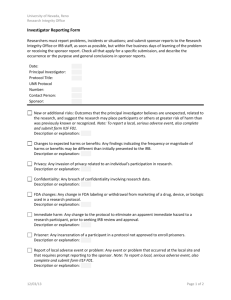
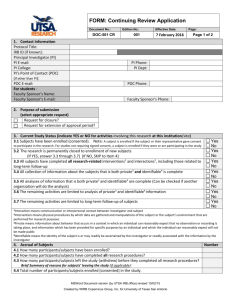
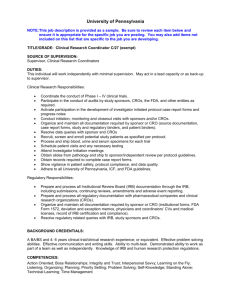
Sample SOPs - Research Compliance
advertisement

SAMPLE SOPS FOR CLINICAL INVESTIGATIONS AT EMORY UNIVERSITY OFFICE OF RESEARCH COMPLIANCE WEBSITE: HTTP://WWW.ORC.EMORY.EDU/ CONTACT: FEBRUARY 2012 ORC@EMORY.EDU SAMPLE SOPS: TABLE OF CONTENTS Table of Contents Introduction Good Clinical Practice (GCP) ............................................................................................. 3 Glossary of Terms ............................................................................................................... 8 Sample Standard Operating Procedures............................................................................ 16 CT 001 Write, Revise, Maintain Standard Operating Procedures (SOPs) ....................... 17 CT 002 Documentation Practices ..................................................................................... 19 CT 003 Training - Investigator and Clinical Research Staff ............................................ 22 CT 004 Responsibilities of the Principal Investigator ...................................................... 25 CT 005 Responsibilities of the Research Staff, Study Task Assignment ......................... 29 CT 006 Assessments of a Study Protocol ......................................................................... 31 CT 007 Set-up of the Study Files & Regulatory Documents Binder ................................ 35 CT 008 Management of Case History Records & Source Documents ............................. 39 CT 009 Case Report Form (CRF) Completion, Corrections, Handling queries ............... 41 CT 010 Control & Accountability of Test Article ............................................................ 44 CT 011 Subject Screening and Enrollment ....................................................................... 46 CT 012 Interactions with the Institutional Review Board (IRB) ...................................... 48 CT 013 Informed Consent Process ................................................................................... 52 CT 014 Monitoring and Audit visits ................................................................................. 55 CT 015 Event Recording, Reporting Requirements ......................................................... 57 CT 016 Reporting Protocol Deviations............................................................................. 61 Forms SAMPLE SOPS INTRODUCTION GOOD CLINICAL PRACTICE (GCP) GCP at Emory covers all clinical investigations involving FDA regulated test articles using human subjects conducted, in whole or in part, by or under the supervision of Emory University faculty, staff or students, or using Emory University facilities, funding or other University resources. GCPs for the investigative site are standards set by the FDA that delineate the roles and responsibilities of clinical investigators and all key personnel involved in the Research Protocol. Sample standard operating procedures (SOPs) are provided as a guide for clinical trials operations. SOPs are subject to applicable regulations, i.e. HHS, FDA, HIPAA; in the event of any conflicts between those laws or regulations and such SOPs, said laws and regulations shall control. The aim of these SOP templates and accompanying example forms is to provide researchers a way to standardize and simplify their organization and documentation relating to clinical trials, fostering conformance to Good Clinical Practice (GCP) requirements in clinical research. These SOPs are written templates that, if implemented, will permit a useful degree of uniformity in the performance of clinical studies. Example forms are included which should be customized. Background: Prior to beginning any Human Subjects Research, the clinical investigator must have acquired the appropriate knowledge and training regarding human research subject protections, the ethical conduct of research, and applicable regulations, as well as the specific knowledge needed to properly conduct his/her specific protocol(s). Prior to initiating work under any Research Protocol, the clinical investigator must thoroughly read and understand the Research Protocol as well as any informed consent and HIPAA Authorization documentation associated with the Research Protocol. The investigator is responsible for both the welfare of subjects and the quality of the data collected during the course of his/her clinical study. The clinical investigator and all key personnel involved in the Research Protocol must comply with all requirements imposed by the FDA Regulations, HHS Regulations, HIPAA Regulations and any other