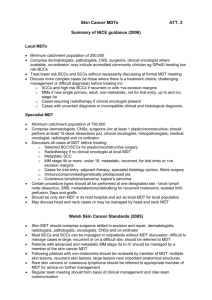
Skin Cancer: Management Guidelines for the Peninsula
advertisement

GUIDELINES FOR THE MANAGEMENT OF SKIN CANCER 11-1C-110j Agreed network-wide clinical guidelines for the management of skin cancer Agreed: April 2015 Review: April 2017 Agreement cover sheet The Guidelines of the Peninsula Cancer Network Skin Cancer Group have been agreed by: Chair Peninsula Cancer Network Skin Cancer Group Name Organisation Name Karen Davies Andrew Watts Duncan MacKenzie Tom Lucke Chris Bower Sheau Ng Karen Davies Northern Devon Healthcare NHS Trust MDT Lead Clinicians Organisation Date agreed 24/04/2012 Date agreed 24/04/2012 Northern Devon Healthcare NHS Trust Plymouth Hospitals NHS Trust 27/09/2011 Royal Cornwall Hospitals NHS Trust Royal Devon & Exeter NHS Foundation Trust South Devon Healthcare NHS Foundation Trust 27/04/2012 21/09/2011 22/09/2011 Date agreed Katie Cross Cancer Lead Clinicians Northern Devon Healthcare NHS Trust Sarah Pascoe Plymouth Hospitals NHS Trust 27/09/2011 Giles Maskell Royal Cornwall Hospitals NHS Trust 27/04/2012 John Rennison Royal Devon & Exeter NHS Foundation Trust 27/04/2012 David Sinclair South Devon Healthcare NHS Foundation Trust 27/04/2012 Name Lynne Kilner Yash Patel Sara Wright Emma Herd Andy Gordon CCG Managers for Cancer Organisation NHS New Devon Western Locality NHS New Devon Eastern Locality NHS New Devon Northern Locality NHS South Devon and Torbay NHS Kernow 27/04/2012 Date agreed Table of Contents 1 Premalignant Lesions ...........................................................................................................................................7 1.1 2 3 4 Primary care referral guidelines..................................................................................................................7 Basal Cell Carcinoma .............................................................................................................................................7 2.1 Primary care referral guidelines ...................................................................................................................7 2.2 Treatment .....................................................................................................................................................9 2.3 Incomplete excisions: ...................................................................................................................................9 2.4 BCC Follow up: ............................................................................................................................................10 Squamous Cell Carcinoma ..................................................................................................................................10 3.1 Primary care referral guidelines .................................................................................................................10 3.2 Primary treatment ......................................................................................................................................10 3.3 Discussion at MDT ......................................................................................................................................11 3.4 Follow up ....................................................................................................................................................11 3.5 Clinical Imaging ...........................................................................................................................................11 Malignant Melanoma .........................................................................................................................................11 4.1 Primary care referral guidelines .................................................................................................................11 4.2 Primary Excision..........................................................................................................................................11 4.3 Dermoscopy ......................................................................................................................................................12 4.4 Wide excision:.............................................................................................................................................12 4.5 Imaging: ......................................................................................................................................................12 4.6 Sentinel Lymph Node Biopsy ......................................................................................................................12 4.7 Completion Lymphadenectomy for Positive SLNB ...........................................................................................12 4.8 Follow up ....................................................................................................................................................12 4.9 Genetic Testing of Tumours .......................................................................................................................13 4.10 Enhanced Follow-up with Imaging for patients at increased risk of metastasis: .......................................13 4.11 Vitamin D Advice ............................................................................................................................................13 4.12 5 6 Melanocytic Lesions of Uncertain Malignant Potential .............................................................................13 Skin Lymphoma` .................................................................................................................................................13 5.1 Referral .......................................................................................................................................................13 5.2 T Cell Lymphoma ........................................................................................................................................13 5.3 Photopheresis and Total Skin Electron Beam Therapy...............................................................................14 5.4 B Cell .........................................................................................................................................................14 Merkel Cell Carcinoma........................................................................................................................................14 6.1 Adequate Local Excision .............................................................................................................................14 7 8 9 6.2 Lymph Nodes ..............................................................................................................................................14 6.3 Radiotherapy ..............................................................................................................................................15 6.4 Distant Metastases .....................................................................................................................................15 6.5 Follow-Up ...................................................................................................................................................15 Skin Cancer for Specific Groups ..........................................................................................................................15 7.1 Skin Cancer of Specific Anatomical Sites ....................................................................................................15 7.2 Skin Cancers in Children & Young People ...................................................................................................16 Immunocompromised and Transplant Patients .................................................................................................16 8.1 Initial assessment .......................................................................................................................................16 8.2 Follow up ....................................................................................................................................................17 8.3 Pre-malignant lesions .................................................................................................................................17 8.4 New or fast-growing skin tumour...............................................................................................................17 8.5 Secondary prevention .............................................................................................................................17 8.6 Alteration in immunosuppression ..............................................................................................................17 Mohs Surgery......................................................................................................................................................17 10 Community Skin Cancer Services ..........................................................................................................................17 10.1 Levels of care that may be treated in the community ..................................................................................18 10.1.1 Definition of Low Risk Basal Cell Carcinoma ...........................................................................................18 10.1.2 Providers that may diagnose and treat low risk BCCs in the Community...............................................19 10.1.3 Practitioners that may perform surgery on pre-diagnosed lesions ........................................................20 10.2 A ccreditation .................................................................................................................................................20 10.2.1 Clinical accreditation ...............................................................................................................................21 10.2.2 GPs performing skin cancer treatment within the framework of the DES or LES under ........................22 GMS or PMS ........................................................................................................................................................22 10.2.3 GPs with a Special Interest................................................................................................................25 10.2.4 Model 2 Practitioners .............................................................................................................................26 10.3 Clinical Governance .......................................................................................................................................26 10.3.1 Overlap between practitioners ...............................................................................................................27 10.3.2 Process for GPs who provide care that is outside of these guidelines ...................................................27 10.4 Quality assurance...........................................................................................................................................27 10.4.1 Histopathology ........................................................................................................................................27 10.5 Data collection and audit ...............................................................................................................................28 10.6 Educational Meeting ......................................................................................................................................28 10.7 Communication..............................................................................................................................................28 10.8 Facilities .........................................................................................................................................................29 10.9 Support Services ............................................................................................................................................29 11 The Multidisciplinary Team ...................................................................................................................................29 12 Clinical Trials ........................................................................................................................................................29 Appendix 1- Primary care referral guidelines for skin cancer ....................................................................................30 Appendix 2 - Referral guidelines between Local and Specialist MDTs .......................................................................33 Appendix 3 - Extract from the South East London Cancer Network Constitution for Skin Cancer.............................34 Appendix 4 - Levels of Care ........................................................................................................................................35 Appendix 5 – Peninsula Cancer Network Urology Site Specific Group Penile Cancer Guidelines 2009.....................37 Appendix 6 - Excision of Skin Cancer in the Community Outside of the Guidelines ..................................................38 Table of Peer Review Measures 11-1C-110j 11-1A-215j 11-1A-208j 11-1A-209j 11-1A-211j 11-1A-212j 11-1A-213j 11-1A-214j 11-1A-216j 11-1A-207j 11-1A-210j 11-1C-111j 11-1A-203j 11-1C-112j 11-1C-113j 11-6A-104j 11-6A-105j 11-1C-113j 11-1C-110j 11-6A-101j 11-1A-207j Agreed network-wide clinical guidelines for the management of skin cancer ................. 1 Arrangements with haemato-oncology teams for lymphoma involving skin ................. 13 Agreed network referral guidelines to named supra-network T-cell lymphoma MDT for TSEBT ........................................................................................................................ 14 Agreed network guidelines for referral for photopheresis............................................. 14 Arrangements for head and neck skin cancer ............................................................. 15 Arrangements for anal and perianal skin cancer.......................................................... 15 Arrangements for skin cancer of external female genitalia .......................................... 15 Arrangements for skin cancer of external male genitalia ............................................. 15 Arrangements with sarcoma MDTs for sarcoma involving skin .................................... 15 Network agreed referral guidelines between teams ..................................................... 15 Agreed network distribution of clinics for immunocompromised patients with skin cancer .................................................................................................................................... 16 NSSG designated hospital practitioners for Mohs surgery and their caseload ............. 17 Policy for the provision of skin cancer services in the community ................................ 17 NSSG agreed clinical governance arrangements for community practitioners............. 17 NSSG agreed training policy for model 2 community practitioners with named trainers/assessors ....................................................................................................... 17 named consultant dermatologist .................................................................................. 17 GPwSI training specific to skin cancer given under the supervision of a named consultant dermatologist .............................................................................................................. 18 GPwSI accreditation group should have a lead clinician of a skin MDT who should be involved in the accreditation and re-accreditation of community skin cancer clinicians 26 NSSG agreed training policy for model 2 community practitioners with named trainers/assessors ....................................................................................................... 26 Agreed network primary care referral guidelines and their distribution......................... 32 Network/PCT agreed primary care referral policy and distribution of the primary care referral guidelines........................................................................................................ 32 Network agreed referral guidelines between teams ..................................................... 33 1 Premalignant Lesions 1.1 Primary care referral guidelines Premalignant lesions may be treated by any GP in the community Includes actinic keratoses, Bowens disease (SCC in situ) 2 Basal Cell Carcinoma 2.1 Primary care referral guidelines High Risk BCC High risk of incomplete excision and recurrence, defined as: recurrent BCCs BCCs on the head (face and scalp) large BCCs > 2cm diameter unless they are superficial BCCs (see below) lesions that have a clinical appearance of morphoeic, infiltrative or basosquamous lesions with poorly defined margins BCCs in patients who are immunosuppressed or have Gorlin‟s syndrome BCCs located over important underlying anatomical structures (for example, major vessels or nerves) or where primary surgical closure may be difficult (for example, digits or front of shin). Extended Low Risk BCC There is no diagnostic uncertainty that the lesion is a primary nodular low-risk BCC and it meets the following criteria: The patient with BCC is not: aged 24 years or younger (that is, a child or young adult) immunosuppressed or has Gorlin‟s syndrome The lesion: Is not on the nose and lips (including nasofacial sulci and nasolabial folds), or around the eyes (periorbital) or ears Is less than 2 cm in diameter if below the clavicle (unless they are superficial BCCs see below). Is less than 1 cm in diameter if above the clavicle (unless they are superficial BCCs see below). Refer to core member of Local MDT Suspected BCCs should usually be referred as routine. Consider 2 week referral if there is particular concern that delay may have an impact because of site or size of lesion. Refer to either Core member of local MDT Or Group 3 GPwSI in dermatology and skin surgery Or Group 3a GPwSI in skin lesions and skin surgery Suspected BCCs should usually be referred as routine. Consider 2 week referral if there is particular concern that delay may have an impact because of site or size of lesion. Is not morphoeic, infiltrative or basosquamous in appearance Does not have poorly defined margins Is not located: o over important underlying anatomical structures (for example, major vessels or nerves) o in an area where primary surgical closure may be difficult (for o example, digits or front of shin) in an area where excision may lead to a poor cosmetic result. If any of the above exclusion criteria apply, or there is any diagnostic doubt, the patient should be referred to the LSMDT. Incompletely excised BCCs should be discussed with a member of LSMDT Low Risk BCC There is no diagnostic uncertainty that the lesion is a primary nodular low-risk BCC and it meets the following criteria: The patient with BCC is not: aged 24 years or younger (that is, a child or young adult) immunosuppressed or has Gorlin‟s syndrome The lesion: is located below the clavicle (that is, not on the head or neck) is less than 1 cm in diameter with clearly defined margins is not a recurrent BCC following incomplete excision is not a persistent BCC that has been incompletely excised according to histology is not morphoeic, infiltrative or basosquamous in appearance is not located o over important underlying anatomical structures (for example, major vessels or nerves) o in an area where primary surgical closure may be difficult (for example, digits or front of shin) o in an area where difficult excision may lead to a poor cosmetic Refer to either Core member of local MDT Or Group 3 GPwSI in dermatology and skin surgery Or Group 3a GPwSI in skin lesions and skin surgery Or GP accredited in Skin Cancer Suspected BCCs should usually be referred as routine. Consider 2 week referral if there is particular concern that delay may have an impact because of site or size of lesion. o result at another highly visible anatomical site (for example, anterior chest or shoulders) where a good cosmetic result is important to the patient. Incompletely excised BCCs should be discussed with a member of the LSMDT. BCC where there is any doubt about high or low risk status Refer to core member of Local MDT Superficial BCCs – on the face Refer to core member of Local MDT Superficial BCCs – not on the face If the lesion is thought to be a superficial BCC the GP should ensure that the patient is offered the full range of medical treatments, including photodynamic therapy. This may require referral to the LSMDT. Refer to either Core member of local MDT Or Group 3 GPwSI in dermatology and skin surgery Or Group 3a GPwSI in skin lesions and skin surgery Or GP accredited in Skin Cancer 2.2 Treatment BCC Type Small well-defined BCCs on trunk and limbs Superficial BCCs High-risk BCCs Treatment excision (with 3-4mm margin) or curettage & cautery excision, cryotherapy, imiquimod, 5-fluorouracil, curettage or PDT: all treatment options guided by site, size, clinician and patient preference Surgical excision with at least 4mm margins Monitoring rather than immediate treatment may be appropriate in cases of asymptomatic BCC in a patient with a short life expectancy. Consider Mohs surgery for more difficult and high risk cases such as: Recurrent BCC Poorly defined BCC Aggressive histology High risk sites Where tissue conservation is particularly important Radiotherapy may be useful, particularly for patients unwilling or unable to tolerate surgery. 