with an estimate of 0.62 (0.45 to 0.74) (Llewellyn et al. 2008). In the Gemini Twin Study (n=4804) at three months of age, enjoyment of food, food responsiveness, slowness in eating, satiety responsiveness, and appetite size were all associated with weight with slowness in eating, satiety responsiveness, and appetite size having heritability estimates of 0.42 (0.26 to 0.54), 0.45 (0.32 to 0.56), and 0.41 (0.28 to 0.52) respectively (Llewellyn et al. 2012). The Gemini Study had previously looked at the same population prior to three months of age and found higher heritability estimates for slowness in eating, satiety responsiveness, and appetite size (Llewellyn et al. 2010) indicating that the relative influence of genetics on these phenotypes may change over time. In older children, satiety responsiveness has been estimated to have a heritability of 0.63 (0.39 to 0.81) and 0.75 (0.52 to 0.85) for food cue responsiveness (Carnell et al. 2008), and 0.51 (+/- 0.10) for eating in the absence of hunger (Fisher et al. 2007). In adult populations, the Three Factor Eating Questionnaire has been used to determine the heritability of cognitive restraint, uncontrolled eating, and emotional eating. In male and female Finnish and British twins, heritability estimates were 0.26 to 0.63 for cognitive restraint, 0.45 to 0.69 for uncontrolled eating, and 0.09 to 0.45 for emotional 11 M.Sc. Thesis – A. Mayhew; McMaster University – Health Research Methodology eating when divided by sex and ethnicity (Keskitalo et al. 2008b). In another study of adult twins (n=110), the same questionnaire provided heritability estimates of 0.44 for cognitive restraint, 0.24 for perceived hunger, and 0.58 for restraint score scales (de Castro and Lilenfeld 2005). A Swedish twin study (n=782 pairs) found heritability estimates of 0.59 (0.52 to 0.66) for cognitive restraint, 0.60 (0.52 to 0.66) for emotional eating and 0.45 (0.36 to 0.53) for uncontrolled eating (Tholin et al. 2005). Number of meals consumed per day is also hereditable with an estimate of 0.44 in adult twin pairs (de Castro 1993). Despite the variation in heritability estimates which could be due to sampling effects, different ethnicities, differences in measuring phenotypes, the effect of age, and different statistical methods, there is strong evidence that food consumption behaviour is at least moderately hereditable. 2.2.4 Conclusions In both children and adults there is a growing body of evidence that a higher intake of calories, the total amount and relative intake of macronutrients including protein, fat, and carbohydrates, food consumption patterns such as eating more high fat foods, more fruits and vegetables, or high protein diets, as well as eating behaviours are moderately to highly heritable traits. At this point in time, not enough studies have been conducted to determine if heritability changes across the lifespan, what the effect of sex is, and how it might change between cultures and ethnicities. Interestingly, most of the studies concluded that the shared environment element (C), did not significantly contribute to the variation in phenotype with the individual environment playing a much larger role. 12 M.Sc. Thesis – A. Mayhew; McMaster University – Health Research Methodology 2.3 Current state of knowledge of the genetics of obesity 2.3.1 Monogenic obesity To date, the investigation of monogenic forms of obesity have provided the majority of the information regarding the genetics of obesity. Monogenic forms of obesity include both syndromic obesity which is associated with specific clinical phenotypes in addition to obesity, often including mild to severe cognitive deficits and unusual behaviour (Chung 2012) as well as non-syndromic obesity which is characterized by early-onset, severe obesity with extreme hyperphagia resulting from a single gene disorder (Choquet and Meyre 2011b). There are over 30 types of syndromic obesity (Choquet and Meyre 2010), however the mechanisms through which the genetic mutations effect energy homeostasis are not understood in all cases (Chung 2012). Prader Willi syndrome is the most common form of syndromic obesity affecting 1 in 15 000 to 20 000 live births and involves a loss of expression of paternal genes in the 15q11-13 region. Other well-known forms of syndromic obesity include Bardet-Biedl syndrome, Alstrom syndrome, and WAGR syndrome (Chung 2012). Though the precise mechanisms of action may not be known, all forms of monogenic obesity involve the central nervous system (CNS) (Choquet and Meyre 2010). Specifically, monogenic forms of obesity involve genes that impact the neuronal differentiation of the periventricular nucleus (PVN) and the leptin/melanocortin pathway. Eleven genes leading to monogenic obesity have been discovered including SH2B1 (Doche et al. 2012), LEP, LEPR, POMC, PCSK1, MC4R, MC3R (Mencarelli et al. 2011), MRAP2 (Asai et al. 2013), SIM1, BDNF and its receptor TrkB coded by the NTRK2 (Choquet and Meyre 2011b). See Table 1 for information about proteins coded by the obesity predisposing SNPs. The leptin/melanocortin pathway plays a critical role in food 13 M.Sc. Thesis – A. Mayhew; McMaster University – Health Research Methodology consumption regulation (Figure 1). Leptin is a cytokine like hormone secreted by adipocytes that acts in the hypothalamus to regulate food intake, energy expenditure, and nutrient portioning. Individuals unable to produce leptin or who have leptin resistance due to faulty receptors experience hyperphagia and consequent obesity (Chung 2012). The exact prevalence of monogenic obesity is unknown as a random cohort of obese subjects has not yet been genotyped, however it is estimated to be between 5 and 10% of all obese individuals for the eleven currently known genes and the 16p11.2 deletion (Choquet and Meyre 2011a). Gene Symbol SH2B1 LEP LEPR POMC PCSK1 MC4R MC3R MRAP2 SIM1 BDNF NTRK2 Protein Coded SH2B adaptor protein 1 Leptin Leptin receptor Proopiomelanocortin prohormone convertase 1 Proprotein convertase 1/3 Melanocortin 4 receptor Melanocortin 3 receptor Melanocortin 2 receptor accessory protein 2 Single-minded homolog 1 Brain derived neurotrophic factor Nueurotrophic tyrosine kinase receptor type 2 – codes TRkB receptor Table 1. Gene Symbols and Proteins Coded 14 M.Sc. Thesis – A. Mayhew; McMaster University – Health Research Methodology Figure 1. The role of monogenic obesity genes in the melanocortin pathway. White adipose tissue releases leptin in response to increased adipose tissue (Doche et al. 2012). Leptin travels to the brain, specifically the hypothalamus located in the periventricular nucleus. There it binds to leptin receptors on POMC neurons and AgRP neurons (do Carmo et al. 2013). SH2B1 plays a role in the leptin response by modulating the ability of leptin to bind to leptin receptors (Doche et al. 2012). On the POMC neurons, leptin binding causes the synthesis of which is then cleaved by PC 1/3 to produce α-MSH (Farooqi et al. 2007; Jung and Kim 2013). On AgPR neurons, leptin binding decreases the neuronal activity of NPY and AgRP. AgRP and α-MSH compete for binding on MC3R and MC4R (Jung and Kim 2013). If α-MSH binds to MC3R and MC4R, the activity of the protein is increased causing a suppression of appetite. If AgRP binds the activity of MC3R and MC4R are reduced and appetite is increased (Jung and Kim 2013). MRAP2 is an accessory protein that causes a small but significant reduction in the surface expression of MC4R and in combination with MRAP also reduces the function of MC3R (Chan et al. 2009). Similarly, a deficiency in SIM1 causes a lower concentration of MC4R mRNA in the periventricular nucleus (Zegers et al. 2014). Though the precise mechanisms are unknown BDNF and its receptor TRkB play a role in moderating the effect of the melanocortin pathway downstream (Bariohay et al. 2009). 15 M.Sc. Thesis – A. Mayhew; McMaster University – Health Research Methodology 2.3.2 Polygenic forms of obesity Three different study types have been used to determine gene variants associated with polygenetic obesity (Choquet and Meyre 2011b). Candidate gene studies involve choosing genetic variants based on biological, physiological, or pharmacological evidence of their role in weight regulation. Both MC4R and BDNF (Stutzmann et al. 2007) were discovered using candidate gene studies but otherwise the approach has not been successful for identifying obesity predisposing SNPs. Genome wide linkage studies are an extension of family studies in which families who have the phenotypic trait of interest are recruited and the association of various genetic markers with obesity are investigated. This strategy has not yielded many significant results, likely because of the small effect size of individual polygenic genes on obesity and confounding caused by the environment. Lastly, GWAS involve several hundred thousand SNPs across the human genome being investigated in a large population for their association with a phenotypic trait. As of June 2014, more than 2894 GWAS have been conducted (Yu et al. 2008). GWAS studies improve upon other designs because the large sample size of individuals allows researchers to find statistically significant results despite the small effect size of the gene (Manolio et al. 2009). Recent studies have provided firm evidence that common variants in or near 70 loci modestly increase BMI variation/obesity risk (Choquet and Meyre 2011b). Despite the highly significant association of many of the SNPs with BMI, the identified genetic variants only account for approximately 2% of the total heritability of obesity (Speliotes et al. 2010; Elks et al. 2012). Nine SNPs identified through GWAS studies (BDNF, NTRK2, LEPR, SH2B1, PCSK1, POMC, MC4R, TUB, SDCCAG8) overlap with monogenic forms of syndromic 16 M.Sc. Thesis – A. Mayhew; McMaster University – Health Research Methodology and non-syndromic obesity (Thorleifsson et al. 2009; Choquet and Meyre 2011a). However, the most frequently studied SNPs are within the fat mass and obesity associated gene (FTO). Shortly after the incidental discovery of an association of rs9939609 (FTO) and obesity in a GWAS study for type 2 diabetes conducted in a European population (Frayling et al. 2007), a GWAS investigating obesity-related quantitative traits in Sardinia found the same association which the authors then replicated in European Americans and Hispanic Americans (Scuteri et al. 2007). A study looking at extremely obese young Germans and their controls found a significant association of rs9939609 (FTO) as well as five other SNPs located in FTO with extreme, early onset obesity (Hinney et al. 2007). This study was followed by another research group concluding that rs1421085 and rs17817449 in FTO are both significantly associated with obesity in a European population using family data to exclude a potential undetected stratification effect (Dina et al. 2007). The association of rs9939609 has also been confirmed in African and Asian populations (Tung and Yeo 2011; Tan et al. 2014). Of all the obesity predisposing SNPs, rs9939609 (FTO) has the largest effect size, with those homozygous for the risk allele weighing on average 3kg more than those homozygous for the protective allele (Frayling et al. 2007). FTO belongs to the superfamily of Fe(II) 2-oxogluterate-dependent dioxygenases which catalyze the Fe(II)- and 2-oxoluterate-dependent demethylation of 3-methylthymine, 3methyluracil, and N6-methyladensoine in single stranded DNA (deoxyribonucleic acid) and RNA (ribonucleic acid). FTO is mostly expressed in the brain, specifically in the arcurate, paraventricular, dorsomedial, and ventromedial hypothalamic nuclei which is responsible for the control of energy homeostasis. Within the arcuate nuclei, FTO is regulated as a function of nutritional status with fasting causing a decrease in FTO 17 M.Sc. Thesis – A. Mayhew; McMaster University – Health Research Methodology expression and high fat diets causing an increase. Specifically, FTO levels appear to be regulated by the availability of essential amino acids. Decreased FTO expression increases food intake while increased FTO expression decreases food intake. Though the biological mechanism of action of FTO regulating total food intake is in line with studies showing an association of FTO SNPs with food intake, it is still unknown how FTO obesity-related SNPs influence FTO. However, based on the location of the SNPs, it appears that the SNPs are likely either up or down regulating FTO expression opposed to being functional mutations (Gulati and Yeo 2013). One of the challenges in understanding the genetics of obesity today is the discrepancy between heritability estimates and the amount of variance which is explained by known genetic variants, identified through GWAS (Golan and Rosset 2011). Despite being highly statistically associated with obesity, the SNPs identified by GWAS only account for approximately 2% of the total heritability of obesity (Elks et al. 2012). Because the effect sizes of obesity predisposing SNPs are relatively small (Manolio et al. 2009), it is possible that many SNPs associated with obesity are not detected because of the statistical significance requirements for a genome wide association, p < 5 x 10-8, (Dudbridge and Gusnanto 2008) and low minor allele frequencies (Yang et al. 2010). New strategies for handling GWAS data including linear model analysis and random effects models to estimate heritability without needing to know all of the genetic variants associated with a phenotype have been proposed (Yang et al. 2010; Golan and Rosset 2011). Yang et al. (2010) applied the linear model analysis method to human height which is estimated to be approximately 80% hereditable. Previously, 50 variants accounted for approximately 5% of the phenotypic variance. Using the linear model analysis method 18 M.Sc. Thesis – A. Mayhew; McMaster University – Health Research Methodology produced a heritability estimate of 84% indicating that statistical techniques may be appropriate for verifying heritability estimates from twin and family studies. The inclusion of SNPs that meet a minimum threshold for association with the disease but are not yet confirmed in modeling techniques can improve the accuracy of disease risk predictions, particularly when used in conjunction with novel technology such as machine learning algorithms which allow for models to take advantage of interactions between genetic markers. This technique was applied to GWAS data for Type 1 Diabetes which significantly improved the predictive value of the model compared to only using confirmed SNPs in regression models (Wei et al. 2009). These findings also indicate that there are many more genetic variants associated with obesity to be discovered. Broadening the scope of GWAS to non-European populations (Manolio et al. 2009) and working towards larger samples sizes to increase power are amongst the steps that can be taken to improve our understanding of the genetics of obesity. Including SNPs that are nominally significant with obesity/BMI increases the variance attributable to genetics, however the heritability estimates still remain far lower than those determined by family and twin studies (Yang et al. 2010). Other explanations of the “missing heritability” include rare variants which may have a large effect size but are not investigated because of their low minor allele frequency, genetic interactions as total heritability estimates assume that the risk alleles do not interact and have an additive effect, gene by environment interactions in which environmental factors modify the effect of risk alleles on the disease (Marian 2012), and copy number variations (Zhao et al. 2012). 19 M.Sc. Thesis – A. Mayhew; McMaster University – Health Research Methodology 2.4 Current state of knowledge of the genetics of eating behaviour After the identification of FTO and other obesity predisposing SNPs, researchers began to look at the association of obesity-predisposing SNPs with eating behaviours in an attempt to better understand the mechanism of action of genes in increasing obesity risk. Behaviours associated with obesity that have been identified to be under genetic control in heritability studies such as energy consumption, macronutrient distribution patterns, food consumption patterns, and eating behaviours have also been found to be associated with obesity predisposing SNPs. Several SNPs have consistently been shown to be associated with increased energy intake including rs9939609 (FTO) in children (Cecil et al. 2008; Timpson et al. 2008) and in adults (Speakman et al. 2008), and rs8050136 (FTO) (Haupt et al. 2009). Some genes have also been found to be associated with macronutrient consumption such as rs7498665 (SH2B1) with increased fat, saturated fat, and monounsaturated fat, rs368794 (KCTD15) with increased carbohydrate intake, rs2568958 (NEGR1) with decreased saturated fat and monounsaturated fat intake (Bauer et al. 2009), rs8050136 (FTO) with an increased percentage of calories from fat and decreased percentage of calories from carbohydrates (Park et al. 2013), and rs1421085 (FTO) with higher protein intake (Tanaka et al. 2013). To take into account that generally as BMI increases energy requirements also need to increase, leading to higher energy consumption, models were adjusted either for BMI/body weight (Cecil et al. 2008; Timpson et al. 2008; Haupt et al. 2009; Tanaka et al. 2013), total energy consumption (Bauer et al. 2009; Park et al. 2013), or basal metabolic rate (Speakman et al. 2008). By adjusting for BMI in the case of studies looking at the association of SNPs with total energy consumption, we can be 20 M.Sc. Thesis – A. Mayhew; McMaster University – Health Research Methodology more sure that the individual is consuming more food because of the SNP rather than because their increased body size requires it. Similarly, by adjusting for total energy intake when considering the association of SNPs with intakes of macronutrients, it indicates that the individual has a greater proportion of their diet coming from a specific macronutrient rather than simply consuming more energy and consequently a proportionate amount more of each macronutrient. Another method of determining if SNPs influence what is consumed is to look at food categories. There is evidence that the risk variant of rs4788099 (SH2B1) is associated with more servings of dairy products per day, and BDNF risk variants (rs10767664, rs6265, and/or rs1401625) are associated with more servings of meat, eggs, nuts and beans (Mccaffery et al. 2012). Some genes also seem to influence how and when people eat food. Having the risk variant for rs142085 (FTO) increases the number of eating episodes per day (Mccaffery et al. 2012), rs17782313 (near MC4R) is associated with an increase in disinhibition and emotional eating scores in females from the Three Factor Eating Questionnaire (Horstmann et al. 2013), nominally significant associations have been found between increased snacking with rs295946 (BDNF) and rs7498665 (SH2B1) (Robiou-du-Pont et al. 2013), statistically significant increases in snacking with rs17782313 (near MC4R) (Stutzmann et al. 2009), an association of decreased fullness after food consumption for rs9939609 (FTO) (Dougkas et al. 2013), increased food responsiveness in children is associated with rs9939609 (FTO) (Velders et al. 2012) as well as reduced satiety (Wardle et al. 2008) and increased food consumption (Wardle et al. 2009). A genotype score, which sums the obesity predisposing alleles for obesity, may also be used to determine if genetics are influencing food related behaviours. Using a gene score, a negative association was found 21 M.Sc. Thesis – A. Mayhew; McMaster University – Health Research Methodology with satiety responsiveness in children while the gene score was positively associated with adiposity and BMI (Llewellyn et al. 2014), and an unexpectedly negative association with total energy intake and higher fibre intake (Rukh et al. 2013). In summary, numerous associations have been found between obesity predisposing genes and food intake behaviour, however many results have not been replicated and the studies have mostly been conducted in European populations. An exception is FTO which has consistently been shown to be associated with food consumption parameters including total energy intake (Cecil et al. 2008; Speakman et al. 2008; Timpson et al. 2008; Haupt et al. 2009), total fat intake (Timpson et al. 2008; Tanofsky-Kraff et al. 2009; Lee et al. 2010; Lear et al. 2011; Park et al. 2013), protein intake (Chu et al. 2013; Tanaka et al. 2013), carbohydrate intake (Park et al. 2013), food category consumption (Brunkwall et al. 2013), satiety (Wardle et al. 2008; Hoed et al. 2009; Rutters et al. 2010; Dougkas et al. 2013), number of eating episodes per day (Mccaffery et al. 2012), and restraint/control of food consumption (Tanofsky-Kraff et al. 2009; Velders et al. 2012; Cornelis et al. 2014). The lack of replications is indicative of the unavailability of food consumption data in large genotyped populations, differences in measurement of dietary parameters, as well as small sample sizes exacerbated by the small effect size of obesity-predisposing SNPs. However, the scatter results also show that though some SNPs may work through modifying food consumption patterns, some genes may be operating through other mechanisms such as altering metabolism. 22 M.Sc. Thesis – A. Mayhew; McMaster University – Health Research Methodology 2.5 Background of eating disorders 2.5.1 Diagnostic criteria The DSM-5 (Diagnostic and Statistical Manual of Mental Disorders, version 5) currently describes three eating disorders, anorexia nervosa (AN), bulimia nervosa (BN), and binge eating disorder (BED). AN is characterized by patients being severely underweight (<85% of expected weight), having an intense fear of gaining weight or becoming fat, a disturbance in body image, a heavy emphasis on body shape for selfevaluation, and denial of the seriousness of their current weight loss (American Psychiatric Association, 2013). There are two types of AN, binge-eating/purging type (ANBP) involving overeating and purging, and the restricting type (ANR) involving dieting without binging or compensatory behaviours. It is unclear if these are distinct subgroups or different phases of the disease (Hartmann et al. 2013). Similar to AN, people with BN place a heavier emphasis on body shape for self-evaluation. The other key characteristic of BN is having recurrent episodes of binge eating during which larger than reasonable quantities of food are consumed during a discrete period of time. During these episodes, people feel a lack of control, either unable to stop eating or limit the amount consumed. After binges, inappropriate compensatory behaviour to prevent weight gain is used. In the purging type of BN, self-induced vomiting, laxative misuse, diuretics or enemas are used. In the nonpurging type of BN the compensatory behaviours include excessive exercise or abuse of medication. This behaviour must occur on average a minimum of once a week for three months to be diagnosed. BED has the same diagnostic criteria as BN, without the inappropriate compensatory behaviour (American Psychiatric Association, 2013). 23 M.Sc. Thesis – A. Mayhew; McMaster University – Health Research Methodology 2.5.2 Symptoms, comorbidities, and mortality of eating disorders Of the three eating disorders, AN is considered the most dangerous. More than 10% of patients with AN will die from it in their lifetime, the highest mortality of any mental disorder (Hoek 2006). Short term symptoms of AN include dizziness, headaches, brain fogginess, feelings of coldness, nausea, weakness, poor sleep and blurred vision while long term issues include osteoporosis, cardiovascular disturbances, electrolyte imbalances, diabetes mellitus, thyroid disorders, gastrointestinal disorders and fertility and pregnancy problems (Fairburn & Harrison, 2003; Meczekalski, Podfigurna to Stopa, & Katulski, 2013). Mood disorders are also common in people with AN, with estimates from 31.0 to 88.9% of patients suffering from other mental health issues. Depression is the most prevalent (40 to 45%), however bipolar affective disease, social phobia, obsessive compulsive disorder, and substance abuse are also common (Meczekalski et al. 2013). BN has a significantly lower mortality rate than AN, estimated to between 0% to 3.3% (Keel and Brown 2010; Franko et al. 2013). There is significant overlap of BN and AN, with 5% of people diagnosed with BN eventually developing AN and 25 to 30% of people receiving treatment for BN previously having been diagnosed with AN (Kaye et al. 2000). The medical complications of BN in comparison to AN are also generally less severe. Permanent dental erosion caused by contact with gastric acid during self-induced vomiting is one of the most common side effects, though it is also found in people with AN who purge. Electrolyte imbalances such as hypokalemia, hypochloremia, and hyponatremia, can occur as a result of repeated vomiting. These electrolyte imbalances can cause arrhythmias. Severe but rare side effects include gastric rupture or esophageal tears (Klein and Walsh 2003). Similarly to those with AN, people with BN suffer from 24 M.Sc. Thesis – A. Mayhew; McMaster University – Health Research Methodology psychiatric comorbidities with a lifetime prevalence of between 64.1% to 84.8% (Jaite et al. 2013; Kessler et al. 2013). Specific disorders include depressive disorders 40.0% to 45.8% (Jaite et al. 2013; Keski-Rahkonen et al. 2013), anxiety disorders - 15.7% (Jaite et al. 2013), and somatoform disorders – 21.1% (Jaite et al. 2013). BED is highly associated with overweight/obesity (Reichborn-Kjennerud et al. 2004; Field et al. 2012) with 2 to 25% of those seeking treatment for obesity being diagnosed with BED (Fairburn et al. 2000; Fairburn and Harrison 2003; Yanovski 2003). The estimated mortality of BED is 0 to 3%, however the follow up period for most studies has been relatively short which may not capture outcomes such as premature death that may occur as a result of obesity (Keel and Brown 2010). An estimated 63.6% of those with BED have some type of psychiatric comorbidity (Hudson et al. 2008), particularly anxiety and mood disorders (Reichborn-Kjennerud et al. 2004; Preti et al. 2009). There is evidence that some patients with BED may also develop BN, with up to 9% of patients developing BN 12 years after the diagnosis of BED (Keel and Brown 2010; Field et al. 2012). 