Total Hip Replacement information for patients
advertisement

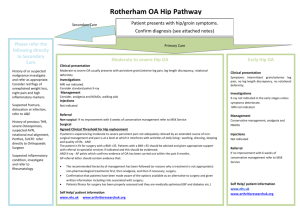
Total Hip Replacement Information for patients Understanding arthritis and hip replacement Patient Name_________________________Hospital Number________________ Consultant______________________ Please keep this booklet and bring it with you to all your appointments, your inpatient stay and your follow up appointment. The blank pages are provided for you to write your own notes Important Dates Pre Assessment Clinic ______________________________ Notes Operation Date_____________________________________ Admission Time____________________________________ Notes Expected discharge Date______________________________ 6-10 week Follow up Appointment______________________ Notes 1 Year Assessment___________________________________ 2 The Hip Joint The Hip Joint The hip joint is a ball and socket joint. The ball is on the top of the thigh bone (femur) and the socket is at the lower part of the pelvic bone and faces sideways. The ends of the bones are covered by a smooth lining known as articular cartilage and the surfaces glide on each over with the help of a natural lubricating fluid, called synovial fluid. The synovial fluid is produced by one of the soft tissues around the hip called the synovium. 3 Osteoarthritis Osteoarthritis Osteoarthritis, often referred to as OA, is the most common form of arthritis, and is the most common reason for joint replacement surgery. Osteoarthritis is a degenerative disease that destroys the joint articular cartilage, often leading to painful bone on bone contact. It can cause pain, stiffness, swelling and loss of motion in the joint, which may vary in duration and severity from person to person. Treatments such as the painkillers, physiotherapy exercise, support braces, and weight reduction can help control the symptoms of osteoarthritis for a time. When these treatments fail to provide adequate relief from pain, total hip replacement may be recommended. Your surgeon will assess your individual condition and prescribe a treatment that will give you the best results. Rheumatoid Rheumatoid arthritis Arthritis Rheumatoid arthritis is an autoimmune deficiency syndrome, meaning the body’s immune system attacks and destroys healthy joint articular cartilage. Rheumatoid arthritis can occur at any age, even in children, and it is considered a systemic disease that affects multiple organs. In the joints, rheumatoid arthritis causes inflammation of the lining tissue, the synovium. Inflammation can cause pain, stiffness, swelling, warmth and redness, and can eventually lead to cartilage loss. Rheumatoid arthritis often affects many joints such as the hips, knees, and hands. This disease can have periods of flare-ups followed by a quick remission of symptoms. Rheumatoid arthritis is a chronic condition that may last a lifetime. However, treatment is available to help reduce pain and swelling, and slow joint destruction. 4 Total Hip Replacement Total Hip Replacement When performing a total hip replacement, the surgeon removes the damaged ball part of the hip and the damaged lining of the socket. The socket is prepared to receive a plastic material to provide a new lining. The ball part of the hip is replaced with a new metal ball which is applied to the top of a metal stem, which is implanted down the shaft of the thigh bone. Usually, the new socket lining and the stem in the thigh bone are cemented into place. Sometimes the surgeon may choose not to use cement and if so obtains fixation of the new hip components directly to the bone. In this situation the components have a titanium lining that the bone will grow onto and lock the components to the bone over the first 4 to six weeks. In some patients the ball and lining to the socket are made from ceramic material if the surgeon feels that this is the best option for the patient. The components that are implanted into the pelvis and thigh bone are designed to closely imitate the mobility of the natural hip joint. The operation takes about one and a half hours to do and you should be able to leave hospital from 2 days after surgery depending on your progress and individual circumstances. Xray of a pelvis showing one hip replaced. 5 Preparing for Surgery surgery Preparing for We aim to see and treat all patients within 18 weeks from referral from the GP, however there will be exceptions depending on any other investigations and treatments which may be required. During this time you will attend several appointments. You will meet one of the orthopaedic surgeons and have xrays to decide that you really do need a hip replacement. You will also need to attend a pre-assessment clinic to make sure that you are fit enough to have the surgery. During this visit you will attend a pre-operative education class during which you will be told a lot more about the operation. You will also have to undergo further tests, depending on your specific problems to ascertain your suitability for surgery. Some patients may need review by an anaesthetist at this