2.3 Incomplete excisions: Lateral margins Deep margins Offer re-excision or observation Recommend immediate re-excision (and possibly Mohs) unless patient very elderly in which case observation may be more appropriate, or consider radiotherapy. 2.4 BCC Follow up: Complete excision or other definitive treatment – no follow up required, re-referral by GP if any sign of recurrence. Exceptions where follow-up may be appropriate: Skin graft/flap reconstruction: review once at 3 months in selected cases to check cosmesis/complications. • High tumour load (ie 2 or more new BCCs per year or previous history of >10 BCCs). This decision to be at the discretion of the treating clinician. • Incomplete excision and opt for observation- consider follow-up 6 monthly for 1 year, then annually for 2 years- or discuss self-observation or GP follow-up. • Treatment with PDT/Imiquimod/Cryotherapy/C&C. Consider review once at 3 months to check on effectiveness of treatment. 3 Squamous Cell Carcinoma 3.1 Primary care referral guidelines Squamous Cell Carcinoma Keratoacanthoma 3.2 2 Week Referral to core member of Local MDT 2 Week Referral to core member of Local MDT Primary treatment SCC Type Treatment Excision with ≥6 mm clinical margins (see below). High risk SCC High risk is defined as one or more risk factors for recurrence or metastasis. The risk factors are defined as: poorly differentiated, recurrent tumours, tumours >2cm across, perineural or lymphovascular extension histologically depth > 6mm transplant or immunosuppressed patients large >2cm lesions site: ear/lip/non-sun-exposed SCCs developing in scars/sinuses/chronic inflammation Low risk SCC Excision with ≥4 mm clinical margins Low risk is defined as not high risk. This therefore includes: Well differentiated tumours with no risk factors Moderately differentiated tumour with no risk factors Small well-defined and obviously well-differentiated tumours in elderly patients may be suitable for treatment via curettage and cautery by practitioners experienced in this technique. Also in patients with high tumour load, where patient is already having long-term follow-up. Re-excision If incomplete re-excise with 5mm margin. Further treatment Dependent upon relative risk of tumour metastasising/recurring. Adjuvant radiotherapy should be considered for large poorly differentiated tumours and those close to excision margins. 3.3 Discussion at MDT Completely excised, well differentiated SCCs need not be discussed at the MDT All other SCCs (ie any incompletely excised SCCs or any moderately or poorly differentiated SCCs) should be discussed that the MDT 3.4 Follow up SCC Type High risk SCC Follow up Consider 3 or 6 monthly follow-up for 2 – 5 years depending on clinical situation (more need for follow-up if more than 1 poor prognostic factor present). Examine for local recurrence, and lymph node draining basins. Consider GP or patient self follow-up if appropriate/acceptable Low risk SCC None required Risk factors should be identified at the time of treatment by the dermatologist. All patients should be made aware of the sign or symptoms that should prompt them to seek medical advice. The Skin Cancer Service should ensure those patients who have problems can quickly and easily be seen by the skin cancer service. 3.5 Clinical Imaging High-risk SCC require CT for recurrent tumours Not required for other primary SCC unless clinically indicated eg lymphadenopathy. 4 Malignant Melanoma 4.1 Primary care referral guidelines Melanoma 4.2 Primary Excision 2-5mm clinical margins 2 Week Referral to core member of Local MDT 4.3 Dermoscopy All pigmented lesions referred for assessment should be assess using dermoscopy carried out by healthcare professional strained in this technique 4.4 Wide excision: Dependent on staging: Lentigo maligna In-situ MM Stage 1 melanoma Stage 2 and above melanoma 4.5 Imaging: Stage III and above: 4.6 5mm excision clinical margin to achieve complete histological excision 5mm margin to achieve complete histological excision 1cm margin at least 2 cm margin Staging CT required Sentinel Lymph Node Biopsy Sentinel Lymph Node Biopsy may be offered to patients with melanoma more than 1mm Breslow thickness. Patients should be offered SLNB as a staging tool and advised about advantages and disadvantages (see NICE guideline NG14 July 2015). Patients should be advised about possible clinical trials and allowed to make an informed choice. 4.7 Completion Lymphadenectomy for Positive SLNB Consider completion lymphadenectomy for people whose SLNB shows micro metastases. Give the patient verbal and written information about advantages and disadvantages as per the NICE guidelines NG14 July 2015. 4.8 Follow up LM or in-situ MM Stage IA Stage IB or above One follow up and then discharge 3 or 6 monthly for 1 year 3 monthly for 3 years, then 6 monthly for a further 2 years At follow up: Examination of scar, in-transit metastases, lymph node basins, liver. General skin check. Discuss self-examination. 4.9 Genetic Testing of Tumours If targeted systemic therapy is a treatment option, offer genetic testing (BRAF etc) on: - the secondary deposit if this is possible, or - the primary if there is no adequate sample from the secondary 4.10 Enhanced Follow-up with Imaging for patients at increased risk of metastasis: (stage 2C with no SLNB, or stage 3) who would be eligible for systemic therapy: Offer patients enhanced follow-up with CT scans chest/abdo/pelvis 6 monthly for 3 years. Consider CT brain for adults. Advise MRI scanning for those under 24 years. Advise patients of advantages and disadvantages (see NICE guideline NG14 July 2105) 4.11 Vitamin D Advice The peninsula network has agreed there is no good evidence for routine measurement of Vitamin D levels in patients with primary melanoma. All melanoma patients should be advised about vitamin D supplementation if they are sun avoiding. There is a very small risk of renal stones with this treatment. 4.12 Melanocytic Lesions of Uncertain Malignant Potential These should be managed as melanoma 5 Skin Lymphoma` 5.1 Referral Systemic or nodal lymphomas should be referred to the haemato-oncology MDTs. Primary cutaneous lymphoma should be discussed at the Skin SSMDTs. 11-1A-215j Arrangements with haemato-oncology teams for lymphoma involving skin 5.2 T Cell Lymphoma Patients may be referred to the Lymphoma Service in Bristol, or to St Johns Institute. St John‟s Institute of Dermatology (Guy‟s & St Thomas‟ NHS Foundation Trust) is the Supra Network T-cell Lymphoma MDT to which the Peninsula relates. It is part of the South East London Cancer Network. See Appendix 3 for the relevant extract from the South East London Cancer Network Skin NSSG Constitution. Stage above 1b: consider/ offer referral to Lymphoma Unit, BUT may not be appropriate or feasible in certain clinical situations eg: single isolated tumours very ill erythrodermic patients who are unable to travel 5.3 Photopheresis and Total Skin Electron Beam Therapy Patients with erythrodermic cutaneous T cell lymphoma (stage 3 and 4) should be referred to the Lymphoma Unit for consideration of photopheresis. Patients with nodular mycosis fungoides (Stage 2b or over) should be referred to St John‟s for consideration of Total Skin Electron Beam Therapy. Some patients may be given Total Skin Electron Beam Therapy locally (in Plymouth) if this is more acceptable for the patient and where the management has been planned by St John‟s. 11-1A-208j Agreed network referral guidelines to named supra-network T-cell lymphoma MDT for TSEBT 11-1A-209j Agreed network guidelines for referral for photopheresis 5.4 B Cell For systemic disease: refer to haematology as above. For primary cutaneous disease: Multiple or recurrent lesions: refer to St Johns Local isolated disease: local skin/ haematology SSMDT 6 Merkel Cell Carcinoma The principles of the management or Merkel cell carcinoma include: All patients should be discussed at SSMDT wide local excision possible frozen section to confirm clearance possible SLNB to assess lymph nodes possible radiotherapy It was agreed that there is no strong evidence base for treatment options. It was agreed that these can be fast growing tumours and that wider excision should be timely, in line with melanoma management. 6.1 Adequate Local Excision Clinical local excision margins of 1-2cm Aim for 1cm margin for tumour less than 2cm diameter. Aim for 1- 2cm margin for tumour greater than or equal to 2cm diameter. Consider using frozen section to confirm margins at time of operation. If performing wider excision where original margins incomplete or close: ensure procedure is arranged urgently (as tumours are potentially fast growing). 