cntctfrm_4b6e2c962bc750795e761f0dec0e3795_REVIEW
advertisement
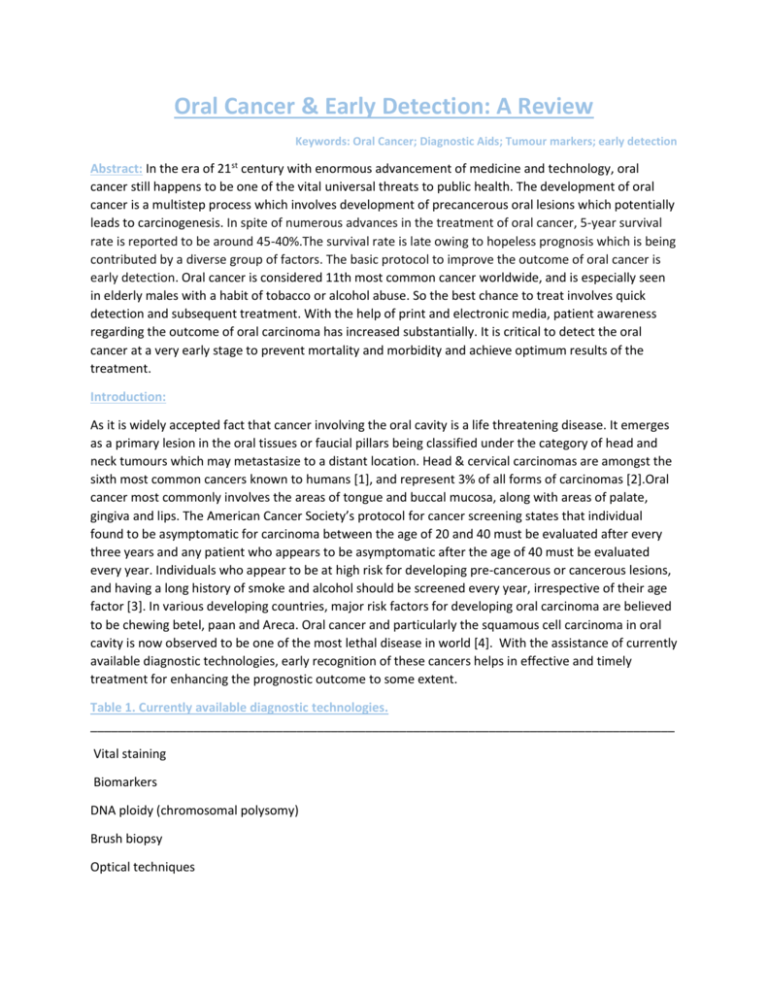
Oral Cancer & Early Detection: A Review Keywords: Oral Cancer; Diagnostic Aids; Tumour markers; early detection Abstract: In the era of 21st century with enormous advancement of medicine and technology, oral cancer still happens to be one of the vital universal threats to public health. The development of oral cancer is a multistep process which involves development of precancerous oral lesions which potentially leads to carcinogenesis. In spite of numerous advances in the treatment of oral cancer, 5-year survival rate is reported to be around 45-40%.The survival rate is late owing to hopeless prognosis which is being contributed by a diverse group of factors. The basic protocol to improve the outcome of oral cancer is early detection. Oral cancer is considered 11th most common cancer worldwide, and is especially seen in elderly males with a habit of tobacco or alcohol abuse. So the best chance to treat involves quick detection and subsequent treatment. With the help of print and electronic media, patient awareness regarding the outcome of oral carcinoma has increased substantially. It is critical to detect the oral cancer at a very early stage to prevent mortality and morbidity and achieve optimum results of the treatment. Introduction: As it is widely accepted fact that cancer involving the oral cavity is a life threatening disease. It emerges as a primary lesion in the oral tissues or faucial pillars being classified under the category of head and neck tumours which may metastasize to a distant location. Head & cervical carcinomas are amongst the sixth most common cancers known to humans [1], and represent 3% of all forms of carcinomas [2].Oral cancer most commonly involves the areas of tongue and buccal mucosa, along with areas of palate, gingiva and lips. The American Cancer Society’s protocol for cancer screening states that individual found to be asymptomatic for carcinoma between the age of 20 and 40 must be evaluated after every three years and any patient who appears to be asymptomatic after the age of 40 must be evaluated every year. Individuals who appear to be at high risk for developing pre-cancerous or cancerous lesions, and having a long history of smoke and alcohol should be screened every year, irrespective of their age factor [3]. In various developing countries, major risk factors for developing oral carcinoma are believed to be chewing betel, paan and Areca. Oral cancer and particularly the squamous cell carcinoma in oral cavity is now observed to be one of the most lethal disease in world [4]. With the assistance of currently available diagnostic technologies, early recognition of these cancers helps in effective and timely treatment for enhancing the prognostic outcome to some extent. Table 1. Currently available diagnostic technologies. _____________________________________________________________________________________ Vital staining Biomarkers DNA ploidy (chromosomal polysomy) Brush biopsy Optical techniques Saliva-based oral cancer diagnostics PCR-Based diagnostic aids _____________________________________________________________________________________ VITAL STAINING: For the early detection of carcinomas or any abnormality of the cervical region and the oral cavity, Toluidine blue which is also referred as Tolonuim chloride has been used extensively in the past. Toluidine Blue is a metachromatic dye which has a clear affinity for selectively staining various acidic tissues since it is acidophilic in nature. It stains structures like DNA and RNA, but will not have any form of affinity for the normal mucosa. A number of conducted studies have shown that use of vital staining has a high positive rate for the early detection of oral carcinomas. Warnakulasuriya and Johnson, in a study, stained the oral mucosa of patients