applicable laws and regulations. The FDA expects that a clinical trial is conducted in accordance with Good Clinical Practice (GCP). Compliance with GCP provides assurance that the rights, well-being, and confidentiality of trial subjects are protected and that trial data are credible. GCP is an international ethical and scientific quality standard for designing, conducting, recording, and reporting trials that involve the participation of human subjects. GCP is delineated in the International Conference on Harmonisation (ICH) guidance entitled “Good Clinical Practice: Consolidated Guideline'' (ICH-E6). The Consolidated Guideline represents the FDA’s current thinking on good clinical practices and describes the essential documents that individually and collectively permit evaluation of the conduct of a clinical study and the quality of the data produced. The guideline is to be followed when generating clinical data that are intended to be submitted to regulatory authorities and should also be applied to other investigations that involve therapeutic intervention in, or observation of, human subjects. The guidance document can be accessed on the FDA website URL: http://www.fda.gov/downloads/regulatoryinformation/guidances/UCM129515.pdf . 3 SAMPLE SOPS INTRODUCTION OUTLINE OF GCP: The rights and welfare of the individual clinical research subject must always be the paramount consideration in conducting clinical research. Accordingly, clinical research must be conducted in a manner that protects the rights, welfare and confidentiality of the human subject and also assures data credibility by protecting the integrity of accurate data that has been demonstrably collected according to the approved protocol. 1. The investigator must read the protocol and is personally responsible for: 1.1. Ensuring that an investigation is conducted according to: 1.1.1. the signed investigator statement/agreement, 1.1.2. the investigational plan (study protocol), 1.1.3. applicable regulations. 1.2. Ensuring that all persons assisting with the trial are adequately informed about: 1.2.1. the protocol, 1.2.2. the investigational product(s) (test article), 1.2.3. their trial-related duties and functions. 1.3. Protection of the rights, safety, and welfare of subjects under the investigator’s care. 1.4. Control of the test articles (drugs & comparators, devices) included in the investigation. 1.5. Assuring that each subject’s informed consent is obtained appropriately. 1.6. Proper delegation of authority for the conduct of various aspects of the study so that the investigator retains control and knowledge of the study. 2. The investigator shall assure that initial and continuing review of the proposed clinical study is performed according to the policies and procedures of the Emory University Institutional Review Board (IRB), as well as with any other IRB that has jurisdiction. 2.1. Continuous approval from the IRB must be maintained. 2.2. All unanticipated problems involving risk to human subjects or others are promptly reported to the IRB. 2.3. Any changes in the research activity are promptly reported to the IRB. 2.4. No changes are made in the research without IRB approval, except where necessary to eliminate apparent immediate hazards to human subjects. 3. The investigator shall control the test articles (drugs & comparators, devices). 3.1. A test article is administered only to subjects under the investigator’s personal supervision or under the supervision of a qualified sub-investigator responsible to the investigator 3.2. A test article is not supplied/provided to any person not authorized to receive it. 3.3. Adequate records of the disposition of the test article are maintained, including dates, quantity, receipt, distribution to subjects, and disposition. 3.4. Investigational Drug Service (IDS) is used for drug studies to control test articles, according to the “Investigational Drug Management for Clinical Studies” Emory University Policy 7.14; access this policy at http://policies.emory.edu/7.14 . Further information regarding use of the IDS service can be found on the OCR website at http://www.ocr.emory.edu/Pre-Award/Investigational_Drug_Service/index.cfm . 4. The PI is responsible for submitting any reports within time periods and according to procedures called for by: 4.1. Applicable federal, state and local regulations, including HHS, FDA and VA, 4 SAMPLE SOPS INTRODUCTION 4.2. 4.3. Emory University or applicable division or departmental policy or procedures, including the Institutional Review Board (IRB), and Office of Clinical Research (OCR), Contractual agreements with sponsors, collaborators, etc. 5. The investigator shall take adequate precautions to prevent theft or diversion when a drug that is a controlled substance is used in an investigation. Minimal precautions include access/use log and restricted access to drugs in a locked and secure storage place. 