stage, depending on your medical history. At this appointment, you may be asked to sign a consent form and the complications associated with surgery will be explained to you before you give your consent. This form is very important and you need to listen carefully to the information given to you. Sometimes this form is completed on the day you come into hospital. Physical Conditioning – It is important to be as fit as possible before undergoing joint replacement. Participating in a doctor-prescribed exercise program before surgery can help patients make a more rapid recovery. Moderate exercise is an integral part of treating arthritis. Activities such as walking, swimming, riding a bike or gardening can assist in keeping your bones strong and your joints supple, which may help relieve stiffness. Low-impact exercise will not wear out your joints. Although exercise may sometimes cause discomfort, proper exercise will help nourish the cartilage, strengthen the muscles, and prolong the life of your joints. Your hip may be so painful and stiff that exercise is not possible, in which case try to keep as active as you can. Having your muscles in good condition prior to surgery will help you in the recovery phase after the operation. 6 Nutrition Proper nutrition is a concern for joint replacement patients. Orthopaedic surgeons recognise that many joint replacement candidates may not be in peak nutritional health. Try to eat a well balanced diet; more information is available from Preoperative assessment clinic. Proper nutrition can assist in a Rapid Recovery by assisting in wound healing and energy levels A high intake of Vitamin C the day before your operation is recommended, fruit and vegetables are a good source of this. Stopping Smoking Before surgery it is absolutely essential to stop smoking. It is necessary to stop smoking at least two to four weeks before the planned procedure. Smoking impairs the transfer of oxygen to the healing tissues, which may increase healing time and the possibility of other complications. The hospital is a non-smoking site so you will not be able to smoke during your hospital stay. There are lots of national initiatives available to help you stop smoking. Patches may help you during your hospital stay. High Blood Pressure High blood pressure can result in your operation being postponed. If, at pre- operative assessment clinic or on admission to the ward, your blood pressure is high, you will be asked to go home and seek advice from your GP. This would obviously be a great disappointment to you and your family as it could delay your surgery until your blood pressure is better controlled. Feet Your feet are very important and need to be well looked after prior to joint surgery. You may have found difficulty in bending due to pain and have been unable to treat your feet, resulting in corns, in growing toe nails etc. If you have any of these problems then a chiropodist can help you. Getting problems sorted out before your admission will help you to regain your mobility quicker. It is probably best to talk to your GP or practice nurse about getting referred to a chiropodist. 7 Bone Donation The Bone Bank co-ordinator may see you in the Theatre Admissions Lounge on the day of surgery to ask if you would be willing to donate the piece of bone, femoral head (ball), removed during surgery. This can be stored and used for others. It requires your consent and a blood test to look for infections passed on by blood donation. This blood test is then repeated 6 months to a year later. You will not be able to donate your bone if you have: A Blood transfusion Hepatitis (Jaundice) Tuberculosis (TB) Cancer Syphilis Rheumatoid Arthritis Leukaemia Haemophilia Multiple Sclerosis Parkinsons Disease HIV/AIDS Long term steroid treatment Crohns disease/ulcerative colitis Pagets disease Perthes Disease If you require further information please ask for the ‘did you know you could become a bone donor leaflet’ or telephone 605312. 8 Healthy Skin For your operation to go ahead your skin needs to be healthy and free from sores or open areas. People who suffer from eczema, psoriasis, leg ulcers or any other skin conditions need to be extra careful. In the weeks leading up to your operation you must ensure that any open areas on your skin are healed and there is no infection present. For advice and treatment of any skin complaint you must consult your GP or practice nurse. There is a possibility that your operation could be cancelled if your skin is not healthy. A swab from your nose and possibly groin will be taken at pre-operative assessment clinic to ensure you are not carrying the bug Methicillin Resistant Staphylococcus Aureus (MRSA). If this swab is positive you will receive treatment through your GP and re-screening. You will not be able to have your operation until the swabs are negative. Urinary Problems This is a problem that nobody likes to talk about. Up to three million people in the UK suffer from stress incontinence (leaking when laughing or coughing). Incontinence can cause urinary infection