Carer`s Guide - Easy Read
advertisement

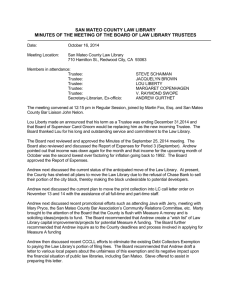
Your Carer’s Guide If you need help to understand this information please ask the Patient Experience Team. Tel: 01604 616000 (text relay calls welcome) Email: patient.experience@standrew.co.uk May 2015 Version 1 Sophia Feurtado, Head of Patient Experience. Developed with patients, carers and staff at St Andrew’s Healthcare. 1 Introduction This guide is to help you understand how St Andrew’s Healthcare can help the person you care for. It is an Easy Read version of our “Your Carer’s Guide”. It has all the main points that are in that version of this document. If you have any questions about this guide, or about St Andrew’s Healthcare, please ask your Social Worker. If you use our website, you will find more information to help carers, families and friends at: www.standrewshealthcare.co.uk/carers 2 Contents Before treatment starts About St Andrew’s Healthcare pages 4 to 6 Becoming a patient The patient’s first day Our care and treatment approach Treatment Reviewing care Preparing to move on The multi-disciplinary care team (MDT) Education and learning pages 6 to 11 Keeping in touch Ways to keep in touch Visiting pages 12 to 14 Family and Carer involvement Keeping people safe Listening to patients Compliments and complaints pages 15 to 17 Other useful information Useful groups and information pages 18 to 27 St Andrew’s locations Glossary 3 About St Andrew’s Healthcare The people we look after (“patients”) are aged from 13 years to adults including older people. We provide specialist care for people who have a range of difficulties and disabilities. These include people with: mental illnesses such as schizophrenia personality disorder learning disability autistic spectrum disorder brain injuries dementia and Huntington’s disease. We have hospitals in Northampton Birmingham Essex and Mansfield, Nottinghamshire. We ask patients if they would like us to include carers in their treatment and care. We check this with the patient from time to time while the patient is with us, to make sure we are doing what they want. 4 Becoming a patient (the “Admission process”) People come to us as patients when a healthcare professional sends us a special request (a “referral”). The person making the referral is usually a doctor or commissioner. How soon a person can become a patient with us depends on things like: how urgently the person needs help from us the commissioner agreeing to pay for the treatment and care; and any legal decisions that might need to be made, for example by a judge in a court. When we get a referral, our staff assess the person to decide if we can provide care and treatment for them. If we can help a person, the “MDT” decide which is the best ward to welcome the person as a patient. The MDT is the “multi-disciplinary team”, This is a group of healthcare professionals such as doctors, nurses and therapists who all care for a patient. We plan for when the patient will arrive with us (“the admission”) with the person’s current mental health team, if they have one. 5 The patient’s first day at St Andrew’s Patients go to their ward when they arrive. Staff from their MDT team welcome them to the ward. When the patient is ready, they have a look around where they will be staying. Staff give the patient information to help them with living on the ward. This information includes who the patient’s care co-ordinator is and the times of meals. We will keep patient’s property safe, if it cannot be with the patient on their ward. Anyone who comes into a secure unit may be searched for prohibited items, which are not allowed on the wards. This is for the safety of everyone. Treatment Each patient has an individual plan for their treatment and care. This based on the “Care Programme Approach” (CPA). We involve patients in deciding what this includes. We ask what worked well and what didn’t in the past. We use a range of professional assessment tools to decide what treatment is best for the patient. This takes up to 12 weeks. 6 Reviewing the patient’s care We meet to look at the progress patients are making. The patient can attend these meetings. They can be involved in deciding what should be in their care plan. Every week: the patient can meet with their Care Coordinator. Every 1-3 weeks: the patient can attend the Care Plan Update meeting (or Ward Round) with the MDT. Every 6 months: the patient can attend the CPA meeting with St Andrew’s MDT, clinicians from the home area and carers or family, if invited by the patient. 7 Preparing to move on The CPA review meeting will identify when a patient is ready to move to a different type of care, or into the community. Depending on the type of move, this may take some time to arrange. This is because there are lots of people outside of St Andrew’s involved, including: the Commissioners Community Health Professionals The Ministry of Justice. The patient may need help to identify a place to live. It can take a while to find the right place for them. The ward team will do their best to progress the move as quickly as possible. 