2.5.3 Treatment The treatment of AN has four main components, helping patients recognize they need help and to maintain their motivation to get better after receiving help, weight restoration, addressing patients’ over evaluation of self based on shape and weight and preoccupation with eating habits, and lastly using compulsory treatment when medically necessary (Fairburn and Harrison 2003). Whether outpatient, day-patient, or inpatient care is provided is dependent on the psychological and physiological severity of the disease. Various forms of therapy are used including family-based treatment in younger patients, and cognitive behaviour therapy (CBT) (Fairburn and Harrison 2003). An estimated 50% 25 M.Sc. Thesis – A. Mayhew; McMaster University – Health Research Methodology of people suffering from AN will recover almost fully, while 30% will continue to have symptoms intermittently throughout their life. The remaining 20% will chronically suffer from the disease, often with death from AN as the final outcome (Kaye et al. 2000). The treatment of BN has been relatively well studied with over 50 randomized controlled trails (RCT). The findings strongly indicate that CBT focusing on modifying the specific behaviours and ways of thinking that maintain the eating disorder is crucial with approximately 20 individual sessions over a 5 month period resulting in one third to one half of patients making a full recovery (Kaye et al. 2000; Fairburn and Harrison 2003; Keski-Rahkonen et al. 2009). The results of the RCTs have also shown that antidepressant drugs have an anti-bulimic effect, decreasing the frequency of binge eating and purging. However, anti-depressant drugs are not as effective as CBT and the results are often not sustained. To date, there is no reliable evidence of predictors for successful treatment (Fairburn and Harrison 2003). An estimated 15 to 30% of patients still meet the diagnostic criteria for BN within 5 to 10 years after diagnosis and the remainder will experience intermittent relapses over their lifetime (Fairburn et al. 2000; Kaye et al. 2000). Treatments for BED focus on two aspects, weight loss and controlling binge eating (Brownley et al. 2007). Treatment options include pharmacotherapy such as antidepressants (fluoxetine, fluvoxamine, sertraline, citalopram, imipramine, desipramine), anticonvulsants (topiramate), appetite suppressants (subutramine), fat absorption inhibitors (orlistat), behavioural interventions with CBT being the most common, though dialectical behaviour therapy has been investigated, and more unique methods such as virtual reality and self-help books (Carter and Fairburn 1998). Combinations of drugs and behavioural interventions are also common (Brownley et al. 26 M.Sc. Thesis – A. Mayhew; McMaster University – Health Research Methodology 2007). Overall, the evidence is limited as to which treatment options are best but the evidence suggests that as with BN, CBT in addition to pharmacotherapy options may provide the best results for controlling binge eating and reducing weight (Brownley et al. 2007). The remission rates reported by studies are highly variable, ranging from 25 to 82% (Fairburn et al. 2000; Keel and Brown 2010), further emphasizing the need for more studies involving BED. 2.5.4 Risk factors for eating disorders Eating disorders, particularly AN and BN are considered a Western disease affecting mostly females in adolescence and early adulthood. Other general risk factors include having a family history of any type of eating disorder, depression, substance misuse, as well as either a family history of obesity or being obese in the case of BN. Life experiences including early menarche (BN), high parental expectations, sexual abuse, family dieting, criticism about one’s shape and size, and participation in activities promoting a low fat mass like distance running, swimming, dancing, and modelling increase risk (Klein and Walsh 2003). Personality characteristics including low selfesteem, perfectionism (particularly in the case of AN), anxiety, and anxiety disorders are also risk factors for eating disorders (Fairburn and Harrison 2003). Personal characteristics: Common personality characteristics of individuals diagnosed with AN and BN include perfectionism, obsessive-compulsiveness, neuroticism, negative emotionality, harm avoidance, low self-directedness, low cooperativeness, and traits associated with avoidant personality disorder (Cassin and von Ranson 2005; Kaye 2008). People with the restrictive type of AN tend to have low novelty seeking, low emotional responsiveness, decreased pleasure, decreased seeking of pleasure, 27 M.Sc. Thesis – A. Mayhew; McMaster University – Health Research Methodology and reduced social spontaneity compared to those with BN who tend to be impulsive, seek out new experiences, and have characteristics of borderline personality disorder (Cassin and von Ranson 2005; Kaye 2008). BED is associated with perfectionism, sensation seeking, and obsessive compulsive personality disorder, overall having many more personality characteristics in common with BN and the purging form of AN compared to the restrictive form of AN (Cassin and von Ranson 2005). Family environment: Historically, many theories of the development of eating disorders focused on the family environment. Typically family dynamics that involve overprotective, intrusive, controlling, emotionally unresponsive, and rigid parents as well as enmeshment of parents and children, poor conflict resolution, and a lack of opportunity for children to express themselves were thought to increase eating disorder risk (Klump et al. 2002; Kardum et al. 2008; O’Shaughnessy and Dallos 2009). The development of an eating disorder was theorized to be a means for communicating avoided messages by adolescents to their parents (O’Shaughnessy and Dallos 2009). Due to the challenges in classifying, diagnosing, and studying eating disorders with the additional complication of family dynamics being difficult to study, there is limited evidence of if and how the family environment affects eating disorder risk. Broadly, a meta-analysis including 17 studies found that families which had at least one person suffering from an eating disorder reported worse family function in comparison to control families. A wide spectrum of features were used to define family functioning including cohesion, adaptability, conflict, affective expression, affective involvement, communication, task accomplishment, problem solving, achievement orientation, role performance, family hierarchy, behaviour control, adherence to values and norms, and constraining implicit family rules. The results across studies for 28 M.Sc. Thesis – A. Mayhew; McMaster University – Health Research Methodology which specific domains of family dysfunction were most relevant to all eating disorders or specific disorders were inconclusive. Some studies found significant differences between family functioning domains for different eating disorder subgroups, however none of the results were replicated across studies (Holtom-Viesel and Allan 2014). A preoccupation with weight in the form of family dieting or receiving criticism about weight, eating or body shape, similarly can increase risk (Fairburn and Harrison 2003). Weight preoccupations enforced by non-family factors, such as participating in sports that encourage thinness like dance or gymnastics or that heavily emphasize weight such as wrestling can also be damaging (Mitchison and Hay 2014). Though not always related to the family, childhood trauma has been found to increase the risk of developing an eating disorder, particularly if the abuse was sexual or physical in nature (Smolak and Murnen 2002; Mitchison and Hay 2014). Gender: AN is most prevalent in females, with a ratio of 10-20 females diagnosed for each male and an overall lifetime prevalence of 0.3 to 3.0% for females and 0.24 to 0.30% for males in Western countries (Favaro et al. 2003; Hoek and van Hoeken 2003; Currin et al. 2005; Hoek 2006; Wade et al. 2006; Hudson et al. 2008; Preti et al. 2009; Marques et al. 2011; Heaner and Walsh 2013; Meczekalski et al. 2013). BN is similarly more prevalent in females with approximately 0.88 to 4.6% of females suffering from the disease in Western countries (Favaro et al. 2003; Hoek and van Hoeken 2003; Hoek 2006; Wade et al. 2006; Hudson et al. 2008; Keski-Rahkonen et al. 2009; Preti et al. 2009; Smink et al. 2012) compared to 0.10 to 1.5% of males (Hudson et al. 2008; Preti et al. 2009; Smink et al. 2012). Compared to AN and BN, BED is more equally distributed between the genders. The lifetime prevalence is estimated to be between 2.5 29 M.Sc. Thesis – A. Mayhew; McMaster University – Health Research Methodology to 3.5% for females and 1.5 to 2.0% for males (Spitzer et al. 1992, 1993; Hay 1998; Kinzl et al. 1999; Hudson et al. 2008). A general estimate is that up to 25% people with BED are male (Fairburn and Harrison 2003). Age: AN and BN both predominantly affect young people, though AN has a slightly earlier age of onset compared to BN (Fairburn and Harrison 2003). The peak incidence of AN is between the years of 10 and 19 (Fornari et al. 1994; Favaro et al. 2003; Hoek and van Hoeken 2003; Currin et al. 2005; Son et al. 2006; Wade et al. 2006; Franko et al. 2013; Kessler et al. 2013) with an estimated 40% of all cases of AN occurring in those 15 to 19 years of age (Hoek and van Hoeken 2003). For BN, there is greater variability in the estimates of peak incidence, which in part could be because of the use of different age cut off points as well as the relatively recent changes in diagnostic criteria. The peak incidence is estimated to be as low as 10 to 20 years of age (Currin et al. 2005; Keski-Rahkonen et al. 2009), or as high as 25 to 29 years (Son et al. 2006) with other estimates falling in between those ranges (Kinzl et al. 1999; Hoek and van Hoeken 2003; Preti et al. 2009).The average age of onset provides more specific estimates, 20.0 years of age for BN purging type, 19.0 years for BN non-purging type (Wade et al. 2006) and between 17.0 and 19.7 years for both types combined (Fornari et al. 1994; Favaro et al. 2003; Hudson et al. 2008). There are currently no reliable estimates of peak incidence for BED. However, three studies have found that the incidence of the disease is relatively equally distributed across the lifespan. (Kinzl et al. 1999; Alegria et al. 2007; Grucza et al. 2007). Point estimates for the age of onset of BED range from 18.3 years (Favaro et al. 2003) to 25.4 years (Barry et al. 2002; Wade et al. 2006; Hudson et al. 2008). In a study consisting of 30 M.Sc. Thesis – A. Mayhew; McMaster University – Health Research Methodology participants from six European countries, it was found that while there were no new cases of AN diagnosed after 20 years of age and only a limited number of cases of BN, BED continued to be regularly diagnosed in people above the age of 40 (Preti et al. 2009). A possible explanation for the differences in peak incidence estimates for BED is provided by Spurrell et al. (1997) who found that there was a statistically significant difference in the age that individuals first met the criteria for BED between those who starting binging first versus those who started dieting first. In the binge first group, the average age of meeting the criteria for BED was 18.81 (+/- 10.74) years and in the diet first group, the average age of meeting the criteria for BED was 33.20 (+/-11.95) years. Similar results were found in a study by Grilo and Masheb (2000). Time Trends: A study conducted in six European countries found an inverse association between cohort (age at interview) and lifetime risk of eating disorders, with the younger cohort (18 to 29 years) having an odds ratio of 7.9 (3.89 to 16.20) of developing any eating disorder in their lifetime compared to the 45 years and older age category (Preti et al. 2009). This relationship was true for all subcategories of eating disorders with the lowest odds ratio for BN (4.1), and the highest for AN (14.5). A metaanalysis of the diagnosis of AN and BN globally with a focus on Westernized countries found a correlation of 0.35 for the association between time and the increase of AN and a correlation of 0.89 for BN (Keel and Klump 2003). A small review by Hoek and van Hoeken (2003) supports that there has been an overall increase in the incidence of BN in the United States, Netherlands, and United Kingdom from the early 1980s to the early 1990s as well as an upwards trend since the 1950s of the incidence in AN, specifically in 31 M.Sc. Thesis – A. Mayhew; McMaster University – Health Research Methodology 15 to 24 year old females, though the same increase in incidence was not found in males and females over 25 years of age. Studies published after the reviews have provided conflicting evidence of if the incidence of eating disorders are increasing over time. A population based sample (n=3001 in 1995, and 3047 in 2005) from metropolitan South Australia, found that there was a 2.4 times greater risk for being diagnosed with BED in 2005 compared to 1995 (Hay et al. 2008). Similarly in the United Kingdom, there was 3 fold increase in the early 1990s for BN, particularly amongst females aged 10 to 39 years. The same study found that since 1996 the incidence has been declining, likely in part because of decreased symptom recognition and changes in service use (Currin et al. 2005). Contrary to other studies, evidence from a cohort of American college aged males and females from 1982, 1992, and 2002, concluded that the prevalence of BN decreased over time, from 4.2%, to 1.3% to 1.7% in females, and 1.1%, 0.4%, and 0% in males (Keel et al. 2006). Possible explanations of the discrepant findings are the altering of diagnostic criteria, shifting attitudes about mental health disorders, the inherent challenge in identifying patients who often try to keep their disease hidden, and various methodologies used (Keel and Klump 2003). Sampling poses a specific issue as some studies recruited from very specific populations such as university students or public school students decreasing the generalizability of the findings. Small sample sizes of less than 500 people are also common. An example of the possibility that revised diagnostic criteria may lead to changes in the frequency of diagnosis of a disease is the dramatic increase in the incidence of BN from pre 1980 to post 1980. The true incidence may have increased or the increase may be attributed to the publication of the DSM-III where BN was first recognized as its own diagnostic category (Hoek and van 32 M.Sc. Thesis – A. Mayhew; McMaster University – Health Research Methodology Hoeken 2003). While the results should be interpreted with caution, the evidence seems to indicate that in Western societies, all three types of eating disorders, AN, BN, and BED may be becoming more common. Ethnicity and Culture: Understanding the roles of ethnicity and culture in eating disorder development is challenging. The concepts of ethnicity and culture are often inappropriately interchanged and are intrinsically connected making it next to impossible to study the effect of ethnicity or culture without confounding. Studying eating disorders in a global context adds additional challenges because environmental factors like the availability of doctors may be unrelated to culture but greatly impact the diagnosis and measurement of the disease. Several studies of eating have been conducted in multiple ethnicities from the same country in an attempt to understand ethnic and cultural effects on the development of eating disorders. Though it is tempting to assume that all people living in the same country have a shared culture and that the differences found between ethnicities would related to their genetics, this is an appropriate conclusion. Within a country there are innumerable subcultures, many of which are highly associated with ethnicity. Therefore, the results of the studies included in this review are unable to conclude if ethnicity is influencing the development of eating disorders because of underlying genetic differences or because people from different ethnic backgrounds are part of different subcultures. Anorexia Nervosa - Eating disorders are often cited as a Western disease however there is evidence that AN is found worldwide. In non-Western countries the prevalence of AN is estimated to be between 0.002% to 0.9%, significantly lower than the estimated prevalence of 0.3 to 3% for females and 0.24% for males in Western countries (Hoek 2006; 33 M.Sc. Thesis – A. Mayhew; McMaster University – Health Research Methodology Wade et al. 2006; Hudson et al. 2008; Preti et al. 2009; Marques et al. 2011; Heaner and Walsh 2013; Meczekalski et al. 2013). A meta-analysis of all reports including grey literature of AN in non-Western nations, taking country, diagnostic criteria, prevalence of cases, presence of weight concern in patients, and level of Western influence into consideration found that there are reported cases of AN worldwide, even in people who are unlikely to have experienced any Western influence. The most significant difference between the cases of AN in Western countries versus non-Western countries is the presence of weight concerns as a motivating factor for food refusal. If weight concerns are removed as a diagnostic criteria for AN, the prevalence of AN is very similar in Western and nonWestern countries (Simpson 2002; Keel and Klump 2003). Though Keel and Klump (2003) concluded that AN occurs in all ethnicities and in all cultures, a study in Curacao, a Caribbean island, found an overall incidence of 1.82 cases of AN per 100 000 persons per year without a single case in Black females (Harten et al. 2005) despite Curacao being under a strong Western influence at the time of the study. Similarly, in the United States, a study including 2046 females from the NHLBI (The National Heart, Lung, and Blood Institute) Growth and Health Survey found that of the 1061 black females participating in the study, not one was diagnosed with AN, despite 1.5% of the white females participating having the disease (Striegel-Moore et al. 2003). Another study conducted in the United States investigating 5191 adults and 1170 adolescents who are African American and Caribbean Black found that the lifetime prevalence of AN in the adult population was 0.15% for African Americans and 0% for Caribbean Blacks (Taylor et al. 2013), significantly lower than the estimated prevalence of 0.3 to 3% for females and 0.24% for males in Western countries. (Hoek and van Hoeken 34 M.Sc. Thesis – A. Mayhew; McMaster University – Health Research Methodology 2003; Currin et al. 2005; Hoek 2006; Wade et al. 2006; Hudson et al. 2008; Preti et al. 2009; Marques et al. 2011; Heaner and Walsh 2013; Meczekalski et al. 2013). The study by Taylor et al. (2003) partially supports Keel and Klump's (2003) theory that preoccupation with weight is a culturally driven attribute. When preoccupation with weight was removed as a diagnostic criteria, there was an increase in prevalence of AN of 0.21% in the African American population though there was no increase in the Caribbean Black population. This result highlights the confusion regarding the role of culture and the role in genetics in ethnicity. The increase in prevalence of AN in African Americans but not Caribbean Blacks could be because of underlying genetic differences that alter the predisposition to the disease, or it could be reflective of African Americans and Caribbean Blacks being part of different subcultures that could alter the risk of AN. One study interested in determining the genetic versus cultural impact of ethnicity investigated the degree of acculturation of Asian-Americans and found that the prevalence of AN was lower than in the White American population independent of acculturation (Nicdao et al. 2007). While the results indicate underlying genetic differences, the results still may be confounded as the degree of acculturation may not capture all relevant elements of culture. Bulimia Nervosa – BN is significantly less studied than AN, particularly in the international context limiting the conclusions that can be made about the role of ethnicity and Westernization in the disease (Keel and Klump 2003). Despite the limited studies available, it is generally accepted that the prevalence of BN is lower in non-Western countries compared to Western countries. A possible explanation is the unique environment necessary for BN which includes the ability to access large quantities of food as well as having weight concerns driving the need to purge (Keel and Klump 2003). The 35 M.Sc. Thesis – A. Mayhew; McMaster University – Health Research Methodology meta-analysis by Keel and Klump (2003) which found that AN exists worldwide no matter the degree the Western influence found the opposite for BN. There were no studies in nonWestern countries reporting the presence of BN in an individual without exposure to Western ideals. Extrapolating from the evidence for AN which found that as countries became more Westernized, there was a transmission of Western beauty ideals emphasizing thinness which coincided with increases in the prevalence of AN (Simpson 2002) it is possible that BN is not as prevalent in non-Westernized countries because people who do not idealize thinness would not fear gaining weight and therefore would not purge to compensate after binging episodes. The importance of Western influence in causing weight concerns motivating eating disorders is supported by a study conducted in the United States Latino population which found that recent immigrants had the lowest rates of BN while those who have resided in the United States for 70% or more of their lives had the highest rates (Alegria et al. 2007). Similarly to the research conducted for AN, the prevalence of BN has been looked at in multiple ethnicities from one country. A study including 2046 females from the NHLBI Growth and Health Survey in the United States found that 2.3% of white females, but only 0.4% of black females had a lifetime diagnosis of BN (StriegelMoore et al. 2003). In a study of African American and Black Caribbean adults living in the United States, the lifetime prevalence of BN was 1.40% for the African Americans and 1.98% for the Caribbean Blacks, lower than the estimated prevalence of 0.88 to 4.6% for all females (Favaro et al. 2003; Hoek and van Hoeken 2003; Hoek 2006; Wade et al. 2006; Hudson et al. 2008; Keski-Rahkonen et al. 2009; Preti et al. 2009; Smink et al. 2012) and 0.10 to 1.5% for males (Hudson et al. 2008; Preti et al. 2009; Smink et al. 2012) in Western countries. Removing preoccupation with body weight resulted in a modest increase in the 36 M.Sc. Thesis – A. Mayhew; McMaster University – Health Research Methodology prevalence of BN (Taylor et al. 2013). These ethnic differences may reflect the consequences of subcultures, specifically what type of body shape is considered ideal, or the potential for underlying genetic differences predisposing individuals to BN. Binge Eating Disorder - BED is distinct from AN and BN because it does not include weight preoccupation as a diagnostic criteria (American Psychiatric Association, 2013). Weight preoccupation is predominantly a Western concern (Simpson 2002) and perhaps also ethnicity specific as evidenced by White American females experiencing a larger discrepancy between their current weight and ideal weight and being more concerned about dieting, regardless of current BMI compared to their African American counterparts (Gluck and Geliebter 2002). Unlike AN and BN where generally there is a higher prevalence in populations of European heritage, most studies have found that the prevalence of BED is as high as or higher in Black Africans compared to Whites. Very limited data is available regarding other ethnicities. The lifetime prevalence of BED is estimated to be between 2.5 to 3.5% for females and 1.5 to 2.0% for males in Western countries (Spitzer et al. 1992, 1993; Kinzl et al. 1999; Ghaderi and Scott 2001; Hudson et al. 2008). A study conducted in African Americans and Caribbean Blacks in the United States partaking in the National Survey of American Life (NSAL) found that the lifetime prevalence of BED in African American adults is 5.02%, and 5.78% for Caribbean Black adults (Taylor et al. 2013). While this study had an exceptionally high prevalence of BED, a study including the pooled data from the NIMH (National Institute of Mental Health) Collaborative Psychiatric Epidemiological Studies in the United States found the lifetime prevalence of BED to be 1.91% in non-Latino Whites, 2.71% in Latinos, 1.66% in Asians, and 2.22% in African Americans females and 0.75%, 1.67%, 0.95%, and 0.97% 37 M.Sc. Thesis – A. Mayhew; McMaster University – Health Research Methodology respectively in males. The only statistically significant differences between groups existed for non-Latino White males versus Latino males, and non-Latino White versus African American males (Marques et al. 2011). Similar lifetime prevalence estimated were found in another study in the United States focusing on the Latino population, 1.55% for males, and 2.31% for females (Alegria et al. 2007). A study involving a biracial population-based cohort of males and females participating in a longitudinal study of cardiovascular risk factor development had similar results indicating the prevalence of BED is approximately the same in White and Black populations. The Revised Questionnaire on Eating and Weight patterns was used to establish BED status among the 3948 (55% females, 48% Black) participants, who were 28 to 49 years of age. Prevalence of BED was 1.5% overall, with similar rates among Black females (2.2%), White females (2.0%), and White males (1.2%), while Black males had a significant lower prevalence (0.4%). (Smith et al. 1998). While less studied, it appears that the lifetime prevalence of BED in Asian Americans is within the general range of the White population with 2.67% of females and 1.36% of males being affected by the disease (Nicdao et al. 2007) The higher prevalence of BED in Blacks compared to Whites may be explained by this lack of weight preoccupation. BN, which involves the same binge eating behaviour seen in BED, but also includes a purging element motivated by the fear of gaining is more prevalent in White females compared to Black females. Even within the BED population, White females are significantly more concerned about eating, dietary restraint, shape concern, and weight concern compared to Black females, despite on average being less overweight (Pike et al. 2001). Because a smaller proportion of African Americans have weight concerns, there is the potential that the population is less likely on average to engage 38 M.Sc. Thesis – A. Mayhew; McMaster University – Health Research Methodology in purging behaviour compared to their White American counterparts. Therefore they receive a diagnosis of BED rather than BN. This is supported by studies such as (Taylor et al. 2013) which found that when weight preoccupation was removed as a criteria, the prevalence of BN in African Americans and Caribbean Blacks increases. Summary of the role of ethnicity and culture in the development of eating disorders – It is generally accepted that the lifetime prevalence of AN according to the current diagnostic criteria is higher in the White population compared to other ethnicities. However, the degree of Westernization may play an important role, especially in the development of AN and BN which both require an individual to have preoccupations with their weight to receive a diagnosis. The idealization of a slim body type and weight preoccupation is a Western phenomenon and there is evidence that the more a person is influenced by Western culture, the more likely it is for them to develop either AN or BN. However, studies have also shown that regardless of acculturation to Western ideals, there are still some significant differences between the prevalence of eating disorders in people of different ethnic backgrounds who have been raised in the same country. These differences may be reflective of subcultures existing within countries that may be strongly associated with ethnicity or that the genetic differences between ethnicities may alter the baseline risking of an individual for developing an eating disorder and that exposure to Western ideals, particularly that a low weight makes one attractive, may modulate the risk. 2.6 Heritability of eating disorders There is very strong evidence that eating disorders are moderately to highly heritable. In a 2005 review of family studies investigating the heritability of AN and BN, 39 M.Sc. Thesis – A. Mayhew; McMaster University – Health Research Methodology all but one study reported increased risk of eating disorders in those with family members displaying eating disorders (Slof-Op ’t Landt et al. 2005). It is estimated that the lifetime risk of AN and BN among female relatives of a person with an eating disorder is 7 to 20 times higher than that of the general population (Strober et al. 2000; Klump et al. 2001). Estimates of the heritability of eating disorders range from 0.28 to 0.76 for twin studies of AN and 0.30 to 0.83 for twin studies of BN. In many of these studies, broad definitions for disease diagnosis were used to increase statistical power because of the low prevalence of the diseases (Slof-Op ’t Landt et al. 2005). Interestingly, a large portion of the remaining variance for the risk of developing either AN or BN is accounted for by non-shared environmental factors, estimated to be between 0.17 to 0.50 compared to the relatively low estimates of the effect of shared environmental factors (Klump et al. 2002; Slof-Op ’t Landt et al. 2005). The lifetime risk of having BED is estimated to be between 1.9 and 2.2 times higher for those with a relative with the disease and twin studies have estimated the heritability is between 0.41 and 0.57 (Thornton et al. 2011). 2.7 Genetics of eating disorders A variety of different types of studies have been conducted to determine the genetic architecture of eating disorders including linkage studies, candidate gene approaches, and GWAS. Linkage studies use related individuals to identify regions of the genome containing genes that predispose individuals to a disease have provided limited (Teare and Barrett 2005). Candidate gene studies investigate genes that have been selected based on their physiological, biochemical, and functional aspects (Zhu and Zhao 2007). GWAS are studies attempt to identify common genetic variants that contribute to disease risk using markers from the entire genome (Bush and Moore 2012). 40 M.Sc. Thesis – A. Mayhew; McMaster University – Health Research Methodology Linkage studies have provided limited results in the context of eating disorders. In a collaboration of 5 studies, there were no AN-affected relative pairs with nonparametric linkage (NPL) scores above 1.80, however people with the restrictive subtype of AN had a linkage peak at 1p33-36 (NPL score = 3.03) and a peak at 4q12-14 (NPL score = 2.44). Investigating the traits of drive for thinness and obsessionality in the AN sample revealed three possible linkages on chromosome 1q31 (LOD (logarithm of odds) score = 3.46) for both traits, 2p11 (LOD score = 2.22) for obsessionality, and 13q13 (LOD score = 2.5) for drive for thinness. For BN, chromosome 10p13 (LOD = 2.92), and 10p14 (LOD score = 2.7) achieved significant linkage results, while 14q22-23 were almost significant (LOD score = 1.97). When regular vomiting in those with BN was used as a phenotype, the linkage on chromosome 10p13 was strengthened (LOD=3.39) (Slof-Op ’t Landt et al. 2005). Genome wide association studies (GWAS) are studies which identify common genetic variants that contribute to disease risk (Bush and Moore 2012) as well as candidate gene studies investigating genes selected based on physiological, biochemical, and functional aspects (Zhu and Zhao 2007) have also been widely used. The results of these studies in relation to eating disorders can be categorized into three main biological pathways, the serotonin pathway, the catecholamine pathway, and the pathway involved with neuropeptide and feeding regulation (Slof-Op ’t Landt et al. 2005) 2.7.1 Serotonin Serotonin (5-HT) is involved with normal brain function including mood state, hunger, sex, sleep, memory, emotion, anxiety, and endocrine function (Haleem 2012). Symptoms of AN such as depression (Meczekalski et al. 2013), refusal to consume food, 41 M.Sc. Thesis – A. Mayhew; McMaster University – Health Research Methodology binging behaviour (American Psychiatric Association, 2013), and hyperactivity (Sternheim et al. 2014) are all linked to circulating serotonin levels (Haleem 2012). Serotonin levels are determined using 5-hydroxyindoleacetic acid (5-HIAA), the primary metabolite of serotonin. 5-HIAA level are elevated in both those suffering from AN and BN as well as those recovered from the diseases indicating the possible role of hyperserotonergic function (Scherag et al. 2010). Furthermore, there is evidence that people suffering from and who have recovered from AN have a reduced ability to experience reward, specifically in the context of food. Though anhedonia, a decreased ability to experience pleasure (Ho and Sommers, 2013) is often cited as the reason for decreased pleasure from food in people with AN, there is also the possibility of reward contamination (Keating et al. 2012). The theory of reward contamination stems from people suffering from eating disorders originally gaining pleasure from losing weight and practicing weight loss activities which then contaminates the usual reward responses, ultimately causing a neural overlap in circuits processing reward and punishment making it difficult for people to correctly regulate their behaviour (Keating 2010). The association of SNPs related to the serotonin pathway with eating disorders is conflicted. The most promising polymorphism is within the 5-HT2A (5-hydroxytryptamine receptor 2A) receptor gene (1438G/A, A is risk allele). In a meta-analysis of 11 studies of individuals with AN, the odds ratio for having the disease if the risk allele (-1438A) is present is 1.22 (95% confidence interval: 1.09 to 1.35) (Martaskova et al. 2009). However high between-study heterogeneity reduces the confidence in the statistically significant increase in risk (Gorwood 2003; Slof-Op ’t Landt et al. 2005). For the association of 1438G/A with BN, five of eight studies were not significant, two were positive indicating 42 M.Sc. Thesis – A. Mayhew; McMaster University – Health Research Methodology the A allele as the risk allele and one study indicated that the G allele is the risk allele (Maj and Monteleone 2008). To our knowledge, no studies have investigated the association of 5-HT2A with BED. 5-HT2A is regulated by estrogen which provides biological support for the association of 5-HT2A and eating disorders, particularly AN, because eating disorders are significantly more prevalent in females than males and in females usually begin at the time of puberty (Frank et al 2002, Kaye et al 2001). Further evidence comes from a study indicating that people currently suffering from or who have recovered from AN have reduced binding of 5-HT2A (Kaye et al. 2013). 