and complications following surgery including wound infection. Getting help with this problem will reduce the risk of infection. A urine sample will be taken at pre- assessment. If positive, you will need antibiotic treatment before your operation. It may possibly delay your surgery date. If you are experiencing any symptoms of a urine infection it is a good idea to visit your GP before your preassessment date. Support on discharge You will need further assistance on discharge as you may not be able to manage some housework and fitting special compression stockings used to prevent thrombosis (see later). Please ensure that you have somebody to help you with these tasks on discharge for a temporary period of time. Please discuss your needs at Pre operative assessment clinic. 9 Home Environment You will be sent a furniture heights form with your appointment to attend pre assessment clinic. It is very important that you complete the form and bring it with you to your appointment. At this appointment a member of the Occupational Therapy team will discuss your heights form with you and agree on the necessary equipment needed to aid you in your post operative recovery and ensure you adhere to your hip precautions. You may need some of your furniture raised depending on your measurements. This will all be ordered and installed before your admission. A Checklist to help you prepare for admission: Ensure you have received all the equipment you are expecting before admission. If not please contact the occupational therapy department. Ensure care arrangements are in place for any dependents or pets you may have. Ensure you will be able to get out of bed on the side of your operation. Organise someone to be able to help you with your thrombo-embolic stockings. Reorganise your kitchen so that you can reach all essential items without bending. Perhaps plan for some ready prepared meals for when you first return home. Make sure your cupboards are well stocked before admission so that you don’t need to worry about shopping on discharge. Try talking to family, friends and neighbours about help with shopping and heavy household tasks. If you normally collect your medication, you may need to ask someone to do this for you initially or organise a delivery service. If you have any concerns about any of the things to do before your admission, please notify the occupational therapist (01793 646114) or a member of the team at your preadmission appointment. 10 In InHospital Hospital Before Surgery You will be admitted to the theatre admissions lounge (TAL). This is a dedicated area within the operating theatres where patients can be assessed and prepared for Orthopaedic surgery. Please bring all your medications into hospital with you. When you arrive the nurse will assess you, take a blood sample and prepare you for theatre. You will also be seen by the anaesthetist who will discuss the type of anaesthetic you are going to have for your operation. A nurse may visit you to discuss bone donation. The surgeon will see you and mark the leg that is to be operated upon. The surgeon will also check your consent formed is correct and signed. This will be completed if not already done at the pre-assessment clinic. Your belongings and medications will be taken up to the ward while you are in theatre. Please do not bring any valuables. The only items needed are sensible footwear, not new as your feet may be swollen, washing items, a set of day clothes which are easy to put on, and nightwear/dressing gown. You must also bring your current medications with you. A small amount of change may be needed for newspaper magazines during your stay. The Anaesthetic While you are in the Theatre Admissions Lounge The Anaesthetist will come to see you to talk about your anaesthetic. Generally the type of anaesthetic used for hip surgery is: Regional anaesthesia with light sedation. This is a spinal anaesthetic which is injected into your spine and makes you numb from the waist down. The advantage to this is that you are awake but sedated. There is a lesser risk of blood clots and chest infection and less sickness associated with this type of anaesthetic. But you may need a urinary catheter and will not be able to feel your legs for 4-6 hours after surgery. If you are unable to have a spinal anaesthetic then a general anaesthetic will be used. This may be supplemented with nerve blocks to numb your leg. The advantage of this is that you are unconscious during the surgery. This anaesthetic can make you quite 11 sleepy and nauseas after surgery. The nausea can be controlled with medication. The Anaesthetist will discuss with you which procedure is best for you. After Surgery You will be collected from the recovery unit by a nurse from the ward. You will be wheeled back up to the ward in your bed. You will have an Intravenous Infusion (IVI) in a needle in the back of your hand or arm when you return to the ward; this will continue for a short while until you are drinking. You may need a urinary catheter, but if it is required it will be removed as