6.2 Lymph Nodes Consider SLNB for patients who are clinically node negative. For patients who are lymph node positive: Fine Needle Aspirate or Open Biopsy If nodes positive then consider lymph node dissection (to improve loco-regional control). If nodes positive then CT scan. 6.3 Radiotherapy Consider for: Large tumour >2cm Lymph node involvement 6.4 Distant Metastases Consider radiotherapy/ chemotherapy. 6.5 Follow-Up As per melanoma patients ie 3 monthly for 3 years, then 6 monthly for further 2 years. With thanks to Suyin Ong for drafting these guidelines 7 Skin Cancer for Specific Groups 7.1 Skin Cancer of Specific Anatomical Sites The pathology for these cases should be referred to the following specified MDTs for an opinion on management. Anatomical Site Head & Neck Cancer Type Nasal Mucosal MM Ocular Mucosal MM Periocular Anal Cancer External female genitalia Any SCC MM BCC Any External male Genitalia/Penile Any Rare Tumours MDT to refer to Head And Neck MDT Ophthalmologists refer to oncologists Oculoplastic/Plastic as Extended Member Of Skin MDT Colorectal MDT Gynae MDT Skin And Gynae MDT Skin And Gynae MDT Avon Somerset& Wilshire Supranetwork MDT (see PCN Guidelines for Penile Cancer – Appendix 5) Sarcoma MDT Exeter or Plymouth Any SSMDT 11-1A-211j Sarcoma (see below) Other rare tumours (see list below) Arrangements for head and neck skin cancer 11-1A-212j Arrangements for anal and perianal skin cancer 11-1A-213j Arrangements for skin cancer of external female genitalia 11-1A-214j Arrangements for skin cancer of external male genitalia 11-1A-216j Arrangements with sarcoma MDTs for sarcoma involving skin 11-1A-207j Network agreed referral guidelines between teams Sarcoma includes all dermal and subcutaneous tumours, namely: Dermatofibrosarcoma protuberans. Leiomyosarcoma. Angiosarcoma. Kaposi‟s sarcoma. Haemangioendothelioma. Epithelioid sarcoma. Primary cutaneous rhabdomyosarcoma. Cutaneous malignant nerve sheath tumours (including cutaneous neurofibrosarcoma and malignant Schwannoma). Other Rare Tumours Merkel Cell Tumours Apocrine carcinoma. Hidradenocarcinoma. Eccrine porocarcinoma. Sebaceous carcinoma. Tumours associated with Muir–Torre syndrome Eccrine epithelioma (syringoid carcinoma) Microcystic adnexal carcinoma Primary adenoid cystic carcinoma Primary mucoepidermoid carcinoma Primary mucinous carcinoma Digital papillary adenocarcinoma Malignant cylindroma Malignant spiradenoma (spiradenocarcinoma) Malignant pilar tumour Malignant pilomatrixoma Neuroendocrine carcinoma (Merkel cell tumour/trabecular carcinoma) Atypical fibroxanthoma 7.2 Skin Cancers in Children & Young People All children (ages 0-16) and young people (ages 16-24) with skin cancer should be discussed with the local lead consultant for children & young people‟s cancer. This should happen as soon as is practical. 8 Immunocompromised and Transplant Patients Clinics/allocated slots for transplant patients to be held at all 5 centres NDH PHT RCH RDE SDH Dr Karen Davies Dr Cairine Wilkinson Dr Samantha Hann Dr Rebecca Batchelor Dr Ng Sheau Clinics to be held 1 – 3 monthly depending on need/ numbers 11-1A-210j Agreed network distribution of clinics for immunocompromised patients with skin cancer 8.1 Initial assessment 1 year post transplant: advice and information particularly sun protection and self monitoring. Assessment for high risk factors including: older patients white skinned patients who have had excess sun exposure presence of pre-malignant warty lesions or actinic keratoses 8.2 Follow up Frequency of follow-up to be decided by clinician on basis of clinical need. This should be annual follow-up as an ideal minimum, but then 3-6 monthly for patients with skin cancers, depending on various factors including tumour type and presence of high risk factors (eg poorly differentiated SCC). 8.3 Pre-malignant lesions There should be active treatment of all pre-malignant lesions. 8.4 New or fast-growing skin tumour Patients should be given instructions on how to access service at short notice in the event of a new or fast-growing skin tumour. 8.5 Secondary prevention Retinoids and/or reduction of immunosuppression as below should be considered. 8.6 Alteration in immunosuppression Transplant physicians should be contacted with regard to possible alteration in immunosuppression particularly with: >25 NMSCs per yr high risk SCC Merkel cell tumour melanoma especially stage 11a or above Management will vary according to type of transplant. 9 Mohs Surgery 11-1C-111j NSSG designated hospital practitioners for Mohs surgery and their caseload The only practitioners authorised to carry out Mohs surgery (including 'Slow Mohs surgery') are the following: Dr Samantha Hann, Dr Tom Lucke (RCHT) Dr Chris Bower, Dr Emily McGrath (RD&E) The Mohs surgery practice is well established in Cornwall, and has started in Exeter. 10 Community Skin Cancer Services This section covers the protocols for the accreditation, training and Governance of skin cancers services carried out in the community. 11-1A-203j Policy for the provision of skin cancer services in the community 11-1C-112j practitioners NSSG agreed clinical governance arrangements for community 11-1C-113j NSSG agreed training policy for model 2 community practitioners with named trainers/assessors 11-6A-104j GPwSI training specific to skin cancer given under the supervision of a named consultant dermatologist All healthcare professionals managing skin lesions in the community should have specialist training in the diagnosis and management of skin lesions appropriate to their role. All GPs who diagnose, manage and excise low-risk BCCs in the community should be fully accredited to do so and undergo continuous professional development in the diagnosis and management of skin lesions to maintain their accreditation. All Services for low-risk BCCs should adhere to national cancer peer review measures. 10.1 Levels of care that may be treated in the community The Levels of Care can be found at Appendix 4. Level of Care 1 2 (low risk BCCs) 3 4 5 6 Practitioners who may diagnoses & treat in the community All GPs and MDT members See below Community outreach from Local or Specialist MDT Community outreach from Local or Specialist MDT Community outreach from Specialist MDT None 10.1.1 Definition of Low Risk Basal Cell Carcinoma Diagnosis Low Risk BCC Criteria There is no diagnostic uncertainty that the lesion is a primary nodular low-risk BCC and it meets the following criteria: The patient with BCC is not: aged 24 years or younger (that is, a child or young adult) immunosuppressed or has Gorlin‟s syndrome The lesion: is located below the clavicle (that is, not on the head or neck) is less than 1 cm in diameter with clearly defined margins is not a recurrent BCC following incomplete excision is not a persistent BCC that has been incompletely excised according to histology is not morphoeic, infiltrative or basosquamous in appearance is not located o o over important underlying anatomical structures (for example, major vessels or nerves) in an area where primary surgical closure may be difficult (for example, digits or front of shin) o in an area where difficult excision may lead to a poor cosmetic result o at another highly visible anatomical site (for example, anterior chest or shoulders) where a good cosmetic result is important to the patient. See below for superficial BCCs Extended Low Risk BCC Incompletely excised BCCs should be discussed with a member of the LSMDT. There is no diagnostic uncertainty that the lesion is a primary nodular low-risk BCC and it meets the following criteria: The patient with BCC is not: aged 24 years or younger (that is, a child or young adult) immunosuppressed or has Gorlin‟s syndrome The lesion: Is not on the nose and lips (including nasofacial sulci and nasolabial folds), or around the eyes (periorbital) or ears Is less than 2 cm in diameter if below the clavicle (unless they are superficial BCCs see below). Is less than 1 cm in diameter if above the clavicle (unless they are superficial BCCs see below). Is not morphoeic, infiltrative or basosquamous in appearance Does not have poorly defined margins Is not located: o over important underlying anatomical structures (for example, major vessels, nerves or temple) o in an area where primary surgical closure may be difficult (for example, digits or front of shin) o in an area where excision may lead to a poor cosmetic result. If any of the above exclusion criteria apply, or there is any diagnostic doubt, the patient should be referred to the LSMDT. Superficial BCCs Incompletely excised BCCs should be discussed with a member of LSMDT. If the lesion is thought to be a superficial BCC the GP should ensure that the patient is offered the full range of medical treatments, including photodynamic therapy. This may require referral to the LSMDT. All superficial BCCs on the face should be referred to the LSMDT 10.1.2 Providers that may diagnose and treat low risk BCCs in the Community Provider Accreditation Community outreach from Local or Specialist MDT (a consultant led service that may include staff grade and Training is covered by conventional specialty training in dermatology, and practitioners are subject to the MDT associate specialist doctors measures for core members in the BCCs that can be treated All and specialist nurses. Group 3 GPwSI in dermatology and skin surgery Manual for Cancer Services. On PCT GPwSI list 1,2 Annually accredited by Local MDT according to Error! Reference source not found. Group 3a GPwSI in skin lesions and skin surgery On PCT GPwSI list 1 (Completion of SS1 and SS2 modules of GPwSI training (without having completed full GPwSI training) Annually accredited by Local MDT according to Error! Reference source not found. Annually accredited by Local MDT according to Error! Reference source not found. GPs performing skin surgery within the framework of the Directed Enhanced Services and Local Enhanced Services under General Medical Services or Personal Medical Services Exte nded Low Risk BCCs Exte nded Low Risk BCCs Low Risk BCC s 1 Department of Health (2007) Guidance and competencies for the provision of services using GPs with special interests (GPwSIs): dermatology and skin surgery. Available from: http://www.dh.gov.uk/en/Publicationsandstatistics/Publications/PublicationsPolicyAndGuidance/DH_074665 Department of Health (2007) Implementing care closer to home: convenient quality care for patients. Part 3: the accreditation of GPs and pharmacists with special interests. London: Department of Health 2 Revised guidance and competences for the provision of services using GPs with Special Interests (GPwSIs) 10.1.3 Practitioners that may perform surgery on pre-diagnosed lesions Model 2 Practitioners A Model 2 practitioner should be one of the following: a medical practitioner performing skin surgery in a community setting a suitably trained specialist nurse. Model 2 practitioners can perform surgery on pre-diagnosed lesions including the full range of BCCs as well as other types of skin cancer provided that they have demonstrated surgical competence surgery is performed after the lesions have been diagnosed by an MDT member and a management plan identified. 