5-HTTLPR (serotonin-transporter-linked polymorphic region), the promoter region of the serotonin transporter coded by the SLC64A gene has provided some promising results in relation to eating disorders. Individuals either have the short allele (S) with only 14 repeats of a sequence versus those with the long allele (L) with 16 repeats. Carriers of the short allele only make half as much of the serotonin transporter protein as those with the long allele (Trace et al. 2013). A meta-analysis using a random effects model of eight independent samples of individuals with AN provided a z-score of 2.54 (p=0.1) for having the S-containing genotype versus the L/L genotype (Calati et al. 2011), similar results to an earlier meta-analysis involving four studies which found an odds ratio of 1.38 (95% confidence interval: 1.16 to 1.72) for people with the short allele variant compared to the long allele variant (Gorwood 2004). In a meta-analysis of individuals from 6 studies with BN, the results were non-significant (Polsinelli et al. 2012) with Calati et al. (2011) concluding that there was no significant difference in the occurrence of the S-containing genotype versus the L/L genotype in BN patients from 7 studies. Interestingly, there is a relationship between 5-HTTLPR and the development of BN in individuals who already 43 M.Sc. Thesis – A. Mayhew; McMaster University – Health Research Methodology have AN indicating the possibility of differences within the eating disorder population based on impulse control (Bailer et al. 2007; Castellini et al. 2012; Trace et al. 2013). To our knowledge, no studies have investigated the association of 5-HTTLPR with BED, however (Akkermann et al. 2012) determined that the 5-HTTLPR risk allele interacted with adverse life events in 18 year olds to increase the risk of binge eating indicating there may be some effect. Other serotonin receptors including the 5HT1B, 5HT1DB, 5HT2C, 5HTR3B, 5HT3B, 5-HT1D, and 5HT7, and the enzymes tryptophan hydroxylase (TPH) responsible for the synthesis of serotonin, and monoamine oxidase A (MAOA) which breaks down serotonin have been studied in relation to eating disorders. However, the studies investigating these receptors and enzymes in the context of their association with eating disorders is limited and inconclusive at this point in time (Rask-Andersen et al. 2010; Scherag et al. 2010; Trace et al. 2013). 2.7.2 Catecholamine pathway The main neurotransmitters involved in the catecholamine pathway are dopamine and norepinephrine (Rask-Andersen et al. 2010; Baik 2013). Dopamine is the primary catecholamine neurotransmitter found in the brain and affects physiological functions such as motor activity, hormone secretion, motivation, and emotional behaviours (Baik 2013; Trace et al. 2013). In the context of eating disorders, it is theorized that increased dopamine activity is associated with symptoms such as weight loss, altered satiety, impulse control, mood, hyperactivity, amenorrhea, body image distortion, and obsessive-compulsive behaviour (Kaye et al. 2013; Trace et al. 2013). Two main theories similar to those for 44 M.Sc. Thesis – A. Mayhew; McMaster University – Health Research Methodology serotonin exist on how dopamine may play a role in the development of AN. The first is that dieting and exercise are initially rewarding behaviours and as time progresses the behaviour is maintained through conditioning (Scheurink et al. 2010), and the second is that people with AN have reduced food consumption because they do not receive pleasure from food (Kontis and Theochari 2012). The effects of dopamine may be different in BN and BED. Blocking dopamine receptors has been found to increase appetite and cause weight gain, therefore overeating during binge periods may be a compensation method for the blunting of the pleasurable response to eating (Barry et al. 2009). Severely obese individuals have been found to have fewer striatal dopamine receptors compared to normal weight people with a decrease in the number of dopamine receptors as weight increases (Wang et al. 2001). Therefore, overweight/obese people may binge on highly palatable and calorically dense foods which stimulate the greatest amount of dopamine activity (Abizaid et al. 2006). It is unknown at this time if low dopamine activity is the cause of overeating (Barry et al. 2009), or if overeating causes elevated dopamine levels leading to the down regulation of dopamine receptors (Wang et al. 2004). SNPs involved with three dopamine receptors (D2, D3, and D4), a dopamine transporter (DAT1), as well as catecholamine-O-methyltransferase (COMT), an enzyme involved in monoamine metabolism, have been investigated for their association with eating disorders. Overall, the evidence is at best weak with more studies being conducted in people with AN than BN or BED. For DRD2 (dopamine receptor 2), a statistically significant relationship was found between DRD2 - +725 3’ G>T and TaqIA C>T with the purging subtype of AN (Bergen et al. 2005) as well as an association between rs1800497, rs2283265 and rs6277 (DRD2) with BED (Davis et al. 2012). However, Nisoli et al (2007) 45 M.Sc. Thesis – A. Mayhew; McMaster University – Health Research Methodology did not find between group differences of TaqA1 C>T in those with AN, BN, those who are obese, and a control group, and Gervasini et al (2013) found no association between rs1800497 (DRD2) and AN. DRD3 has been less studied, however both Gervasini et al. (2013) and Bruins-Slot et al. (1998) found no association between AN and the DRD3 Ser/Gly variant and DRD3 with Val1 polymorphism in exon 1 respectively. Two studies have found a positive association between DRD4 (7 repeat allele) and a greater risk of AN (OR=1.74, 95% CI 1.01 to 2.97) and BED (OR=3.25, 95%CI 1.43 to 7.41) (Gervasini et al. 2013). Other positive results include an association between AN and DRD4-616C/C ( odds ratio: 3.83, 95% confidence interval: 1.05 to 13.98) (Gervasini et al. 2013) and an association between DRD4 - C-521T’C’ allele and AN (Bachner-Melman et al. 2007). However two studies found no between group differences for DRD4 (13-bp and 48-bp deletion) in patients with AN, underweight students, and obese children/adolescents (Hinney et al. 1999) and DRD4 (22, 24, 33, 34, 44 repeats, 27, 37, 47 repeats, and 77 repeats) prevalence in female siblings, one with and one without AN (Karwautz et al. 2001). Only one study investigated DAT1 and AN and found no association (Gervasini et al. 2013). For COMT, only AN has been reasonably well studied, with a meta-analysis of COMT (rs4680) and AN including 11 datasets (2021 cases, 2848 controls, 89 informative trios) concluding there is no association and very little between study heterogeneity (Brandys et al. 2012). To conclude, the evidence supporting the link between dopamine genes and eating disorders is extremely limited, with the strongest, yet still weak evidence, supporting an association with DRD4. Potential reasons for the inconsistencies and lack of findings are small sample sizes and changing diagnostic criteria for eating disorders. 46 M.Sc. Thesis – A. Mayhew; McMaster University – Health Research Methodology Despite the lack of success in genetic association studies, there is significant biological evidence of the role of serotonin in eating disorders. PET (positron emission tomography) studies have revealed that patients recovered from AN have increased binding of DA D2/D3 receptors in the anterior ventral striatum relative to controls, indicating either a reduction in the intrasynaptic dopamine concentrations or an increase in the density or affinity of the D2 and D3 receptors. A decrease in homovanillic acid (HVA), a metabolite of dopamine in the cerebrospinal fluid of recovered AN patients supports a decrease in intrasynamptic dopamine concentrations (Kaye et al. 2013). There is also evidence that patients recovered from AN have feelings of anxiety after the release of dopamine (contrary to the usual euphoria in controls without the disease), indicating that patients with AN may restrict eating to avoid the release of anxiety causing dopamine. (Kaye et al. 2013). Specifically in patients with BN, peripheral and central HVA are lower compared to people without the disease and there is evidence that HVA levels which are depressed while suffering from the disease can be returned to normal levels after treatment (Bello and Hajnal 2011) 2.7.3 Norephinephrine Norepinephrine is thought to influence eating patterns through its actions on the hypothalamic paraventricular nucleus (PVN). Norepinephrine can either increase or reduce eating, depending on where it is and the balance of α1- and α2- adrenoreceptors present. α1adrenoreceptors supress appetite, while α2- adrenoreceptors increase appetite (Wellman 2000). Though there is a plausible role for norepinephrine in eating disorders, very little research has been conducted in the area. One study found a novel 343-bp sequence with 5 additional AAGG repeat islands within the norepinephrine transporter (NET) gene 47 M.Sc. Thesis – A. Mayhew; McMaster University – Health Research Methodology promoter region. In the NET gene promoter polymorphic region (NETpPR), a 4-bp deletion (S4) or insertion (L4) in the AAGG4 resulted in the net loss or gain, respectively, of a putative Elk-1 transcription factor site. There was a significant preferential transmission of L4 (odds ratio 2.1) from parent to child with restricting AN (Urwin et al. 2002). Hu et al. (2007) attempted to replicate the results, however did not find any statistically significant results in a sample of 142 family trios with AN from London, United Kingdom, and Vienna, Austria. 2.7.4 Neuropeptides and Feed Regulations Opioids: Opioid receptors are involved in food intake, reward sensitivity, and pain and are thought to play a role in vulnerability to addictive disorders (Trace et al. 2013). Endogenous opioids are linked to the enjoyment of food with sweet and fatty foods increasing opioid receptor binding and binge eating leading to changes in the endogenous opioid system, creating a cyclical pattern of binging (Mathes et al. 2010; Bello and Hajnal 2011). The current hypothesis is that people with AN have a dysregulation of the opioid system and are predisposed towards being addicted and that restriction and exercise are a means to compensate for the diminished response to reward (Trace et al. 2013). Betaendorphin, an agonist of opioid receptors has been measured in people with eating disorders. In both AN and BN patients it is unclear if beta-endorphin levels, are increased, decreased, or unchanged though overall evidence indicates decreased (Brewerton et al. 1992; Johnson 1995). A genome wide linkage analysis of 192 families was conducted finding an association between marker D1S3721 on chromosome 1p with restrictive type AN (Grice et al. 2002) leading to the investigation of opioid delta receptor (OPRD1), located on chromosome 1 (chr1p36.3-34.3) as a candidate gene. Three of five OPRD1 48 M.Sc. Thesis – A. Mayhew; McMaster University – Health Research Methodology SNPs were significantly associated with AN (OPRD1(8214T>C), p=0.045 for alleles, OPRD1 (23340A>G), p=0.046 for alleles, OPRD1(47821A>G), p=0.003 for genotypes and 0.01 for alleles) (Bergen et al. 2003). The association of OPRD1 SNPs with AN was further supported when three gene polymorphisms (rs569356, p=0.0011 for genotype for all types of AN, rs521809, p=0.163 for restrictive subtype, rs4654327, p=0.0246) were found to be associated with AN (Brown et al. 2007). To date, no genetic association studies have been conducted with BN or BED patients. Neuropeptide Y (NPY): Neuropeptide Y is released by both the sympathetic nervous system and from isolated adipocytes and plays a role in adipocyte regulation. Activation of Y2 receptors in abdominal fat prompts the body to store abdominal fat, contributing to obesity as well as increasing appetite (Bulloch and Daly 2014). Activation is thought to occur when body fat stores are diminished and the body is attempting to achieve homeostasis, however in patients with AN, despite increased NPY levels in the spinal fluid and brain, the disease persists (Södersten et al. 2008). In patients with BN, cerebrospinal fluid (CSF) level concentrations are not significantly different than those without the disease, however, plasma concentrations are significantly elevated (Smitka et al. 2013). Only one study to date has tested the genetic association between NPY and eating disorders, finding no association between NPY gene SNP (rs16139) and all eating disorders combined, or AN, BN, and BED separately, p<0.479 for genotype (Kindler et al. 2011). Peptide YY (PYY): PYY is secreted by the digestive tract after food consumption, promoting satiety. Two forms of PYY are secreted, PYY1-36 and PYY3-36, with evidence supporting that PYY3-36 may exert its anorectic effect by inhibiting dopamine and norepinephrine release through its bonding on NPY Y2 receptors in the hypothalamus. 49 M.Sc. Thesis – A. Mayhew; McMaster University – Health Research Methodology Negative associations between PYY with leptin and grehlin have also been found. Limited evidence exists about PYY concentrations in those with eating disorders. For those with AN and BN there is conflicting evidence on basal PYY levels, however there may be some effect on PYY after food is consumed (Smitka et al. 2013). Melanocortin Pathway (MC4R): MC4R deficiency is the most common cause of monogenic obesity in addition to contributing to polygenic obesity. MC4R exerts its effect on obesity by regulating appetite through the leptin-melanocortin signalling system (Valette et al. 2013a). Leptin, a hormone released by adipocytes that causes feelings of satiety though the release of anorexigenic peptides, such as POMC, as well as supressing AgRP (Rask-Andersen et al. 2010; Valette et al. 2013a). When POMC is cleaved, it produces α-MSH which then binds to MC4R to decrease food intake (Valette et al. 2013a). The agouti protein, closely related to AgRP, which has been extensively studied in mice because of its link to obesity, hyperphagia, hyperinsulimia, hyperglycemia (in males), and ability to antagonize MC4R preventing α-MSH from binding (Corander and Coll 2011). When AGRB binds to MC4R it promotes food consumption (Valette et al. 2013a). Leptin: Leptin levels are negatively associated with obesity and people suffering from AN have significantly reduced leptin levels compared to controls, as well as increased soluble leptin receptor levels (Brewerton et al. 2000; Dolezalova et al. 2007). The evidence is less clear with BN patients who may experience a decrease, increase, or no change in leptin levels. It appears that severity and duration of the disease may play a role in decreasing leptin levels. In BED, no changes in leptin have been observed (Monteleone et al. 2004). The leptin receptor was of interest because it is located in 1p31.2, close to the marker at 1p34.2 previously identified for increasing susceptibility to AN through linkage 50 M.Sc. Thesis – A. Mayhew; McMaster University – Health Research Methodology studies (Grice et al. 2002). Despite mutations causing a complete lack of circulating leptin irrevocably leading to severe obesity without exogenous leptin treatment (Bastard and Feve 2012), there is no evidence that genetic variants in LEP or LEPR are associated with any eating disorders. Three LEPR SNPs (Lys109Arg, Gln223Arg, Lys656Asn) were compared in females with and without AN, however there were no significant differences in allele or genotype frequency, even when AN patients were categorized into restrictive and purging types (Quinton et al. 2004). Similarly, two novel mutations in the coding region of the leptin gene (ser-91-ser; glu-126-gln), and a novel polymorphism (-1387 G/A) in the leptin gene linked upstream region (LEGLUR) were not found to be associated with AN, BN, underweight, or early onset obesity (Hinney et al. 1998) Proopiomelancortin Gene (POMC): There are not any studies to date investigating genetic variants in POMC and eating disorders. Agouti Related Peptide (AgRP): In patients with AN, AgRP is elevated, however after returning to a normal weight, AgRP are similar to healthy controls (Moriya et al. 2006; Merle et al. 2011). In BN, there is a negative correlation between AgRP and selfreported BN symptoms (Lofrano-Prado et al. 2011). Only two studies have investigated the genetic relationship between AgRP SNPs and eating disorders. A significant effect of Ala67Thr-AGRP (p=0.046) and AN was found (Dardennes et al. 2007) as well as a relationship between two mutations in perfect linkage disequilibrium, 760A and 526A in AgRP and AN with carriers 2.63 times more likely to develop AN (Vink et al. 2001). Melanocortin 4 Receptor (MC4R): Four studies have investigated the association of functional MC4R mutations and BED in obese people. No studies have been conducted for BN or AN. Three of the four studies found no association (Hebebrand et al. 2004; 51 M.Sc. Thesis – A. Mayhew; McMaster University – Health Research Methodology Lubrano-Berthelier et al. 2006; Valette et al. 2013b) while one study found that all obese people with MC4R functional mutations display binge eating behaviour compared to 14.2% of obese people without mutations and 0% of normal weight subjects without mutations (p<0.001) (Branson et al. 2003). However, this study used a different questionnaire to diagnose BED and was done in a sample eligible for bariatric surgery that may not generalizable to other obese populations. Ghrelin: Ghrelin is an appetite-stimulating hormone that increases during fasting and decreases following a meal and that is inversely associated with BMI (Atalayer et al. 2013; Trace et al. 2013). Ghrelin is predominantly produced in the stomach and takes action in the hypothalamus by activating NPY and AgRP containing neurons to increase appetite. A review of the evidence of ghrelin in eating disorders found that in 11 of 16 studies, people with AN had higher ghrelin levels than controls, 6 out 9 studies found that people with BN have no difference in ghrelin levels, and 2 out of 2 studies found that people with BED have less ghrelin than controls (Atalayer et al. 2013). Further support of the role of ghrelin in eating disorders comes from exogenous ghrelin administration increasing food intake in females with AN (Hotta et al. 2009). Overall, genetic studies seem to indicate that polymorphisms of the ghrelin gene are not associated with risk of eating disorders. Of 5 studies investigating AN, four found no association between Arg51Gln (rs34911341), Leu72Met (rs696217), Gln90Leu (rs4684677), 3056T>C (rs2075356) (Ando et al. 2006; Cellini et al. 2006; Monteleone et al. 2006; Kindler et al. 2011) and one study found a statistically significant relationship for the transmission of Leu72Met to offspring with AN (p=0.004), including the binging subtype specifically (p=0.005) (Dardennes et al. 2007). Three of four studies investigating BN found no association 52 M.Sc. Thesis – A. Mayhew; McMaster University – Health Research Methodology between Arg51Gln (rs34911341), Leu72Met (rs696217), and Gln90Leu (rs4684677), with BN (Cellini et al. 2006; Monteleone et al. 2006; Kindler et al. 2011) and one study conducted in Japanese females found that Leu72Met (rs696217, p=0.0410, OR=1.48, 95%CI: 1.01 to 2.15) and 3056T>C(rs2075356, p=0.0035, OR=1.63, 95%CI: 1.17 to 2.26) are associated with BN as well as an association between all eating disorders and 3056T>C (rs2075356, p=0.0110, OR 1.37, 95%CI: 1.07 to 1.74) (Ando et al. 2006). Only one study investigated BED and found no association with the SNPs Arg51Gln (rs34911341), Leu72Met (rs696217), Gln90Leu (rs4684677) (Kindler et al. 2011). Brain Derived Neurotrophic Factor (BDNF): BDNF is part of the nerve growth family which binds to a specific receptor, tropomyosin receptor kinase (Trk) B, that is responsible for the growth and regulation of neuronal cells by moderating survival, development, and enhanced synaptic activity in addition to BDNF’s role of modulating neurotransmitters including dopamine, serotonin, and glutamate providing a biological pathway for BDNF to influence food consumption (Nakazato et al. 2012). Serum BDNF has strong evidence indicating it is positively associated with BMI, however there is conflicting evidence of if BDNF levels increase or decrease in patients with eating disorders (Nakazato et al. 2012). Further evidence of the role of BDNF in food consumption behaviours comes from studies of humans with mutation deletions in the BDNF region. Individuals with the deletion mutation suffer from extreme hyperphagia and obesity (Gray et al. 2006; Han et al. 2008). A 2007 meta-analysis of the effect of BDNF Val66Met (rs6265) including five studies estimated that individuals with the Met/Met or Met/Val genotypes have a 36% greater chance of developing an eating disorder than those with the Val/Val genotype. 53 M.Sc. Thesis – A. Mayhew; McMaster University – Health Research Methodology Though the pooled effect was positive, only two of the five studies had statistically significant results and one of the studies had a negative association (Gratacòs et al. 2007). Since the meta-analysis, further studies have yielded inconclusive results. For Val66Met (rs6265) specifically, four out of five studies investigating the gene found no statistically significant relationship with AN (Dardennes et al. 2007; Ando et al. 2012; Brandys et al. 2013; Gamero-Villarroel et al. 2013) and the study with the positive outcome for Val66Met (rs6265) as well as rs2030324 was no longer significant after adjusting for multiple testing (p-values between 0.002 to 0.21 for genotypes and 0.00 to 0.039 for alleles) (DmitrzakWeglarz et al. 2013). Two studies published prior to the meta-analysis but not included found positive associations between the Met allele of the Val66Met BDNF polymorphism and restricting type AN and minimum BMI in a Spanish population (Ribasés et al. 2003) and a positive association between the Met allele of the Val66Met BDNF polymorphism and restrictive type AN, and minimum BMI (Ribasés et al. 2005). One study found a positive result for BDNF (rs7934165A/270T) and AN (p=0.008) (Mercader et al. 2007). Addition BDNF SNPs that were found to not have an association include rs11030102, rs10835210, rs16917237, rs56164415, and rs11030119 with both AN and BN (GameroVillarroel et al. 2013), and rs712442, rs11030107, rs7103873, rs11030123, rs17309930, rs2049048, and rs1491851 with AN (Slof-Op ’t Landt et al. 2011) Other Mechanisms: There are other proposed mechanisms that may have genetic links to eating disorders though they are less well studied. Cholecystokinin, a hormone which decreases appetite through receptors in the CNS as well as stimulating the digestion of lipids and proteins in the small intestine has had suggestive evidence linking it to AN (Rask-Andersen et al. 2010). Glutamate receptor (NMDAr) also plays a role in eating 54 M.Sc. Thesis – A. Mayhew; McMaster University – Health Research Methodology behaviour through its action on the reward system for food consumption and is associated with the SK3 Channel which in the brain, regulates the ion flow through the NMDA receptor. Genes coding for SK3 and NMDAr have both been shown to be associated with AN (Rask-Andersen et al. 2010). 2.7.5 Summary Though there is an undeniable genetic component to the development of eating disorders, with heritability estimates from twin studies ranging from 0.28 to 0.76 for AN and 0.30 to 0.83 for BN (Strober et al. 2000; Klump et al. 2001), and between 0.41 to 0.57 for BED (Thornton et al. 2011). Our review of genetic association studies found very little evidence supporting the role of functional variants in genes that may influence eating disorders. There was inconclusive evidence for genes related to serotonin (5HT2A, 5-HTTLPR, 5-HT1B, 5-HT1DB, 5-HT2C, 5-HTR3B, 5-HT1D, 5-HT7), dopamine (DRD2, DRD3, DRD4, COMT), norepinephrine (NET), and peptide YY with studies finding a range of negative, positive, and no effect results. Genes associated with Neuropeptide Y, Leptin (LEPR), and ghrelin, had evidence indicating a lack of association with eating disorders while AGRP was found to have a possible association with AN, MC4R a possible association with BED, and BDNF with all eating disorders. The strongest evidence was for OPRD1 (opioid receptor) with AN. 55 M.Sc. Thesis – A. Mayhew; McMaster University – Health Research Methodology 3.0 Justification and Objectives As the prevalence of obesity continues to increase worldwide (Finucane et al. 2011), there is a dire need to better understand the disease to curb the obesity epidemic and help prevent health complications (Schelbert 2009), decreases in life expectancy (Fontaine et al. 2003), and reduce the economic burden (Lehnert et al. 2013). Obesity treatments fall on spectrum of effectiveness. Lifestyle interventions are very limited in their success, pharmacotherapy options are successful in some cases, and bariatric surgeries can lead to significant weight loss. However, the more effective the treatment, the higher the risk for serious complications (Gray et al. 2012; Wyatt 2013). Investigating methods of preventing obesity, rather than treating it may be the most viable solution (Gortmaker et al. 2011). The moderate to high hereditability of obesity, estimated to be between 0.47 and 0.90 using twin studies and between 0.24 and 0.81 using family studies (Elks et al. 2012), the hereditability of eating characteristics such as energy consumption and dietary macronutrient distribution (Hur et al. 1998; Faith et al. 2004; Fisher et al. 2007; Hasselbalch et al. 2008; Dubois et al. 2013), and the identification of common variants located in or near approximately 70 loci that are associated with obesity (Choquet and Meyre 2011b) suggest that understanding the underlying genetic architecture of obesity may be an important step in determining how to prevent obesity. Researchers are investigating ways in which genetics may be causing weight increase by testing the association of obesity predisposing SNPs with eating behaviours among other endophenotypes (e.g. energy expenditure). The strongest evidence currently involves total energy intake (Cecil et al. 2008; Speakman et al. 2008; Timpson et al. 2008; 56 M.Sc. Thesis – A. Mayhew; McMaster University – Health Research Methodology Haupt et al. 2009), though some SNPs have also been found to be associated with macronutrient intakes (Bauer et al. 2009; Park et al. 2013; Tanaka et al. 2013) or amount of food consumed from specific food groups (Mccaffery et al. 2012). Studies have also shown associations between obesity predisposing SNPs and how people eat such as the number of eating episodes, the amount of disinhibition when eating, snacking habits, and satiety (Wardle et al. 2008; Stutzmann et al. 2009; Mccaffery et al. 2012; Robiou-du-Pont et al. 2013). Though there is sufficient evidence to conclude that eating behaviours at least partially mediate the relationship between the obesity predisposing SNPs and measures of obesity, the limited access to genotypic and phenotypic data in large populations as well as small effect sizes require a further investigation of these relationships to confirm current findings as well as to look at other eating patterns. Eating disorders, including AN, BN, and BED are extreme eating patterns that are also worthy of investigation. They are heritable diseases with hereditability estimates of 0.28 to 0.78 for AN, 0.30 to 0.83 for BN (Slof-Op ’t Landt et al. 2005), and 0.41 to 0.57 for BED (Thornton et al. 2011). Despite the moderate to high heritability of the diseases, there is little evidence supporting the role of functional mutations in genes that may be increasing risk for the eating disorders. Because eating disorders are heritable there is reason to believe that historically, characteristics of the diseases would have offered a competitive advantage for survival. Theorizing about potential evolutionary advantages of symptoms of eating disorders with the support of modern epidemiological evidence may help future gene identification efforts. With adequate sample sizes GWAS should be able to identify genes predisposing to eating disorders and the evolutionary theories may help provide strong biological evidence strengthening the findings of GWAS. Understanding 57 M.Sc. Thesis – A. Mayhew; McMaster University – Health Research Methodology the genetic architecture of eating disorders, particularly BN and BED which involve excessive food consumption, may help to identify new genes associated with obesity or disordered eating behaviours as well as determining biological pathways through which genes are regulating feeding behaviour. The objectives of this thesis are: 1. To investigate the association of obesity predisposing SNPs and a gene score with nutrient consumption parameters including the intake of total energy, total fat, saturated fat, trans fat, monounsaturated fat, polyunsaturated fat, carbohydrates, and protein intake in a population of European ancestry. 2. To look at eating disorders from an evolutionary perspective using current epidemiological evidence to help in future gene identification efforts for eating disorders. 