6. The investigator shall keep and maintain adequate and accurate records, including: 6.1. Case histories on each individual study subject that record all observations and other data pertinent to the investigation. 6.2. Screening, enrollment, and informed consent documentation; demonstrating that informed consent was obtained prior to participation in the study. 6.3. Study reports, including reports of progress, safety, financial disclosure and final completion. 6.4. Records retention as required. 6.4.1. Consult Emory records retention schedule; see http://records.emory.edu/ . 6.4.2. FDA regulation requires an investigator to retain records a minimum of two years after the close of the study or after the records are no longer required to support a drug or marketing application, whichever is longer. 6.4.3. Contract commitments must be met. 6.4.4. Consider transferring records to the Sponsor for contractual retention requirements that exceed FDA or Emory records retention schedules. 6.5. Reconcile ownership conflicts during study set up. FDA requires the clinical investigator to retain records. Emory considers research records to belong to the university. Departmental guidance should be established and followed, especially if the investigator leaves the university before the scheduled destruction of records. 6.6. Record transfer or record destruction should be verified and documented. 7. The investigator shall permit properly authorized persons such as governmental officials, Sponsor representatives or internal quality reviewers, to have access to copy, and verify records or reports made by the investigator. 7.1. Notice of such inspectional privileges shall be included in the Informed Consent form and HIPAA Authorization form. 7.2. The investigator is not required to divulge subject names to government inspectors unless there is a specific government request for this information; e.g. for the records of particular individuals require a more detailed study of the cases, or there may be reason to believe that the records do not represent actual case studies, or do not represent actual results obtained. 8. An MD must be designated as responsible for all trial-related medical decisions. Medical decisions must be made by a qualified person permitted by state licensure laws to make or enact such decisions. The investigator should: 8.1. Ensure that adequate medical care is provided to a subject for any adverse events related to the trial, during and as followup to a subject's participation. 8.2. Inform a subject when medical care is needed for intercurrent illness(es) of which the investigator becomes aware. 5 SAMPLE SOPS INTRODUCTION 8.3. Inform the subject's primary physician about the subject's participation in the trial if the subject agrees to the primary physician being informed, and has signed a HIPAA Authorization form permitting such disclosure. 6 SAMPLE SOPS INTRODUCTION References: Conducting Clinical Trials within the Emory University School of Medicine (EUSOM), access at link called “User Manual for Clinical Trials” from http://www.ocr.emory.edu/index.cfm . Emory University Institutional Review Board Policy & Procedures (IRB P&P) http://www.irb.emory.edu/researchers/formstools/docs/other/PoliciesAndProcedures.pdf . Compliance Program Guidance Manual for FDA Staff – Compliance Program 7348.811 Bioresearch Monitoring: Clinical Investigators; especially Part III Inspectional http://www.fda.gov/ICECI/EnforcementActions/BioresearchMonitoring/ucm133562.htm . Device Advice, FDA Center for Devices and Radiological Health (CDHR), at http://www.fda.gov/cdrh/devadvice/ . Good Clinical Practice in FDA-Regulated Clinical Trials, at http://www.fda.gov/oc/gcp/default.htm . Office for Human Research Protections at http://www.hhs.gov/ohrp/ . Form FDA 1572 Statement of Investigator, at http://www.fda.gov/opacom/morechoices/fdaforms/FDA-1572.pdf . 