soon as possible after your surgery. There may also be drain coming out from your thigh to drain away any blood which might otherwise accumulate in the operation site. The anaesthetist will advise you before the operation as to the best method of pain relief for your operation. The nurses will be giving you regular painkillers. If these are ineffective then please ask the nursing staff to review the painkillers that you are receiving. Keeping your pain controlled enables you to start physiotherapy as soon as possible after your operation. The physiotherapists will come and help you to stand and maybe take a few steps as early as 2 hours after you return to the ward. If you are going to stand up on the day of your surgery the nurse looking after you may put some extra fluid into the intravenous drip in your arm just before you stand and you should eat something. It is important to start moving as soon as possible after surgery to encourage blood flow, to regain motion and to facilitate the recovery process. Early mobility also helps to prevent complications, see page 17. You will be out of bed and walking with walking aids very soon after your surgery, often on the day of the operation. A positive frame of mind is vital to your recovery and you will be encouraged to spend the day out of bed and in comfortable day clothes, returning to your night wear and bed only for sleeping. Although they will look after you and care for you, the hospital staff will encourage you to take responsibility for your recovery and you will be expected to become independent as you progress following your surgery. While you are in hospital your progress will be reviewed by medical staff. You may not see your consultant or the surgeon who carried out your operation but members of his or her team, which includes doctors and physicians assistants, will assess your recovery and make any changes to your drugs or treatment that is deemed necessary. 12 Any concerns about your recovery will be discussed with your consultant via the medical team. Discharge You can expect to stay in hospital for 2-4 days after your surgery, please be organised with transport home and put other domestic arrangements in place. The Occupational therapist will visit you on the ward before your discharge to discuss your individual home set up. The role of the Occupational Therapist is to assist you in your return to independence in activities of daily living, at the same time ensuring that you comply with your post op instructions. You will be given advice on what you can and can not do on your return home and ways of modifying activities to carry them out safely. You will be issued with some aids to assist you to get dressed. The Occupational Therapist will ensure you are able to use these independently prior to your discharge. You will be shown, by a physiotherapist how to safely climb and descend stairs, how to get into and out of a seated position and how to care for your hip once you return home. It is a good idea to enlist the help of friends or family once you do return home. Before you go home you will be shown some exercises, see page 24. You should be able to perform these exercises once you are at home. You may experience increased pain with exercise, but this will settle with rest. Most people are ready to go home very soon after surgery and this is an important step in your recovery. When at home, it is important to continue with your exercises as instructed by your surgeon and physiotherapist. Wound Your wound will be redressed prior to you going home. Some slight oozing of blood through this dressing is perfectly normal and should settle down after a couple of days. The dressing only needs to be changed if it becomes saturated and if so, the wound should be checked by a nurse or doctor. It is normal for your wound to be warm and reddish for up to a week as this is part of the healing process. The wound must be kept dry until the sutures are removed 12-14 days after the surgery. You will be asked to make an appointment with your practice nurse for removal of sutures or clips on a specified date. You must do this as soon as you are at home. 13 Swelling and bruising Bruising can be extensive and reach down to your knee but it should settle in a couple of weeks. Your whole leg can swell after hip surgery. You can help reduce this by raising your leg on a small stool (approx 18 inches in height) whilst sitting. You will be advised to use an ice pack on your hip; a bag of frozen peas wrapped in a towel will work very well. Normal post operative swelling should improve (but not always completely disappear) overnight while your leg is elevated and rested. You will find that your leg swelling gets worse during the day while you are using it. If the swelling does not improve overnight or the calf or thigh gets very hard and warm please contact your GP. Swelling can remain for 3-6 months after surgery. Pain It is normal for the hip to be painful after surgery, especially once you go home and start to walk more and exercise it. If there is a sudden increase