58 M.Sc. Thesis – A. Mayhew; McMaster University – Health Research Methodology 4.0 The Association of Obesity SNPs with Food Consumption Patterns 4.1 Introduction The rise of obesity in the past three decades has reached worldwide epidemic proportions (Finucane et al. 2011). Obesity is associated with numerous psychosocial and health-related complications including type 2 diabetes mellitus, gallbladder disease, osteoarthritis, coronary heart disease, some types of cancer, and decreased life expectancy (Must et al. 1999; Calle et al. 2003; Fontaine et al. 2003). The treatment options offered to obese patients vary based on the degree of obesity and associated co-morbidities as well as the potential side effects of the therapeutic options. For those with moderate forms of obesity, lifestyle interventions including food restriction and increased energy expenditure through physical activity are recommended. As the degree of obesity increases or in the presence of co-morbidities, pharmacotherapy options which work to decrease appetite such as sibutramine or decrease fat absorption such as orlistat may be offered and for the most obese patients, surgical interventions may be considered (Gray et al. 2012; Wyatt 2013). Though pharmacotherapy options have yielded successful results, they are associated with complications such as gastrointestinal problems with orlistat or cardiovascular risk with sibutramine (Gray et al. 2008). Bariatric surgery is associated with significant weight loss (Kral and Näslund 2007). However the most effective techniques involve rerouting the digestive tract. This can lead to malabsorption which can cause nutritional deficiencies if an adequate diet and supplementation regime is not maintained as well as post-operative complications including hemorrhage, staple-line dehiscence, thromboembolism, and death (Runkel et al. 2011). Despite the availability of diverse treatment options, there is evidence 59 M.Sc. Thesis – A. Mayhew; McMaster University – Health Research Methodology of only a modest effect of lifestyle interventions and pharmacotherapy and surgical options are associated with numerous complications, suggesting that preventing opposed to treating obesity may be the best strategy for curbing the obesity epidemic (Gortmaker et al. 2011). An excessive consumption of calories is the main risk factor for obesity with environmental and societal factors encouraging calorie consumption (Young and Nestle 2002). The current “obesogenic” environment is characterized by calorically dense food being inexpensive, abundant, served in large portions (Young and Nestle 2002), and heavily marketed while demands for physical activity decrease (Mitchell et al. 2011; Swinburn et al. 2011). Though the environment is an important contributor to obesity, the inter-individual differences in obesity (Elks et al. 2012) and food behaviors such as energy consumption, macronutrient consumption distribution, food preferences, and satiety responsiveness in the presence of the obesogenic environment can in part be explained by genetic factors (Breen et al. 2006; Hasselbalch et al. 2008; Llewellyn et al. 2012; Cornelis et al. 2014). In addition, heritability studies in twins evidenced a shared genetic component between obesity and food behaviors (Keskitalo et al. 2008b; Llewellyn et al. 2012). This suggests that the genetic architecture of food behaviors and obesity may be at least partially overlapping. Monogenic forms of obesity include both syndromic types in which obesity occurs in conjunction with other symptoms and non-syndromic types in which obesity is the main clinical feature. Both types of monogenic obesity are characterized by severe hyperphagia (Choquet and Meyre 2011b). GWAS and candidate gene studies have identified close to 70 loci associated with obesity-related traits, nine of which (BDNF, NTRK2, LEPR, SH2B1, 60 M.Sc. Thesis – A. Mayhew; McMaster University – Health Research Methodology PCSK1, POMC, MC4R, TUB, SDCCAG8) overlap with monogenic forms of syndromic and non-snydromic obesity (Thorleifsson et al. 2009; Choquet and Meyre 2011a). To date, only a limited number of obesity-predisposing SNPs (FTO, MC4R, BDNF, SH2B1, NEGR1, MTCH2) have been reliably associated with food-related traits (Cecil et al. 2008; Bauer et al. 2009; Stutzmann et al. 2011; Mccaffery et al. 2012; Robiou-du-Pont et al. 2013; Rukh et al. 2013). Though an obesity genotype score consisting of 13 risk alleles was associated with higher body mass index (BMI), it was unexpectedly associated with lower total energy intake and higher intake of fiber in 26,107 Northern European subjects, (Rukh et al. 2013) . A genotype score consisting of 24 risk alleles was not associated with snacking behavior in 7,502 European subjects (Robiou-du-Pont et al. 2013). A recent two-stage genome-wide association meta-analysis for macronutrient intake in more than 70,000 European subjects identified FTO and a new locus (FGF21) not previously associated with obesity as significant contributors to protein and carbohydrate / lipid intake, respectively (Chu et al. 2013; Tanaka et al. 2013). Collectively, these data suggest that the genetic predisposition to polygenic obesity is at best selectively related to food intake and food behavior meaning that other possible mechanisms involved in genetic predisposition to obesity should be explored. The positive association between increased energy intake and BMI is well established (Prentice and Jebb 2004), however some questions still remain such as if increased energy intake is the cause of increased BMI or a consequence of it. Higher total energy intake has been associated with subsequent weight gain in children in longitudinal studies (Berkey et al. 2000) but the association between total energy intake and weight gain 61 M.Sc. Thesis – A. Mayhew; McMaster University – Health Research Methodology across time is controversial in adults (Jørgensen et al. 1995; Halkjaer et al. 2006). This complex pattern of association may relate to the fact that increased BMI results in higher basal metabolic rates and higher energy requirements (Byrne et al. 2012). This question also applies to genetic variants associated both with food-related traits and obesity (Robiou-du-Pont et al. 2013). To gain more insight into the role of obesity predisposing SNPs on energy intake and macronutrient distribution, we investigated the association between 14 obesity predisposing SNPs as well as a genotype score on overall energy intake, macronutrients, different types of fat, using a validated FFQ in 1,850 Canadian subjects of European ancestry. 4.2 Methods 4.2.1 Participants The EpiDREAM study included a total of 24,872 individuals from 191 centres in 21 countries who were screened for eligibility to enter in the DREAM clinical trial (Anand et al. 2012). All individuals who were deemed to be at risk for dysglycemia defined by family history, ethnicity and abdominal obesity, between the ages of 18 to 85 years, were screened using a 75 gram oral glucose tolerance test (OGTT) from July 2001 to August 2, 2003. Detailed methods and description of the study cohort have been described earlier (Anand et al. 2012). We included in the present study 1,850 Canadian subjects of European ancestry having both FFQ and genotypic information available at baseline (Figure 2). All non-Canadians with FFQ data were removed because country specific FFQs were used, limiting the comparability of participants across countries. We excluded participants with >5% of FFQ data not filled out or those with implausible dietary intakes. Self-reported 62 M.Sc. Thesis – A. Mayhew; McMaster University – Health Research Methodology white European ethnicity has been validated using the Eigensoft software (http://genepath.med.harvard.edu/~reich/Software.htm). Samples that failed to cluster with individuals of European ancestry were removed. The EpiDREAM study has been approved by local ethics committee and informed consent was obtained from each subject before participating in the study, in accordance with the Declaration of Helsinki. Figure 2. EpiDREAM Participant Flow Chart 63 M.Sc. Thesis – A. Mayhew; McMaster University – Health Research Methodology 4.2.2 Phenotyping Height (m) and weight (kg) were measured in clinical centers by a trained medical staff. Standing height was measured to the nearest 0.1 cm with the participant looking straight ahead in bare feet and with his/her back against a wall. Weight was measured to the nearest 0.1 kg in light clothing. BMI was calculated as weight in kilograms (kg) divided by height in meters (m) squared. Diet was measured using a validated semiquantitative FFQ previously developed for the SHARE (Study of Health Assessment and Risk Evaluation) study. Pearson correlation coefficients between the diet records and FFQ in the European population ranged from 0.30 for polyunsaturated fat to 0.65 for saturated fat (Kelemen et al. 2003). 4.2.3 Genotyping Buffy coats for DNA extraction have been collected from all willing participants of the EpiDREAM study. DNA has been extracted by the Gentra System. Genotyping was performed using the Illumina CVD bead chip microarray ITMAT Broad Care (IBC) array (Keating et al. 2008). Genotyping was performed at the McGill University and Genome Quebec Innovation Centre using the Illumina Bead Studio genotyping module, version 3.2. Marker with a missing call rate of greater than 10% and individuals with a 3% or greater call rate were removed, as well as marker with a minor allele frequency of less than 0.00001. We selected 14 SNPs that display genome-wide significant association (P<5×108 ) for BMI and / or binary obesity status in the literature and were genotyped on the versions 1 and 2 of the IBC 50K SNP array. The 14 SNPs are: rs1514176 (TNN13K), rs6235 (PCSK1), rs6232 (PCSK1), rs2206734 (CDKAL1), rs2272903 (TFAP2B), rs1211166 64 M.Sc. Thesis – A. Mayhew; McMaster University – Health Research Methodology (NTRK2), rs6265 (BDNF), rs1401635 (BDNF), rs997295 (MAP2K5), rs7203521 (FTO), rs9939609 (FTO), rs1805081 (NPC1), rs2075650 (TOMM40/APOE/APOC1), rs11671664 (GIPR). The 14 SNPs showed no deviation from Hardy-Weinberg equilibrium (HWE) (all P > 0.06, Table 2. The call rate for each of the 14 SNPs was 100%. Gene SNP Risk Allele Major Allele Minor Allele Genotype Count Genotyping Call Rate (%) HWE pvalue TNN13K rs1514176 G A G 650 893 307 100 0.9922 PCSK1 rs6235 C G C 1018 693 139 100 0.1639 PCSK1 rs6232 G A G 1660 187 3 100 0.3389 CDKAL1 rs2206734 C C T 1179 606 65 100 0.2314 TFAP2B rs2272903 G G A 1494 341 15 100 0.3535 NTRK2 rs1211166 A A G 1212 565 73 100 0.4828 BDNF rs6265 G G A 1213 577 60 100 0.3903 BDNF rs1401635 C G C 932 748 170 100 0.2611 MAP2K5 rs997295 T T G 670 885 295 100 0.9230 FTO rs7203521 A A G 746 828 276 100 0.0637 FTO rs9939609 A T A 639 871 340 100 0.1543 NPC1 rs1805081 A A G 662 891 297 100 0.9227 TOMM40/AP OE/APOC1 rs2075650 A A G 1400 413 37 100 0.3140 GIRP rs11671664 G A A 1478 351 21 100 0.9749 Table 2: Genotypic Information for Obesity Predisposing SNPs 4.2.4 Statistical methods Statistical analyses were performed using SPSS (IBM Corp 2011). The overlap of information between nutrition measures was assessed using Pearson correlation. For each of the 14SNPs, the previously identified obesity risk allele was used as the risk allele. 65 M.Sc. Thesis – A. Mayhew; McMaster University – Health Research Methodology Single SNP analyses were performed under the additive model. A genotype score was calculated by summing the alleles predisposing to obesity for the 14 SNPs so that the score ranged from 0 to 28. We used a unweighted score as Janssen et al (2007). previously showed that weighting had no major impact on the score. We constructed multivariate linear regression models to determine the effect of each of the 14 SNPS and the genotype score on BMI in addition to food consumption parameters. The regression models were adjusted for sex, age and BMI. To determine the effect of the relative intake of nutrients independent of caloric intake, nutrient intakes were adjusted for caloric intake by regression analysis (Willett and Stampfer 1986). Two-tailed P-values are presented in this manuscript and P < 0.05 were considered as nominally significant. After applying a Bonferroni’s correction for multiple testing, a p <1.754x10-4 (0.05/285 tests) was considered as significant. QUANTO (Gauderman and Morrison 2001), was used to measure the power of finding an association between individual SNPs and BMI for varying allelic frequencies and beta-coefficients (Figure 3) . 66 M.Sc. Thesis – A. Mayhew; McMaster University – Health Research Methodology A 1 0.9 0.8 Power 0.7 Beta 0.1 0.6 Beta 0.2 0.5 Beta 0.3 0.4 Beta 0.4 0.3 Beta 0.5 0.2 Beta 0.6 0.1 0 0 0.1 0.2 0.3 0.4 0.5 0.6 0.7 0.8 0.9 1 Allele Frequency B 0.2 0.18 0.16 Power 0.14 Beta 0.1 0.12 Beta 0.2 0.1 Beta 0.3 0.08 0.06 Beta 0.4 0.04 Beta 0.5 0.02 Beta 0.6 0 0 0.2 0.4 0.6 0.8 1 Allele Frequency Figure 3. Statistical power for detecting associations between individual SNPs and BMI according to allele frequency and beta-coefficients with a sample size of 1,850 participants. A – Power for testing associations according to risk allele frequency and beta-coefficient, assuming a two-sided P-value of 0.05 unadjusted for multiple testing. B – Power for resting associations according to risk allele frequency and beta-coefficient, assuming a two-sided Pvalue of 1.754x10-4 after adjustment for multiple testing. 67 M.Sc. Thesis – A. Mayhew; McMaster University – Health Research Methodology 4.3 Results Table 3 describes the characteristics of the 1,850 study participants. The different nutrient components (total energy, total fat, saturated fat, monounsaturated fat (MUFA), polyunsaturated fat (PUFA), trans-fat, carbohydrates and protein) were all significantly correlated with each other in the study (Pearson correlation coefficient range 0.311 to 0.986; Table 4). The correlation between carbohydrates and total fat and fat subcomponents was more modest, as well as the correlation between trans-fat and all other nutrient components. BMI was significantly associated with total energy intake as well as all energy-adjusted nutrients (Table 5). All (n=1850) Males (n=643, 34.8%) Females (n=1207, 65.2%) Age 53.07 (+/- 10.579) 55.20 (+/- 10.850) 51.93 (+/- 10.256) BMI (kg/m2) 30.83 (+/-6.441) 30.37 (+/- 5.172) 31.07 (+/- 7.014) Total energy (kcal) 1891.75 (+/- 657.076) 2103.13 (+/- 691.026) 1779.15 (+/- 609.286) Total fat (g/day) 64.90 (+/- 27.354) 72.19 (+/- 30.655) 61.02 (+/- 24.257) Saturated fat (g/day) 22.24 (+/- 10.278) 24.92 (+/- 11.531) 20.82 (+/- 9.237) Monounsaturated fat (g/day) 24.82 (+/- 11.031) 27.90 (+/- 12.405) 23.19 (+/- 9.845) Polyunsaturated (g/day) 9.86 (+/- 4.477) 10.85 (+/-4.979) 9.33 (+/- 4.091) Trans fat (g/day) 0.63 (+/- 0.739) 0.71 (+/- 0.805) 0.591 (+/- 0.699) Carbohydrates (g/day) 241.84 (+/- 91.252) 263.48 (+/- 95.074) 230.31 (+/- 87.016) Protein (g/day) 82.636 (+/- 31.146) 89.11 (+/- 32.606) 79.19 (+/- 29.783) fat Table 3: EpiDREAM Participant Characteristics 68 M.Sc. Thesis – A. Mayhew; McMaster University – Health Research Methodology 0.844 0.819 0.416 0.91 0.882 0.951 0.986 0.918 0.523 0.652 0.844 0.912 0.769 0.463 0.593 0.787 0.936 0.53 0.605 0.816 0.573 0.631 0.774 0.312 0.311 Polyunsaturated Fat Trans Fat 0.711 Carbohydrates Protein All correlations significant at the 0.01 level (two-tailed) Table 4: Pearson Correlations for Unadjusted Nutrient Intakes Association with BMI Energy Total Fat Saturated Fat Monounsaturated Fat Polyunsaturated Fat Trans Fat Carbohydrates Protein Protein Trans Fat 0.819 Monounsaturated Fat Carbohydrates Polyunsaturated Fat 0.878 Saturated Fat Monounsaturated Fat Saturated Fat Total Fat Total Fat Energy Energy Beta SE p-value 0.001 0.057 0.080 0.117 0.243 0.603 -0.011 0.037 2.340E-04 0.012 0.027 0.027 0.060 0.239 0.004 0.010 0.002 3.000E-06 0.003 1.700E-05 4.900E-05 0.012 0.006 3.640E-04 Table 5: Association of Energy and Energy Adjusted Nutrients with BMI 69 M.Sc. Thesis – A. Mayhew; McMaster University – Health Research Methodology 4.3.1 Association of obesity predisposing SNPs and genotype score with BMI Two out of 14 SNPs showed a directionally consistent and nominally significant association with BMI: rs9939609 SNP in FTO (beta = 0.72 ± 0.21, P = 0.001) and rs1514176 in TNNI3K (beta = 0.57 ± 0.21, P = 0.008) (Table 6). The genotype score was also positively associated with BMI (beta / per additional risk allele = 0.14 ± 0.06, P = 0.03). Further adjustment for total energy intake did not modify the association between rs9939609 and rs1514176 SNPs in FTO and TNNI3K or the genotype score and BMI (Table 5). 70 M.Sc. Thesis – A. Mayhew; McMaster University – Health Research Methodology Gene/SNP GIRP rs11671664 Gene Score - TOMM40/A POE/APOC1 - rs2075650 NPC1 rs1805081 - FTO rs9939609 - FTO rs7203521 - MAP2K5 rs997295 - BDNF rs1401635 - BDNF rs6265 - beta 0.571 -0.228 -0.065 0.246 0.003 0.033 -0.055 0.302 -0.071 0.089 0.717 0.053 -0.360 0.336 0.140 SE 0.215 0.237 0.481 0.269 0.356 0.266 0.273 0.229 0.216 0.214 0.210 0.216 0.309 0.343 0.064 p-value 0.008 0.336 0.893 0.360 0.993 0.900 0.842 0.187 0.744 0.678 0.001 0.806 0.244 0.328 0.030 beta 0.552 -0.256 -0.038 0.240 0.028 0.035 -0.089 0.264 -0.061 0.108 0.721 0.041 -0.370 0.308 0.132 SE 0.215 0.236 0.480 0.268 0.355 0.266 0.273 0.229 0.215 0.214 0.210 0.216 0.309 0.343 0.064 p-value 0.010 0.278 0.937 0.371 0.937 0.895 0.743 0.250 0.776 0.613 0.001 0.848 0.231 0.368 0.039 beta 0.018 0.028 -0.016 0.012 -0.015 0.001 0.022 0.026 -0.007 -0.011 -0.001 0.010 0.004 0.025 0.007 SE 0.012 0.013 0.026 0.015 0.019 0.014 0.015 0.012 0.012 0.012 0.011 0.012 0.017 0.019 0.003 p-value 0.115 0.028 0.550 0.411 0.431 0.932 0.138 0.034 0.570 0.331 0.922 0.407 0.827 0.180 0.039 beta 0.011 -0.010 0.000 0.002 -0.004 -0.010 0.018 0.017 -0.007 -0.011 -0.001 0.002 -0.001 0.015 0.001 SE 0.007 0.007 0.015 0.008 0.011 0.008 0.009 0.007 0.007 0.007 0.007 0.007 0.010 0.011 0.002 p-value 0.102 0.197 0.993 0.769 0.715 0.222 0.032 0.020 0.281 0.091 0.881 0.776 0.892 0.177 0.662 beta 0.013 -0.014 0.010 -0.002 -0.011 -0.014 0.016 0.016 0.001 -0.015 -0.007 -0.005 -0.004 0.008 -0.001 SE 0.009 0.010 0.020 0.011 0.015 0.011 0.011 0.009 0.009 0.009 0.009 0.009 0.013 0.014 0.003 p-value 0.149 0.155 0.613 0.828 0.445 0.212 0.164 0.083 0.923 0.096 0.397 0.604 0.757 0.549 0.689 beta 0.013 -0.012 0.001 0.002 -0.004 -0.008 0.021 0.017 -0.014 -0.013 0.004 0.005 0.002 0.020 0.001 SE 0.008 0.009 0.018 0.010 0.013 0.010 0.010 0.008 0.008 0.008 0.008 0.008 0.011 0.013 0.002 71 NTRK2 rs1211166 - TFAP2B rs2272903 - CDKAL1 rs2206734 MUFA - Saturated Fat PCSK1 rs6232 Total Fat - Total Energy Intake PCSK1 rs6235 BMI adjusted for total energy intake - TNN13K rs1514176 BMI M.Sc. Thesis – A. Mayhew; McMaster University – Health Research Methodology PUFA Trans Fat Carbohydrates Protein p-value 0.107 0.187 0.945 0.874 0.742 0.395 0.036 0.046 0.080 0.090 0.571 0.565 0.859 0.107 0.540 beta 0.017 -0.008 -0.012 0.008 0.008 -0.010 0.029 0.024 -0.020 -0.007 0.010 0.007 0.000 0.013 0.004 SE 0.008 0.009 0.019 0.011 0.014 0.010 0.011 0.009 0.008 0.008 0.008 0.008 0.012 0.013 0.003 p-value 0.050 0.403 0.523 0.423 0.565 0.323 0.007 0.008 0.017 0.386 0.223 0.392 0.970 0.346 0.126 beta 0.068 -0.015 0.093 0.003 0.034 -0.090 0.022 0.090 0.004 -0.003 -0.009 -0.013 -0.042 -0.052 0.005 SE 0.031 0.034 0.069 0.039 0.051 0.038 0.039 0.033 0.031 0.031 0.030 0.031 0.045 0.049 0.009 p-value 0.029 0.671 0.178 0.933 0.505 0.019 0.576 0.006 0.889 0.929 0.758 0.678 0.342 0.289 0.558 beta -0.009 0.010 0.002 0.004 -0.002 0.002 -0.009 -0.004 0.005 0.002 -0.001 -0.005 -0.006 -0.001 -0.001 SE 0.005 0.006 0.012 0.007 0.009 0.007 0.007 0.006 0.005 0.005 0.005 0.005 0.008 0.009 0.002 p-value 0.113 0.079 0.860 0.577 0.797 0.758 0.192 0.471 0.350 0.663 0.921 0.337 0.458 0.866 0.679 beta -0.005 0.002 -0.004 0.001 0.001 0.004 0.001 -0.004 -0.011 0.005 0.005 0.005 -0.001 0.002 0.000 SE 0.006 0.007 0.013 0.008 0.010 0.007 0.008 0.006 0.006 0.006 0.006 0.006 0.009 0.010 0.002 p-value 0.433 0.782 0.781 0.944 0.928 0.605 0.873 0.550 0.066 0.363 0.371 0.417 0.865 0.875 0.948 Table 6: The Association of Obesity Predisposing SNPs with BMI and Energy Adjusted Nutrients 72 M.Sc. Thesis – A. Mayhew; McMaster University – Health Research Methodology 4.3.2 Association of obesity predisposing SNPs and genotype score with dietary intake parameters Six out of the 14 SNPs and the genotype score displayed nominally significant associations with at least one energy adjusted dietary intake parameter: rs1514176 (TNN13K) with trans-fat (beta = 0.068 ± 0.031, p = 0.029), rs6235 (PCSK1) with total energy (beta = 0.028 ± 0.013, p = 0.028), rs1211166 (NTRK2) with trans-fat (beta = -0.09 ± 0.038, p = 0.019), rs6265 (BDNF) with total fat (beta = 0.018 ± 0.009, p = 0.032), MUFA (beta = 0.021 ± 0.01, p = 0.036), and PUFA (beta = 0.029 ± 0.011, p = 0.007), rs1401635 (BDNF) with total energy (beta = 0.026 ± 0.012, p = 0.034), total fat (beta = 0.017 ± 0.007, p = 0.020), MUFA (beta = 0.017 ± 0.008, p = 0.046), PUFA (beta = 0.024 ± 0.009, p = 0.008), and trans fat (beta = 0.090 ± 0.033, p = 0.006), rs997295 (MAP2K5) with PUFA (beta = -0.020 ± 0.008, p = 0.017), and the genotype score with total energy (beta/ additional risk allele = 0.007 ± 0.003, p = 0.039). Further adjustment for BMI did not significantly modify any of the relationships (Table 6). 4.4 Discussion This study confirms the association of BMI with total energy intake, macronutrient intake, and the subcomponents of fat as well as the association of rs9939609 (FTO) and rs1514176 (TNN13K), and genotype score with BMI in a North American population of European ancestry. Six of the 14 SNPs as well as the genotype score were nominally associated with at least one of the dietary intake parameters. Of particular interest was the association between two separate SNPs located in or near BDNF (rs6265 and rs1401635), with total fat, MUFA, and PUFA intake with rs1401635 also being associated with total energy and trans-fat intake. The study also found an association between rs6235 (PCSK1) and the genotype score and total energy intake. 73 M.Sc. Thesis – A. Mayhew; McMaster University – Health Research Methodology After applying the Bonferroni correction to adjust for the 285 tests conducted for analysis a p-value <1.754x10-4 was considered significant. After adjustment, only the association between total fat, MUFA, and PUFA intake with BMI remained significant. Because our results are otherwise nominally significant, at least some of them are likely false positive results. However, the literature supports most of our results, though the more novel discoveries require further replication. We replicated findings of the association of FTO (Dina et al. 2007; Frayling et al. 2007; Willer et al. 2009), and TNNI3K (Willer et al. 2009; Hong and Oh 2012; Mccaffery et al. 2012; Cornelis et al. 2014) with BMI. The lack of association of other SNPs with BMI reflects the modest power of the study, supported by the nominal association of the 14 SNP genotype score with BMI. Though we did not find a significant association between either BDNF SNPs with BMI in the current study, the association between BDNF and obesity is well established with BDNF being linked to both monogenic hyperphagic obesity (Gray Diabetes 2006) and polygenic human obesity (Thorleifsson et al. 2009). In mouse models, heterozygous BDNF+/- are hyperphagic and gain significant weight in young adulthood compared to wild type mice (Lyons et al. 1999). Mice which have BDNF eliminated from the brain after birth similarly display hyperphagia, consuming 74% more food and experiencing a 80-150% increase in body weight compared to controls (Rios et al. 2001). Additionally, BDNF (rs925946) has previously been found to be associated with food related behaviours, such as increased snacking (Robiou-du-Pont et al. 2013) and increased energy consumption (rs10767664 and rs6265) (Mccaffery et al. 2012). No previous studies have found an association between BDNF risk variants and fat consumption, however an association between BDNF and an increased number of servings of both dairy products and products from the meat, eggs, nuts, and beans food group was found (Mccaffery et al. 2012). Dairy products as well as meat, eggs, and nuts, can be higher sources of fat in the diet therefore potentially supporting a link 74 M.Sc. Thesis – A. Mayhew; McMaster University – Health Research Methodology between BDNF risk variants and higher fat consumption. Additional evidence of a link between BDNF and fat consumption comes from mice models in which young BDNF mutants experienced premature development of hyperphagia when fed a high fat diet but not when fed a balanced diet (Fox and Byerly 2004). In this study, two BDNF variants were associated with total fat, MUFA, and PUFA consumption reducing the likelihood that the relationship is a spurious result. Similarly to BDNF, PCSK1, is linked to both monogenic hyperphagic obesity (Farooqi et al. 2007) and polygenic forms of obesity (Benzinou et al. 2008). To the author’s knowledge, this study is the first to find an association between PCSK1 and increased energy consumption. Evidence from the monogenic form of obesity involving PCSK1 supports a hypothetical relationship. In the monogenic form of obesity, a total PCSK1 deficiency causes a prohormone convertase 1/3 deficiency leading to extreme hyperphagia because of an inability to cleave prohormones related to metabolism such as pro-insulin or pro-POMC (Creemers et al. 2012; Frank et al. 2013). It is conceivable that other functional variants in PCSK1 could similarly decrease prohormone convertase 1/3 levels, leading to overeating and a milder form of obesity as seen in polygenic forms of obesity. The reduced effect of the functional variants compared to total PCSK1 deficiency may be part of the reason no previous studies have detected a relationship as the effect size is small. Mice models also support the role of prohormone convertase in obesity with a study finding that mice with a novel allele of mouse prohormone convertase (PC1, N222D) experienced increased energy intake and elevated body weight compared to wild type littermates. The mutation is semi-dominant as mice heterozygous for the trait experienced a more mild increase in energy consumption and obesity (Lloyd et al. 2006). 75 M.Sc. Thesis – A. Mayhew; McMaster University – Health Research Methodology The current evidence associating a genotype score with dietary intake parameters is inconclusive. Both (Cornelis et al. 2014) and (Rukh et al. 2013) found that a higher genotype risk score is associated with high BMI, however while (Cornelis et al. 2014) found that the genotype risk score had a positive association with emotional and uncontrolled eating, (Rukh et al. 2013) and (Robiou-du-Pont et al. 2013) found that an increased risk score was associated with a decrease in energy consumption and had no association with snacking respectively. In our study we found that the genotype score was positively associated with both BMI and total energy consumption. One possible explanation for the discrepancy between studies is that while monogenic forms of obesity are always associated with increased energy consumption (Choquet and Meyre 2011a), the association of obesity predisposing SNPs may modulate BMI through other mechanisms than food intake. For example, rs9939609 (FTO) has consistently been shown to interact with high energy or high saturated fat diets to lead to obesity (Ahmad et al. 2011; Corella et al. 2011; Moleres et al. 2012; Phillips et al. 2012). PPARG which encodes peroxisome proliferator-activated receptor y (PPARy), a nuclear receptor involved in fatty acid sensing and the regulation of adipocyte differentiation, lipid metabolism, fat storage, and insulin sensitivity is associated with obesity and BMI and suggests that lipid metabolism may be an important component of obesity (Cecil et al. 2012). Various SNPs located in or near MC4R, a gene involved in monogenic forms of obesity, have been found to be associated with basal metabolic rate (rs11872992), respiratory quotient, fat oxidation, total energy expenditure, insulin resistance, and leptin (SNP – 1385), and total activity levels (SNP – 1704) (Cole et al. 2010). Some obesity SNPs likely work through mechanisms other than increased energy consumption. For example olfactomedin 4 (OLFM4) and homebox protein (HOXB5) are associated with common early-onset obesity. OLFM4 plays a role in immunity function against 76 M.Sc. Thesis – A. Mayhew; McMaster University – Health Research Methodology Helicobacter pylori infection with increased weight being associated with more bacteria and homebox protein (HOXB5), coded for by the HOXB5 gene, is proposed to play a role in gut function with transcription factors increasing after fat loss (Bradfield et al. 2012). However, there is also substantial evidence that some SNPs, in particular FTO are associated with energy consumption independently of BMI (Cecil et al. 2008; Speakman et al. 2008; Timpson et al. 2008; Haupt et al. 2009). Our study found an association between rs1401635 (BDFN), rs1401625 (PCSK1) and the genotype score and total energy consumption supporting the view that obesity predisposing SNPs are causally involved in the regulation of energy intake. Currently, excessive energy intake is considered the primary risk factor for obesity, far more so than decreased physical activity (Speakman and O’Rahilly 2012). People who are genetically predisposed to obesity, either from rare and severe monogenic forms or from common polygenic variants with an accumulation of variants with individual modest effect on disease risk, are much more vulnerable to the effects of the “obesogenic” environment in which food is inexpensive, abundant, served in large portions, and heavily marketed (Mitchell et al. 2011). With the knowledge from this study and previous research, we can conclude that because many people are genetically predisposed to obesity and certain negative food consumption patterns, changes to the accessibility and quality of the food available are required which can be accomplished through changes to policy. Strengths of our study included using a FFQ validated for total energy intake, macronutrients, and three of the four subcomponents of fat we investigated in the study. An ethnically homogenous sample while decreasing the generalizability of our findings, decreases the risk that the FFQ would less accurately estimate food consumption for certain ethnicities and helps to control for culturally specific habits that may relate to obesity. Though a modest sample size limited the statistical power for the study, our nominally significant results are well supported by 77 M.Sc. Thesis – A. Mayhew; McMaster University – Health Research Methodology either prior research or additional biological evidence, decreasing the likelihood that results are spurious (Ioannidis et al. 2008). Additionally, the use of a genotype score is relatively novel. Limitations of this study include using a cross-sectional sample which does not allow for the temporal relationship between energy intake and obesity to be examined in the context of obesity predisposing SNPs, the use of FFQ data opposed to ad libitum tests or dietary recall methods which decreases the accuracy of the food parameter estimates, and the need for some of the novel nominally significant results to be replicated. 