Supplementary Material Journal of Neuro
advertisement

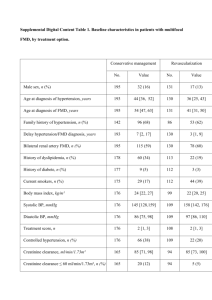
Supplementary Material Journal of Neuro-Oncology Adverse event grading following CTCAE v3.0 underestimates hypertensive side effects in patients with glioma under Bevacizumab Elisabeth Bumes*, Sarah Rzonsa*, Markus Hutterer, Martin Proescholdt, Ulrich Bogdahn, Markus J. Riemenschneider, Martin Uhl, Christina Wendl, Peter Hau *equal contribution Corresponding Author: Peter Hau, MD, Department of Neurology and Wilhelm-Sander NeuroOncology Unit, University of Regensburg Medical School, Franz Josef Strauß-Allee 11, 93053 Regensburg, Germany. Phone: 0049/941 941 0. Fax: 0049/941 941 3292. E-Mail: peter.hau@ukr.de. CTCAE Grade 1 Grade 2 Version 3.0 Asymptomatic, transient (<24 hrs) increase by >20 mmHg (diastolic) or to >150/100 if previously WNL; intervention not indicated Recurrent or persistent (≥24 hrs) or symptomatic increase by >20 mmHg (diastolic) or to >150/100 if previously WNL; monotherapy may be indicated Grade 3 Requiring more than one drug or more intensive therapy than previously Grade 4 Life-threatening consequences (e.g. hypertensive crisis) Grade 5 Death Version 4.0 Prehypertension (systolic BP 120 - 139 mmHg or diastolic BP 80 – 89 mmHg) Stage 1 hypertension (systolic BP 140 159 mmHg or diastolic BP 90 - 99 mmHg); medical intervention indicated; recurrent or persistent (≥24 hrs); symptomatic increase by >20 mmHg (diastolic) or to >140/90 mmHg if previously WNL; monotherapy indicated Stage 2 hypertension (systolic BP ≥160mmHg or diastolic BP ≥100mmHg); medical intervention indicated; more than one drug or more intensive therapy than previously used indicated Life-threatening consequences (e.g. malignant hypertension, transient or permanent neurologic deficit, hypertensive crisis); urgent intervention indicated Death Supplementary Table 1: Arterial Hypertension: Comparison of CTCAE v3.0 and v4.0 CTCAE, Common Terminology Criteria for Adverse Events; hrs, hours; WNL, within normal limits; BP, blood pressure CTC° ≥3 Hypertension Proteinuria Leukopenia Neutropenia Venous thrombembolic events Arterial thrombembolic events Bleeding Wound healing disorder BRAIN-trial arm 1* 8.3% 0% 0% 1.3% 3.6% 2.4% 0% 2.4% BRAIN-trial arm 2* 1.3% 1.3% 6.3% 8.9% 8.9% 2.5% 4% 1.3% Own data 9,5% 7.1% 7.1% 0% 2.4% 2.4% 0% 0% * Friedman HS, Prados MD, Wen PY, Mikkelsen T, Schiff D, Abrey LE, Yung WK, Paleologos N, Nicholas MK, Jensen R, Vredenburgh J, Huang J, Zheng M, Cloughesy T (2009) Bevacizumab alone and in combination with irinotecan in recurrent glioblastoma. J Clin Oncol 27 (28):4733-4740. doi:JCO.2008.19.8721 [pii] 10.1200/JCO.2008.19.8721 [doi] Supplementary Table 2: Toxicity compared to BRAIN-Trial BRAIN-trial: arm 1: BEV 10mg/kg every two weeks, arm 2: BEV 10mg/kg + IRI 125/340mg/m² every two weeks. Graded according to CTCAE version 3.0 BEV, Bevacizumab, IRI, Irinotecan; CTCAE, Common Terminology Criteria for Adverse Events