8 The multi-disciplinary team A lot of people help provide care for patients. Depending on what an individual patient needs, these people may include: Chefs Our qualified chefs make sure meals are freshly made using local ingredients. Patients discuss menu options with chefs. Menus include meals to meet a wide range of cultural, religious and individual needs. Dietitians Help patients to be healthy and manage weight and allergies. They may also develop individual plans. Nurses and Healthcare Assistants Support patients with doing things on the ward. This may be things like having meetings or taking part in therapy sessions. Occupational Therapists Help the patient to do as much as they can for themselves. This can be things like getting dressed, having a shower, cooking or taking part in activities. Physical Healthcare team Develops individual care plans that help patients be active, fit and healthy. They use equipment on wards, in our sports halls or at local leisure centres, with agreement of the MDT. Physiotherapists Help patients improve their mobility, general health and prevent injuries. 9 Psychologists Deal with the way the mind works. They focus on behaviour and the thoughts, feelings and motivation underlying it. They aim to reduce distress and enhance psychological well-being by delivering a range of one-to-one and group therapeutic interventions. Psychiatrists Are the responsible clinicians (“RC”) in overall charge of a patient’s care. Only Psychiatrists can prescribe medication and will monitor how successful it is. Social Workers They help make sure the patient’s social needs are met. They help with arranging visits. They help patients keep in contact with their families, if they want to. They make sure everything is organised for the people to leave St Andrew’s when they are ready to move on. Speech and Language Therapists Support patients who have difficulty with communication, eating and drinking. This may, for example, help patients with voice problems or hearing loss, and to find the right words to say. 10 Education and learning We can help patients learn in ways that meet their individual needs, even if they have had poor experiences of learning in the past. We look at this as part of care planning with patients. Workbridge offers a range of opportunities to learn new social, technical and life skills in: Catering Ceramics Horticulture Office skills. St Andrew’s college offers a broad range of education programmes including English, Mathematics and Science, to meet our adolescent’s needs. 11 Keeping in touch Contact with carers, families and friends can help people to be happy and well. There are lots of ways people choose to do this. Telephone Please make telephone calls at times when patients are not doing therapy activities. The Social Work team can advise you of the best time to call. Letters Patients can choose to write letters. They can buy stamps at St Andrew’s, if they want. They may be asked not to write letters to someone if their letter is likely to upset that person. Patients can receive letters. Webcam/Video call We can arrange a secure video call using our system call Radvision (similar to Skype). There are special times when people can make these calls. The calls need to be booked in advance. Please ask staff if you would like to do this. Visits to St Andrew’s Before you visit a patient at St Andrew’s you will need to ensure you are on the Approved Visitor List. We ask that visits are at weekends and evenings if possible. Your Social Worker can help you with this. Home Visits If the patient is well enough, a home visit can be arranged with the Social Worker. 12 Visiting Visits usually last between 1-2 hours and take place in dedicated visiting rooms, some with CCTV. Depending on individual circumstances visits may take place in other locations. Anyone under 18 must be accompanied by an adult. A member of the Social Work team will supervise the first visit. A risk assessment will be completed before a visit. Costs of visiting St Andrew’s may be able to help towards the costs of visits. Please talk to staff about this before you plan your visit. Can I park on-site? Please reserve a parking space in advance. Please tell us if you need a disabled access space. Please bring your blue badge with you. Is it possible to stay overnight? There is some family accommodation in Northampton. St Andrew’s staff can help you find a place to stay near any of our hospitals. What do I do when I arrive? Please go to the main reception. Staff will take your photograph and issue you with a visitor’s badge. What do I need to bring with me? Please display your parking permit (if you have one). Please bring photographic ID for reception. 13 What can’t I bring with me? Each area will have its own list of things you can’t take onto the ward. The Social Work team will be able to tell you about the area you are visiting. Will I be searched? People entering secure areas may be searched. This includes carers, families and friends. Can I bring food with me? Home-made food can only be brought with the agreement of the Lead Nurse. Food cannot be stored on site and can usually only be taken into the visiting rooms. Can I bring gifts for the patient? You can bring gifts for the patient. Please check first that the patient is allowed to have them at St Andrew’s or on the ward. Your Social Worker can tell you about this. Can a visit be refused or cancelled? From time-to-time it may not be possible for a visit to go ahead, for example, if the patient is unwell or if there is an infection or outbreak of illness (such as flu). We try to minimise the number of visits which are cancelled. 