which they found to be suspicious lesions on clinical examination. The study involved 102 patients and out of that about 18 number of patients proved to have oral carcinomas and all malignant lesions stained with toluidine blue. Results showed a sensitivity of 100% for detection of oral cancer by vital staining. However, the overall specificity was low at 0.62. [5] Toluidine blue, on the basis of study by Warnakulasuriya and Johnson is believed to be excellent at early oral carcinoma detection but it was observed that toluidine blue is positive in only about half of the lesions with dysplasia. Also, it also frequently stains non-specific ulcers. Following a study of Martin et al. [6], he studied a number of specimens and subjects. The purpose of the study was to establish the absorption of stain to areas of carcinoma or dysplasia. The result showed to be positive for all location of carcinomas, but only 42% were positive for dysplasia. Lugol’s solution is utilized for portrayal of the malignancy detected which is seen to fabricate a brown and dark black stain when the iodine recoils with the glycogen. So toluidine blue and Lugol’s iodine can prove to be excellent diagnostic tools which can be assisted in patients who are suspected to have malignancy in order to choose the most appropriate site for biopsy. TUMOUR MARKERS: Tumor markers are biochemical substances produced by tumor cells due to response to malignant process produced by host to differentiate a tumor from normal tissue and also to determine the occurrence of a tumor by the judging the measurements [8] The human body, in response to cancerous content, will release tumour markers which may be detected in cell cytoplasm, plasma membrane and blood or any body fluids.. If a patient has been detected with oral squamous cell carcinoma, the most important prognostic tools will include angiogenic markers, tumour Suppressor genes and oncogenes along with cell proliferation and cell adhesion molecules. Oral Squamous cell carcinoma can be detected by the use of cytokeratin markers which help to analyze the alteration in keratin expression. [9] DNA PLOIDY: DNA ploidy can be described as the quantification of DNA proportion that provides a thorough assessment of genetic mutilation. The chromosomal segregation is deranged if the chromosomes are not systematically distributed to the daughter cells during cell division or if some parts of chromosomes become disengaged which is a very usual characteristic of carcinoma. Cancer development and progress is granted by some form of genetic instability, and dysplastic lesions are differentiated by abnormal DNA [10]. The cytological smears are stained with the help of the Feulgen dye and contrasted against a reference cluster of cells. Technology of monitor based analysis helps in identifying the anomalies of cellular DNA. DNA image cytometry is a very useful non-invasive method for cancer detection. [11] BRUSH BIOPSY: The Brush Biopsy (CDx Laboratories) was developed way back in 1999 with an objective of early carcinoma detection. It studied those lesions that would not be opted to undergo a biological examination because carcinoma was not suspected Few studies have shown promising achievements with oral brush biopsy for evaluation of cancerous cells. Detailed work by Scuibba et al. [12] established the sensitivity of brush biopsy (OralCDx) for the early diagnosis of cancerous lesions of the oral cavity. He recorded the brush biopsy results were recorded as positive, or negative or atypical. He used OralCDx and surgical biopsy method for 298 patients with clinically suspicious lesions. The remaining 647 patients were only subjected to OralCDx testing. The results after the study showed sensitivity as well the specificity of 100% if positive test results were indicating cancer. The specificity was found to be 92.9% when atypical results were believed to be symbolic