4.5 Conclusions In conclusion, our study showed nominally significant associations of rs9939609 (FTO) and rs1514176 (TNN13K), and genotype score with BMI, an association of six of the 14 SNPs and the genotype score with dietary intake parameters. The associations of BDNF (rs6265 and rs1401635), with total fat, MUFA, and PUFA intake with rs1401635 also being associated with total energy and trans-fat intake and rs6235 (PCSK1) and the genotype score and total energy intake in particular warrant further investigation. Our data supports the view that the genetic predisposition of obesity includes some obesity SNPs influencing energy consumption (O’Rahilly and Farooqi 2008). 78 M.Sc. Thesis – A. Mayhew; McMaster University – Health Research Methodology 5.0 An Evolutionary Perspective on Eating Disorders 5.1 Introduction There is an ongoing debate about the causes of eating disorders. It is clear that there is a complex interplay between life experiences, personal characteristics/environmental factors, and genetics. The life experiences that are associated with eating disorders, such as early menarche (BN), high parental expectations, sexual abuse, family dieting, criticism about one’s shape and size, and participation in activities promoting a low fat mass like distance running, swimming, dancing, and modelling (Klein and Walsh 2003) are well established. In addition to life experiences, personal characteristics and environmental factors such as gender, age, birth cohort, ethnicity, and culture are likely important contributors to the development of eating disorders. Despite the high hereditability of eating disorders, estimated to be between 0.28 and 0.76 for AN, 0.30 to 0.83 for BN (Slof-Op ’t Landt et al. 2005), and 0.41 to 0.57 for BED (Thornton et al. 2011), there is very limited evidence of robust association between eating disorders and candidate genes or associations detected through GWAS. The high heritability of eating disorders as well as their relatively high prevalence, at least in Western societies, indicate that eating disorders, or behaviours affiliated with eating disorders, may have previously provided an evolutionary advantage. Using personal characteristics and environmental factors which have been identified as risk factors for eating disorders, different evolutionary theories are investigated. 5.2 Suppression of reproduction and sexual competition Some believe that AN is a method through which females can either supress or delay reproduction to avoid procreating at a time when their offspring will have threatened survival. This 79 M.Sc. Thesis – A. Mayhew; McMaster University – Health Research Methodology would ultimately be an advantage as females who supressed reproduction until more favourable environmental conditions would likely have higher lifetime reproductive success therefore would be more likely to pass on the genes responsible for AN characteristics. The theory also states that through social stress, females can try to supress the reproduction of other females in an attempt to increase the chance of finding a high quality mate and create a better environment for their offspring (Wasser and Barash 1983). While it may be advantageous for dominant females to supress the reproductive capacity of others, Gatward (2007) proposes that it may also be in the best interest of subordinate females to supress their reproduction through restricting food access. Historically, being accepted as part of a group was critical for survival. While weight loss could be used to become more attractive, severe weight loss such as with AN could be interpreted as a sign of subordination and the potential lack of fertility would remove the subordinate female as a threat to the dominant female. If the subordinate female poses no threat to the dominant female, there is no reason for her to be excluded from the group. Another element of suppression of reproduction is in young girls who have not yet reached sexual maturity. Maintaining a lower weight may delay menarche allowing them to pursue other activities such as academics in modern times before having children (Surbey 1987). The theories involving suppression of reproduction are limited however, because they do not explain the hyperactivity seen in AN patients, the denial of the seriousness of their disease and distorted body image, or the presence of AN in males (Kardum et al. 2008). A theory of inter-female competition excluding the concept of purposeful suppressed reproduction has also been developed (Abed 1998). The hypothesis states that from an evolutionary perspective, the ability to restrict food access may have been beneficial for females in order to attract potential partners. A “nubile” shape consisting of a low waist to hip ratio is a 80 M.Sc. Thesis – A. Mayhew; McMaster University – Health Research Methodology sign of reproductive potential because it indicates youthfulness as well as no current pregnancy. Being more attractive would increase a female’s likelihood of obtaining and maintaining a high quality partner, therefore providing an advantage to her offspring explaining the high heritability of eating disorders. This theory translates well into modern times where females have been delaying having children until later in life, therefore females may decrease their weight in order to stay competitive with younger females. However, despite the potential for the prevalence of eating disorders to be increasing over time (Hoek and van Hoeken 2003; Preti et al. 2009), the disease still predominantly affects young females with an peak in incidence between 10 to 19 years (Hoek and van Hoeken 2003; Currin et al. 2005; Son et al. 2006) which is not the demographic hypothesized to be trying to lose weight to compete with younger females. As with the suppression of reproductive potential theories, there are limitations to the hypothesis including a lack of applicability to males, the potentially incorrect assumption that a thin body type was/is universally desirable, and that the theory was developed in the context of modern observations. The suppression of reproduction theory and the sexual competition theory are also contradictory. The suppression of reproduction theory indicates that anorectic tendencies decrease fertility while the sexual competition theory indicates that anorectic tendencies will increase the quality of mate and subsequent offspring and not have a negative consequence on fertility. 5.3 Adapted to flee famine hypothesis and rogue hibernation The adapted to flee famine hypothesis (AFFH) provides an explanation for a possible adaptive advantage to what are now known as symptoms of AN. It proposes that food restricting behaviour, hyperactivity, and denial of seriousness of weight loss previously enabled migration during periods of local food insecurity. These characteristics would allow individuals to ignore their near starvation state and continue to be physically active until reaching a more food secure 81 M.Sc. Thesis – A. Mayhew; McMaster University – Health Research Methodology area. These adaptive mechanisms would be positively selected for as only those capable of reaching food secure areas would be able to survive and reproduce, explaining the high heritability of eating disorders (Guisinger 2003). Elaborating upon this theory, Scolnick and Mostofsky (2014) propose that in today’s food abundant environment, people with AN are trapped in a state of semi-starvation, hypothermia, and hyperactivity because their metabolic pathways are falsely signaling that they are in a food scare environment. This is based upon the metabolic similarities between AN and another physiological adaptation to food scarcity, mammalian hibernation. Mammalian hibernation involves a decreased metabolic rate, hypothermia, and a switch in the metabolic fuel supply from carbohydrates to lipids and ketones. Hibernation allows the animal to survive cold, nutrient depleted winters. The cycle of weight accumulation pre-hibernation, weight loss during hibernation, and subsequent weight gain in spring after hibernation mimic periods of binging and purging in AN (Scolnick and Mostofsky 2014). For both the AFFH and rogue hibernation theories of AN, it is proposed that in modern food secure environments, the traits of restricting food consumption, hyperactivity, and denial of seriousness of weight loss can be turned on by dieting or other contextual reasons for decreasing food consumption (Guisinger 2003; Scolnick and Mostofsky 2014). The idea that motivations other than the sole intention to lose weight can initiate AN may be important to consider in an international context. Keel and Klump (2003) determined that if weight concerns were removed as diagnostic criteria for AN, the prevalence would be similar in Western and nonWestern countries. Both of these theories are supported by epidemiological information on AN. For example the peak incidence of AN is between the years of 10 and 19 (Hoek and van Hoeken 2003; Currin et al. 2005; Son et al. 2006). Fertility declines as age increases (Nelson et al. 2013) therefore it 82 M.Sc. Thesis – A. Mayhew; McMaster University – Health Research Methodology would be most advantageous for young females capable of bearing children in the future to be able to relocate during times of food insecurity. Similarly, AN is mostly found in females with a ratio of 10 to 20 females diagnosed for each male (Favaro et al. 2003; Hoek and van Hoeken 2003; Currin et al. 2005; Hoek 2006; Wade et al. 2006; Hudson et al. 2008; Preti et al. 2009; Marques et al. 2011; Heaner and Walsh 2013; Meczekalski et al. 2013). A far greater number of females would be required to re-establish a society compared to males as female’s capacity to reproduce is comparatively far lower. In our review of the ethnic and cultural differences in the prevalence of eating disorders we concluded that differences in prevalence of AN in different ethnicities likely have a strong cultural component, but that there is the possibility that underlying genetic differences between ethnicities may also be a contributing factor. The studies conducted have been limited by the challenges of separating culture and genetics and there is no real evidence confirming or denying the possible role of genetic differences between ethnicities influencing the risk of developing eating disorders. However, if genetic differences are found to be an important risk factor for the development of eating disorders, the evidence would fit in well with the AFFH. People of European and African have some distinct genetic differences. It is possible that the genes promoting AN characteristics were more advantageous in European ancestors compared to African ancestors because of the vastly different climates and consequent patterns of food availability. The migration patterns of Africans versus all other ethnic groups, including Europeans, may have selected for different genes as well. Europeans migrated significantly further than Africans which may have made genes allowing people to continue to migrate despite food scarcity a much more significant advantage. This may explain why AN is much more prevalent in people of European descent compared to other ethnicities. 83 M.Sc. Thesis – A. Mayhew; McMaster University – Health Research Methodology Culture has an important role in modern day AN. To receive the diagnosis of AN, an individual must have a preoccupation with their weight which is likely a cultural construct stemming from the beauty ideal of a thin shape. Keel and Klump (2003) found that if preoccupation with body weight is removed as a diagnostic criterion, a similar proportion of the general and psychiatric populations in Western and non-Western countries are found to have the disease. Using the AFFH which suggests that food restriction causes the metabolic changes leading to the symptoms of AN, regardless of if the goal is to lose weight or not, other food restriction behaviours like fasting, or decreased food consumption because of stress could also bring on the disease. However, in these cases, the disease would not be considered AN because the individuals would not have a weight preoccupation. Further support for the AFFH and rogue hibernation theories comes from the general lack of association of AN with genes related to serotonin, dopamine, and opioids which all play roles in the pleasure and enjoyment of food. Though levels of serotonin, dopamine, opioids, and related metabolites and receptors appear to be altered in people in AN, the lack of evidence showing a link between relevant genes and the disease indicate that the abnormal physiological state may be a result of the disease, rather than the cause of it. 5.4 Thrifty gene hypothesis Fewer theories exist about how symptoms of BN and BED previously could have been an evolutionary advantage compared to AN. The leading theory relates to the thrifty genotype hypothesis which focuses on how historically, having extra fat stores were protective. Adipocytes are used for fat storage in the form of triglycerides. Having these fat stores play a role in helping to avoid malnutrition, regulate reproduction, and allow for survival during variations in the energy supply. Both hunter/gathers as well as agricultural societies experienced fluctuations in the food supply. However hunter/gathers were able to migrate more easily decreasing the fluctuation in 84 M.Sc. Thesis – A. Mayhew; McMaster University – Health Research Methodology energy available to them which relates back to the AFFH for AN (Wells 2006). Mass immigration is also thought to have selected for thrifty genes because people are often escaping food scarce conditions and may be exposed to more food scarcity through the immigration process and intense competition for food (Wells 2006). As agricultural societies developed, people were less able to relocate to avoid famine and as a result, “thrifty” genes were selected for (Neel 1962, 1999; Wells 2006). These genes which previously promoted survival in food insecure environments are no longer protective in the modern “obesogenic” environment, characterized by food that is inexpensive, abundant, served in large portions, and heavily marketed while demands for physical activity decrease (Wells 2006; Mitchell et al. 2011; Swinburn et al. 2011). While the thrifty gene hypothesis provides an explanation for the underlying predisposition to obesity, it alone does not explain many of the disordered eating patterns observed. In particular, it does not explain AN, which has an underlying advantage of allowing people to function well despite having little energy available to them. However, the development of BN involving a cycle of binging and purging, BED which is similar to BN but without purging after periods of binging, as well as people with AN who also binge (Klein and Walsh 2003) may in part be explained by the thrifty genotype hypothesis. Both BN and BED involve binging on food, estimated to be between 3000 – 4500kcal in a binge episode (Wolfe et al. 2009). It is plausible that the loss of control and drive to eat, particularly energy dense foods, is caused by the same genes that previously promoted fat accumulation and food consumption according to the thrifty gene hypothesis. The historical food context may also help explain the benefits of binge eating. In hunter gather societies, a successful hunt would provide a large quantity of food that would be shared. Being able to consume large amounts of food in a short time span would be beneficial to individuals, allowing them to have a greater portion of the available food. Furthermore, before the 85 M.Sc. Thesis – A. Mayhew; McMaster University – Health Research Methodology invention of refrigeration and preservation techniques, food had a relatively short life span and being able to consume large quantities before the food became unsafe to eat would have been advantageous. The purging behaviour seen in some people with AN and those with BN may be a modern iteration of the historical benefits of purging. Prior to the development of the obesogenic environment, it is unlikely that many people were able to find enough food to binge on to gain an undesirable amount of weight and thinness may not have been idealized as it now is in Western society. However, with the current overabundance of food available it is very easy for people to gain weight and most people with BN are within normal weight ranges (Kaye et al. 2000) while those with BED are overweight or obese (Reichborn-Kjennerud et al. 2004; Field et al. 2012). It is possible that people with BN, who by definition of the disease are preoccupied and concerned about their weight (American Psychiatric Association 2013) are driven by the genes that would be associated with the thrifty gene hypothesis to eat, however because of societal pressures to be thin have adopted purging behaviours to compensate. Though the inter-female competition theory is specific to AN (Abed 1998), it is possible that the same motivation to attract a high quality partner that is proposed to cause AN may also cause purging behaviour in BN. Support of the role of the thrifty gene hypothesis in conjunction with inter female competition in the development of BN and BED can be found by comparing and contrasting the diseases. Applying the thrifty gene concept, we hypothesize that the root causes of binging are the same in BN and BED. There is a biological drive to consume food when available which is a relic from the period of time in human evolution when food was scarce. The significant difference between BN and BED is that BN involves purging in addition to binging which may be a cultural linked behaviour or a combination of AN and BED present in an individual. Evidence supporting 86 M.Sc. Thesis – A. Mayhew; McMaster University – Health Research Methodology this theory comes from the risk factors for the two diseases. The risk of developing BN increases in family environments in which parents have high expectations and focus on weight as well as when individuals are involved with activities which promote a lean shape (Klein and Walsh 2003). This suggests that people with BN have been taught that being overweight is bad and use purging to avoid it. The ratio of males to females with BN is lower than that of BED. While both males and females are influenced by media exposure for beauty ideals, there is evidence that it affects females more, particularly the ideal of being thin (Hausenblas et al. 2013). Therefore, it is logical that if BN and BED both stem from the same genetic predisposition to over consume food, more females would have BN rather than BED because of a greater impact of societal standards of beauty. The peak incidence of developing the disease provide further evidence. For BN the peak incidence is between 17.0 and 19.7 years of age (Fornari et al. 1994; Favaro et al. 2003; Hudson et al. 2008) whereas BED appears to be more equally distributed across the lifespan (Kinzl et al. 1999; Alegria et al. 2007; Grucza et al. 2007). Biologically, the need to store energy to survive future famines would continue to occur across the lifespan, however concerns about being at an ideal weight to attract an appropriate partner would be more relevant at the younger ages seen in BN patients. We found that compared to BN, BED is more equally distributed across ethnicities (Smith et al. 1998; Striegel-Moore et al. 2003; Alegria et al. 2007; Nicdao et al. 2007; Marques et al. 2011; Taylor et al. 2013). This could in part be because weight preoccupation is predominantly a Western concern (Pike et al. 2001; Simpson 2002), therefore people from non-Western countries who binge may not feel the same drive to purge compared to their Western counterparts. The thrifty genotype has been focused upon in this thesis, however it is important to note that the thrifty genotype is a controversial theory to explain obesity. Speakman has been one of the most vocal opponents of the thrifty genotype hypothesis. His main arguments include that 87 M.Sc. Thesis – A. Mayhew; McMaster University – Health Research Methodology mortality during times of famine is not enough to lead to genetic selection nor are the people who often die during famine, the elderly and the young the ones that would strongly influence the gene pool and that historical patterns of famine are incompatible with a selective hypothesis (Speakman 2008). Others have agreed with Speakman that the mortality rates in famine are not sufficient to explain the possible genetic selection, however argue the effect of famine on fertility selection can explain the genetic selection. Speakman’s argument that the historical patterns of famine are incompatible with the thrifty genotype hypothesis has been strongly refuted, including by Neel himself (Prentice et al. 2008). The original thrifty genotype hypothesis states that the selective pressure for thrifty genes would have existed during the Paleolithic era in hunter gather societies (Neel 1962). It is generally accepted that famines and seasonal food shortages are much more applicable to agricultural societies in comparison to hunter gathers societies (Prentice et al. 2008). As an alternative to the thrifty genotype hypothesis, Speakman proposed what is now referred to as the drifty gene hypothesis proposing that obesity was previously selected against by the risk of predators. The upper limit of human weight was limited by predators as people who were too large to run away or adequately protect themselves would not survive. Speakman proposes that with the development of social behaviour, weapons, and fire the risk of predators was significantly decreased and that the distribution of body fatness increased because there were no longer any selective pressures to not have a higher BMI. Because the selective pressures to maintain a minimum weight were still in place, such as immune function and decreased risk of starvation, random mutations and drifting gradually increased the distribution of BMI in the population (Speakman 2007). Another evolutionary theory of obesity that has been proposed is the thrifty phenotype which proposes that maternal nutrition, low birth weight, and a prediction of low food sources cause an adaptive insulin resistance (Hales and Barker 2013; Levitan and Wendland 2013). 88 M.Sc. Thesis – A. Mayhew; McMaster University – Health Research Methodology The thrifty phenotype theory applies to diabetes reasonably well, however is limited for explaining obesity in developed countries. Very few mothers experience malnutrition during pregnancy despite the high prevalence of obesity in developed countries (Levitan and Wendland 2013). A final theory called the thrifty epigenotype combines the thrifty genotype and thrifty phenotype. It postulates that through genetic canalization, genes coding for a thrifty genotype have been well preserved in the genome across all ethnicities and in all individuals. The theory also suggests the epigenetics, changes in gene activity that are not caused by alternations of DNA sequences but DNA methylation, histone modifications, remodeling of chromatin, and non-coding RNAs, is a critical element which is in line with the thrifty genotype theory indicating that the fetal environment influences adult health (Stöger 2008). 5.5 Summary of evolutionary theories Of the evolutionary theories proposed, the AFFH best explains AN. Historically, having the motivation to be physically active, avoiding a preoccupation with food during caloric scarcity, and denying the seriousness of weight loss would enable individuals to migrate from food insecure to food secure areas and consequently increase their chances of survival and future reproduction. Though the people most commonly afflicted by AN are from Western countries where food scarcity is generally not an issue, Scolnick and Mostofsky (2014) proposed that behaviour such as dieting could trigger the same physiological adaptations as living in a food scarce environment. The diagnosis of AN today requires an individual to be preoccupied with their weight. This may be best viewed as a contributing factor to the development of the disease, rather than a symptom of it. The AFFH is supported by the general patient characteristics of AN. AN mostly occurs in young females of child bearing age which would be the most desirable individuals to be able to flee from famine as more females than males required to re-establish the 89 M.Sc. Thesis – A. Mayhew; McMaster University – Health Research Methodology population. While the contribution of genetics and culture to ethnic differences in the prevalence of AN is still unresolved, if there are genetic differences the AFFH also can explain why AN is predominantly found in White populations (Keel and Klump 2003; Striegel-Moore et al. 2003; Taylor et al. 2013). The evolutionary pressure on Europeans in regards to food would be different compared to other regions of the world, therefore the genes promoting AN characteristics may have been more beneficial to Europeans compared to other ethnicities. The lack of association of genes related to serotonin, dopamine, and opioids which have been heavily explored because of their role in the pleasure and enjoyment of food indicate that altered levels of these neurotransmitters could be a result of the disease, rather than the cause of it, supporting the AFFH proposition that the biochemical changes are in response to famine. The thrifty gene hypothesis was initially developed to explain obesity. It may also explain the overeating behaviour seen in BN and BED. Historically, accumulating fat during times of food abundance would be beneficial to survival during periods of food insecurity as the fat could be used as energy stores. However, in the food abundant environments that people in the Western world live in today, the genes allowing for the overconsumption of food when it was available may be now encouraging chronic overconsumption. This can explain the binging seen in BN and BED, however to explain the purging seen in BN, an elaboration of the theory in necessary. The purging behaviour can be explained by the desire to stay thin despite the binging episodes. BN is predominantly found in Western cultures where thinness is idealized while BED is seen more equally across ethnicities. We propose that there could be common genes associated with BN and BED, with the desire to be thin determining which disease category individuals fall within based on purging behaviour. 90 M.Sc. Thesis – A. Mayhew; McMaster University – Health Research Methodology Examining the evolutionary theories of eating disorders can help future gene identification efforts by focusing on novel candidate genes as well as guiding the development of biological evidence to support the findings of GWAS. With the increasing use of GWAS approaches, evolutionary theories of eating disorders can also help determine new phenotypes to use as outcome variables. Genetic studies to date have provided limited success, which may be because they are focusing on symptoms of the disease, especially in AN, rather than the causes of it. For AN, abnormal neurotransmitter and hormone levels have been widely observed, but genetic association studies have been widely negative. However, if the altered neurotransmitter and hormone levels are a result of a physiological adaptation to low food consumption rather than one of the causes of the low food consumption as we propose, then we would not expect genes involved with the production and reception of those neurotransmitters and hormones to be altered. We propose that genes related to metabolism, specifically genes relating to mammalian hibernation in other species, would be more beneficial to investigate compared to genes involved in the production of neuropeptides. The genes relating to neuropeptide production in BN and BED may still be relevant, however because BED is equally prevalent worldwide, it indicates that the genes promoting an increased consumption of food may be more broadly found with almost undetectable effect sizes. Though looking at genes related to metabolism may lead to a further understand the genetic architecture of eating disorders, there is also the possibility that hormones relevant to eating disorders are yet to be discovered. Investigating metabolites, transcription factors, and protein profiles in people with eating disorders and comparing these to levels after recovery of the disease or between episodes as well as with controls may help to identify novel biomarkers and pathways in the etiology of eating disorders. 