in pain associated with extra activity, try using an ice pack, taking painkillers and reducing the activity for a day. It may pass but if it doesn’t and is stopping you from walking and/or bending your hip, contact your GP or the ward for advice on 01793 646333. It is important that you keep your hip moving and therefore you may need to take pain killers regularly for the first couple of weeks or even longer. We will give you a supply of painkillers when you are discharged. If you need any more, you will need to visit your GP. Rehabilitation Exercise is necessary to help promote the healing process and ideally you should start with gentle exercise prior to your surgery to build and strengthen your muscles. Patients having hip replacement surgery do not tend to need physiotherapy. This will be discussed with you prior to discharge. It is very important that you continue to increase your mobility and carry out your exercises after you have been discharged home, as this will aid your recovery and help you achieve good results. 14 An example Timetable explaining what will happen to you during your hospital stay Day of operation DAY 1 DAY 2 You will be assisted out of bed to sit in the chair. You may walk with a Zimmer frame if you feel able. You will start to mobilise with a zimmer frame and assistance. You will have a blood test. You will need to start hip exercises and practice walking with the frame around the ward. Your drip will be taken down once you are drinking well. Take regular painkillers and also laxatives to prevent constipation. You may progress onto sticks and practice stairs with the Physiotherapist. The wound will be checked. The Occupational therapist (OT) will discuss your home situation. Take regular painkillers and also laxatives to prevent constipation. The drain (if you have one) will be removed if it has stopped draining. Try to drink plenty of fluids and eat a normal diet. Your catheter should be removed tonight if you have one. You may progress onto sticks and practice stairs with the Physiotherapist. Take regular pain killing tablets. If you are ready the Physiotherapist or Rehab Assistants may practice your Try to drink plenty of fluids and transfers and teach you hip eat a light diet. exercises. You may have an x-ray. You may have an x-ray (if not done day 2). Try to drink plenty of fluids and eat a normal diet You may want to get dressed with help and advice from the OT or nurses. The OT will check you have the right equipment at home. Talk to the nurse about your discharge home/transport etc You will be discharged as soon as you are considered medically fit. 15 Blank for your notes 16 Risks and Complications Risks and Complications Whilst rare, there are some risks and complications associated with hip replacement surgery. Some complications include infection, blood clots, implant breakage, mal-alignment, and premature wear. Although implant surgery is extremely successful in most cases, some patients still experience pain and stiffness. No implant will last forever and factors such as the patient’s post-surgical activities and weight can affect longevity of the implant. Be sure to discuss these and other risks with your surgeon. There are many things that your surgeon may do to minimise the potential for complications. You may need to have your dental work up to date and may be shown how to prepare your home to avoid falls. The Anaesthetic As with any surgery there are risks associated with anaesthetic. There is an increased risk of heart attack, stroke, deep vein thrombosis, a clot in the lung or even death either during the operation or shortly after it. This risk is minimised by the assessment process at pre admission clinic where blood tests, heart recordings and x-rays will be carried out. Following this you may be referred to see an anaesthetist in the Cherwell Pre Assessment Clinic. Unfortunately unexpected complications do still occur. Breathing Exercise. It is important to regularly take several deep breaths every hour; this will help to reduce the complications that can be experienced following joint replacement surgery. Deep Vein Thrombosis This is a blood clot in the veins of the leg, most commonly in the calf, but can also occur in the thigh/groin. Precautions are taken to avoid this happening but orthopaedic surgery means that you are at risk. When you are seen in pre-assessment clinic you will be assessed for your risk of deep vein thrombosis and the treatment you are given will depend on your risk factors. The main way to avoid a blood clot is to keep the muscles in your legs working and the best way to do this is to walk around. Whilst you are in bed you should do the following exercises. 