for carcinoma. OPTICAL TECHNIQUES: Tissue reflectance: For the detection of malignancies in cervical tissues, tissue reflectance (ViziLite Plus, MicroLux DL) has been adapted for use as a diagnostic equipment. In recent past, tissue reflectancebased examination has been used for detection of malignancies in the oral cavity sold under the brands ViziLite and MicroLux. The main objectives of such devices and materials is to increase the chances of early detection of any form of abnormality in the oral. According to the method indicated, patient is instructed to rinse the mouth with a 1% acetic acid solution. Later on there is a visual study of the oral cavity with the help of blue light. ViziLite Plus has the facility of a disposable light packet and on the other hand MicroLux has been subjected to reusable source. The basic reason behind asking the patient to rinse with 1% acetic acid is to free the oral cavity of any form of debris and potentially increase the clarity of cells. With the study of blue illumination, it has been found that the normal epithelium would have the appearance of light blue color as opposed to abnormal epithelium which will appear white. ViziLite has the provision of tolonium chloride solution, which helps to mark the lesion for biopsy. ViziLite has also been used to examine a variety of oral lesions, which includes leukoedema, ulcer, and frictional keratosis etc. [13] Narrow-emission tissue fluorescence (VELscope): Fluorescence spectroscopy is a modern day technology which exposes tissues to numerous wavelengths in order to detect the differences present between a normal oral tissue and abnormal tissues. In complete contrast, fluorescence imaging involves exposing tissues to a very particular wavelength of light, ultimately leading to autofluorescence of fluorophores following their excitation. It has been mentioned that existence of cellular variations will result into a revision of the concentrations of fluorophores, which subsequently influences the smattering and absorption of light, which will result into changes in shades. The appropriate usage of VELscope is a simple procedure and a complete check-up can be completed in nearly 2 minutes. However, it is a relatively new device and so far only a limited number of studies have been done on its effectiveness as a diagnostic adjunct for oral cancer [14]. Using this device, Lane et al., described the potential of the technique to diagnose oral cancer at an early stage. The subtle study had an approximate number of 44 subjects with a history of either dysplasia or anaplasia. Later on, there was a screening of oral cavity with the help of VELSCOPE for detection of areas which happened to show dropping of autofluorescence. The biopsy specimen of the tissues were included. With the help of histology as a basic, VELSCOPE depicted sensitivity of 98% and a 100% specificity which helped to differentiate the oral dysplasia and oral cancers from normal tissue. [15] In Vivo Confocal Microscopy: Confocal microscopy is a major imaging technology used for various researches in cellular study. It has the huge advantage of optical fragmenting and appreciative optical resolution. This technique of microscopical study provides images which can effectively demonstrate the characteristic attributes such as nuclear irregularity which can be used detect cancer. However, a lot of improvements is still needed for in vivo confocal microscopy to be rated as a favorable non-invasive tool. SALIVA-BASED ORAL CANCER DIAGNOSTICS: Saliva has been used as a very efficient diagnostic tool for oral cancer detection and its use meets the demands of relatively cheaper and non-invasive diagnostic tool. Saliva, as a diagnostic tool, has a variety of advantages which includes • Non-invasive • Highly Economical • Can be used for mass screening DNA transcripts, metalloproteinase, cytokines, mRNAs and other enzymes and