14 Keeping people safe It is important to us that everyone feels safe and free from abuse and bullying when they are at St Andrew’s. The law says that everyone should be treated with dignity and respect. The law says that everyone should enjoy equality and human rights, even when detained under the Mental Health Act. So we always try to work in ways that help us to respect everyone’s rights. We hope you never feel unsafe, or that a patient is unsafe. If you do have any concerns, please tell us as soon as possible. This will help sort things out quickly. You can tell staff at St Andrew’s such as: - the MDT - Complaints Department tel: 01604 616 829 - Patient Experience Team - Safeguarding Lead tel: 01604 616 701. Or, you can tell an independent organisation such as: - VoiceAbility - local Safeguarding Team - Healthwatch - The Care Quality Commission (CQC). If you use the internet, you can find more information about rights and organisations at: http://www.standrewshealthcare.co.uk/safeguarding 15 Listening to Patients There are lots of ways people can tell us about their experience and wishes at St Andrew’s. All of our wards provide access to advocacy or solicitor services. Advocacy VoiceAbility provides independent, free, confidential advocacy to all St Andrew’s patients. Advocates visit the wards at St Andrew’s regularly to provide patients with the opportunity to find out more about their rights or to discuss their care and treatment. Befriending A volunteer befriender may be assigned to offer additional support if the patient would like one. Befrienders attend specialist training and have enhanced checks before we match them with a patient. Solicitors We use the Law Society’s database of solicitors, which offers a full range of services. St Andrew’s do not recommend any solicitors. 16 Complaints and feedback We welcome feedback to help us improve. If possible, please discuss any concerns you have with the multi-disciplinary team first. This helps to sort thing out quickly. If you would prefer, you can contact the Complaints Department directly. Telephone 01604 616 829 (text relay calls welcome) Email Complaints@standrew.co.uk Post Complaints Department Patient Experience Team St Andrew’s Healthcare Cliftonville Road Northampton NN1 5DG. Internet If you use the internet, you can download a form to give us feedback or make a complaint. This is the link: www.standrewshealthcare.co.uk/complaints 17 Other useful information and groups for carers There is a range of additional support available to you. The MDT looking after the patient can provide you with information about local groups. Our Chaplaincy and Spiritual Care team can offer support, call 01604 616 613 (text relay calls welcome). Organisations that can provide support include: NHS Carers Direct Tel: 0808 8020 202 www.nhs.uk/conditions/social-care-and-support-guide Rethink Tel: 0300 5000 927 www.rethink.org/carers-family-friends Mental Health Foundation www.mentalhealth.org.uk/ Who looks after you? Tel: 01933 677 907 www.wholooksafteryou.co.uk/ Royal College of Psychiatrists www.rcpsych.ac.uk/healthadvice/parentsandyouthinfo.a spx 18 Young Minds (Adolescent) Tel: 0808 8025 544 www.youngminds.org.uk Dementia Friends www.dementiafriends.org.uk/ Headway (Brain Injury) Tel: 0808 8002 244 www.headway.org.uk/caring.aspx Foundation for people with learning disabilities www.learningdisabilities.org.uk/ Mencap Tel: 0808 8081 111 www.mencap.org.uk/about-learning-disability/aboutlearning-disability National Autistic Society Tel: 0808 8004 104 www.autism.org.uk/living-with-autism/parents-relativesand-carers Action on Hearing Loss Telephone 0808 8080 123 Textphone 0808 8089 000 SMS 0780 0000 360 www.actiononhearingloss.org.uk/supportingyou/factsheets-and-leaflets.aspx Royal Association for Deaf People http://deafcarers.royaldeaf.org.uk/ Forums to join for carers at St Andrew’s You may be able to join a carers’ forum. Please ask your Social Worker or ward team to find out more. The Carers, Families and Friends Strategy Monitoring Group is open to all and meets regularly in Northampton. 19 St Andrew’s Locations Northampton We care for over 500 young people, men, women and older adults in Northampton. These services are medium and low secure, locked and open, so people may be with us when they are very unwell and when they are preparing to live in the community. We have a range of facilities to help patients on their recovery journey including: En-suite bedrooms Arts and crafts workshops Music studios Gym Café There are lots of buildings at St Andrew’s in Northampton. Some have their own reception. When you plan your journey, please check which reception you will need to go to when you arrive. Your Social Worker will be able to tell you. There are lots of things for patients to do. Patients are risk assessed to decide what they can do. Activities include: Art therapy Music Drama Sport and exercise Health and well-being sessions Work skills Adult education Vocational therapy at Workbridge. Northampton is in the middle of England. It has good road, train, coach and bus services. If you use the internet, you can find more information at: www.standrewshealthcare.co.uk/northampton 20 There are cafés you can use at Workbridge on Cliftonville Road and at the Tompkins Centre (towards the Billing Road end of the site). Birmingham We care for care for over 120 men and women in Birmingham. They have conditions such mental illness – for example psychosis and schizophrenia – and autistic spectrum disorder. These services are medium and low secure, so people may be with us when they are very unwell and when they are preparing to live in the community. There are lots of things for patients to do. Patients are risk assessed to decide what they can do. Activities include: - Art therapy - Music - Drama - Computer sessions - Sport and exercise - Health and well-being sessions - Spiritual and cultural time - Work skills - Adult education - Community outreach. There are lots of places to visit in the city. They include: - West Midland safari park - National Sea Life Centre, - Cadbury World, - museums and galleries. 