17 1. Circulatory exercise. When lying or sitting, rotate both ankles in a clockwise and anticlockwise direction. Repeat 10 times every hour. 2. Extension exercise. Lying on your back with your legs straight. Pull your toes up towards you, and then tighten your knees by pushing them down firmly towards the bed. Hold for 5 seconds then extend your toes away from you and hold for 5 seconds and relax. Repeat 10 times every hour. You will receive a small injection of a blood thinning drug every day during your hospital stay. You will be given medication to take at home and some anti- embolic stockings to wear for the first 6 weeks at home. Anti embolic stockings help to prevent DVT by increasing blood flow to prevent pooling of blood in the veins. They help to keep the veins tight and stop dilation of the veins. You will be measured for and given a pair on admission by the nurse admitting you; you need to wear your stockings to go to theatre. The signs and symptoms of a blood clot are extensive swelling in the calf which may also be warm and tender to touch. Walking on the leg can also cause pain in the calf. As already mentioned, swelling occurs after hip surgery but normal swelling usually improves when the leg is elevated for a period of time. If the swelling does not improve overnight when the leg is elevated, shows any signs listed above, or you are worried please seek advice from your GP. Occasionally a blood clot can move to the lungs and this is called a pulmonary embolus (PE). This is a serious condition if you experience any chest pain which is worse when taking a deep breath or any unexplained shortness of breath please come to the emergency department for urgent assessment. 18 Stiffness Although the new hip is very good at removing pain and making walking easier it does not move as far as a normal, natural hip joint. Sometimes the hip joint becomes quite stiff because of excessive bone or scar formation in the muscles around the hip. Most people find, however, that the relief of their arthritic pain is so good that a certain amount of stiffness does not worry them. Swelling Your leg may swell after your operation for some time (3-6months). Elevate your leg on a foot stool on and off during the day. The foot stool should be no higher than the chair you are sitting on. Dislocation It takes three months for the muscles and tissues to heal around the hip. During this time there is a danger that your new hip could dislocate, that is, the ball part of the joint coming out of the socket. The following precautions will help to prevent this from happening. 1. Do not cross your legs The operated leg must always be held out to the side, away from the midline of the body. 2. Do not bend the hip more than 90° Do not sit on low chairs or beds, do not lean forward. When sitting do not bend down to reach the floor – use your ‘easy reach’ 3. Do not twist your body while keeping your legs still. For example: reaching too far across your body and turning corners. 4. Do not lie on your unoperated side. For the first 4-6 weeks you should sleep on your back. After 4-6 weeks you can sleep on your operated side with a pillow between your knees. Remember – if it hurts, stop it!! 19 Wearing out and loosening All hip replacements wear with the passage of time and this leads to loosening of the hip within the bone. The younger you are at operation the more likely you are to wear the hip out. Approximately 1% of hip replacements fail per year so that by 10 years 10% will have failed. When the hip wears out and fails it becomes painful again and unfortunately the bone tends to get damaged by the loose hip. It is the quality of the remaining bone and your health at the time that determines whether a new hip can be done. This is known as a revision hip replacement. Leg Lengths The arthritic process in your hip often causes the leg to become a little shorter. It is usually possible to correct most of this at the hip operation. However, not all hips get full correction and some legs can even end up a fraction longer. This is usually because the surgeon has to make sure that the hip is as stable as possible to prevent dislocation. Sometimes an insole or small raise on the shoe is required to balance the leg length. Continuing pain Occasionally, patients do have some remaining discomfort after the operation, often because of some arthritis in the spine producing pain felt in the hip region. Infection and loosening can produce pain again. The area of the scar can be tender to lie on in bed at night. Constipation Unfortunately the medications required to control your pain can cause constipation. This causes you to be unable to open your bowels properly and in rare circumstances your bowel becoming completely blocked, which is very serious. Please be aware of this and increase the fibre in your diet, drink plenty of fluids and take the laxatives which are prescribed for you. If you become very uncomfortable, are not passing wind and/or your bowels are not working normally, please seek advice from your GP Rarer Complications Damage to the main nerves that run around the hip resulting in numbness and weakness in the leg or ankle, called a drop foot, which may be permanent. This may mean having to wear a splint to hold the ankle steady while walking. Occasionally the bone gets cracked in the placement of the new hip, If this happens the consultant will speak with you and discuss the changes that will be made to your recovery. It may mean having to use crutches for the first few months while the bone heals. 