91 M.Sc. Thesis – A. Mayhew; McMaster University – Health Research Methodology 5.6 Coexistence of Anorexia Nervosa and Bulimia Nervosa in binge/purge subtype Anorexia Nervosa The evolutionary theories of eating disorders clearly distinguish between AN and the other two eating disorders, BN and BED. However, there is a significant amount of overlap between the diseases, particularly when looking at the subtypes of AN. AN(R) (Anorexia Nervosa restrictive subtype) is the diagnosis given to people who weigh less than 85% of what they should weight and consume a limited amount of calories per day while AN(BP) (Anorexia Nervosa binge/purge) is the diagnosis given to people who weigh less than 85% of their ideal weight and go through cycles of binging and purging (American Psychiatric Association 2013). AN(BP) is very similar to BN, except that individuals with BN do not meet the weight cut offs for AN. In addition to the similarities of some of the diagnostic criteria, there is a significant amount of cross-over between those with AN(R), AN(BP), and BN. In seven years of follow-up, 49% of women initially diagnosed with AN crossed over between AN subtypes and 34% crossed over from AN to BN. Of those initially diagnosed with AN(R) 55% changed diagnostic categories to AN(BP) and 10% crossed over to a BN diagnosis. Women also crossed over from a diagnosis of BN to AN, with 14% crossing over to AN(BP) and 4% then crossing over to AN(R) (Eddy et al. 2013). Below, we propose theories as to why the traits seen in BN, AN(R), and AN(BP) overlap from a genetic perspective. 5.6.1 Binge eating as protection against Anorexia Nervosa AN is considered the most dangerous of all mental disorders with more than 10% of patients dying from the disease (Hoek 2006). Theoretically, the denial of nutrients to the body seen in the restrictive subtype of AN could switch on a pathway encouraging the consumption of calories, explaining the binging behaviour seen in people with the binge/purge subtype of AN. 92 M.Sc. Thesis – A. Mayhew; McMaster University – Health Research Methodology The cross-over of patients from the subcategories of AN supports this theory when considering that more people cross over from the restrictive subtype to the binge/purge subtype (Eddy et al. 2013). Similarly, approximately 25 to 30% of people receiving treatment for BN have been found to previously have been diagnosed with AN while only 5% of people initially diagnosed with BN being diagnosed with either subtype of AN (Kaye et al. 2000). This supports that the restrictive behaviour seen in AN(R) may be difficult to maintain and consequently cross over to AN(BP) when the drive to eat becomes overwhelming. The cross-over of individuals from AN(BP) to BN shows that the binging behaviour may slowly lead to weight gain, as the only significant diagnostic difference between AN(BP) and BN is weight with people with AN being less than 85% of their ideal weight (American Psychiatric Association 2013). However, this theory ignores that binge eating is seen outside of the context of AN in both BN and BED and that some people with AN(R) do not cross-over to AN(BP) during the duration of their disease. 5.6.2 Accumulation of independent genes leading to binge eating and Anorexia Nervosa Taking into account the limitations of the previous theory as to why binge/purging behaviour coexists with AN, we have hypothesized that it is possible that independent genes lead to the binge/purging behaviour seen in BN and the extreme weight loss seen in AN. Through random segregation within populations, it is possible that some people cumulate both the genes predisposing to AN and the genes predisposing to BN. This theory is unlikely though because both AN and BN are relatively rare diseases. Using an estimated prevalence of 0.3 to 3.0% of AN in females (Favaro et al. 2003; Hoek and van Hoeken 2003; Currin et al. 2005; Hoek 2006; Wade et al. 2006; Hudson et al. 2008; Preti et al. 2009; Marques et al. 2011; Heaner and Walsh 2013; Meczekalski et al. 2013) and estimated prevalence of 0.88 to 4.6% for BN in females (Favaro et al. 2003; Hoek and van Hoeken 2003; Hoek 2006; Wade et al. 2006; Hudson et al. 93 M.Sc. Thesis – A. Mayhew; McMaster University – Health Research Methodology 2008; Keski-Rahkonen et al. 2009; Preti et al. 2009; Smink et al. 2012), the prevalence of both AN and BN, therefore the AN(BP) subtype should be between 0.0026 and 0.138% while the actual prevalence of AN(BP) is likely somewhere between 0.15 to 1.5% of women based on half of the people with AN having the binge/purge subtype (Eddy et al. 2013). Therefore, we can conclude that because the actual prevalence of AN(BP) is higher than would be expected from accumulation of independent genes leading to BN and AN, the genes associated with the individual diseases are either in linkage disequilibrium or the same genes are causing the two different diseases. 5.6.3 Mutations/structural gene variants with opposite effects in the same gene lead to AN or BN The theory that the accumulation of independent genes causing binging behaviour and extreme weight loss explain the cross-over of diagnostic criteria in eating disorders is likely incorrect based on the much higher prevalence of AN(BP) in the population compared to theoretical prevalence of the genes crossing over. As discussed in the evolutionary theories section, the ability to consume large amounts of food when readily available may have been advantageous leading to the selection of genes that now promote binge eating in the modern food abundant environment (Neel 1962, 1999; Wells 2006; Wells et al. 2006; Mitchell et al. 2011; Swinburn et al. 2011). The ability to also be highly functioning with minimal caloric intake may also have been beneficial as it would enable migration from food insecure areas to more food secure areas promoting genes that may now lead to what is known as AN (Guisinger 2003; Scolnick and Mostofsky 2014). It is possible that mutations or structural variants such as deletion/duplication, gain of function/loss of function, gain of expression/loss of expression in the same genes may lead to AN and binging behaviour. This ties in with the evolutionary 94 M.Sc. Thesis – A. Mayhew; McMaster University – Health Research Methodology theories as these genes may have been positively selected for in the past under different environmental conditions and people with both types of mutations may have been favoured. This could lead to partial linkage disequilibrium between mutations in the population, leading to the high prevalence of the mixed phenotypes. In the past, people possessing both the loss of function and gain of function mutations may not have suffered from any negative side effects allowing for the transmission of the genes on to future generations. It is feasible that the mixed phenotypes are now only problematic in the obesogenic environment. Weight concerns are a relatively modern concept and dieting to lose weight could trigger the metabolic changes allowing for survival despite low caloric consumption. However, if the same genes are also causing binging behaviour, individuals may purge in order to balance the conflicting biological drives to survive with minimal caloric consumption and to take advantage of the food available to them. The possibility of a single gene having both loss of function and gain of function mutations is supported by recent findings on MC4R and the 16p locus where deletion/loss of function mutations lead to hyperphagic obesity while duplications/gain of function mutations lead to leanness and food-related phenotypes (Geller et al. 2004). To test this hypothesis, a genelevel association using a whole-exome sequencing approach could be conducted in patients with AN(R), AN(BP), BN, BED, and healthy controls could be conducted. 5.6.4 Mutations in nearby genes result in partial linkage disequilibrium of Anorexia Nervosa and binge eating traits Similar to the theory that the same genes may contain loss of function/gain of function mutations causing the cross-over of traits seen in eating disorders is the theory that the genes coding for the different characteristics of eating disorders are in genes located near each other, 95 M.Sc. Thesis – A. Mayhew; McMaster University – Health Research Methodology 5.6.5 Summary of the role of genetics in the coexistence of Anorexia Nervosa and Bulimia Nervosa in binge/purge subtype Anorexia Nervosa We have proposed four theories for why there is an overlap of characteristics seen in AN(R), AN(BP), BN, and BED. 1. Binge eating is used as a protective mechanism against starvation in people with AN who are not meeting their energy requirements 2. AN(BP) occurs in individuals who have both the independent genes for AN and the independent genes for binge eating 3. Mutations/structural gene variants with opposite effects in the same gene lead to AN or BN 4. Mutations in nearby genes result in partial disequilibrium of the genes for AN and the genes for binge eating causing a higher than expected number of people to display the mixed phenotype AN(BP) than would be expected if the genes were not in partial linkage disequilibrium We found that it is unlikely that that binge eating is purely a protective mechanism against AN because it doesn’t account for the high proportion of people who binge eat without having prior starvation as seen in BN and BED. We also discount the theory that AN(BP) occurs in individuals who have the genes for both AN(R) and binge eating as the prevalence of AN(BP) far surpasses what would be expected if the genes for AN(R) and binge eating are independent of each other. It is feasible that both mutations/structural gene variants in the same gene causing opposite effects and that mutations in nearby genes resulting in partial disequilibrium for the genes causing AN(R) and binge eating can explain the overlap of phenotypes seen in AN(BP). 96 M.Sc. Thesis – A. Mayhew; McMaster University – Health Research Methodology 5.7 Conclusions We combined the evolutionary perspective of eating disorders with the possibility of the genetic overlap causing mixed phenotypes, and the epidemiological evidence of differences in prevalence of eating disorders in different ethnicities and cultures to create a framework suggesting under which conditions each eating disorder will occur (Figure 4). In this framework, we propose that there are separate genes predisposing individuals to AN(R) and genes that predispose individuals to binge eating. These genes are likely to overlap because they are in partial linkage disequilibrium, either because mutations/structural variants within the same gene code for loss of function/gain of function mutations or because the genes are located close to each other. Therefore, a greater number of people would have characteristics of both diseases than would be expected if the genes were independent. Thus three genotypic categories were created, people with only AN(R) genes, people with only binge eating genes, and people with genes predisposing to both diseases. Another critical element of the framework is the differences in prevalence of the eating disorders seen in different cultures/ethnicities. Because of the challenges in untangling the effect of culture versus ethnicity it is impossible to determine how much of the between-ethnicity variability in the prevalence of eating disorders is attributable to genetics versus how much is attributable to culture. However, it is well established that White women are more concerned about weight have lower weight ideals in comparison to Black women (Pike et al. 2001; Gluck and Geliebter 2002; Simpson 2002) and it is very feasible that at least some of the greater prevalence of AN and BN in White females is because they feel an increased pressure to be thin. The pressure to be thin is not exclusively related to ethnicity and consequently in our framework we created a binary variable of either the presence or absence of pressure to be thin. 97 M.Sc. Thesis – A. Mayhew; McMaster University – Health Research Methodology The two independent variables consisting of the three genotypic groups and the presence or absence of the pressure to be thin create six categories. Individuals with only the genes predisposing to AN(R) will develop AN(R) if there is sufficient pressure to be thin using the elaboration of AFFH and rogue hibernation theories which indicate that dieting can cause the metabolic shift leading to the diseases. In the absence of weight concerns, an individual would not develop AN(R) despite having predisposing genes unless starvation was achieved through famine, fasting, or other non-weight related reasons why food consumption may be lowered. People with only the genes predisposing to binge eating in the presence of the pressure to be thin will be at risk for developing BN because genetically they are driven to eat however have a strong desire to maintain a normal weight and therefore use inappropriate compensatory behaviours. Without the pressure to maintain a certain weight, only BED will occur because the individual is not driven to compensate for the overconsumption of calories. For those with the mixed genotype, in the presence of having a weight preoccupation AN(BP) occurs because the individual cannot avoid binging on food, however is highly motivated to maintain a minimum weight and has the genetic advantage of being able to be functional despite their low energy intake. People with the mixed phenotype who do not feel pressure to be thin will be at increased risk for BED because they are driven to binge, yet do not feel the need to compensate for the overconsumption of calories. 98 M.Sc. Thesis – A. Mayhew; McMaster University – Health Research Methodology Genes predisposing Genes predisposing to Anorexia Nervosa to AN (restrictive (restrictive subtype) subtype) and genes predisposing to binge eating Genes predisposing to binge eating Presence of pressure to be thin Anorexia Nervosa (restrictive subtype) Anorexia Nervosa (binge/purge subtype) Bulimia Nervosa Absence of pressure to be thin No disease – unless Anorexia Nervosa is triggered by factors other than weight loss, such as lack of food availability or fasting Binge Eating Disorder Binge Eating Disorder Figure 4: Framework for the risk of developing an eating disorder based on genotypic category and presence or absence of pressure to be thin This framework provides a simplified view of the interaction of the potential genetics of eating disorders and the environment, specifically the pressure to be thin. There are many other factors that contribute to the risk of developing eating disorders not captured in the model such as epigenetics, gene by gene interactions, gene by environment interactions in addition to the pressure of being thin, any potential genetic factors which contribute to the predisposition of being more sensitive to the pressure of being thin, and a plethora of other environmental factors. 99 M.Sc. Thesis – A. Mayhew; McMaster University – Health Research Methodology 6.0 Ethical Considerations The investigation of genetic susceptibility of diseases and the subsequent research to determine the biological pathways through which the genes are functioning is working towards personalized medicine. The concept of personalized medicine involves using an individual’s unique genetics as well their life context to predict which diseases or medical conditions they will suffer from and ideally prevent the disease from occurring, as well as providing targeted treatment plans if a disease is not preventable (Joyner and Prendergast 2014). Examples of genotyping being used to help health care practitioners decide on the treatment or management of disease exist today. Screening for the BRCA1 and BRCA2 genes in females with familial breast cancer allows for increased screening or preventative measures to be taken if necessary (Foulkes and Shuen 2013). Phenylketonuria, an inability to convert phenylalanine to tyrosine caused by mutations in the gene encoding for phenylalanine hydroxylase can be detected by blood tests and genetic testing can confirm the diagnosis. If identified at birth, phenylketonuria can be effectively managed, however if not it causes severe mental retardation amongst other issues (van Spronsen 2010). Despite the current successes using genetic information to improve human health, the ability to sequence the entire human genome has created an ethical debate about how to best protect the privacy of individuals who participate in genomic research (Callier et al. 2014). A specific ethical consideration of genetic research is how to handle disclosure to the individual (Li and Meyre 2014)) and to the family (Rothstein 2013). Telling an individual that they have an increased risk for a medical condition, particularly one for which preventative measures or treatments may be unavailable could cause the participant stress. On the other hand, knowing about late onset, non-preventable diseases may allow people to plan reproductive decisions and finances accordingly (Li and Meyre 2014). However, not telling participants if they are at risk could also 100 M.Sc. Thesis – A. Mayhew; McMaster University – Health Research Methodology be ethically unsound because of an individual’s right to know that information and take whatever actions they see fit. More complicated is if an individual involved in a study is found to have a genetic disorder that could be passed on to their family. In some cases the participant may be contacted to determine if they would like to tell family members but in cases where the participant has passed away, an ethical dilemma occurs. There are no current guidelines indicating if disclosing the information to the family is legal, ethical, or what the consequences could be (Rothstein 2013). Researchers can in part avoid this situation by asking about the release of information to family members in life and in death on the consent form, however in participants who do not want the information shared, there can still be an ethical dilemma if the lives of family members could be saved by knowing the information (Rothstein 2013). Beyond the concerns of how genetic information can be used, there are also issues about for whom genetic testing will be available. The cost to sequence the whole human genome has rapidly dropped from approximately $2.7 billion for the first genome sequenced to $5000 in June 2013. As genetic testing becomes more affordable, physicians will need to start determining who needs genetic testing versus which individuals it is medically unnecessary for to avoid using health care dollars inappropriately. Another consequence of the increasing affordability of genetic testing is that individuals can seek out private testing. This could create system in which people of higher socioeconomic status could be in a position to receive better health care. However, the traditional health care system has not yet fully transitioned to genomic medicine and only 10% of American doctors feel comfortable using approved genetic tests. Though patients want doctors to interpret their genetic testing results, many of them also do not feel that doctors are sufficiently trained to do the task. (Li and Meyre 2014). 101 M.Sc. Thesis – A. Mayhew; McMaster University – Health Research Methodology Specific to the research included in this thesis, the only ethical consideration is keeping the data collected from participants confidential which has been built into the study design of EpiDREAM. The EpiDREAM study was approved by the local ethics committee and informed consent was obtained from each subject before participating in the study, in accordance with the Declaration of Helsinki. The individual and collective effect size of obesity predisposing genes on obesity and food consumption patterns is extremely modest. Therefore, the conclusions of this study while supporting the role of genetics in obesity risk also are not significant enough to warrant telling participants or their families about their slightly enhanced risk for obesity. As the field of personalized medicine advances forward and genetic testing becomes more frequent, it is important that guidelines for both research and clinical applications are developed to take the advancements into consideration. For genetics research, it is especially important to determine what results will be passed on to the participants and/or their families and to have this information included as part of the informed consent process. Continued guideline development will be necessary protect individuals from genetic discrimination from insurance companies or potential employers and what information from genetic testing should be provided to individuals and their families. For clinical applications, there will need to be a sufficient number of genetic counsellors available, or extra training provided to relevant physicians, to discuss the implications of the results of the genetic testing. 102 M.Sc. Thesis – A. Mayhew; McMaster University – Health Research Methodology 7.0 Conclusions and Future Work The first half of this thesis focused on the association of 14 obesity predisposing SNPs and a gene score with dietary consumption parameters including daily intakes of total energy, total fat, saturated fat, trans fat, monounsaturated fat, polyunsaturated fat, carbohydrates and protein. Our results confirmed the positive association of two of the obesity predisposing SNPs as well as the gene score with BMI. Adjusting for energy did not significantly change the association, indicating that these SNPs are associated with BMI independent of how much food is consumed, supporting that an increase in energy consumption is not the only biological mechanism leading to obesity. We also found statistically significant relationships between six of the obesity predisposing SNPs and the gene score with at least one energy adjusted dietary parameter, specifically with total energy, total fat, and subcategories of fat. Adjusting these relationships for BMI did not significantly attenuate the relationships demonstrating that participants were not consuming more energy or having higher fat diets because of their increased weight. The most significant finding was the novel association of two separate SNPs located in or near BDNF (rs6265 and rs1401635) with total fat, MUFA, and PUFA intake, with rs1401635 also being associated with total energy and trans fat intake. Biological support of the relationship comes from the role of BDNF in monogenic forms of obesity which are characterized by hyperphagia and mouse models in which dietary fat moderates the relationship between mice with BDNF mutations and hyperphagia. The association of rs6235 (PCSK1) and the genotype score with total energy intake were similarly novel with biological evidence supporting PCSK1 because it is also a gene affiliated with monogenic forms of obesity and that a total PCSK1 deficiency leads to extreme hyperphagia. The second half of this thesis discussed the evolutionary history of eating disorders. Using current epidemiological evidence, we propose that the AFFH best explains AN because it takes 103 M.Sc. Thesis – A. Mayhew; McMaster University – Health Research Methodology into account the weight loss element, increased energy expenditure, and ethnic/cultural differences observed in people with AN. Theories involving suppression of reproduction and sexual competition do not take the increased energy expenditure into account. The sexual competition theories have a further flaw as they indicate that often it is older females who attempt to lose weight to compete with younger females. However, eating disorders, particularly AN are much more prevalent in young females compared to old females. Furthermore, the suppression of fertility that can occur with severe eating disorders does not account for the high heritability of the diseases as those with supressed reproduction would have a less opportunity to reproduce and pass on the genes. We also propose that BN and BED may not be distinct diseases but instead categories of the same disease. Historically, a drive to consume food when available may have been protective during times of food scarcity, however in today’s calorie abundant environment it is an undesirable trait. Both BN and BED feature binge eating as a diagnostic criteria. People with BN use inappropriate compensatory behaviours, often purging, after binges and people with BED do not use inappropriate compensatory behaviours. Evidence that BED and BN have the same basic cause comes from the ethnic differences. The prevalence of BED is relatively equal across ethnicities whereas BN is mostly seen in Western cultures where thinness is idealized. Therefore it could be the socially constructed strive for thinness causing the purging, rather than a unique genetic determinant. The much higher prevalence of AN in Western cultures may also be explained by environmental factors encouraging the drive for thinness. The AFFH does not involve the preoccupation with food which is now part of the AN diagnostic criteria, but instead proposes that the metabolic changes seen in AN came about because of food scarcity. Voluntary food restriction 104 M.Sc. Thesis – A. Mayhew; McMaster University – Health Research Methodology in the form of dieting because of a preoccupation with weight may trigger the same biological response. Together, the two components of this thesis provide evidence supporting that obesity and disordered eating patterns have a strong genetic basis. However, both sections also indicate that there is a need to widen the scope of biological mechanisms and genes being investigated in the context of obesity and eating disorders. Most research conducted in obesity promoting SNPs is focused on excessive energy intake, however the lack of association of most of the obesity promoting SNPs and the modest association of the gene score with energy consumption point to alternative biological mechanisms, such as alterations in metabolism. Despite the high likelihood that there are genetically linked features other than food consumption that are associated with weight, there is still the need of adequately powered studies to confirm the currently known associations of obesity predisposing SNPs with food behaviour as well as detect unknown associations. Using novel populations such as obese people who are successfully losing weight through caloric restriction, or those who are gaining weight for GWAS may also help identify relevant genes. Having a better understanding of the behaviours that SNPs are modifying obesity through will help determine the specific biological pathways that are being impacted. This information will be crucial in the development of preventative strategies for obesity. Great strides have been made in conducting GWAS for obesity in ethnicities other than Europeans, however studies focusing on nutrient consumption patterns and other factors that could be causing obesity are still mostly limited to Europeans. The evidence indicates that some obesity predisposing genes are ethnicity specific. If the ultimate goal of understanding the genetics of obesity is to come up with strategies to avoid weight gain, researchers need to have the information required to create ethnic specific programs. As the field of obesity genetics grows, more emphasis will also need to 105 M.Sc. Thesis – A. Mayhew; McMaster University – Health Research Methodology be placed on understanding gene by gene interactions, gene by environment interactions, and epigenetics. Creating consortiums by pooling large amounts of genetic and phenotypic data from multiple research groups with help to facilitate this research by providing the sample sizes required to have adequately powered studies. To better understand the genetics of eating disorders, many critical questions need to be answered. Not specifically pertaining to genetics is the need for better phenotyping of eating disorders. In our review, we propose that weight preoccupation which is a requirement for the diagnosis of AN may not a relevant diagnostic criteria. Using the adapted to flee famine hypothesis, any food restriction could bring on the metabolic changes seen in AN. In Western cultures, dieting may be the most frequent and relevant instigator but evidence shows that AN occurs world wide, regardless of the idealization of thinness. To determine if the theory that the preoccupation with thinness is a Western ideal instead of an intrinsic part of eating disorders is correct, biochemical data including hormones, metabolites, transcription factors, and protein profiles should be compared between patients who present with all symptoms of AN except for a preoccupation with weight and patients who have all symptoms of AN including a preoccupation with weight. If the biochemical changes are similar in the two populations, this would indicate that the diagnostic criteria for AN should be broadened. While the treatment for people with and without weight occupations may be different, widening the diagnostic criteria may allow for more people in need to receive treatment. Similarly, more research is required to determine if purging, the only difference between BN and BED, is purely because of a desire to be thin, or if there are other biological mechanisms that induce purging. For genetic studies, the next step should be changing the focus from looking at genes associated with neuropeptides and hormones which may only be a symptom of the disease to 106 M.Sc. Thesis – A. Mayhew; McMaster University – Health Research Methodology looking at genes that are linked to metabolism. Small sample sizes are a significant problem in eating disorder research as many people attempt to hide the disease. Establishing clearer phenotypes and subdividing into categories such as people with AN who have weight preoccupations and those who do not have weight preoccupations could increase sample sizes as would collaborations. Because eating disorders are extreme abnormalities in eating patterns, if common gene variants are found to be associated with the diseases, then they are likely to be good candidate genes to investigate for obesity as well, particularly genes associated with BN and BED. Future candidate genes could also be discovered by studying hormones, metabolites, transcription factors, and protein profiles in specific phenotypes, such as people who have successfully recovered from eating disorders versus those who have not. If genes associated with AN can be correctly identified and the biological mechanisms deduced, there is the possibility that the findings could be used to not only help treatment people with AN, but also those who are obese. For example, if the genes that allow people with AN to avoid fixation with food despite low caloric intake can be identified and the biochemical pathway they act through be determined, pharmacotherapy options capitalizing on the information could be developed. The continued decrease in cost of next-generation methods of genome sequencing and the creation of consortiums providing access to genetic information for extremely large sample sizes will also play a significant role in determining the genetic architecture of eating disorders. The large sample sizes will provide adequate power for detecting the small effect sizes seen in polygenic forms of the diseases. However, for GWAS methods to be the most successful, eating disorder phenotypes need to be clearly defined and the same phenotypes used in multiple studies to allow for potential replication of findings. 