21 CFR 50 ----- Protection of Human Subjects 21 CFR 54 ----- Financial Disclosure by Clinical Investigators 21 CFR 56 ---- Institutional Review Boards 21 CFR 312---- Investigational New Drug Application 21 CFR 314---- Applications for FDA Approval to Market a New Drug 21 CFR 809---- In Vitro Diagnostic Products for Human Use 21 CFR 812---- Investigational Device Exemptions 21 CFR 814---Premarket Approval of Medical Devices 45 CFR 46 ----- Protection of Human Subjects 45 CFR 160---- General Administrative Requirements 45 CFR 164 Security and Privacy http://www.accessdata.fda.gov/scripts/cdrh/cfdocs/cfCFR/CFRSearch.cfm ICH E2A – FDA Guideline for Industry – Clinical Safety Data Management: Definitions and Standards for Expedited Reporting; March 1995 ICH E2C – FDA Guideline for Industry – Clinical Safety Data Management: Periodic Safety Update Reports for Marketed Drugs; November 1996 ICH E6 – FDA Guidance for Industry – Good Clinical Practice: Consolidated Guidance; 1996 http://www.ich.org/cache/compo/276-254-1.html 7 SAMPLE SOPS: INTRODUCTION: GLOSSARY OF TERMS GLOSSARY OF TERMS ACRONYM TERM AE Adverse Event or Adverse Effect Is this a UP now? Or keep AE and add UP? an AE does not necessarily have a causal relationship with the study treatment. An AE can therefore be any unfavorable and unintended sign (including an abnormal laboratory finding), symptom, or disease temporally associated with testing the investigational product, whether or not related to the product. (ICH-E2A) “Attributable, Legible, Contemporaneous, Original, Accurate”, expectations of the FDA to demonstrate acceptable data quality. Case History Records The information comprising an individual case, includes the Case Report Form (CRF) and supporting data such as signed/dated Informed Consent Forms, research notes and protocol test records; may also include physician progress notes, nurses’ notes, hospital charts, medical records, etc. Case Report Form A printed, optical, or electronic document designed to record all of the protocol-required information to be reported to the Sponsor on each trial subject. A CRF is used to record all relevant individual subject or study patient data. The Sponsor will use this data to perform statistical analysis; the resultant analyses are included in the medical report. The CRF is designed by the Study Sponsor, possibly in collaboration with the Investigator, and is based on the Study Protocol. Clinical Investigation Any experiment in which a Test Article is administered or dispensed to, or used, involving one or more human subjects. An experiment is any use of a Test Article except for the use of a marketed product in the course of medical practice. (FDA) ALCOA CRF DEFINITION Any untoward medical occurrence in a clinical investigation subject; Clinical trial: A biomedical or behavioral research study of human subjects that is designed to answer specific questions about biomedical or behavioral interventions (drugs, treatments, devices, or new ways of using known drugs, treatments, or devices). (NIH definition) Note – throughout these CT SOPs “clinical investigation”, “study”, and “clinical trial” may be used interchangeably. CI CRC CT Clinical Investigator See “Investigator” Clinical Research Coordinator Assists the Principal Investigator (PI) in the setup and conduct of a clinical trial, working at a clinical research site under the immediate direction of a PI and whose research activities are conducted under Good Clinical Practice (GCP) Guidelines. Refer to the online user manual for research personnel “Conducting Clinical Trials within the Emory University School of Medicine” found on the OCR website http://www.ocr.emory.edu/Education_&_Outreach/OCR_User_M anual/index.cfm . Clinical Trial See Clinical Investigation 8 SAMPLE SOPS: INTRODUCTION: GLOSSARY OF TERMS ACRONYM TERM CTA Clinical Trial Agreement DEFINITION The CTA defines the responsibilities of each party with respect to specific trial-related duties, indemnity and financial matters: what costs will be covered, and when and how payments will be made. The CTA must be processed through and signed by appropriate individuals in the Office of Sponsored Programs. Individual PIs are not authorized to enter into CTAs or contracts on behalf of Emory University. For sponsored trials, a CTA signed between Emory University and the sponsor of a clinical trial is required prior to subject enrollment, and should be in place before expenditure of funds. CFR Code of Federal Regulations The codification of the general and permanent rules published in the Federal Register by the executive departments and agencies of the Federal Government. It is divided into 50 titles that represent broad areas subject to Federal regulation, updated once each calendar year. FDA and DHHS/Public Welfare regulations are found in 21 CFR and 45 CFR, respectively. CDA Confidential Disclosure Agreement A legal contract between the signing parties that outlines the confidential materials the parties wish to share for the purpose(s) specified. CDAs are also known as confidentiality agreements or non-disclosure agreements (see also NDA). Confidential information is generally a “trade secret” and means information that derives actual or potential value from not being generally known to, and not being readily ascertainable