20 AtAtHome Home What activity range can be expected after this surgical procedure? Diligent physiotherapy, proper diet and a willingness to follow all of the recommendations your medical team makes will contribute to a successful recovery after surgery. Most patients are able to walk with the aid of sticks or crutches almost immediately. You should start to move without support as soon as you feel comfortable to do so. This will vary from individual to individual but many people find that they only need one stick when outdoors after approximately 6 weeks. It is recommended that you do not drive for a minimum of 6 weeks as your speed of reaction is affected. The responsibility for when you return to work is yours, however, you will find that your leg gets swollen and that swelling increases with the more activity you perform. Activities such as golf, doubles tennis and swimming can usually be resumed but not until three months after the operation. Always follow your doctor’s recommendations, as recovery time will vary for each patient. You will typically not be allowed to participate in high-impact activities or contact sports. These types of activities place extreme amounts of pressure on the joints, which could lead to complications. Ask your surgeon which activities you should avoid after surgery. Hydrotherapy (exercise in water) is beneficial for your recovery and can be commenced slowly once your wound has healed fully. If you would like to be referred for hydrotherapy please mention it at your 1st follow up appointment. Follow Up You will be seen 6 weeks after your operation by a nurse or physiotherapist who specialise in seeing people after joint replacement surgery. This is to evaluate your progress. You will not have an x-ray at this appointment. You will then be seen 1 year after surgery for an x-ray and consultation with a nurse or physiotherapist. If everything is ok at this appointment you will be discharged. The First Three Months Gardening involving kneeling and bending should be avoided for three months. Exercise in water or hydrotherapy is often helpful to improve your strength and mobility. Ask your physiotherapist about this. Swimming breaststroke should be avoided for three months. 21 Common Questions How long will my joint replacement last? We usually say that the majority will last at least 10 years but many last 15 – 20 years or maybe longer. Can my joint replacement wear out? The more you use your new joint the quicker you will wear it out but returning to normal activities and some sports is fine. You should avoid high impact exercise such as jumping, jogging and skiing. You should also avoid twisting your hip too much. How long will it take for me to recover from the operation? A hip replacement is a major operation and it can take many months for the joint to settle down properly and for you to feel completely well again. Most people feel a lot better in 3-6 months but you may still get some small improvements up to 1 year after the operation. When can I drive? Do not drive for six weeks, even if you have an automatic gearbox. Tests show that you will not regain your speed of reaction until 6 weeks have passed. Your car insurance will not cover you during the six weeks. You should inform your insurance company that you have had an operation. When can I go back to work? Most people need to take about 3 months off work depending on their job. When you do go back to work you need to avoid standing or sitting for long periods as your hip will become stiff. Many people go back to work on a gradual basis. How long do I need to take the hip precautions for? You should avoid bending, twisting and sitting on low furniture for 3 months. After this you can gradually start to return to normal activities but your hip may not be as flexible as a normal hip. 22 Can I have sexual intercourse? Sexual intercourse may be resumed 6-8 weeks after the operation. A side to side position with the operated leg uppermost and supported by a pillow or your partners’ thigh is usually comfortable. Please ensure your operated leg does not cross the midline. Men may find it more comfortable to lie on their back, with their partner kneeling astride them. After 3-4 months, intercourse with the man on top may be resumed, but women should avoid twisting their legs outwards too far. How and when can I increase my exercise? Many patients find that after about 3 months they want to start increasing their exercise. You may also be interested in going to a gym. Under a special scheme you may be able to be referred by your GP to receive special instruction in the gym at a reduced price. This scheme is called ‘Steps to Health’. What should I do if I think that there is a problem? If you start to experience any problems with your joint replacement either before or after your 1 year follow up appointment you should contact us on the number below or see your GP who can arrange for you to be seen at the hospital if necessary. Claire Woodruffe – Orthopaedic Specialist Nurse 01793 605312 Go for short walks regularly, remembering to take equal length strides, and gradually increasing the distance you walk at a rate that is comfortable to you. 23 Home Exercises 1. Stand on your good (un-operated) leg. Raise your operated leg up towards your nose by bending it at the knee. Take care not to bed the hip beyond 90° (a right angle). Hold for 34 seconds, if you can, then lower gently and repeat. Make sure you stand up straight when you do this exercise. 