107 M.Sc. Thesis – A. Mayhew; McMaster University – Health Research Methodology The moderate to high heritability of obesity and eating disorders in conjunction with the findings that the shared environment has little effect highlight the need for environmental changes to help people lead healthier lives. Obesity specifically is often viewed as the fault of the individual but understanding that weight is under genetic control and the way people are raised has little effect on their weight point to the need for stronger policies to help curb the obesogenic environment. Many people who are obese, as well as those who have BN and BED, struggle to moderate what and how much they are eating, showing a preference for unhealthy options. If these options were less readily available, or if health information was more accessible in conjunction with higher health literacy, people may be more equipped to make healthy choices. AN is a more complex disease, but if the desire to be thin is causing the voluntary restriction in food intake prompting the majority of cases of the disease in Western countries, there is a strong argument to invest more in changing the social environment to accept bodies of all shapes and sizes. For future research of both obesity and eating disorders, better defining phenotypes, taking advantage of large consortium data, and investigating novel hormones, metabolites, transcription factors, and protein profiles will be critical in better understanding the diseases. Novel phenotypes should also be investigated as the current missing heritability can be partially attributed to only looking at a limited range of phenotypes, such as just obese people rather than looking at people gaining and losing weight. 108 M.Sc. Thesis – A. Mayhew; McMaster University – Health Research Methodology 8.0 References Abed R. The sexual competition hypothesis for eating disorders. Br J Med Psychol. 1998;71:525–47. Abizaid A, Gao Q, Horvath TL. Thoughts for food: brain mechanisms and peripheral energy balance. Neuron. 2006 Sep 21;51(6):691–702. Ahmad T, Lee I-M, Paré G, Chasman DI, Rose L, Ridker PM, et al. Lifestyle interaction with fat mass and obesity-associated (FTO) genotype and risk of obesity in apparently healthy U.S. women. Diabetes Care. 2011 Mar;34(3):675–80. Akkermann K, Kaasik K, Kiive E, Nordquist N, Oreland L, Harro J. The impact of adverse life events and the serotonin transporter gene promoter polymorphism on the development of eating disorder symptoms. J Psychiatr Res. Elsevier Ltd; 2012 Jan;46(1):38–43. Alegria M, Woo M, Cao Z, Torres M, Meng X, Striegel-moore R. Prevalence and correlates of eating disorders in Latinos in the United States. Int J Eat Disord. 2007;40:S15–S21. American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5th ed. Arlington, Virginia: American Psychiatric Association; 2013. Anand SS, Dagenais GR, Mohan V, Diaz R, Probstfield J, Freeman R, et al. Glucose levels are associated with cardiovascular disease and death in an international cohort of normal glycaemic and dysglycaemic men and women: the EpiDREAM cohort study. Eur J Prev Cardiol. 2012 Aug;19(4):755–64. Ando T, Ishikawa T, Hotta M, Naruo T, Okabe K, Nakahara T, et al. No association of brainderived neurotrophic factor Val66Met polymorphism with anorexia nervosa in Japanese. Am J Med Genet. 2012 Jan;159B:48–52. Ando T, Komaki G, Naruo T, Okabe K, Takii M, Kawai K, et al. Possible role of preproghrelin gene polymorphisms in susceptibility to bulimia nervosa. Am J Med Genet. 2006 Dec 5;141B:929–34. Asai M, Ramachandrappa S, Joachim M, Shen Y, Zhang R, Nuthalapati N, et al. Loss of function of the melanocortin 2 receptor accessory protein 2 is associated with mammalian obesity. Science (80- ). 2013 Jul 19;341:275–8. Atalayer D, Gibson C, Konopacka A, Geliebter A. Ghrelin and eating disorders. Prog NeuroPsychopharmacology Biol Psychiatry. Elsevier B.V.; 2013 Jan 10;40:70–82. Bachner-Melman R, Lerer E, Zohar AH, Kremer I, Elizur Y, Nemanov L, et al. Anorexia nervosa, perfectionism, and dopamine D4 receptor (DRD4). Am J Med Genet. 2007 Sep 5;144B:748–56. 109 M.Sc. Thesis – A. Mayhew; McMaster University – Health Research Methodology Baik J-H. Dopamine signaling in reward-related behaviors. Front Neural Circuits. 2013 Jan;7(152). Bailer UF, Frank GK, Henry SE, Price JC, Meltzer CC, Becker C, et al. Serotonin transporter binding after recovery from eating disorders. Psychopharmacology (Berl). 2007 Dec;195(3):315–24. Bariohay B, Roux J, Tardivel C, Trouslard J, Jean A, Lebrun B. Brain-derived neurotrophic factor/tropomyosin-related kinase receptor type B signaling is a downstream effector of the brainstem melanocortin system in food intake control. Endocrinology. 2009 Jun;150(6):2646–53. Barry D, Clarke M, Petry NM. Obesity and its relationship to addictions: is overeating a form of addictive behavior? Am J Addit. 2009;18(6):439–51. Barry DT, Grilo CM, Masheb RM. Gender differences in patients with binge eating disorder. Interrnational J Eat Disord. 2002;31:63–70. Bastard J-P, Feve B. The secretory face of the adipose cell: A trbiute to two queens, leptin and adiponectin. Biochimie. 2012;94(10):2063–190. Bauer F, Elbers CC, Adan RAH, Loos RJF, Onland-moret NC, Grobbee DE, et al. Obesity genes identified in genome-wide association studies are associated with adiposity measures and potentially with nutrient-specific food preference 1 – 3. Am J Clin Nutr. 2009;90(3):951–9. Bello NT, Hajnal A. Dopamine and binge eating behaviors. Pharmacol Biochem Behav. 2011;97(1):25–33. Benzinou M, Creemers JWM, Choquet H, Lobbens S, Dina C, Durand E, et al. Common nonsynonymous variants in PCSK1 confer risk of obesity. Nat Genet. 2008 Aug;40(8):943– 5. Bergen a W, van den Bree MBM, Yeager M, Welch R, Ganjei JK, Haque K, et al. Candidate genes for anorexia nervosa in the 1p33-36 linkage region: serotonin 1D and delta opioid receptor loci exhibit significant association to anorexia nervosa. Mol Psychiatry. 2003 Apr;8:397–406. Bergen AW, Yeager M, Welch R a, Haque K, Ganjei JK, van den Bree MBM, et al. Association of multiple DRD2 polymorphisms with anorexia nervosa. Neuropsychopharmacology. 2005 Sep;30:1703–10. Berkey CS, Rockett HRH, Field AE, Gillman MW, Frazier L, Camargo CA, et al. Activity , Dietary Intake , and Weight Changes in a Longitudinal Study of Preadolescent and Adolescent Boys and Girls Lindsay Frazier , Carlos A . Camargo , Jr , MD and Graham A . Colditz The online version of this article , along with updated information. Pediatrics. 2000;105(56). 110 M.Sc. Thesis – A. Mayhew; McMaster University – Health Research Methodology Boomsma D, Busjahn A, Peltonen L. Classical twin studies and beyond. Nat Rev Genet. 2002 Nov;3(11):872–82. Bradfield JP, Taal HR, Timpson NJ, Scherag A, Lecoeur C, Warrington NM, et al. A genomewide association meta-analysis identifies new childhood obesity loci. Nat Genet. 2012 May;44(5):526–231. Brandys MK, Kas MJH, van Elburg A a, Ophoff R, Slof-Op’t Landt MCT, Middeldorp CM, et al. The Val66Met polymorphism of the BDNF gene in anorexia nervosa: new data and a meta-analysis. World J Biol Psychiatry. 2013 Aug;14:441–51. Brandys MK, Slof-Op’t Landt MCT, van Elburg A a, Ophoff R, Verduijn W, Meulenbelt I, et al. Anorexia nervosa and the Val158Met polymorphism of the COMT gene: meta-analysis and new data. Psychiatr Genet. 2012 Jun;22:130–6. Branson R, Potoczna N, Kral JG, Lentes K-U, Hoehe MR, Horber FF. Binge eating as a major phenotype of melanocortin 4 receptor gene mutations. N Engl J Med. 2003 Mar 20;348(12):1096–103. Bray G a, Paeratakul S, Popkin BM. Dietary fat and obesity: a review of animal, clinical and epidemiological studies. Physiol Behav. 2004 Dec 30;83(4):549–55. Van den Bree MB, Eaves LJ, Dwyer JT. Genetic and environmental influences on eating patterns of twins aged >/=50 y. Am J Clin Nutr. 1999 Oct;70(4):456–65. Breen FM, Plomin R, Wardle J. Heritability of food preferences in young children. Physiol Behav. 2006 Jul 30;88(4-5):443–7. Brewerton TD, Lesem MD, Kennedy A, Garvey WT. Reduced plasma leptin concentrations in bulimia nervosa. Psychoneuroendocrinology. 2000 Oct;25:649–58. Brewerton TD, Lydiard RB, Laraia MT, Shook JE, Ballenger JC. CSF beta-endorphin and dynorphin in bulimia nervosa. Am J Psychiatry. 1992 Aug;149(8):1086–90. Brown KMO, Bujac SR, Mann ET, Campbell D a, Stubbins MJ, Blundell JE. Further evidence of association of OPRD1 & HTR1D polymorphisms with susceptibility to anorexia nervosa. Biol Psychiatry. 2007 Feb 1;61:367–73. Brownley KA, Berkman ND, Sedway JA, Lohr KN, Bulik CM. Binge eating disorder treatment: A systematic review of randomized controlled trials. Int J Eat Disord. 2007;40:337–48. Bruins-Slot L, Gorwood P, Bouvard M, Blot P, Adès J, Feingold J, et al. Lack of association between anorexia nervosa and D3 dopamine receptor gene. Biol Psychiatry. 1998 Jan 1;43:76–8. 111 M.Sc. Thesis – A. Mayhew; McMaster University – Health Research Methodology Brunkwall L, Ericson U, Hellstrand S, Gullberg B, Orho-melander M, Sonestedt E. Genetic variation in the fat mass and obesity-associated gene (FTO) in association with food preferences in healthy adults. Food Nutr Res. 2013;57:20028. Bulloch JM, Daly CJ. Autonomic nerves and perivascular fat: Interactive mechanisms. Pharmacol Ther. Elsevier Inc.; 2014 Feb 18;143:61–73. Bush WS, Moore JH. Chapter 11: Genome-wide association studies. PLoS Comput Biol. 2012 Jan;8(12):e1002822. Byrne NM, Wood RE, Schutz Y, Hills a P. Does metabolic compensation explain the majority of less-than-expected weight loss in obese adults during a short-term severe diet and exercise intervention? Int J Obes (Lond). Nature Publishing Group; 2012 Nov;36(11):1472–8. Cai G, Cole S a, Bastarrachea R a, Bastarrachea-Sosa R a, Maccluer JW, Blangero J, et al. Quantitative trait locus determining dietary macronutrient intakes is located on human chromosome 2p22. Am J Clin Nutr. 2004 Nov;80(5):1410–4. Calati R, De Ronchi D, Bellini M, Serretti A. The 5-HTTLPR polymorphism and eating disorders: a meta-analysis. Int J Eat Disord. 2011 Apr;44(3):191–9. Calle EE, Rodriquez C, Walker-Thurmond K, Thun MJ. Overweight, obesity, and mortality from cancer in a prospectively studied cohort of U.S. adults. New Engl J Med. 2003;348(17):1625–38. Callier S, Husain R, Simpson R. Genomic data-sharing: what will be our legacy? Front Genet. 2014 Jan;5:34. Do Carmo JM, Silva AA, Dubinion J, Sessums PO, Sabira H, Wang Z, et al. Control of metabolic and cardiovascular function by the leptin-brain melanocortin pathway. IUBMB Life. 2013;65(8):201–7. Carnell S, Haworth CM a, Plomin R, Wardle J. Genetic influence on appetite in children. Int J Eat Disord. 2008 Oct;32(10):1468–73. Carter JC, Fairburn CG. Cognitive-behavioral self-help for binge eating disorder: A controlled effectiveness study. J Counsulting Clin Psychol. 1998;66(4):616–23. Cassin SE, von Ranson KM. Personality and eating disorders: a decade in review. Clin Psychol Rev. 2005 Nov;25(7):895–916. Castellini G, Ricca V, Lelli L, Bagnoli S, Lucenteforte E, Faravelli C, et al. Association between serotonin transporter gene polymorphism and eating disorders outcome: a 6-year follow-up study. Am J Med Genet. 2012 Jul;159B:491–500. 112 M.Sc. Thesis – A. Mayhew; McMaster University – Health Research Methodology De Castro JM. Genetic influences on daily intake and meal patterns of humans. Physiol Behav. 1993 Apr;53(4):7777–82. De Castro JM, Lilenfeld LRR. Influence of heredity on dietary restraint, disinhibition, and perceived hunger in humans. Nutr. 2005 Apr;21(4):446–55. Cecil J, Dalton M, Finlayson G, Blundell J, Hetherington M, Palmer C. Obesity and eating behaviour in children and adolescents: contribution of common gene polymorphisms. Int Rev Psychiatry. 2012 Jun;24(3):200–10. Cecil JE, Tavendale R, Watt P, Hetherington MM, Palmer CNA. An obesity-associated FTO gene variant and increased energy intake in children. N Engl J Med. 2008;359:2558–66. Cellini E, Nacmias B, Brecelj-anderluh M, Bellodi L, Boni C, Di D, et al. Case – control and combined family trios analysis of three polymorphisms in the ghrelin gene in European patients with anorexia and bulimia nervosa. Psychiatr Genet. 2006;700:51–2. Chan LF, Webb TR, Chung T-T, Meimaridou E, Cooray SN, Guasti L, et al. MRAP and MRAP2 are bidirectional regulators of the melanocortin receptor family. Proc Natl Acad Sci U S A. 2009 Apr 14;106(15):6146–51. Choquet H, Meyre D. Genomic insights into early-onset obesity. Genome Med. 2010 Jan;2(36). Choquet H, Meyre D. Genetics of obesity: What have we Learned? Curr Genomics. 2011 a May;12(3):169–79. Choquet H, Meyre D. Molecular basis of obesity: current status and future prospects. Curr Genomics. 2011 b May;12(3):154–68. Chu AY, Workalemahu T, Paynter NP, Rose LM, Giulianini F, Tanaka T, et al. Novel locus including FGF21 is associated with dietary macronutrient intake. Hum Mol Genet. 2013 May 1;22(9):1895–902. Chung WK. An overview of monogenic and syndromic obesities in humans. Pediatr Blood Cancer. 2012;58(1):122–8. Cole SA, Butte NF, Voruganti VS, Cai G, Haack K, Jr JWK, et al. Evidence that multiple genetic variants of MC4R play a functional role in the regulation of energy expenditure and appetite in Hispanic. 2010;22. Cooke LJ, Haworth CM, Wardle J. Genetic and environmental influences on children’s food neophobia. Am J Clin Nutr. 2007;86:428–33. Corander MP, Coll AP. Melanocortins and body weight regulation: Glucocorticoids, agoutirelated protein and beyond. Eur J Pharmacol. 2011;1(11):111–8. 113 M.Sc. Thesis – A. Mayhew; McMaster University – Health Research Methodology Corella D, Arnett DK, Tucker KL, Kabagambe EK, Tsai M, Parnell LD, et al. A high intake of saturated fatty acids strengthens the association between the fatt mass and and obesityassociated gene and BMI. J Nutr. 2011;141:2219–25. Cornelis MC, Rimm EB, Curhan GC, Kraft P, Hunter DJ, Hu FB, et al. Obesity susceptibility loci and uncontrolled eating, emotional eating and cognitive restraint behaviors in men and women. Obesity. 2014 May;22(5):135–41. Creemers JWM, Choquet H, Stijnen P, Vatin V, Pigeyre M, Beckers S, et al. Heterozygous mutations causing partial prohormone convertase 1 deficiency contribute to human obesity. Diabetes. 2012 Feb;61(2):383–90. Currin L, Schmidt U, Treasure J, Jick H. Time trends in eating disorder incidence. Br J Psychiatry. 2005 Feb;186:132–5. Dardennes RM, Zizzari P, Tolle V, Foulon C, Kipman A, Romo L, et al. Family trios analysis of common polymorphisms in the obestatin/ghrelin, BDNF and AGRP genes in patients with Anorexia nervosa: association with subtype, body-mass index, severity and age of onset. Psychoneuroendocrinology. 2007 Feb;32(2):106–13. Davis C, Levitan RD, Yilmaz Z, Kaplan AS, Carter JC, Kennedy JL. Binge eating disorder and the dopamine D2 receptor: genotypes and sub-phenotypes. Prog NeuroPsychopharmacology Biol Psychiatry. Elsevier Inc.; 2012 Aug 7;38(2):328–35. Dina C, Meyre D, Gallina S, Durand E, Körner A, Jacobson P, et al. Variation in FTO contributes to childhood obesity and severe adult obesity. Nat Genet. 2007 Jun;39(6):724–6. Dmitrzak-Weglarz M, Moczko J, Skibinska M, Slopien A, Tyszkiewicz M, Pawlak J, et al. The study of candidate genes related to the neurodevelopmental hypothesis of anorexia nervosa: classical association study versus decision tree. Psychiatry Res. Elsevier; 2013 Mar 30;206(1):117–21. Doche ME, Bochukova EG, Su H, Pearce LR, Keogh JM, Henning E, et al. Human SH2B1 mutations are associated with maladaptive behaviors and obesity. J Clin Invest. 2012;122(12):4732–6. Dolezalova R, Lacinova Z, Dolinkova M, Kleiblova P, Haluzikova D, Housa D, et al. Changes of endocrine function of adipose tissue in anorexia nervosa: comparison of circulating levels versus subcutaneous mRNA expression. Clin Endocrinol (Oxf). 2007 Nov;67(5):674–8. Dougkas A, Yaqoob P, Givens DI, Reynolds CK, Minihane AM. The impact of obesity-related SNP on appetite and energy intake. Brit J Nutr. 2013 Sep 28;110(6):1151–6. Dubois L, Diasparra M, Bédard B, Kaprio J, Fontaine-Bisson B, Pérusse D, et al. Geneenvironment contributions to energy and macronutrient intakes in 9-year-old children: 114 M.Sc. Thesis – A. Mayhew; McMaster University – Health Research Methodology results from the Quebec Newborn Twin Study. Physiol Behav. Elsevier Inc.; 2013 Jul 2;119:30–7. Dudbridge F, Gusnanto A. Estimation of significance thresholds for genomewide association scans. Genet Epidemiol. 2008 Apr;32(3):227–34. Eddy KT, Dorer DJ, Franko DL, Tahilani K, Thompson-Brenner H, Herzog DB. Diagnostic crossover in Anorexia Nervosa and Bulimia Nerovsa: implications for the DSM-V. Am J Psychiatry. 2013;165:245–50. Elks CE, den Hoed M, Zhao JH, Sharp SJ, Wareham NJ, Loos RJF, et al. Variability in the heritability of body mass index: a systematic review and meta-regression. Front Endocrinol (Lausanne). 2012 Jan;3:29. Fairburn CG, Cooper Z, Doll H a, Norman P, O’Connor M. The natural course of bulimia nervosa and binge eating disorder in young women. Arch Gen Psychiatry. 2000 Jul;57(7):659–65. Fairburn CG, Harrison PJ. Eating disorders. Lancet. 2003 Feb 1;361(9355):407–16. Faith MS, Heo M, Keller KL, Pietrobelli A. Child food neophobia is heritable, associated with less compliant eating, and moderates familial resemblance for BMI. Obesity. 2013 Aug;21(8):1650–5. Faith MS, Keller KL, Johnson SL, Pietrobelli A, Matz PE, Must S, et al. Familial aggregation of energy intake in children. Am J Clin Nutr. 2004 May;79(5):844–50. Faith MS, Rhea SA, Corley RP, Hewitt JK. Genetic and shared environmental influences on children’s 24-h food and beverage intake: sex differences at age 7 y. Am J Clin Nutr. 2008;87:903–11. Farooqi IS, Volders K, Stanhope R, Heuschkel R, White A, Lank E, et al. Hyperphagia and early-onset obesity due to a novel homozygous missense mutation in prohormone convertase 1/3. J Clin Endocrinol Metab. 2007 Sep;92(9):3369–73. Favaro A, Ferrara S, Santonastaso P. The spectrum of eating disorders in young women: A prevalence study in a general population sample. Psychosom Med. 2003 Jul 1;65(4):701–8. Field AE, Sonneville KR, Micali N, Crosby RD, Swanson S a, Laird NM, et al. Prospective association of common eating disorders and adverse outcomes. Pediatrics. 2012 Aug;130(2):e289–295. Finucane MM, Stevens GA, Cowan MJ, Danaei G, Lin JK, Paciorek CJ, et al. National, regional, and global trends in body-mass index since 1980: systematic analysis of health examination surveys and epidemiological studies with 960 country-years and 9·1 million participants. Lancet. Elsevier Ltd; 2011 Feb 12;377(9765):557–67. 115 M.Sc. Thesis – A. Mayhew; McMaster University – Health Research Methodology Fisher JO, Cai G, Jaramillo SJ, Cole S a, Comuzzie AG, Butte NF. Heritability of hyperphagic eating behavior and appetite-related hormones among Hispanic children. Obesity. 2007 Jun;15(6):1484–95. Fontaine KR, Redden DT, Wang C, Westfall AO, Allison DB. Years of life lost due to obesity. J Am Med Assoc. 2003;289(2):187–93. Fornari VM, Braun DL, Sunday SR, Sandberg DE, Matthews M, Chen I, et al. Seasonal patterns in eating disorder subgroups. Compr Psychiatry. 1994;35(6):450–6. Foulkes WD, Shuen AY. In brief: BRCA1 and BRCA2. J Pathol. 2013 Aug;230(4):347–9. Fox EA, Byerly MS. Physiological Regulation of Appetite A mechanism underlying matureonset obesity : evidence from the hyperphagic phenotype of brain-derived neurotrophic factor mutants. 2004;47907:994–1004. Frank GR, Fox J, Candela N, Jovanovic Z, Bochukova E, Levine J, et al. Severe obesity and diabetes insipidus in a patient with PCSK1 deficiency. Mol Genet Metab. The Authors; 2013;110(1-2):191–4. Franko DL, Keshaviah A, Eddy KT, Krishna M, Davis MC, Keel PK, et al. A longitudinal investigation of mortality in anorexia nervosa and bulimia nervosa. Am J Psychiatry. 2013 Aug 1;170(8):917–25. Frayling TM, Timpson NJ, Weedon MN, Zeggini E, Freathy RM, Lindgren CM, et al. A common variant in the FTO gene is associated with body mass index and predisposes to childhood and adult obesity. Science (80- ). 2007 May 11;316:889–94. French SA, H EL, JEffery RW, Blundell JE, Wardle J. Eating behavior dimensions. Associations with energy intake and body weight. A review. Appetite. 2012;59(1):541–9. Gaesser GA. Carbohydrate quantity and quality in relation to body mass index. J Am Diet Assoc. 2007 Oct;107(10):1768–80. Gamero-Villarroel C, Gordillo I, Carrillo JA, García-Herráiz A, Flores I, Jiménez M, et al. BDNF genetic variability modulates psychopathological symptoms in patients with eating disorders. Eur Child Adolesc Psychiatry. 2013 Nov 29; Gatward N. Anorexia nervosa: an evolutionary puzzle. Eur Eat Disord Rev. 2007 Jan;15(1):1– 12. Gauderman J, Morrison J. QUANTO. Los Angeles, California: Department of Preventive Medicine, University of Southern California; 2001. 116 M.Sc. Thesis – A. Mayhew; McMaster University – Health Research Methodology Geller F, Reichwald K, Dempfle A, Illig T, Vollmert C, Herpertz S, et al. Melanocortin-4 receptor gene variant I103 is negatively associated with obesity. Am J Hum Genet. 2004 Mar;74(3):572–81. Gervasini G, Gordillo I, García-Herráiz A, Flores I, Jiménez M, Monge M, et al. Influence of dopamine polymorphisms on the risk for anorexia nervosa and associated psychopathological features. J Clin Psychopharmacol. 2013 Aug;33(4):551–5. Ghaderi A, Scott B. Prevalence, incidence and prospective risk factors for eating disorders. Acta Psychiatr Scand. 2001 Aug;104(2):122–30. Gluck ME, Geliebter A. Racial/ethnic differences in body image and eating behaviors. Eat Behav. 2002 Jan;3(2):143–51. Golan D, Rosset S. Accurate estimation of heritability in genome wide studies using random effects models. Bioinformatics. 2011 Jul 1;27(13):i317–23. Gortmaker SL, Swinburn BA, Levy D, Carter R, Mabry PL, Finegood DT, et al. Changing the future of obesity: science, policy, and action. Lancet. Elsevier Ltd; 2011 Aug 27;378(9793):838–47. Gorwood P. The human genetics of anorexia nervosa. Eur J Pharmacol. 2003 Nov 7;480:163–70. Gorwood P. Eating disorders, serotonin transporter polymorphisms and potential treatment response. Am J Pharmacogenomics. 2004;4:9–17. Gratacòs M, González JR, Mercader JM, de Cid R, Urretavizcaya M, Estivill X. Brain-derived neurotrophic factor Val66Met and psychiatric disorders: meta-analysis of case-control studies confirm association to substance-related disorders, eating disorders, and schizophrenia. Biol Psychiatry. 2007 Apr 1;61(7):911–22. Gray J, Yeo GSH, Cox JJ, Morton J, Adlam A-LR, Keogh JM, et al. Hyperphagia, severe obesity, impaired cognitive function, and hyperactivity associated with functional loss of one copy of the brain-derived neurotrophic factor (BDNF) gene. Diabetes. 2006 Dec;55(12):3366–71. Gray J, Yeo GSH, Cox JJ, Morton J, Adlam AR, Keogh M, et al. Hyperphagia, severe obesity, impaired cognitive function, and hyperactivity associated with functional loss of one copy of the brain-derived neurotrophic factor (BDNF) gene. Diabetes. 2008;55(12):3366–71. Gray LJ, Cooper N, Dunkley a, Warren FC, Ara R, Abrams K, et al. A systematic review and mixed treatment comparison of pharmacological interventions for the treatment of obesity. Obes Rev. 2012 Jun;13(6):483–98. 117 M.Sc. Thesis – A. Mayhew; McMaster University – Health Research Methodology Grice DE, Halmi K a, Fichter MM, Strober M, Woodside DB, Treasure JT, et al. Evidence for a susceptibility gene for anorexia nervosa on chromosome 1. Am J Hum Genet. 2002 Mar;70(3):787–92. Grilo CM, Masheb RM. Onset of dieting vs binge eating in outpatients with binge eating disorder. Int J Obes. 2000 Apr;24(4):404–9. Grucza RA, Przybeck TR, Cloninger CR. Prevalence and correlates of binge eating disorder in a community sample. Compr Psychiatry. 2007;48(2):124–31. Guisinger S. Adapted to flee famine: adding an evolutionary perspective on anorexia nervosa. Psychol Rev. 2003 Oct;110(4):745–61. Gulati P, Yeo GSH. The biology of FTO: from nucleic acid demethylase to amino acid sensor. Diabetologia. 2013 Oct;56(10):2113–21. Haleem DJ. Serotonin neurotransmission in anorexia nervosa. Behav Pharmacol. 2012 Sep;23:478–95. Hales CN, Barker DJP. Type 2 (non-insulin-dependent) diabetes mellitus: the thrifty phenotype hypothesis. Int J Epidemiol. 2013 Oct;42(5):1215–22. Halkjaer J, Tjonneland A, Thomsen BL, Overvad K, Sorensen TI. Intake of macronutrients as predictors of 5-y changes in waist. Am J Clin Nutr. 2006;84(9):789–97. Han JC, Liu Q-R, Jones M, Levinn RL, Menzie CM, Jefferson-George KS, et al. Brain-derived neurotrophic factor and obesity in the WAGR syndrome. N Engl J Med. 2008 Aug 28;359(9):918–27. Harten PN Van, Hermans KME, Katzman MA, Matroos GE, Susser ES. The Incidence of Anorexia Nervosa on Curaçao. Am J Psychiatry. 2005;162:748–52. Hartmann AS, Greenberg JL, Wilhelm S. The relationship between anorexia nervosa and body dysmorphic disorder. Clin Psychol Rev. 2013;33(5):675–85. Hasselbalch AL, Heitmann BL, Kyvik KO, Sørensen TIA. Studies of twins indicate that genetics influence dietary intake. J Nutr. 2008;138:2406–12. Haupt A, Thamer C, Staiger H, Tschritter O, Kirchhoff K, Machicao F, et al. Variation in the FTO gene influences food intake but not energy expenditure. Exp Clin Endocrinol Diabetes. 2009 Apr;117(4):194–7. Hausenblas H a, Campbell A, Menzel JE, Doughty J, Levine M, Thompson JK. Media effects of experimental presentation of the ideal physique on eating disorder symptoms: a metaanalysis of laboratory studies. Clin Psychol Rev. Elsevier Ltd; 2013 Feb;33(1):168–81. 118 M.Sc. Thesis – A. Mayhew; McMaster University – Health Research Methodology Hay P. The epidemiology of eating disorder behaviors: an Australian community-based survey. Int J Eat Disord. 1998 May;23(4):371–82. Hay PJ, Mond J, Buttner P, Darby A. Eating disorder behaviors are increasing: findings from two sequential community surveys in South Australia. PLoS One. 2008 Jan;3(2):e1541. Heaner MK, Walsh BT. A history of the identification of the characteristics eating disturbances of bulimia nervosa, binge eating disorders and anorexia nervosa. Appetite. Elsevier Ltd; 2013 Jun;65:185–8. Hebebrand J, Geller F, Dempfle A, Heinzel-Gutenbrunner M, Raab M, Gerber G, et al. Bingeeating episodes are not characteristic of carriers of melanocortin-4 receptor gene mutations. Mol Psychiatry. 2004 Aug;9(8):796–800. Hinney A, Bornscheuer A, Depenbusch M, Mierke B, Tölle A, Middeke K, et al. No evidence for involvement of the leptin gene in anorexia nervosa, bulimia nervosa, underweight or early onset extreme obesity: identification of two novel mutations in the coding sequence and a novel polymorphism in the leptin gene linked upstream regio. Mol Psychiatry. 1998 Nov;3(6):539–43. Hinney A, Nguyen TT, Scherag A, Friedel S, Brönner G, Müller TD, et al. Genome wide association (GWA) study for early onset extreme obesity supports the role of fat mass and obesity associated gene (FTO) variants. PLoS One. 2007 Jan;2(12):e1361. Hinney A, Schneider J, Ziegler A, Lehmkuhl G, Poustka F, Schmidt MH, et al. No evidence for involvement of polymorphisms of the dopamine D4 receptor gene in anorexia nervosa, underweight, and obesity. Am J Med Genet. 1999 Dec 15;88(6):594–7. Ho N, Sommers M. Anhedonia: a concept analysis. Arch Psychiatr Nurs. Elsevier Inc.; 2013 Jun;27(3):121–239. Hoed M Den, Westerterp-Plantenga MS, Bouwman FG, Mariman ECM, Westerterp KR. Postprandial responses in hunger and satiety are associated with the rs9939609 single nucleotide polymorphism in FTO. Am J Clin Nutr. 2009;90:1426–32. Hoek HW. Incidence, prevalence and mortality of anorexia nervosa and other eating disorders. Curr Opin Psychiatry. 2006 Jul;19(4):389–94. Hoek HW, van Hoeken D. Review of the prevalence and incidence of eating disorders. Int J Eat Disord. 2003 Dec;34(4):383–96. Holtom-Viesel A, Allan S. A systematic review of the literature on family functioning across all eating disorder diagnoses in comparison to control families. Clin Psychol Rev. Elsevier Ltd; 2014 Feb;34(1):29–43. 119 M.Sc. Thesis – A. Mayhew; McMaster University – Health Research Methodology Hong KW, Oh B. Recapitulation of genome-wide association studies on body mass index in the Korean population. Int J Obes. 2012 Aug;36(8):1127–30. Horstmann A, Kovacs P, Kabisch S, Boettcher Y, Schloegl H, Tönjes A, et al. Common genetic variation near MC4R has a sex-specific impact on human brain structure and eating behavior. PLoS One. 2013 Jan;8(9):e74362. Hotta M, Ohwada R, Akamizu T, Shibasaki T, Takano K, Kangawa K. Ghrelin increases hunger and food intake in patients with restricting-type anorexia nervosa: a pilot study. Endocr J. 2009 Jan;56(9):1119–28. Hu X, Karwautz A, Wagner G, Holliday J, Li T, Treasure J, et al. No association between a promoter polymorphism in the noradrenaline transporter gene and anorexia nervosa. Psychiatr Genet. 2007 Aug;17(4):247–8. Hudson JI, Hiripi E, Jr HGP, Kessler RC. The prevalence and correlates of eating disorders in the National Comorbidity Survey replication. Biol Psychiatry. 2008;61(3):348–58. Hur YM, Bouchard TJ, Eckert E. Genetic and environmental influences on self-reported diet: a reared-apart twin study. Physiol Behav. 1998 Jul;64(5):629–36. IBM Corp. IBM SPSS Statistics for Windows. Armonk, NY: IBM Corp; 2011. Ioannidis JP a, Boffetta P, Little J, O’Brien TR, Uitterlinden AG, Vineis P, et al. Assessment of cumulative evidence on genetic associations: interim guidelines. Int J Epidemiol. 2008 Feb;37(1):120–32. Jaite C, Hoffmann F, Glaeske G, Bachmann CJ. Prevalence, comorbidities and outpatient treatment of anorexia and bulimia nervosa in German children and adolescents. Eat Weight Disord. 2013 Apr 16;18(2):157–65. Janssens CJW, Moonesinghe R, Yang Q, Steyerberg EW, van Duijn CM, Khoury MJ. The impact of genotype frequencies on the clinical validity of genomic profiling for predicting common chronic diseases. Genet Med. 2007 Aug;9(8):528–35. Johnson RD. Opioid involvement in feeding behaviour and the pathogenesis of certain eating disorders. Med Hypotheses. 1995 Nov;45(5):491–7. Jørgensen L, Sørensen T, Schroll M, Larsen S. Influence of dietary factors on weight change assessed by multivariate graphical models. Int J Obes Relat Metab Disord. 