by, other persons who could obtain economic value from its disclosure or use. Confidential information may include intellectual property, technical or nontechnical data, a formula, pattern, compilation, program, device, method, technique, drawing, process, financial data, financial plans, product plans, or other information which is not commonly known by or available to the public and is the subject of reasonable efforts to maintain its secrecy. A person that assumes one or more of the obligations of a Sponsor, as an independent contractor to the Sponsor. Confidential Information CRO Contract Research Organization CV Curriculum Vitae A written description of an individual’s work experience, educational background, and skills; may include a list of publications, presentations, awards, honors, affiliations and other details. Refer to http://www.medicine.emory.edu/faculty_staff/faculty/promotions/cv.cfm or http://www.med.emory.edu/dean/docs/Standard_CV_Template.pdf . DHHS Department of Health and Human Services One of the largest federal agencies, the Department of Health and Human Services is the principal agency for protecting the health of all Americans. DHHS’ responsibilities include public health, biomedical research, Medicare and Medicaid, welfare, social services, and more. DHHS agencies include FDA, NIH and the CDC. 9 SAMPLE SOPS: INTRODUCTION: GLOSSARY OF TERMS ACRONYM TERM Device Drug EHSO EUSOM or SOM Environmental Health and Safety Office DEFINITION A device is intended to affect the structure or any function of the body; it does not achieve its primary intended purposes through chemical action or metabolism within or on the body. A medical device is a physical item (an instrument, apparatus, implement, machine, contrivance, implant) or an in vitro reagent, or other similar article that is intended for use in the diagnosis of disease or other conditions, or in the cure, mitigation, treatment or prevention of disease. Medical devices range from simple tongue depressors and bedpans to complex programmable pacemakers with micro-chip technology and laser surgical devices. A drug is a chemical substance that is intended for use in the diagnosis, cure, mitigation, treatment, or prevention of disease, and substances, other than food, intended to affect the structure or any function of the body. “Investigational new drug” or “investigational drug” means a new drug that is used in a clinical investigation and includes a biological product that is used in vitro for diagnostic purposes. ICH defines “investigational product” as a pharmaceutical form of an active ingredient or placebo being tested or used as a reference in a clinical trial, including a product with a marketing authorization when used or assembled (formulated or packaged) in a way different from the approved form, or when used for an unapproved indication, or when used to gain further information about an approved use. Emory University EHSO is chiefly responsible for risk assessment and hazard mitigation from biological, chemical or radiological sources. Emory University School of Medicine http://www.med.emory.edu/ FDA Food and Drug Administration The FDA is the federal agency responsible for protecting the public health by assuring the safety, efficacy, and security of human and veterinary drugs, biological products, medical devices, food supply, cosmetics, and products that emit radiation; and that these products are honestly, accurately and informatively represented to the public. GCP Good Clinical Practice An internationally recognized standard for the design, conduct, performance, monitoring, auditing, recording, analysis, and reporting of clinical trials that provides assurance that the data and reported results are credible and accurate, and that the rights, integrity, and confidentiality of trial subjects are protected. HHS Health and Human Services Shortened form of DHHS. Health Information: Any information whether oral or recorded in any form that is created or received by the Emory Covered Component that relates to an individual’s past, present or future physical or mental health or to the payment for such health care. 10 SAMPLE SOPS: INTRODUCTION: GLOSSARY OF TERMS ACRONYM TERM HIPAA Health Insurance Portability and Accountability Act Individually Identifiable Health Information DEFINITION Privacy rules promulgated by the US government directing health care entities (covered entities) to establish procedures to ensure the security, integrity, privacy and authenticity of health information and to safeguard its access and disclosure. Health Information including demographic information that identifies an Individual or with respect to which there is a reasonable basis to