2. Again standing on your good leg and continuing to stand up straight, take your operated leg behind you. \Do not bend your knee. You will feel your bottom muscles tighten up, and again try to hold for 3-4 seconds, before lowering gently and repeating. Your leg will not move far, so don’t be discouraged. 3. Standing as you did for exercises 1 and 2, take your operated leg out to the side. Make sure that you lead out with your heel, not your toes, and keep your pelvis still. You will want to cheat, so again, do not be disheartened if the movement is small to begin with! Hold for 3-4 seconds, then lower gently and repeat. 4. For this exercise you sit in your chair with your feet on the floor. Now raise your foot off the floor as high as it will go out in front of you, keeping your thigh supported on the chair seat. You should see your foot lift straight up in front of you. Again hold for 3-4 seconds before lowering and gently repeating. 24 After 12 weeks Do not carry these exercises out before 12 weeks after your operation. Lying on your back with your knees bent Squeeze your buttocks together and lift your bottom off the floor. Return to the starting position Repeat 20 times. Aim to do this exercise 3 times a day. Lying face down. Lift your leg towards the ceiling keeping your knee straight. Repeat 20 times Aim to do this exercise 3 times a day. Sidelying. Keep the leg on the bed bent and the upper leg straight. Lift the upper leg straight up with the ankle flexed and the heel leading the movement. Repeat 20 times Aim to do this exercise 3 times a day Stand with a rubber exercise band around your ankle Pull the band by bringing your leg straight backwards. Repeat 20 times. Aim to do this exercise 3 times a day. 25 Stand with a rubber exercise band around your ankle. Pull the band by bringing your leg out to the side. Repeat 20 times. Aim to do this exercise 3 times a day. Standing against a wall with feet 3040cms from the wall and knees slightly bent. Place a ball between your kness Squeeze the ball between your knees and release. Repeat 20 times. Aim to do this exercise 3 times a day. Sitting with your arms crossed. Stand up and then sit down slowly on a chair. (This can be made easier and more difficult by changing the height of the chair) Repeat 20 times. Aim to do this exercise 3 times a day. 26 Summary We know the decision to have surgery is sometimes difficult. We hope this brochure has helped you understand some of the basics of total hip replacement surgery so that you can make the best decision for yourself. Millions of others have made this choice, allowing them to return back to a more active life. Some quotes from patients who have received joint replacement surgery here. “Don’t give up, sometimes it hurts and is depressing but, the results can be amazing” “sleep pattern is doing my head in, but have to put up with it” “REALLY amazed that all the arthritis pain has gone, in fact NO pain at all, just the aching” “That’s 2 weeks post op, still not a whole nights sleep, no pain, just aching” “I can really see how easy it would be to just sit around and end up with a stiff leg and a limp! I want to get back to normal, so I MUST PERSEVERE” “Listen to the professionals as to what you can or can’t do” “try to know the difference between ‘ouch that REALLY hurts, I have to stop’ and ‘oh that hurts a bit, but I need to do this’” “Remember a couple of months hard work can give you back a quality of life that you probably haven’t had for years” This brochure is not intended to replace the experience and advice of your orthopaedic surgeon. If you have any further questions, please speak with your orthopaedic surgeon. 27 The British Orthopaedic Association Orthocard Did you know that you can register your new hip joint? Registering your new hip will protect your new joint. It will show that you have an artificial joint, which helps prevent infection by letting your dentist, nurse and doctor know that you have one. It also will help at the airport when going through metal detectors and other security measures. If you are interested, please see the nurses on the ward when you are discharged. You will be given a pack with all the information needed, and once registered you will be able to use your card. http://www.boa.ac.uk/Pages/Welcome.aspx 28 Author/location Claire Woodruffe, JPI Information gathered from internet and Norfolk and Norwich Hospitals Review Date Updated August 2014 August 2012 Contact telephone Number 01793 60 53 12 Leaflet Number PALs Pil - 0435 29