1995;19(12):909–15. Joyner MJ, Prendergast FG. Chasing Mendel: five questions for personalized medicine. J Physiol. 2014 Jun 1;592(11):2381–8. 120 M.Sc. Thesis – A. Mayhew; McMaster University – Health Research Methodology Jung CH, Kim M-S. Molecular mechanisms of central leptin resistance in obesity. Arch Pharm Res. 2013 Feb;36(2):201–7. Kardum I, Gra A, Hudek-Kneževi J. Evolutionary explanations of eating disorders. Psychol Top. 2008;17(2):247–63. Karwautz A, Rabe-Hesketh S, Hu X, Zhao J, Sham P, Collier D a, et al. Individual-specific risk factors for anorexia nervosa: a pilot study using a discordant sister-pair design. Psychol Med. 2001 Feb;31(2):317–29. Kaye W. Neurobiology of anorexia and bulimia nervosa. Physiol Behav. 2008 Apr 22;94(1):121–35. Kaye WH, Klump KL, Frank GK, Strober M. Anorexia and bulimia nervosa. Annu Rev Med. 2000 Jan;51:299–313. Kaye WH, Wierenga CE, Bailer UF, Simmons AN, Bischoff-Grethe A. Nothing tastes as good as skinny feels: the neurobiology of anorexia nervosa. Trends Neurosci. Elsevier Ltd; 2013 Feb;36(2):110–20. Keating BJ, Tischfield S, Murray SS, Bhangale T, Price TS, Glessner JT, et al. Concept, design and implementation of a cardiovascular gene-centric 50 k SNP array for large-scale genomic association studies. PLoS One. 2008 Jan;3(10):e3583. Keating C. Theoretical perspective on anorexia nervosa: the conflict of reward. Neurosci Biobehav Rev. 2010 Jan;34(1):73–9. Keating C, Tilbrook AJ, Rossell SL, Enticott PG, Fitzgerald PB. Reward processing in anorexia nervosa. Neuropsychologia. Elsevier Ltd; 2012 Apr;50(5):567–75. Keel PK, Brown T a. Update on course and outcome in eating disorders. Int J Eat Disord. 2010 Apr;43(3):195–204. Keel PK, Heatherton TF, Dorer DJ, Joiner TE, Zalta AK. Point prevalence of bulimia nervosa in 1982, 1992, and 2002. Psychol Med. 2006 Jan;36(1):119–27. Keel PK, Klump KL. Are eating disorders culture-bound syndromes? Implications for conceptualizing their etiology. Psychol Bull. 2003 Sep;129(5):747–69. Kelemen LE, Anand SS, Vuksan V, Yi Q, Teo KK, Devanesen S, et al. Development and evaluation of cultural food frequency questionnaires for South Asians, Chinese, and Europeans in North America. J Am Diet Assoc. 2003 Sep;103(9):1178–84. Keski-Rahkonen A, Hoek HW, Linna MS, Raevuori A, Sihvola E, Bulik CM, et al. Incidence and outcomes of bulimia nervosa: a nationwide population-based study. Psychol Med. 2009 May;39(5):823–31. 121 M.Sc. Thesis – A. Mayhew; McMaster University – Health Research Methodology Keski-Rahkonen A, Raevuori A, Bulik CM, Hoek HW, Sihvola E, Kaprio J, et al. Depression and drive for thinness are associated with persistent bulimia nervosa in the community. Eur Eat Disord Rev. 2013 Mar;21(2):121–9. Keskitalo K, Silventoinen K, Tuorila H, Perola M, Pietiläinen KH, Rissanen A, et al. Genetic and environmental contributions to food use patterns of young adult twins. Physiol Behav. 2008 a Jan 28;93:235–42. Keskitalo K, Tuorila H, Spector TD, Cherkas LF, Knaapila A, Kaprio J, et al. The Three-Factor Eating Questionnaire, body mass index, and responses to sweet and salty fatty foods: a twin study of genetic and environmental associations. Am J Clin Nutr. 2008 b Aug;88:263–71. Kessler RC, Berglund P a, Chiu WT, Deitz AC, Hudson JI, Shahly V, et al. The prevalence and correlates of binge eating disorder in the World Health Organization World Mental Health Surveys. Biol Psychiatry. 2013 May 1;73(9):904–14. Kindler J, Bailer U, de Zwaan M, Fuchs K, Leisch F, Grün B, et al. No association of the neuropeptide Y (Leu7Pro) and ghrelin gene (Arg51Gln, Leu72Met, Gln90Leu) single nucleotide polymorphisms with eating disorders. Nord J Psychiatry. 2011 Jun;65(3):203–7. Kinzl JF, Traweger C, Trefalt E, Mangweth B, Biebl W. Binge eating disorder in females: a population-based investigation. Int J Eat Disord. 1999 Apr;25(3):287–92. Klein DA, Walsh BT. Eating disorders. Int Rev Psychiatry. 2003 Aug;15(3):205–16. Klump KL, Kaye WH, Strober M. The evolving genetic foundations of eating disorders. Psychiatr Clin North Am. 2001 Jun;24(2):215–25. Klump KL, Wonderlich S, Lehoux P, Lilenfeld LRR, Bulik CM. Does environment matter? A review of nonshared environment and eating disorders. Int J Eat Disord. 2002 Mar;31(2):118–35. Knaapila A, Silventoinen K, Broms U, Rose RJ, Perola M, Kaprio J, et al. Food neophobia in young adults: genetic architecture and relation to personality, pleasantness and use frequency of foods, and body mass index--a twin study. Behav Genet. 2011 Jul;41:512–21. Knaapila A, Tuorila H, Silventoinen K, Keskitalo K, Kallela M, Wessman M, et al. Food neophobia shows heritable variation in humans. Physiol Behav. 2007 Aug 15;91:573–8. Kontis D, Theochari E. Dopamine in anorexia nervosa: a systematic review. Behav Pharmacol. 2012 Sep;23:496–515. Kral JG, Näslund E. Surgical treatment of obesity. Nat Clin Pract Endocrinol Metab. 2007 Aug;3(8):574–83. 122 M.Sc. Thesis – A. Mayhew; McMaster University – Health Research Methodology Lear S a, Deng WQ, Paré G, Sulistyoningrum DC, Loos RJF, Devlin A. Associations of the FTO rs9939609 variant with discrete body fat depots and dietary intake in a multi-ethnic cohort. Genet Rest Camb. 2011 Dec;93(6):419–26. Lee H-J, Kim IK, Kang JH, Ahn Y, Han B-G, Lee J-Y, et al. Effects of common FTO gene variants associated with BMI on dietary intake and physical activity in Koreans. Clin Chim Acta. Elsevier B.V.; 2010 Nov 11;411:1716–22. Lehnert T, Sonntag D, Konnopka A, Riedel-Heller S, König H-H. Economic costs of overweight and obesity. Best Pract Res Clin Endocrinol Metab. 2013 Apr;27(2):105–15. Levitan RD, Wendland B. Novel “thrifty” models of increased eating behaviour. Curr Psychiatry Rep. 2013 Nov;15(11):408. Li A, Meyre D. Jumping on the Train of Personalized Medicine : A Primer for Non- Geneticist Clinicians : Part 3 . Clinical Applications in the Personalized Medicine Area. 2014; Llewellyn CH, Jaarsveld CHM Van, Boniface D, Carnell S, Wardle J. Eating rate is a heritable phenotype related to weight in children. Am J Clin Nutr. 2008;88:1560–6. Llewellyn CH, Jaarsveld CHM Van, Johnson L, Carnell S, Wardle J. Nature and nurture in infant appetite : analysis of the Gemini twin birth cohort. Am J Clin Nutr. 2010;91:1172–9. Llewellyn CH, Jaarsveld CHM Van, Plomin R, Fisher A, Wardle J. Inherited behavioral susceptibility to adiposity in infancy : a multivariate genetic analysis of appetite and weight in the Gemini birth cohort 1 – 3. 2012; Llewellyn CH, Trzaskowski M, van Jaarsveld CHM, Plomin R, Wardle J. Satiety mechanisms in genetic risk of obesity. JAMA Pediatr. 2014 May;168(4):338–44. Lloyd DJ, Bohan S, Gekakis N. Obesity, hyperphagia and increased metabolic efficiency in Pc1 mutant mice. Hum Mol Genet. 2006 Jun 1;15(11):1884–93. Lofrano-Prado MC, Prado WL Do, de Piano A, Tock L, Caranti DA, Nascimento CMO Do, et al. Eating disorders in adolescents: correlations between symptoms and central control of eating behavior. Eat Behav. 2011 Jan;12(1):78–82. Lubrano-Berthelier C, Dubern B, Lacorte J-M, Picard F, Shapiro A, Zhang S, et al. Melanocortin 4 receptor mutations in a large cohort of severely obese adults: prevalence, functional classification, genotype-phenotype relationship, and lack of association with binge eating. J Clin Endocrinol Metab. 2006 May;91(5):1811–8. Lyons WE, Mamounas L a, Ricaurte G a, Coppola V, Reid SW, Bora SH, et al. Brain-derived neurotrophic factor-deficient mice develop aggressiveness and hyperphagia in conjunction with brain serotonergic abnormalities. Proc Natl Acad Sci U S A. 1999 Dec 21;96(26):15239–44. 123 M.Sc. Thesis – A. Mayhew; McMaster University – Health Research Methodology Maes HH, Neale MC, Eaves LJ. Genetic and environmental factors in relative body weight and human adiposity. Behav Genet. 1997 Jul;27(4):325–51. Maj M, Monteleone P. Genetic susceptibility to eating disorders: associated polymorphisms and pharmacogenetic suggestions. Pharmacogenomics. 2008;9(10):1487. Malik VS, Willett WC, Hu FB. Global obesity: trends, risk factors and policy implications. Nat Rev Endocrinol. 2013;9:13–27. Manolio T a, Collins FS, Cox NJ, Goldstein DB, Hindorff L a, Hunter DJ, et al. Finding the missing heritability of complex diseases. Nature. Nature Publishing Group; 2009 Oct 8;461(7265):747–53. Marian AJ. Elements of “missing heritability.”Curr Opin Cardiol. 2012 May;27:197–201. Marques L, Alegria M, Becker A, Chen C, Fang A, Chosak A, et al. Comparative prevalence, correlates of impairment, and service utilization for eating disorders across U.S. ethnic groups: Implications for reducing ethnic disparities in health care access for eating disorders. Int J Eat Disord. 2011;44(5):412–20. Martaskova D, Slachtova L, Kemlink D, Zahorakova D, Papezova H. Polymorphisms in serotonin-related genes in anorexia nervosa. The first study in Czech population and metaanalyses with previously performed studies. Folia Biolgica. 2009;55:192–7. Mathes WF, Brownley, Kimberly A, Mo X, Bulik CM. The biology of binge eating. Appetite. 2010;52(3):545–53. McAllister EJ, Dhurandhar N V, Keith SW, Aronne LJ, Barger J, Baskin M, et al. Ten putative contributors to the obesity epidemic. Crit Rev Food Sci Nutr. 2009 Nov;49(10):868–913. Mccaffery JM, Papandonatos GD, Peter I, Huggins GS, Raynor HA, Delahanty LM, et al. Obesity susceptibility loci and dietary intake in the Look AHEAD Trial. Am J Clin Nutr. 2012;95:1477–86. Meczekalski B, Podfigurna-Stopa A, Katulski K. Long-term consequences of anorexia nervosa. Maturitas. Elsevier Ireland Ltd; 2013 Jul;75(3):215–20. Mencarelli M, Dubern B, Alili R, Maestrini S, Benajiba L, Tagliaferri M, et al. Rare melanocortin-3 receptor mutations with in vitro functional consequences are associated with human obesity. Hum Mol Genet. 2011 Jan 15;20(2):392–9. Mercader JM, Ribasés M, Gratacòs M, González JR, Bayés M, de Cid R, et al. Altered brainderived neurotrophic factor blood levels and gene variability are associated with anorexia and bulimia. Genes, Brain Behav. 2007 Nov;6(8):706–16. 124 M.Sc. Thesis – A. Mayhew; McMaster University – Health Research Methodology Merle J V, Haas V, Burghardt R, Döhler N, Schneider N, Lehmkuhl U, et al. Agouti-related protein in patients with acute and weight-restored anorexia nervosa. Psychol Med. 2011 Oct;41(10):2183–92. Mitchell BD, Rainwater DL, Hsueh W-C, Kennedy AJ, Stern MP, Maccluer JW. Familial aggregation of nutrient intake and physical activity: results from the San Antonio Family Heart Study. Ann Epidemiol. 2003 Feb;13(2):128–35. Mitchell NS, Catenacci V a, Wyatt HR, Hill JO. Obesity: overview of an epidemic. Psychiatr Clin North Am. Elsevier Inc.; 2011 Dec;34(4):717–32. Mitchison D, Hay PJ. The epidemiology of eating disorders: genetic, environmental, and societal factors. Clin Epidemiol. 2014 Jan;6:89–97. Moleres A, Ochoa MC, Rendo-Urteaga T, Martínez-González MA, Azcona San Julián MC, Martínez JA, et al. Dietary fatty acid distribution modifies obesity risk linked to the rs9939609 polymorphism of the fat mass and obesity-associated gene in a Spanish casecontrol study of children. Brit J Nutr. 2012 Feb;107(4):533–8. Monteleone P, DiLieto A, Castaldo E, Maj M. Leptin functioning in eating disorders. CNS Spectr. 2004;9(7):523–9. Monteleone P, Tortorella A, Castaldo E, Di Filippo C, Maj M. No association of the Arg51Gln and Leu72Met polymorphisms of the ghrelin gene with anorexia nervosa or bulimia nervosa. Neurosci Lett. 2006 May 8;398(3):325–7. Moriya J, Takimoto Y, Yoshiuchi K, Shimosawa T, Akabayashi A. Plasma agouti-related protein levels in women with anorexia nervosa. Psychoneuroendocrinology. 2006 Oct;31(9):1057– 61. Must A, Spadano J, Coakley EH, Field AE, Colditz G, Dietz WH. The disease burden associated with overweight and obesity. J Am Med Assoc. 1999;282(16):1523–9. Nakazato M, Hashimoto K, Shimizu E, Niitsu T, Iyo M. Possible involvement of brain-derived neurotrophic factor in eating disorders. Life. 2012 May;64(5):355–61. Neel J V. Diabetes mellitus: a “thrifty” genotype rendered detrimental by “progress.”Am J Hum Genet. 1962;14:353–62. Neel J V. The thrifty genotype in 1998. Nutr Rev. 1999;57:S2–S7. Nelson SM, Telfer EE, Anderson R a. The ageing ovary and uterus: new biological insights. Hum Reprod Update. 2013;19(1):67–83. 125 M.Sc. Thesis – A. Mayhew; McMaster University – Health Research Methodology Nicdao EG, Hong S, Takeuchi DT. Prevalence and correlates of eating disorders among Asian Americans: Results from the National Latino and Asian American Study. Int J Eat Disord. 2007;40:S22–S26. O’Rahilly S, Farooqi IS. Human obesity as a heritable disorder of the central control of energy balance. Int J Obes (Lond). 2008 Dec;32 Suppl 7:S55–61. O’Shaughnessy R, Dallos R. Attachment research and eating disorders: a review of the literature. Clin Child Psychol Psychiatry. 2009 Oct;14(4):559–74. Park SL, Cheng I, Pendergrass S a, Kucharska-Newton AM, Lim U, Ambite JL, et al. Association of the FTO obesity risk variant rs8050136 with percentage of energy intake from fat in multiple racial/ethnic populations: the PAGE study. Am J Epidemiol. 2013 Sep 1;178(5):780–90. Phillips CM, Kesse-Guyot E, Mcmanus R, Hercberg S, Lairon D, Planells R, et al. High dietary saturated fat intake accentuates obesity risk associated with the fatt mas and obesityassociated gene in adults. J Nutr. 2012;142:824–31. Pike KM, Dohm F a, Striegel-Moore RH, Wilfley DE, Fairburn CG. A comparison of black and white women with binge eating disorder. Am J Psychiatry. 2001 Sep;158(9):1455–60. Polsinelli GN, Levitan RN, De Luca V. 5-HTTLPR polymorphism in bulimia nervosa: a multiple-model meta-analysis. Psychiatr Genet. 2012 Oct;22(5):219–25. Prentice A, Jebb S. Energy Intake / Physical Activity Interactions in the Homeostasis of Body Weight Regulation. 2004;62(7). Prentice AM, Hennig BJ, Fulford AJ. Evolutionary origins of the obesity epidemic: natural selection of thrifty genes or genetic drift following predation release? Int J Obes. 2008 Nov;32(11):1607–10. Preti A, Girolamo G De, Vilagut G, Alonso J, Graaf R De, Bruffaerts R, et al. The epidemiology of eating disorders in six European countries: results of the ESEMeD-WMH project. J Psychiatr Res. Elsevier Ltd; 2009 Sep;43(14):1125–32. Quinton ND, Meechan DW, Brown K, Eastwood H, Blakemore a IF. Single nucleotide polymorphisms in the leptin receptor gene: studies in anorexia nervosa. Psychiatr Genet. 2004 Dec;14(4):191–4. Rask-Andersen M, Olszewski PK, Levine AS, Schiöth HB. Molecular mechanisms underlying anorexia nervosa: focus on human gene association studies and systems controlling food intake. Brain Res Rev. Elsevier B.V.; 2010 Mar;62(2):147–64. Razak F, Anand SS, Shannon H, Vuksan V, Davis B, Jacobs R, et al. Defining obesity cut points in a multiethnic population. Circulation. 2007 Apr 24;115:2111–8. 126 M.Sc. Thesis – A. Mayhew; McMaster University – Health Research Methodology Reichborn-Kjennerud T, Bulik CM, Sullivan PF, Tambs K, Harris JR. Psychiatric and medical symptoms in binge eating in the absence of compensatory behaviors. Obes Res. 2004 Sep;12(9):1445–54. Ribasés M, Gratacòs M, Armengol L, de Cid R, Badía A, Jiménez L, et al. Met66 in the brainderived neurotrophic factor (BDNF) precursor is associated with anorexia nervosa restrictive type. Mol Psychiatry. 2003 Aug;8(8):745–51. Ribasés M, Gratacòs M, Fernández-Aranda F, Bellodi L, Boni C, Anderluh M, et al. Association of BDNF with restricting anorexia nervosa and minimum body mass index: a family-based association study of eight European populations. Eur J Hum Genet. 2005 Apr;13(4):428–34. Rijsdijk F V, Sham PC. Analytic approaches to twin data using structural equation models. Brief Bioinform. 2002 Jun;3(2):119–33. Rios M, Fan G, Fekete C, Kelly J, Bates B, Kuehn R, et al. Conditional deletion of brain-derived neurotrophic factor in the postnatal brain leads to obesity and hyperactivity. Mol Endocrinol. 2001 Oct;15(10):1748–57. Robiou-du-Pont S, Yengo L, Vaillant E, Lobbens S, Durand E, Horber F, et al. Common variants near BDNF and SH2B1 show nominal evidence of association with snacking behavior in European populations. J Mol Med. 2013 May 3; Rothstein M a. Should researchers disclose results to descendants? Am J Bioeth. 2013 Jan;13(10):64–5. Rukh G, Sonestedt E, Melander O, Hedblad B, Wirfält E, Ericson U, et al. Genetic susceptibility to obesity and diet intakes: association and interaction analyses in the Malmö Diet and Cancer Study. Genes Nutr. 2013 Jul 17;8(6):535–47. Runkel N, Colombo-Benkmann M, Hüttl TP, Tigges H, Mann O, Sauerland S. Bariatric surgery. Dtsch Arztebl Int. 2011 May;108(20):341–6. Rutters F, Lemmens SGT, Born JM, Bouwman F, Nieuwenhuizen AG, Mariman E, et al. Genetic associations with acute stress-related changes in eating in the absence of hunger. Patient Educ Couns. Elsevier Ireland Ltd; 2010 Jun;79(3):367–71. Schelbert KB. Comorbidities of obesity. Prim Care Clin Off Pr. Elsevier Ltd; 2009 Jun;36(2):271–85. Scherag S, Hebebrand J, Hinney A. Eating disorders: the current status of molecular genetic research. Eur Child Adolesc Psychiatry. 2010 Mar;19(3):211–6. Scheurink AJW, Boersma GJ, Nergårdh R, Södersten P. Neurobiology of hyperactivity and reward: agreeable restlessness in anorexia nervosa. Physiol Behav. Elsevier Inc.; 2010 Jul 14;100(5):490–5. 127 M.Sc. Thesis – A. Mayhew; McMaster University – Health Research Methodology Scolnick B, Mostofsky DI. Anorexia nervosa: A rogue hibernation? Med Hypotheses. Elsevier Ltd; 2014 Feb;82(2):231–5. Scuteri A, Sanna S, Chen W-M, Uda M, Albai G, Strait J, et al. Genome-wide association scan shows genetic variants in the FTO gene are associated with obesity-related traits. PLoS Genet. 2007 Jul;3(7):e115. Silventoinen K, Kaprio J. Genetics of tracking of body mass index from birth to late middle age: evidence from twin and family studies. Eur J Obes. 2009 Jan;2(3):196–202. Silventoinen K, Rokholm B, Kaprio J, Sørensen TIA. The genetic and environmental influences on childhood obesity: a systematic review of twin and adoption studies. Int J Obes. 2010 Jan;34:29–40. Simpson KJ. Anorexia nervosa and culture. J Psychiatr Ment Health Nurs. 2002 Feb;9(1):65–71. Slof-Op ’t Landt MCT, van Furth EF, Meulenbelt I, Slagboom PE, Bartels M, Boomsma DI, et al. Eating disorders: from twin studies to candidate genes and beyond. Twin Res Hum Genet. 2005 Oct;8(5):467–82. Slof-Op ’t Landt MCT, Meulenbelt I, Bartels M, Suchiman E, Middeldorp CM, HouwingDuistermaat JJ, et al. Association study in eating disorders: TPH2 associates with anorexia nervosa and self-induced vomiting. Genes Brain Behav. 2011 Mar;10(2):236–43. Smink FRE, van Hoeken D, Hoek HW. Epidemiology of eating disorders: incidence, prevalence and mortality rates. Curr Psychiatry Rep. 2012 Aug;14(4):406–14. Smith DE, Marcus MD, Lewis CE, Fitzgibbon M, Schreiner P. Prevalence of binge eating disorder, obesity, and depression in a biracial cohort of young adults. Ann Behav Med. 1998 Jan;20(3):227–32. Smitka K, Papezova H, Vondra K, Hill M, Hainer V, Nedvidkova J. The role of “mixed” orexigenic and anorexigenic signals and autoantibodies reacting with appetite-regulating neuropeptides and peptides of the adipose tissue-gut-brain axis: Relevance to food intake and nutritional status in patients with anorexia nervosa. Int J Endocrinol. 2013 Jan;2013:483145. Smolak L, Murnen SK. A meta-analytic examination of the relationship between child sexual abuse and eating disorders. Int J Eat Disord. 2002;31(2):559–74. Södersten P, Nergårdh R, Bergh C, Zandian M, Scheurink A. Behavioral neuroendocrinology and treatment of anorexia nervosa. Front Neuroendocrinol. 2008 Oct;29(4):445–62. Son E Van, Hoeken D Van, Bartelds AIM, Furth EF Van, Hoek HW. Time trends in the incidence of eating disorders: A primary care study in the Netherlands. Int J Eat Disord. 2006;39:565–9. 128 M.Sc. Thesis – A. Mayhew; McMaster University – Health Research Methodology Speakman JR. A nonadaptive scenario explaining the genetic predisposition to obesity: the “predation release” hypothesis. Cell Metab. 2007 Jul;6(1):5–12. Speakman JR. Thrifty genes for obesity, an attractive but flawed idea, and an alternative perspective: the “drifty gene” hypothesis. Int J Obes. 2008 Nov;32(11):1611–7. Speakman JR, O’Rahilly S. Fat: an evolving issue. Dis Model Mech. 2012 Sep;5(5):569–73. Speakman JR, Rance K a, Johnstone AM. Polymorphisms of the FTO gene are associated with variation in energy intake, but not energy expenditure. Obesity. 2008 Aug;16:1961–5. Speliotes EK, Willer CJ, Berndt SI, Monda KL, Thorleifsson G, Jackson AU, et al. Association analyses of 249,796 individuals reveal 18 new loci associated with body mass index. Nat Genet. 2010 Nov;42(11):937–48. Spitzer R., Devlin M, Walsh TB, Hasin DS, Wing R, Marcus M, et al. Binge eating disorder: A multisite field trial of the diagnostic criteria. Int J Eat Disord. 1992;11:191–204. Spitzer R., Yanovski SZ, Wadden T, Wing R, Marcus MD, Stunkard A., et al. Binge eating disorder: Its further validation in a multi-site study. Int J Eat Disord. 1993;13:137–54. Van Spronsen FJ. Phenylketonuria: a 21st century perspective. Nat Rev Endrocrinol. 2010;6:509–14. Spurrell EB, Wilfley DE, Tanofsky MB, Brownell KD. Age of onset for binge eating: are there different pathways to binge eating? Int J Eat Disord. 1997 Jan;21(1):55–65. Sternheim L, Danner U, Adan R, van Elburg A. Drive for activity in patients with anorexia nervosa. Int J Eat iDsorders. 2014 Mar 29;0(00):1–4. Stöger R. The thrifty epigenotype: an acquired and heritable predisposition for obesity and diabetes? BioEssays. 2008 Feb;30(2):156–66. Striegel-Moore RH, Dohm F a, Kraemer HC, Taylor CB, Daniels S, Crawford PB, et al. Eating disorders in white and black women. Am J Psychiatry. 2003 Jul;160(7):1326–31. Strober M, Freeman R, Lampert C, Diamond J, Kaye W. Controlled family study of anorexia nervosa and bulimia nervosa: evidence of shared liability and transmission of partial syndromes. Am J Psychiatry. 2000 Mar;157(3):393–401. Stunkard AJ, Harris JR, Pedersen NL, McClearn GE. The body mass index of twins who have been reared apart. N Engl J Med. 1990;322:1483–7. Stutzmann F, Cauchi S, Durand E, Calvacanti-Proença C, Pigeyre M, Hartikainen A-L, et al. Common genetic variation near MC4R is associated with eating behaviour patterns in European populations. Int J Obes. 2009 Mar;33(3):373–8. 129 M.Sc. Thesis – A. Mayhew; McMaster University – Health Research Methodology Stutzmann F, Cauchi S, Durand E, Pigeyre M, Hartikainen A, Sheehy AM, et al. The disease burden associated with overweight and obesity. Int J Obes. Elsevier Ltd; 2011 Jan 12;282(1):1523–9. Stutzmann F, Vatin V, Cauchi S, Morandi A, Jouret B, Landt O, et al. Non-synonymous polymorphisms in melanocortin-4 receptor protect against obesity: the two facets of a Janus obesity gene. Hum Mol Genet. 2007 Aug 1;26(15):1837–44. Surbey MK. Anorexia nervosa, amenorrhea, and adaptation. Ethol Sociobiol. 1987;8:47–61. Swinburn B a, Sacks G, Hall KD, McPherson K, Finegood DT, Moodie ML, et al. The global obesity pandemic: shaped by global drivers and local environments. Lancet. Elsevier Ltd; 2011 Aug 27;378(9793):804–14. Tan L-J, Zhu H, He H, Wu K-H, Li J, Chen X-D, et al. Replication of 6 obesity genes in a metaanalysis of genome-wide association studies from diverse ancestries. PLoS One. 2014 Jan;9(5):e96149. Tanaka T, Ngwa JS, van Rooij FJ a, Zillikens MC, Wojczynski MK, Frazier-Wood AC, et al. Genome-wide meta-analysis of observational studies shows common genetic variants associated with macronutrient intake. Am J Clin Nutr. 2013 Jun;97:1395–402. Tanofsky-Kraff M, Han JC, Anandalingam K, Shomaker LB, Columbo KM, Wolkoff LE, et al. The FTO gene rs9939609 obesity-risk allele and loss of control over eating. Am J Clin Nutr. 2009;90:1483–8. Taylor JY, Caldwell CH, Baser RE, Matuski N, Faison N, Jackson JS. Classification and correlates of eating disorders among blacks: Findings from the National Survey of American Life. J Heal Care Poor Underserved. 2013;24(1):289–310. Teare MD, Barrett J. Genetic Epidemiology 2: Genetic linkage studies. Lancet. 2005;366:1036– 44. Teucher B, Skinner J, Skidmore PML, Cassidy A, Fairweather-Tait SJ, Hooper L, et al. Dietary patterns and heritability of food choice in a UK female twin cohort. Twin Res Hum Genet. 2007 Oct;10(5):734–48. Tholin S, Rasmussen F, Tynelius P, Karlsson J. Genetic and environmental influences on eating behavior: the Swedish Young Male Twins Study. Am J Clin Nutr. 2005 Mar;81:564–9. Thorleifsson G, Walters GB, Gudbjartsson DF, Steinthorsdottir V, Sulem P, Helgadottir A, et al. Genome-wide association yields new sequence variants at seven loci that associate with measures of obesity. Nat Genet. 2009 Jan;41(1):18–24. Thornton LM, Mazzeo SE, Bulik CM. The heritability of eating disorders: Methods and current findings. Curr Top Behav Neurosci. 2011;6:141–56. 130 M.Sc. Thesis – A. Mayhew; McMaster University – Health Research Methodology Timpson NJ, Emmett PM, Frayling TM, Rogers I, Hattersley AT, McCarthy MI, et al. The fat mass- and obesity-associated locus and dietary intake in children. Am J Clin Nutr. 2008 Oct;88(4):971–8. Trace SE, Baker JH, Peñas-Lledó E, Bulik CM. The genetics of eating disorders. Annu Rev Clin Psychol. 2013 Jan;9:589–620. Tung Y-CL, Yeo GSH. From GWAS to biology: lessons from FTO. Ann N Y Acad Sci. 2011 Mar;1220:162–71. Urwin RE, Bennetts B, Wilcken B, Lampropoulos B, Beumont P, Clarke S, et al. Anorexia nervosa (restrictive subtype) is associated with a polymorphism in the novel norepinephrine transporter gene promoter polymorphic region. Mol Psychiatry. 2002 Jan;7(6):652–7. Valette M, Bellisle F, Carette C, Poitou C, Dubern B, Paradis G, et al. Eating behaviour in obese patients with melanocortin-4 receptor mutations: a literature review. Int J Obes. 2013 a Aug;37(8):1027–35. Valette M, Poitou C, Kesse-Guyot E, Bellisle F, Carette C, Le Beyec J, et al. Association between melanocortin-4 receptor mutations and eating behaviors in obese patients: a casecontrol study. Int J Obes. 2013 b Oct 9;38(6):883–5. Velders FP, De Wit JE, Jansen PW, Jaddoe VW V, Hofman A, Verhulst FC, et al. FTO at rs9939609, food responsiveness, emotional control and symptoms of ADHD in preschool children. PLoS One. 2012 Jan;7(11):e49131. Vink T, Hinney A, van Elburg AA, van Goozen SH, Sandkuijl LA, Sinke RJ, et al. Association between an agouti-related protein gene polymorphism and anorexia nervosa. Mol Psychiatry. 2001 May;6(3):325–8. Vinkhuyzen AA, Wrap NR, Yang J, Goddard ME, Visscher PM. Estimation and partioning of heritability in human populations using whole genome analysis methods. Annu Rev Genet. 2014;47:75–95. Wade TD, Bergin JL, Tiggemann M, Bulik CM, Fairburn CG. Prevalence and long-term course of lifetime eating disorders in an adult Australian twin cohort. Aust N Z J Psychiatry. 2006 Jan;40(2):121–8. Wang G, Volkow ND, Thanos PK, Fowler JS. Similarity between obesity and drug addiction as assessed by neurofunctional imaging. J Addict Dis. 2004;23(3):39–53. Wang GJ, Volkow ND, Logan J, Pappas NR, Wong CT, Zhu W, et al. Brain dopamine and obesity. Lancet. 2001 Feb 3;357(9253):354–7. 131 M.Sc. Thesis – A. Mayhew; McMaster University – Health Research Methodology Wardle J, Carnell S, Haworth CM a, Farooqi IS, O’Rahilly S, Plomin R. Obesity associated genetic variation in FTO is associated with diminished satiety. J Clin Endocrinol Metab. 2008 Sep;93:3640–3. Wardle J, Cooke L. Genetic and environmental determinants of children’s food preferences. Brit J Nutr. 2008 Mar;99 Suppl 1:S15–21. Wardle J, Llewellyn C, Sanderson S, Plomin R. The FTO gene and measured food intake in children. Int J Obes. 2009 Jan;33:42–5. Wasser SK, Barash DP. Reproductive suppression among female mammals: implications for biomedicine and sexual selection theory. Q Rev Biol. 1983 Dec;58(4):513–38. Wei Z, Wang K, Qu H-Q, Zhang H, Bradfield J, Kim C, et al. From disease association to risk assessment: an optimistic view from genome-wide association studies on type 1 diabetes. PLoS Genet. 2009 Oct;5(10):e1000678. Wellman PJ. Norepinephrine and the control of food intake. Nutrition. 2000 Oct;16(10):837–42. Wells JCK. The evolution of human fatness and susceptibility to obesity: an ethological approach. Biol Rev. 2006 May;81(2):183–205. Wells JE, Oakley Browne M a., Scott KM, McGee M a., Baxter J, Kokaua J. Prevalence, interference with life and severity of 12 month DSM-IV disorders in Te Rau Hinengaro: The New Zealand Mental Health Survey. Aust N Z J Psychiatry. 2006 Jan;40(10):845–54. Willer CJ, Speliotes EK, Loos RJF, Li S, Lindgren CM, Heid IM, et al. Six new loci associated with body mass index highlight a neuronal influence on body weight regulation. Nat Genet. 2009 Jan;41(1):25–34. Willett W, Stampfer MJ. Re: “Total energy intake: implications for epidemiologic analyses”. Am J Epidemiol. 1986 Apr 1;124(1):17–27. Wolfe BE, Baker CW, Smith AT, Kelly-Weeder S. Validity and utility of the current definition of binge eating. Int J Eat Disord. 2009 Dec;42(8):674–86. World Health Organization. Please see the Table of Contents for access to the PDF files. Wyatt HR. Update on treatment strategies for obesity. J Clin Endocrinol Metab. 2013 Apr;98(4):1299–306. Yang J, Benyamin B, McEvoy BP, Gordon S, Henders AK, Nyholt DR, et al. Common SNPs explain a large proportion of the heritability for human height. Nat Genet. 2010 Jul;42(7):565–9. 132 M.Sc. Thesis – A. Mayhew; McMaster University – Health Research Methodology Yanovski SZ. Binge eating disorder and obesity in 2003: could treating an eating disorder have a positive effect on the obesity epidemic? Int J Eat Disord. 2003 Jan;34 Suppl:S117–120. Young LR, Nestle M. The contribution of expanding portion sizes to the US obesity epidemic. Am J Public Health. 2002 Mar;92(2):246–9. Yu W, Clyne M, Yesupriya A, Khoury MJ. A navigator for human genome epidemiology. Nat Genet. 2008;40(2):124–5. Zegers D, Beckers S, Hendrickx R, Van Camp JK, de Craemer V, Verrijken A, et al. Mutation screen of the SIM1 gene in pediatric patients with early-onset obesity. Int J Obes. Nature Publishing Group; 2014 Jul;38(7):1000–4. Zhao W, Wineinger NE, Tiwari HK, Mosley TH, Broeckel U, Arnett DK, et al. Copy number variations associated with obesity-related traits in African Americans: a joint analysis between GENOA and HyperGEN. Obesity (Silver Spring). Nature Publishing Group; 2012 Dec;20(12):2431–7. Zhu M, Zhao S. Candidate gene identification approach: progress and challenges. Int J Biol Sci. 2007 Jan;3(7):420–7. 133