growth factors along with endothelin, and cytokeratins can be measured by the study of saliva [16]. CA125, Cyfra 21-1, (CEA) and SCC, are very commonly studied in saliva of the patients suffering from carcinoma. PCR-BASED DIAGNOSTIC AIDS: The polymerase chain reaction (PCR) is a widely used medical technique in molecular biomechanics in the detection of malignancies associated with head and neck regions. PCR assists in the understanding the nature of cancer and impart deep meaningful understanding of the pathogenesis of carcinoma. PCR is being currently used in detection of mutations in oncogenes and tumor suppressor and aids as an important detection tool [17]. PCR also helps in the detection of amplified C-myc proto-oncogene. CONCLUSION: Potential malignancies constitute an important danger to the life of an individual. Along with dentists and oral surgeons, all health professionals constitute a very important role in quick detection and treatment of cancer, thus tackling the cancerous lesions and enhancing the overall prognosis. Even though there has been an exponential rise in the development of extensive oral cancer screening techniques in last couple of decades, still many researchers are working for more efficient and faster aids of diagnosing the oral cancer. References: 1. Williams HK. Molecular pathogenesis of oral squamous carcinoma. Mol Pathology 2000; 53(4):165-72. 2. Jemal A, Siegel R, Ward E, Hao Y, Xu J, Thun MJ. Cancer statistics. Ca-Cancer J Clin 2009; 59(4):225-49 3. American Cancer Society, California Division and Public Health Institute, California Cancer Registry 4. Binnie WH, Rankin KV (1984). Epidemiological and diagnostic aspects of oral squamous cell carcinoma. J Oral Pathology, 13, 333-41. 5. Warnakulasuriya KA, Johnson NW. Sensitivity and specificity of OraScan (R) in the detection of oral cancer and precancer. Journal Oral Pathology Med 1996; 25(3):97–103 6. Martin IC, Kerawala CJ, Reed M. Application of toluidine blue in the detection of epithelial dysplasia. Oral Surgery Oral Med Oral Path Oral Radio Endodontics 1998; 85(4):444–6 7. Sujata Satoskar, Ajit Dinakar (2006). Diagnostic aids in early oral cancer detection- a review. J Indian Academy of Oral Med & Radiology, 18, 82-9 8. Nayak AG Tumour Markers: An Overview; Indian Academy of Oral Medicine and Radiology 2010 July 147-150 9. Vaidya MM, Borges AM, Pradhan SA, Rajpal RM, Bhisey AN (1989). Altered keratin expression in buccal mucosal squamous cell carcinoma. Journal Oral Pathology Med, 18, 282-6. 10. Bradley G, Odell EW, Raphael S, Ho J, Le LW, Benchimol S, et al. Abnormal DNA content in oral epithelial dysplasia is associated with increased risk of progression to carcinoma. Br J Cancer 2010; 103(9):1432-42 11. Crispian Scully, José Bagan V, Colin Hopper, Joel Epstein B (2008). Oral cancer: Current and future diagnostic techniques. Am J Dentistry, 21, 199-209 12. Scuibba JJ. Improving detection of precancerous and cancerous oral lesions. Computer-assisted analysis of the oral brush biopsy. US Collaborative OralCDx Study Group. J Am Dent Association 1999;130 (10):1445–57. 13. Huber MA, Bsoul SA, Terezhalmy GT. Acetic acid wash and chemiluminescent illumination as an adjunct to conventional oral soft tissue examination for the detection of dysplasia: a pilot study. Quintessence Int 2004; 35(5):378–84 14. Yi-Shing Lisa Cheng, John Wright (2011). Advances in Diagnostic Adjuncts for Oral Squamous Cell Carcinoma. The Open Pathology J, 5, 3-7. 15. Lane PM, Gilhuly T, Whitehead P, Zeng H, Poh CF, Ng S, et al. Simple device for the direct visualization of oral-cavity tissue fluorescence. J Biomed Opt 2006; 11(2):024006 16. Nagler RM. Saliva as a tool for oral cancer diagnosis and prognosis. Oral Oncol 2009; 45:1006-10 17. Richard Jordan CK., Troy Daniels E, John Greenspan S, Joseph Regezi A (2001). Advanced diagnostic methods in oral and maxillofacial pathology., 92, 650-69