10.2 A ccreditation All community skin cancer clinicians should identify the Local Skin Cancer MDT to which they relate. Good communication should be established to ensure the consistency and continuity of services for patients. The accreditation and governance arrangements are set out in the table below. Service Clinical accreditation by MDT Placed on PCT GPwSI list Community outreach from Local or Specialist MDT (a consultant led service that may include staff grade and associate specialist doctors and specialist nurses. Model 2 Practitioners Assumed through consultant led service No Yes No Group 3 GPwSI in dermatology and skin surgery Yes Yes Group 3a GPwSI in skin lesions and skin surgery Yes Yes GPs performing skin surgery within the framework of the DES and LES Enhanced Services under GMS or PMS Yes No, but placed on PCT list for GPs performing skin surgery within the framework of the DES and LES Enhanced Services under GMS or PMS *Some GPs may be accredited as both a GPwSI and a Model 2 practitioner. Employer responsible for clinical governance Acute Trust hosting MDT Acute Trust hosting MDT GP Practice or GPwSI (depending on contractual arrangement s) GP Practice or GPwSI (depending on contractual arrangement s) GP Practice 10.2.1 Clinical accreditation Clinical accreditation will only assure competency and knowledge at the time and setting of accreditation. It does not confer any responsibility on the MDT for the actual service. Nor does it make any judgment on the suitability of the service model or environment in which the service is carried out. These issues are a matter for the clinical governance of the provider and their commissioner. 10.2.2 GPs performing skin cancer treatment within the framework of the DES or LES under GMS or PMS There are contractual requirements for GPs and other primary care health care professionals performing skin surgery within the framework of the DES under General or Personal Medical Services. National guidance sets out how these contractual requirements should be assessed. These are set out below with an indication of the method of assessment. Contractual requirements for GPs and other primary care health care professionals performing skin surgery within the framework of the DES under General or Personal Medical Services Contractual Measures of competency and activity against these Assessment requirement requirements method The contractor ensures A. Has a new skin surgery practitioner demonstrated Skin Cancer that any health care competency to a suitably qualified external body Course professional who is using objective evidence and competency based involved in performing assessment tool (ie Direct Observation of any surgical Procedural Skills, known as DOPS)? procedures has: Skin Cancer B. Has an existing practitioner demonstrated Course competency to perform the designated i. any necessary procedure(s) to a suitably qualified external body experience, using objective skills and evidence and competency based assessment training with tools within the preceding three years? DOPS regard to that assessment is appropriate procedure C. Does the practitioner continue to perform skin Revalidation to surgery with a regular, sustained level of activity and ii. resuscitation skills assess that follow a program of revalidation? 100 skin surgery at least 20 procedures per year that leave a scar (excluding cases of skin cryosurgery) is recommended. If less than 100 cancer have procedures per year are performed, it is suggested been treated that the practitioner demonstrate ongoing per year competency to perform the designated procedure(s) by completion of further DOPS assessments at Commission three yearly intervals, unless the activity increases er to asses to the recommended amount that at 100 skin surgery procedures per year that leave a scar (excluding cryosurgery) are undertaken (accounting for suspected skin cancer and non skin cancer procedure s) The contractor: i. obtains written consent for the surgical procedure before it is carried out (where a person consents on a patient‟s behalf, that person‟s relationship to the patient must be recorded on the consent form), and takes all reasonable steps to ensure that the consent form is included in the lifelong medical records held by the patient‟s general practitioner The contractor ensures that all tissue removed by surgical procedures is sent for histological examination, unless there are acceptable reasons for not doing so D. Has the practitioner demonstrated training and ongoing medical education in the recognition and management of skin lesions appropriate to their role (for example, a practice nurse performing skin surgery on pre-diagnosed skin lesions will have different skin lesion diagnostic skill requirements to a GP diagnosing and excising lesions)? E. Does the practitioner have evidence of annual training in resuscitation? F. Is the practitioner familiar with Department of Health and General Medical Council guidance on informed consent, particularly in relation to the Mental Capacity Act and obtaining consent from minors, and has best practice as detailed in these guidance documents been adopted? Skin Cancer Course G. Does the practitioner send all skin specimens removed to histology for analysis and provide information about the site of excision and provisional diagnosis on the histology request form? H. Does the practitioner maintain a ‟fail-safe„ log of all procedures performed with histological outcome to ensure that patients are informed of the final diagnosis, and whether any further treatment or follow-up is required? Is this undertaken in a timely fashion? I. Is the practitioner aware of, and following, all Skin Cancer Course Revalidation Commission er to assess Skin Cancer Course ii. The contractor Revalidation Revalidation Commission ensures that it has appropriate arrangements for infection control and decontamination in premises where surgical procedures are undertaken The contractor ensures that all records relating to all surgical procedures are maintained in such a way: i. that aggregated data and details of individual patients are readily accessible for lawful purposes, and ii. as to facilitate regular audit and peer review by the contractor of the performance of surgical procedures under the plan relevant national guidance in relation to policies and procedures (for example premises, facilities, infection control, needlestick injuries etc)? er to assess J. Does the practitioner provide evidence of an annual review of clinical compared with histological accuracy in diagnosis to demonstrate diagnostic competency? K. Has a wound infection and patient experience study Revalidation been completed? L. When low risk BCCs are excised, does the practitioner demonstrate that the requirements in Improving Outcomes for people with skin tumours including melanoma (update) - The management of low-risk basal cell carcinomas (May 2010) are met (see Annex E). M. Is the above considered as part of the annual appraisal process? Revalidation Revalidation Revalidation Skin Cancer Course Skin Cancer Courses will be run in the Peninsula to train and accredit GPs against measures A, B, D, F & G and the following appropriate treatment selection. performance of local anaesthesia, punch biopsy, shave excision, curettage and elliptical excision. knowledge of NICE and Peninsula Skin Cancer Guidance for treatment of skin cancer. Accreditation will involve completion of 4 satisfactory formal assessments: 2 clinical assessments (modified mini-CEX) relating to diagnosis of benign and malignant skin lesions 2 DOPS (Directly Observed Practices) assessments relating to surgical procedures Fulfilment of the above criteria is likely to require attendance at secondary care clinics for training, unless the practitioner can demonstrate adequate previous experience and quality of care. Initial Accreditation GPs operating on Skin Cancer will need to attend a Skin Cancer Course that fulfils the requirements set out above and be accredited as having met the clinical requirements of the course. Be accredited by their commissioner against measures C, E & I. be linked to a named skin cancer MDT and be accredited by the Skin MDT Lead. Revalidation GPs should attend an annual Skin Cancer Review. This will be organised by the Peninsula Cancer Network. GPs should collect and present information at this annual review sufficient to demonstrate: Measure C specifically the treatment, using any modality, of at least 20 cases of suspected skin cancer in the previous year. Measure D – specifically one CPD session (a total of 4 hours) on skin lesion recognition and the diagnosis and management of low-risk BCCs Measure G (histology) Measure H (fail safe log) Measure J – specifically that at least 90% of excisions of skin cancers have a clear margin Measure L (compliance with Guidance) Measure M (annual appraisal) Measure J - specifically a diagnostic accuracy of 70% (ie clinical vs. histological diagnosis) for the low-risk BCCs they have managed. GPs that are unable to meet these revalidation requirements will need to undergo further training and accreditation as per initial accreditation. Practitioners operating on Skin cancer in the Community should follow these guidelines (Section 9.5 – 9.9) regarding facilities and support services (Community skin services may only be carried out in facilities approved by the PCT), data collection and audit, and communication. 