believe the information can be used to identify the Individual. ICF Informed Consent Form A statement explaining the study to a potential subject, including the risks entailed in participation. The ICF is used to document the subject’s voluntary agreement, based upon adequate knowledge and understanding of relevant information, to participate in research or to undergo a diagnostic, therapeutic, or preventive procedure. Also called Informed Consent Document (ICD). IRB Institutional Review Board An appropriately constituted group that has been formally designated to review and monitor research involving human subjects; having the authority to approve, require modifications in, or disapprove research. This group review serves an important role in the protection of the rights and welfare of human research subjects. IDS Investigational Drug Service Emory University IDS, located at the Emory University Hospital and Clinic A. A clinical investigator is any listed or identified investigator or subinvestigator who is directly involved in the treatment or evaluation of research subjects. The principal investigator: is the individual responsible for the conduct of a clinical trial at a trial site, under whose immediate direction the test Article is administered or dispensed to a subject. If a trial is conducted by a team of individuals at a trial site, the investigators are co-investigators. The principal investigator is the responsible leader of the team. Co-investigators sign a Form FDA 1572 or the investigator agreement with the Sponsor and each coinvestigator is individually held responsible for all investigator responsibilities, as agreed to by signing on the 1572 or investigator agreement. Sub-investigator includes any individual member of the clinical trial team designated and supervised by the investigator at a trial site to perform critical trial-related procedures and/or to make important trial-related decisions (e.g., associates, residents, research fellows). A sub-investigator is listed on the 1572, but does not sign it. See “Sponsor-investigator” Clinical investigators sign investigator agreements/statements that attest to their knowledge of and agreement with their responsibilities under FDA regulations as researchers. Drug or biologics trials use Form FDA 1572 (investigator statement) for this purpose and device trials use an investigator agreement. Investigator: CI Clinical investigator PI Principal investigator Co-I or Co-PI Co-investigator Sub-I Sub-investigator SI Sponsor Investigator Investigator Agreement/Statement 11 SAMPLE SOPS: INTRODUCTION: GLOSSARY OF TERMS ACRONYM TERM IIT Investigator Initiated Trial Key personnel LAR legally-authorized representative Monitor DEFINITION A clinical trial developed by the investigator and the investigator is a Sponsor-investigator. Those persons associated with a specific clinical investigation whose assigned duties may include contact with subjects/research volunteers; activities that may affect subject welfare or study compliance; or impact data integrity. An individual or judicial or other body authorized under applicable law to consent on behalf of a prospective subject to the subject’s participation in the procedures involved in the Research. [45 CFR § 46.102(c), 21 CFR § 50.3(l)] A monitor oversees the progress of the study on behalf of the Sponsor; ensuring that the study is conducted, recorded and reported according to the study protocol, SOPs of the Sponsor, GCP and regulatory requirements. The monitor‘s main role is to help ensure proper study conduct and the timely generation and collection of quality data for the Sponsor, generally accomplished by routine inspection/monitoring of the study site. Except for an investigator-initiated study under the direction of a Sponsor-investigator, the monitor should be independent of the investigative staff conducting the research at the site or institution, and should not be employed or supervised by the investigative site or the institution. Clinical Research Associate (CRA) is the standard industry term for the monitor (distinct from the Emory University HR job description for “Clinical Trial Associate”). NDA Nondisclosure Agreement A legal contract between the signing parties that outlines the confidential materials the parties wish to share for the purpose(s) specified. NDAs can restrict all parties in their use of the materials provided, or they can only restrict a single party. NDAs are also known confidential disclosure agreements (see CDA). OCR Office of Clinical Research OCR is part of Emory University’s Office of Research Administration. The mission of the OCR is to organize and enhance operational processes that support the efforts