21 Birmingham is in the middle of England. It has good road, train, coach and bus services. If you use the internet, you can find more information at: www.standrewshealthcare.co.uk/birmingham Essex We care for over 80 men and women in Essex. They have conditions such as complex mental health and personality disorders. There are lots of things for patients to do Patients are risk assessed to decide what they can do. Activities include: - Art therapy - Music - Drama - Computer sessions - Sport and exercise - Health and well-being sessions - Spiritual and cultural time - Work skills - Adult education - Community outreach. Our hospital is in Benfleet, not far from London. It is easy to reach by car. If you use the internet, you can find more information at: www.standrewshealthcare.co.uk/essex. 22 Nottinghamshire We care for up to 64 men at our Mansfield site. They have conditions such as autistic spectrum disorder and learning disabilities. There are lots of things for patients to do. Patients are risk assessed to decide what they can do. Activities include: - Art therapy - Music - Drama - Computer sessions - Sport and exercise - Health and well-being sessions - Spiritual and cultural time - Work skills - Adult education - Community outreach. Nottinghamshire is centrally located. It is easy to reach by car. If you use the internet, you can find more information at: www.standrewshealthcare.co.uk/Nottinghamshire 23 Glossary There may be a lot of new words to learn. This word list explains some of the words used in this leaflet and at St Andrew’s. We hope that this list will be helpful to you. Contraband A word some people use for “restricted or prohibited items”. Those are things that people cannot have at St Andrew’s for safety reasons. AWOL “Absent Without Leave” is when a detained patient does not have permission (“leave”) to be in the grounds or community. Best interests Under the Mental Capacity Act anything done for a person who cannot make decisions for themselves must be in their “best interests”. This means thinking about what is best for the person and not about what anyone else wants. The law has a checklist of things to think about when deciding on someone’s best interests. Capacity In mental health, this term has a technical meaning relating to the Mental Capacity Act. Having “mental capacity” means being able to make your own decision about something at a particular time. “Lacking capacity” is when a person is not able to make their own decision about something. Code of Practice Both the Mental Health Act and the Mental Capacity Act – have a “Code of Practice”. The Code of Practice tells doctors and nurses, in particular, how to make sure they are following the law. 24 Detained A person is detained if they are being kept in hospital under a section of the Mental Health Act and cannot leave. Informal patient This is when a person has chosen to be a patient at St Andrew’s. They are not detained. They have rights like other people not detained under the Mental Health Act. Leave Leave is when a patient, who is detained at St Andrew’s under the Mental Health Act, has permission to go into the hospital grounds or community. There are different types of leave. The type of leave a patient has describes where they have permission to go and when they can go there. For example “community leave” or “grounds leave”. Mental Capacity Act This law helps people who cannot make their own decisions because of their disability or “mental disorder”. Staff must use this law to help them decide whether a person is able, or unable, to make a particular decision. Mental disorder When the Mental Health Act talks about someone with mental health problems and whether or not they should be sectioned, it often uses the term “mental disorder”. The Act defines says this is any disorder or mental disability. It includes learning disability. It includes disability that makes you act in way which may seem dangerous to yourself of other people ( “abnormally aggressive” or 25 “seriously irresponsible”). Mental Health Act 1983 (“MHA”) This is a law in England and Wales which allows people to be detained in hospital (“sectioned”) if they have a mental illness and need treatment. A patient can only be kept in hospital if certain conditions are met. Nearest relative This is a family member who has certain responsibilities and powers if a person is detained in hospital under the Mental Health Act. These include the right to information and to discharge in some situations. The law sets out a list to decide who will be the nearest relative. The nearest relative can sometimes be changed. Section (“on a section”) This refers to the specific bit of law used to keep (or “detain”) a patient at St Andrew’s under the Mental Health Act. There are various different sections. People can be detained as patients for different lengths of time. Patients have the right to know why they have been detained and how long for. The law states that the professionals must review their detention periodically to confirm whether it is still necessary. Section 2 allows a person to be detained for up to 28 days in order to be assessed for their mental disorder. During this time the doctor can ask for an assessment under section 3 of the Act. Section 3 allows a person to be detained initially for up to six months so they can receive treatment in hospital. If necessary, detention under Section 3 can be renewed for a further six months and then yearly thereafter. Section 35 allows the Courts to remand a person to hospital for a report on their 26 mental condition. Section 37 (without restrictions), section 37/41(with restrictions) allows the Courts, on the advice of two doctors, to remand a person in hospital rather than prison. 27