10.2.3 GPs with a Special Interest This accreditation applies to: Group 3 GPwSI in dermatology and skin surgery Group 3a GPwSI in skin lesions and skin surgery A new „Group 3a GPwSI in skin lesions and skin surgery‟ is being developed by the Department of Health whose role is as follows: training and accreditation to the same standard as the „Group 3 GPwSI in dermatology and skin surgery‟ but for skin lesions only (excluding the inflammatory skin disorders) all other criteria, including referral pathways, link to the MDT, clinical governance arrangements and CPD requirements, to match the Group 3 GPwSI in dermatology and skin surgery Initial accreditation GPwSIs performing skin surgery should follow the framework for the training and accreditation of GPwSIs, which is defined by the Department of Health as follows: they are accredited by the PCTs according to national guidance appropriate to their role as GPwSIs. This will include demonstrating competency in performing local anaesthesia, punch biopsy, shave excision, curettage and elliptical excision using the direct observation of procedural skills (DOPS) assessment tool in the Department Health Guidance for GPwSIs in dermatology and skin surgery. t e GPwSI is linked to a named skin cancer MDT. h Revalidation GPwSIs will need to maintain accreditation annually and should: demonstrate adherence to the requirements for community skin cancer clinicians specified in the dermatology and skin surgery GPwSI guidance. Fulfil the revalidation requirements set out for GPs performing skin surgery within the framework of the DES or LES under GMS or PMS (see above). attend four MDT meetings per year skin cancer clinical practice is audited annually as defined in the GPwSI guidance GPwSIs who are unable to meet these revalidation requirements will need to undergo further training and accreditation as per initial accreditation. 11-6A-104j GPwSI training specific to skin cancer given under the supervision of a named consultant dermatologist 11-6A-105j GPwSI accreditation group should have a lead clinician of a skin MDT who should be involved in the accreditation and re-accreditation of community skin cancer clinicians 10.2.4 Model 2 Practitioners Initial accreditation Model 2 practitioners should: be trained in and have demonstrated competency in skin surgery techniques (as per SS1 and SS2 frameworks in the GPwSI guidance) be associated with a named MDT perform surgery on pre-diagnosed skin cancers, receiving referrals from core MDT members with an agreed treatment plan. Revalidation Practitioners will need to maintain accreditation annually and should demonstrate: Measure C specifically the treatment, using any modality, of at least 20 cases of suspected skin cancer in the previous year. Measure D – specifically one CPD session (a total of 4 hours) on skin the management of lowrisk BCCs Measure G (histology) Measure H (fail safe log) Measure J – specifically that at least 90% of excisions of skin cancers have a clear margin Measure L (compliance with Guidance) Measure M (annual appraisal) Model 2 Practitioners who are unable to meet these revalidation requirements will need to undergo further training and accreditation as per initial accreditation. 11-1C-113j NSSG agreed training policy for model 2 community practitioners with named trainers/assessors 10.3 Clinical Governance All providers of community dermatology services that include skin cancer should ensure that: Clinical governance arrangements are in place for all healthcare professionals providing these services (including private providers contracted to treat NHS patients) and they are accredited to perform skin lesion excisions. All healthcare professionals providing these services work in accordance with the Network Skin Cancer Guidelines (covering referral, treatment and follow-up. Healthcare professionals managing skin lesions in the community should obtain informed consent before any treatment is undertaken. The clinical governance therefore sits with the employer of individual practitioners. PCTs will want to be assured that this is in place for all providers that they commission services from. As the Guidance states that the clinical governance for Model 2 practitioners sits with the MDT, the MDT will want either to directly employ the Model 2 practitioner (for the relevant sessions) or formally subcontract with the practitioner. Other, informal, relationships will compromise the ability of the MDT to discharges its clinical governance responsibilities for which it is accountable. 10.3.1 Overlap between practitioners An individual practitioner may be accredited in more than one group ie: GPwSIs Model 2 practitioner GPs working under the DES or LES It is the responsibility of the practitioner and their employer to ensure that there is clarity about which role the practitioner is operating under and to ensure that the relevant guidance is followed in all cases. 10.3.2 Process for GPs who provide care that is outside of these guidelines All GPs who perform treatment outside of these guidelines will be sent the statement “Excision of Skin Cancer in the Community Outside of the Guidelines” (Appendix 6). Each MDT and its lead PCT will agree which party sends the statement. All occasions of GPs operating outside of these Guidelines will be shared with the PCT. GPs who continue to operate outside of these guidelines will be subject to the PCTs Poor Performance Process1 Where a patient needs further treatment, a letter will be sent from the MDT specifying the actions that should be taken by the GP. 10.4 Quality assurance 10.4.1 Histopathology All skin lesion samples (excision, incision, punch biopsy and curettage) should be sent for histological examination as recommended in the NICE „Referral guidelines for suspected cancer‟. This should provide information about the site of excision and provisional diagnosis on the histology request form. If a person has more than one lesion, samples should be sent in separate specimen pots with referral forms. Histology request and reporting forms, and the electronic recording of these data items, should be improved to capture the national skin cancer minimum dataset requirements2 and the Royal College of Pathology dataset). All healthcare professionals should have a failsafe mechanism in place to ensure that they receive results for the skin lesion samples they send for histological assessment and act upon the results. This means that: all samples sent to the laboratory should be accompanied with a numerical checklist any sample not received by the laboratory should be immediately notified to the operating GP all results should be cross checked to ensure they have been seen and actioned. Healthcare professionals should take appropriate action if the histology result reclassifies the lesion as a high-risk BCC or a SCC, malignant melanoma or other rare skin tumour and refer to approved specialists as recommended in „Improving outcomes for people with skin tumours including melanoma‟ (NICE guidance on cancer services). The following histological criteria denote high-risk BCC: incomplete excision margins morphoeic, infiltrative, micronodular or basosquamous perineural invasion below the dermis. Each PCT should commission histopathology skin cancer services that clearly identify each individual healthcare professional. Audit data should be presented in an anonoymised fashion using individual identifier numbers, but individual healthcare professionals and PCTs should be given data that is identifiable. GPs operating under DES/LES should send their low-risk BCC samples to the main histopathology laboratory that are linked to their local MDT. 1 NHS Devon - Policy And Procedures For Managing General Practitioners, Dentists And Pharmacists In Devon Whose Performance Gives Cause For Concern NHS Cornwall & IOS – Cause for Concern Process 2 National Cancer Intelligence Network dataset project [in development Available from the National Cancer Intelligence Network (NCIN): http://www.ncin.org.uk/index.shtml 10.5 Data collection and audit Healthcare professionals managing low-risk BCCs in the community should maintain a written or electronic record of the suspected and actual skin cancers they have managed in their individual caseload. This will need to specify the treatments offered and carried and the rationale for choosing a particular treatment modality. As required by the „Manual for cancer services 2008: skin measures‟ all BCCs excised by healthcare professionals in the community should be audited. The PCT should make these audit results available to the multidisciplinary team (MDT), cancer network and the individual practitioner on a quarterly basis and they should be included in the cancer network annual audit (cancer standards 08-6A-103J36). The quarterly dataset should be a standard PCT contract monitoring item for the DES. Individual healthcare professionals should be responsible for collating their individual audit data for revalidation. The MDT should source suitable patient reported outcome measures for the treatment of BCCs. All BCCs should be registered with cancer registries to allow national, regional and local epidemiology and health service epidemiological studies to take place. 10.6 Educational Meeting The Skin Cancer Network Site Specific Group should run two educational meetings per year, which should: present the 6-monthly BCC network audit results, including a breakdown of individual practitioner performance include one CPD session (a total of 4 hours) on skin lesion recognition and the diagnosis and management of low-risk BCCs 10.7 Communication All healthcare professionals managing BCCs in the community should provide information, advice and support for patients and their families or carers. 