of the clinical research team and to facilitate the timely initiation, execution, management and completion of clinical trials at Emory. OGCA Office of Grants and Contracts ( at Emory University) The Office of Grants & Contracts, among other things, provides the central oversight for the post-award fiscal activities of all grants and contracts and maintains the labor and effort reporting systems. OSP Office of Sponsored Programs (Emory) Collaborates with the Emory community to identify, obtain and administer extramural funding in support of the University mission. NIDPOE Notice of Initiation of Disqualification Proceedings and Opportunity to Explain A NIDPOE letter informs the recipient clinical investigator (CI) that FDA is initiating an administrative proceeding to determine whether the CI should be disqualified from receiving investigational products. FDA may issue a NIDPOE letter when it believes the CI repeatedly or deliberately violated FDA's regulations governing the proper conduct of clinical studies involving investigational products, or submitted false information to the Sponsor. 12 SAMPLE SOPS: INTRODUCTION: GLOSSARY OF TERMS ACRONYM TERM P&P Policy and Procedures PI PHI SAE DEFINITION So called when a university, departmental or other unit’s policy is accompanied and supported by standard operating procedures. The procedures may be requisite approved procedures requiring adherence or may be template/example procedures that are designed as guidance or recommended practice. The policy should clearly state if accompanying Procedures are for guidance. Principal Investigator See “Investigator” Protected Health Information Certain Individually Identifiable Health Information created, transmitted or maintained by a covered entity. Protocol A document that describes the objective(s), design, eligibility requirements of subjects, methodology, statistical considerations, and organization of a trial; for these SOPs includes the protocol and the protocol amendments. Protocol Deviation Any noncompliance with the protocol, good clinical practices, regulatory or institutional requirements. Regulatory Documents Binder (Reg. Binder) A study file created for each study containing study specific information relating to the overall study, in contradistinction to case history documentation. Aka “Critical Documents Binder”, “Essential Documents Files” Research A systematic investigation, including research development, testing and evaluation, designed to develop or contribute to generalizable knowledge. (HHS definition) FDA has defined “Clinical Investigation” to be synonymous with “Research”. Serious Adverse Event Any untoward medical occurrence that results in any of the following outcomes: death, a life-threatening adverse experience, inpatient hospitalization or prolongation of existing hospitalization, a persistent or significant disability/incapacity, or a congenital anomaly/birth defect. Source Data All information in original records and certified copies of original records of clinical findings, observations, or other activities in a clinical trial necessary for the reconstruction and evaluation of the trial. Source data are contained in source documents, either original records or certified copies. Source Documents Original documents, data, and records (e.g., hospital records, clinical and office charts, laboratory notes, memoranda, subjects’ diaries or evaluation checklists, pharmacy dispensing records, recorded data from automated instruments, copies or transcriptions certified after verification as being accurate and complete, microfiches, photographic negatives, microfilm or magnetic media, x-rays, subject files, and records kept at the pharmacy, at the laboratories and at medico-technical departments involved in the clinical trial). 13 SAMPLE SOPS: INTRODUCTION: GLOSSARY OF TERMS ACRONYM TERM Sponsor DEFINITION An individual, company, institution, or organization that takes responsibility for and initiates a clinical investigation. The role of Sponsor is NOT related to funding or financial support. SI Sponsor-Investigator An individual who both initiates and conducts, alone or with others, a clinical trial, and under whose immediate direction the investigational product is administered to, dispensed to, or used by a subject. The term does not include any person other than an individual (it does not include a corporation or an agency). The obligations of a Sponsor-investigator include both those of a Sponsor and those of a principal investigator. SOP Standard Operating Procedure Written documents that describe the routine procedures to be followed for a specific operation, analysis, or action. Consistent use of an approved SOP ensures