Week 6 case study
advertisement

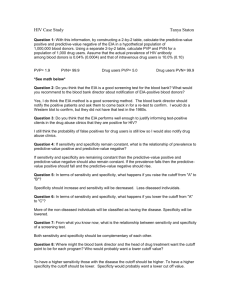
Abigail Smith Week 6 Case Study Question 1: With this information, by constructing a 2-by-2 table, calculate the predictive-value positive and predictive-value negative of the EIA in a hypothetical population of 1,000,000 blood donors. Using a separate 2-by-2 table, calculate PVP and PVN for a population of 1,000 drug users. Assume that the actual prevalence of HIV antibody among blood donors is 0.04% (0.0004) and that of intravenous drug users is 10.0% (0.10). PVP = 400/20392 = .0196 or 1.96% PVN = 979587/979608 = .999 or 99.9% PVP = 100/118 = .847 or 84.7% PVN = 877/882 = .994 or 99.4% Question 2: Do you think that the EIA is a good screening test for the blood bank? What would you recommend to the blood bank director about notification of EIA-positive blood donors? I think the EIA is a good screening test with a high sensitivity and specificity that will help identify those individuals who carry the antibody. I would recommend stating that there can be false positives and to get tested to be sure you actually possess the antibody. It will be crucial to let those who test positive know that the test can sometimes be wrong, but in order to protect those who are receiving the blood, you can not accept their donation until further testing is completed. Question 3: Do you think that the EIA performs well enough to justify informing test-positive clients in the drug abuse clinics that they are positive for HIV? I do think the EIA performs well enough to use it to inform test-positive clients in drug abuse clinics. Question 4: If sensitivity and specificity remain constant, what is the relationship of prevalence to predictive-value positive and predictive-value negative? If sensitivity and specificity remain constant, when the prevalence of the antibody falls so will the predictive value positive and the predictive value negative will rise. Having a low PVP means that any individual who has a positive screening test would have a low probability of having the disease. Question 5: In terms of sensitivity and specificity, what happens if you raise the cutoff from "A" to "B"? A cut point of "A" maximizes both sensitivity and specificity while a cut point of "B" will cause an increase in specificity at the expense of sensitivity. Question 6: In terms of sensitivity and specificity, what happens if you lower the cutoff from "A" to "C"? Moving the cut point to "C" causes sensitivity to approach 100% and specificity will be lowered because more of the nondiseased individuals will be classified as diseased. Question 7: From what you know now, what is the relationship between sensitivity and specificity of a screening test. The relationship between sensitivity and specificity is a directly proportional one, as sensitivity increases, specificity will decrease. Question 8: Where might the blood bank director and the head of drug treatment want the cutoff point to be for each program? Who would probably want a lower cutoff value? The director of the blood bank would want the cut off at "A" to ensure no person with the antibody donates blood. The drug treatment program would want a cutoff at "B" to ensure no false positives get mixed into the results. Those who are receivung the blood transfusions would want a lower cutoff to ensure they will not be given infected blood. Question 9: What is the actual antibody prevalence in the population of persons whose blood samples will undergo a second test? 400/20392 = .0196 or 1.96% Question 10: Calculate the predictive-value positive of the two sequences of tests: EIA-EIA and EIA-Western blot. Assume that the sensitivity and specificity of the EIA are 95.0% and 98.0%, respectively. Assume that the sensitivity and specificity of the Western blot are 80.0% and 99.99%, respectively. Also assume that the tests are independent, even though they may not be (e.g., those with cross-reactive proteins are likely to cross-react each time). EIA-EIA: PVP - 400/800 = .5 or 50% EIA-Western blot: PVP - 400/402 = .995 or 99.5% Question 11: Why does the predictive-value positive increase so dramatically with the addition of a second test? Why is the predictive value positive higher for the EIA-WB sequence than for the EIA-EIA sequence? The second test helps to confirm what was discovered in the first test. The second test helps to weed out the false positives causing the actual positives to be discoverd and raising the predictive value positive dramatically. Since the Western blot has such a high specificity it has the ability to identify the true negatives more accurately than the EIA is able to identify. Question 12: What criteria would you consider in evaluating this proposed screening program? The cost of the program needs to be evaluated along with where funding will come from for the program. Also, the populations wilingness to participate in the blood test will have to be evaluated. What also needs to be considered are the number of people who have never engaged in sexual activity or intravenous drug use, therefore not having the ability to contract the disease and those who have used protection every time, also not having much of an ability to have contracted the disease. The benefits need to far outweigh the cost for the program to be implemented. Question 13: Compute the cost of the screening program. Assume a cost of $50.00 for every initial EIA test ($10.00 lab fee and $40.00 health-care-provider visit) and an additional $100.00 for EIA-positive persons who will need additional testing. What is the cost of the screening program in the next year? What is the cost per identified antibody-positive person? Cost of screening program in the next year: (50 X 60,000) + (100 X 143) = $3,014,300 Cost per identified antibody-positive person: 3,014,300/22 = $137,013.64 Question 14: What is your final recommendation to the Governor? My recommendation would be that the cost of the program is much too high for the benefits it will ultimately provide. My hopes would be that those individuals who have participated in high risk behavior will get tested on their own and be truthful with their partner. This will dramatically cut down on the cost since not all 60,000 people who are getting married need to be tested.