10.8 Facilities Community skin services may only be carried out in facilities approved by the PCT (with guidance as appropriate by the MDT). Facilities should be assessed for: Operating equipment Lighting Storage and use of liquid nitrogen (if being used, should be in line with Health and Safety guidance) Infection control and decontamination issues 10.9 Support Services Community skin cancer services are responsible for: The provision of information, advice and support for patients managed in primary care and their carers Assessment and management of risk within the service Community skin cancer services should have their own guidelines to include: Type of patients seen Frequency of consultations Range of interventions Referral criteria Communication pathways Confidentiality Community skin cancer services must be supported by: Adequate record keeping and appropriate documentation Close links to the Skin MDT Clinical audit programme, including patient satisfaction survey Complaints process and review Incident reporting process and review, including significant event monitoring 11 The Multidisciplinary Team The Following principles apply to the members of MDTs to ensure the correct decisions are made to ensure best treatment. Dermatologists who regularly treat skin cancer (and where this is a significant part of their workload) should be a core member of their local MDT Those who do skin cancer work as a low percentage of their overall work (eg 10% of their workload) – and this will often apply to Plastic Surgeons - may be extended members of the MDT ie attend 4 MDT meetings per year, but need not be core members of the MDT. 12 Clinical Trials Participation in clinical trials is encouraged, especially those which are part of the national Cancer Research network portfolio. In some instances the trial protocol will require diagnosis; treatment or follow-up which is at odds with these clinical guidelines. This should not be a concern where the trial has been through the appropriate ethical approval. Appendix 1- Primary care referral guidelines for skin cancer Premalignant lesions Includes actinic keratoses, Bowens disease (SCC in situ) High Risk BCC High risk of incomplete excision and recurrence, defined as: recurrent BCCs BCCs on the head (face and scalp) large BCCs > 2cm diameter (unless they are superficial BCCs see below) lesions that have a clinical appearance of morphoeic, infiltrative or basosquamous lesions with poorly defined margins BCCs in patients who are immunosuppressed or have Gorlin‟s syndrome BCCs located over important underlying anatomical structures (for example, major vessels or nerves) or where primary surgical closure may be difficult (for example, digits or front of shin). Extended Low Risk BCC There is no diagnostic uncertainty that the lesion is a primary nodular low-risk BCC and it meets the following criteria: The patient with BCC is not: aged 24 years or younger (that is, a child or young adult) immunosuppressed or has Gorlin‟s syndrom e The lesion: Is not on the nose and lips (including nasofacial sulci and nasolabial folds), or around the eyes (periorbital) or ears Is less than 2 cm in diameter if below the clavicle (unless they are superficial BCCs see below). Is less than 1 cm in diameter if above the clavicle (unless they are superficial BCCs see below). Is not morphoeic, infiltrative or basosquamous in appearance Does not have poorly defined margins Is not located: o over important underlying anatomical structures (for example, major vessels or nerves) o in an area where primary surgical May be treated by any GP in the community Refer to core member of Local MDT Suspected BCCs should usually be referred as routine. Consider 2 week referral if there is particular concern that delay may have an impact because of site or size of lesion. Refer to either Core member of local MDT Or Group 3 GPwSI in dermatology and skin surgery Or Group 3a GPwSI in skin lesions and skin surgery Suspected BCCs should usually be referred as routine. Consider 2 week referral if there is particular concern that delay may have an impact because of site or size of lesion. o closure may be difficult (for example, digits or front of shin) in an area where excision may lead to a poor cosmetic result. If any of the above exclusion criteria apply, or there is any diagnostic doubt, the patient should be referred to the LSMDT. Incompletely excised BCCs should be discussed with a member of LSMDT Low Risk BCC There is no diagnostic uncertainty that the lesion is a primary nodular low-risk BCC and it meets the following criteria: The patient with BCC is not: aged 24 years or younger (that is, a child or young adult) immunosuppressed or has Gorlin‟s syndrom e The lesion: is located below the clavicle (that is, not on the head or neck) is less than 1 cm in diameter with clearly defined margins is not a recurrent BCC following incomplete excision is not a persistent BCC that has been incompletely excised according to histology is not morphoeic, infiltrative or basosquamous in appearance is not located o over important underlying anatomical structures (for example, major vessels or nerves) o in an area where primary surgical closure may be difficult (for example, digits or front of shin) o in an area where difficult excision may lead to a poor cosmetic result o at another highly visible anatomical site (for example, anterior chest or shoulders) where a good cosmetic result is important to the patient. Refer to either Core member of local MDT Or Group 3 GPwSI in dermatology and skin surgery Or Group 3a GPwSI in skin lesions and skin surgery Or GP accredited in Skin Cancer Suspected BCCs should usually be referred as routine. Consider 2 week referral if there is particular concern that delay may have an impact because of site or size of lesion. Incompletely excised BCCs should be discussed with a member of the LSMDT. BCC where there is any doubt about high or low risk status Refer to core member of Local MDT Superficial BCCs – on the face Refer to core member of Local MDT Superficial BCCs – not on the face If the lesion is thought to be a superficial BCC the GP should ensure that the patient is offered the full range of medical treatments, including photodynamic therapy. This may require referral to the LSMDT. Refer to either Core member of local MDT Or Group 3 GPwSI in dermatology and skin surgery Or Group 3a GPwSI in skin lesions and skin surgery Or GP accredited in Skin Cancer Suspected BCCs should usually be referred as routine. Consider 2 week referral if there is particular concern that delay may have an impact because of site or size of lesion. Squamous Cell Carcinoma Keratoacanthoma Melanoma 2 Week Referral to core member of Local MDT 2 Week Referral to core member of Local MDT 2 Week Referral to core member of Local MDT It is recognised that some skin cancers will be excised accidentally by GPs where the diagnosis was not apparent. These guidelines assume that GPs will not knowingly treat patients beyond their remit. See Section 9 for the Governance of skin cancer services in the community. 11-1C-110j Agreed network primary care referral guidelines and their distribution 11-6A-101j Network/PCT agreed primary care referral policy and distribution of the primary care referral guidelines Appendix 2 - Referral guidelines between Local and Specialist MDTs Local MDT Plymouth Hospital North Devon Hospital Royal Devon and Exeter Hospital South Devon Hospital Royal Cornwall Hospital Specialist MDT Plymouth Hospital Royal Devon and Exeter Hospital Royal Cornwall Hospital Patients requiring care level 5 and above should be referred from the Local to the Specialist MDT, including: Metastatic SCC Radiotherapy Other adjuvant therapy Mohs‟ surgery Selected SCCs and BCCs Skin lymphoma Sarcoma Other rare tumours Patients with genetic syndromes including Gorlin‟s (these patients may be reviewed regularly by the LSMDT team, with input as necessary from the SSMDT). Malignant melanomas stage 11b or above All malignant melanomas for patients under 19yrs (whose management plan need to be agreed with the principal Treatment Centre for Children‟s Cancer in Bristol) Metastatic Malignant melanomas See Section 5 for referral guidance for Skin Lymphomas See Section 6 fore referral for Kaposi‟s sarcoma and other rare skin cancers 11-1A-207j Network agreed referral guidelines between teams Appendix 3 - Extract from the South East London Cancer Network Constitution for Skin Cancer 9. T-Cell Lymphoma MDT Supra Network for Total Surface Electron Beam Therapy (TSBET). See also supporting document TSEB Guidelines May 2009 The St John‟s Institute of Dermatology, Guys‟ and St Thomas‟ NHS Foundation Trust will provide supra Network specialist services and the supra Network MDTs for SE London and wider populations to be determined in conjunction with the Specialist Commissioning Group. St John‟s operates as a supraregional centre for skin cancers and in the three years to 2006 received more than 600 referrals for primary cutaneous T-cell and B-cell lymphoma, of which three quarters came from outside SE London. It will continue to offer supra regional services for skin cancers referred from across the country Patient Pathway Joint Skin Tumour Unit Out Patients St Johns Institute, St Thomas‟ Hospital Consultant Clinical Oncologist makes decision to offer TSEBT Patient Consent and Information given Patient Planning Appointment Patient Treatment Patient Follow up 2 weeks prior to start date Boost treatment Positions planned Shielding planned Patch treatment planned Radiotherapy Prescribed Weekly medical review Daily radiographer review See in Clinical Oncology Outpatients at weeks 1-3 if toxicity and ongoing care needed ST Johns joint Clinic 1 month post Audit and Outcome Monitoring 10. Referral for Photopheresis See also supporting document TSEB Guidelines May 2009. There is a photopheresis facility available at St John‟s Institute of Dermatology, Guy‟s & St Thomas Hospital. Cutaneous tumour Stage T3 N0-1 M0 (IIB) Complete responses with TSEBT are lower with stage T3 tumours in the region 36 – 54% 4,6,12. This is however much superior to skin directed superficial radiotherapy and topical Nitrogen Mustard which has complete response rates of 8%. Therefore patients with stage IIB disease are offered TSEBT as first line treatment for its superior response rate and rapid palliative effect. It is combined with adjuvant treatment such as PUVA which improves the 5 year relapse free survival from 30% with TSEBT alone to 55% with TSEBT and adjuvant PUVA. Erythroderma stage T4N0-1M0 (III) TSEBT can produce rapid and sustained responses in erthrodermic MF ameleriorating the severe cutaneous symptoms experienced by such patients. The reported complete response to TSEBT for stage III MF ranges from 60-100% with 5 year progression free survival of 69%. The complete response rate and progression free survival is less in patients with blood or visceral involvement. These patients may benefit from adjuvant photophoresis. TSEBT is an appropriate first line therapy for these patients. We currently use it as second line therapy following treatment with PUVA, A-interferon, photopheresis or methotrexate. Appendix 4 - Levels of Care Care Leve l 1 2 3 4 5 Case mix or Procedures Benign lesions Actinic Keratoses Precancerous – SCC, in situ/Bowen‟s Low risk BCC – defined as not high risk (see Level 3) High risk BCC other than categories below High Risk BCC - defined as recurrent BCCs BCCs on the head (face and scalp) large BCCs > 2cm diameter unless they are superficial BCCs that can be managed non-surgically lesions that have a clinical appearance of morphoeic, infiltrative or basosquamous lesions with poorly defined margins BCCs in patients who are immunosuppressed or have Gorlin‟s syndrome BCCs located over important underlying anatomical structures (for example, major vessels or nerves) or where primary surgical closure may be difficult (for example, digits or front of shin). SCC other than categories below High risk BCC Recurrent or with +ve excision SCC Recurrent or with +ve excision Malignant Melanoma (MM) – new, single primary, adult, non-metastatic, not for approved trial entry, up to and including stage II a (must fulfil all these criteria) Radiotherapy if attendance by clinical oncologist at LSMDT Lesion where diagnosis is uncertain but may be malignant Incompatible clinical and histological findings Selected BCCs and SCCs needing plastic/reconstructive surgery by SSMDT core member (as per Network clinical guidelines) • Radiotherapy (as per Network clinical guidelines). If not discussed and treated by LSMDT clinical oncology core team member Metastatic SCC on presentation or newly metastatic MM – stage IIb or more, or < 19 years or metastatic on presentation or newly metastatic or recurrent or for approved trial entry Any cases for approved trial entry Any cases for adjuvant therapy (as per Network clinical guidelines) Histology opinion from SSMDT core pathology team member Mohs surgery Skin Cancer in immunocompromised patients including organ transplant recipients Skin Cancer in genetically predisposed patients including Gorlin‟s Syndrome. Cases to be dealt with by only one agreed SSMDT per Network, if more than one in the Network: Cutaneous lymphoma Kaposi‟s sarcoma Cutaneous sarcoma above superficial fascia. (Below fascia, refer to sarcoma MDT) in cancers Other rare skin cancers (see appendix 1 in the Skin Cancer IOG pg 128/129. Notes: 6 Where a network chooses to have a MMDT all cases of MM for level 5 care from the MMDT’s catchment area should be referred to the MMDT. There should be agreed working arrangements with certain site specialised MDT’s (see topic 08-1A). T-cell Cutaneous Lymphoma: Total Body Surface Electron Beam Therapy Appendix 5 – Peninsula Cancer Network Urology Site Specific Group Penile Cancer Guidelines 2009 The NSSG has adopted the Guidelines of the Avon, Somerset and Wiltshire Network as the Supra Network for penile cancer. These local guidelines are designed to explain the presentation and assessment which will be carried out within the PCN before referral to the penile cancer team, as well as the treatments which may be conducted locally after discussion at the Supra Network MDT meeting. They are not intended to be exhaustive list of different presentations, findings and assessments that apply to every single patient. PRIMARY CARE SETTING Presentation will usually be with an ulceration or mass on the penis. The presence of phimosis may make assessment difficult. Patients should be referred under the 2 week wait system if there is suspicion of cancer. SECONDARY CARE SETTING Patients will be assessed clinically at the out-patient department, specifically penile examination and assessment of inguinal lymph nodes. Biopsy of suspicious penile lesions may be carried out by the local team, and also aspiration cytology of any suspicious inguinal lymph nodes. Following histological confirmation, CT or MR scanning of the thorax, abdomen and pelvis is performed for further staging and referral made directly to Mr D Dickerson, Southmead Hospital for discussion at the Supranetwork MDT meeting, with a view to seeing the patient to discuss further management. In some unfit patients referral may be made back to the local hospital for simple partial penectomy. More complex surgery will either be performed by the core penile team at Southmead Hospital, or by Mr J Palmer, Plastic Surgeon, Royal Devon and Exeter Hospital, or Mr R Pearcy, Derriford Hospital, who are members of the extended penile cancer team. Discussion of further staging, surgery or adjuvant treatment is detailed in the ASW supranetwork guidelines, and under their direction. Follow-up may be delegated back to the local team after an appropriate period, as decided by the core team Appendix 6 - Excision of Skin Cancer in the Community Outside of the Guidelines In response to NICE Guidance, the Peninsula Cancer Network has agreed guidelines on the management of skin cancer in the community. [PCT Name] is committed to ensuring all services are carried out in accordance with this guidance, in collaboration with the Skin Cancer Multidisciplinary Team at [hospital name]. NHS [xxx] will be using information from the local Skin Cancer Multidisciplinary Team (MDT) Departments to review adherence to this guidance. A Skin Cancers that SHOULD NOT be managed in primary care GPs, including GPwSIs, should not knowingly treat the following skin cancers Malignant melanoma Squamous cell carcinoma High risk basal cell carcinoma (BCC) The following definition of high-risk BCC should be used for clinical triage in primary care: recurrent BCCs BCCs on the nose and lips (including nasofacial sulci and nasolabial folds), or around the eyes (periorbital) or ears BCCs greater that 2 cm in diameter if below the clavicle (unless they are superficial BCCs that can be managed non-surgically). BCCs greater that 1 cm in diameter if above the clavicle (unless they are superficial BCCs that can be managed non-surgically). lesions that have a clinical appearance of morphoeic, infiltrative or basosquamous lesions with poorly defined margins BCCs in patients who are immunosuppressed or have Gorlin‟s syndrome BCCs located over important underlying anatomical structures (for example, major vessels or nerves) in an area where primary surgical closure may be difficult (for example, digits or front of shin) in an area where excision may lead to a poor cosmetic result. Patients where there is diagnostic uncertainty Patients aged 24 years or younger BCCs that have been incompletely excised according to histology Superficial BCCs on the face B Skin Cancers that MAY be managed by an accredited GPwSI Extended Low Risk BCC There is no diagnostic uncertainty that the lesion is a primary nodular low-risk BCC or superficial BCC and it meets the following criteria: The patient with BCC is not: aged 24 years or younger (that is, a child or young adult) immunosuppressed or has Gorlin‟s syndrome The lesion: Is not on the nose and lips (including nasofacial sulci and nasolabial folds), or around the eyes (periorbital) or ears Is less than 2 cm in diameter if below the clavicle (unless they are superficial BCCs that can be managed non-surgically). Is less than 1 cm in diameter if above the clavicle (unless they are superficial BCCs that can be managed non-surgically). Is not morphoeic, infiltrative or basosquamous in appearance Does not have poorly defined margins Is not located: o over important underlying anatomical structures (for example, major vessels or nerves) o in an area where primary surgical closure may be difficult (for example, digits or front of shin) o in an area where excision may lead to a poor cosmetic result. Incompletely excised BCCs should be discussed with a member of Skin Cancer MDT C Skin Cancers that MAY be managed by an accredited GP primary care Low Risk BCC The patient with BCC is not: aged 24 years or younger (that is, a child or young adult) immunosuppressed or has Gorlin‟s syndrome The lesion: is located below the clavicle (that is, not on the head or neck) is less than 1 cm in diameter with clearly defined margins is not a recurrent BCC following incomplete excision is not a persistent BCC that has been incompletely excised according to histology is not morphoeic, infiltrative or basosquamous in appearance is not located o over important underlying anatomical structures (for example, major vessels or nerves) o in an area where primary surgical closure may be difficult (for example, digits or front of shin) o in an area where difficult excision may lead to a poor cosmetic result o at another highly visible anatomical site (for example, anterior chest or shoulders) where a good cosmetic result is important to the patient. Incompletely excised BCCs should be discussed with a member of the LSMDT. D Superficial Basal Cell Carcinomas Patients with superficial BCCs (not usually classified as high risk) should be appropriately referred in order that they can be offered a full range of medical treatments, including photodynamic therapy. This may require referral to the Skin Cancer Multidisciplinary Team. Healthcare professionals managing superficial BCC in the community should have experience and knowledge of this condition. All superficial BCCs on the face should be referred to the Skin Cancer MDT. Histological Specimens ALL skin specimens removed should be sent to histology for analysis. GPs should provide information about the site of excision and provisional diagnosis on the histology request form. 4 2. Topical and ablative therapies (ie cryotherapy) should only be used if the diagnosis is certain. 1.