conformance with organizational practices, reduced work effort, reduction in error occurrences, and improved data comparability, credibility, and defensibility. SOPs also serve as resources for training and for ready reference and documentation of proper procedures. SOP may alternatively be called a “Procedure”, as in “Policy and Procedures” . Subject An individual who is or becomes a participant in research, either as a recipient of the test article or as a control, or on whose specimen an investigational device is used. A subject may be in normal health or may have a medical condition or disease. Also called “Human Subject”, “Study Patient”, and “Research Subject”. Test Article The object of an investigation for human use subject to FDA regulations: that drug, biological product, medical or investigational device, or the study control, used in a clinical investigation. The term “test article” includes placebos and comparators identified in the study protocol, as well as the investigation product. Unanticipated problem An event not previously identified involving risk to the participant or others. (Refer to IRB P&P § 64.) UP 14 SAMPLE SOPS: INTRODUCTION: GLOSSARY OF TERMS ACRONYM TERM Witness or Impartial Witness DEFINITION Someone whose signature attests that the subject has provided consent of their own free will and has been fully informed of the study. The best witness is a subject’s friend or family member who has been present while the study was being explained to the subject. A witness must have no vested interest in the study. Alternatively, a witness signature may attest only to subject signature, in which case this limited role of the witness must be clearly stated. OR A person, who is independent of the trial, who cannot be unfairly influenced by people involved with the trial, who attends the informed consent process if the subject or the subject’s legally authorized representative cannot read, and who reads the informed consent form and any other written information supplied to the subject. (ICH E6 –1.26) 15 SAMPLE SOPS SAMPLES OF STANDARD OPERATING PROCEDURES SAMPLE STANDARD OPERATING PROCEDURES The SOPs presented in this guide are intended to provide examples of clinical trial SOPs. PIs and/or clinical trial units are strongly encouraged to prepare custom SOPs to substantiate clear and consistent workflow throughout a human research study. In the event of a conflict, applicable laws, regulations or approved Emory University policies and procedures will take precedence over departmental or study-specific SOPs. 16 SAMPLE SOPS CT 001 WRITE, REVISE, MAINTAIN STANDARD OPERATING PROCEDURES (SOPS) PURPOSE: To provide instructions to produce, approve, control, and revise Standard Operating Procedures (SOPs). SCOPE: This SOP delineates systematic process activities and functions for Emory University unit in compliance with Good Clinical Practices (GCP) requirements for the management and coordination of clinical trial operations. It applies to unit personnel engaged in clinical trial research, administration or management. Procedure: 1. An SOP may be initiated or revised based upon need. Revisions may respond to changes in governmental regulations or guidelines, to Emory research practice or policy, or to improve clarity or ease of use. 1.1 Any qualified person may prepare a draft SOP for consideration. 1.2 Anyone may propose changes to an existing SOP; users are encouraged to make recommendations. 2. An SOP is adopted as of the Effective Date shown on each SOP, after obtaining the approval signatures. 3. Investigators, and affiliated research and administrative staff will sign a training log documenting their training on relevant SOPs. The training log should specify topics and SOPs covered. 4. Departmental, Divisional or Unit SOP: 4.1 Local SOPs must clearly delineate the scope of the SOP, including who is covered and what activities are affected. 4.2 Any user may submit a request for change, modification or revisions of an SOP to the office or unit having approved the SOP. 4.3 Initial versions and any revisions to unit SOPs must be approved by a Unit Manager or Department/Division Head. The second approver would generally be familiar with the unit’s research and with good clinical practice, i.e. a clinical investigator, a unit business administrator or research administrator. 4.4 Study Specific SOP should be approved by at least two people, including the Principal Investigator. The second approver would generally be a member of the research team, i.e. the research nurse or clinical research coordinator. 4.5 Departmental or protocol specific SOPs may be maintained and kept available by the department research administrator or the clinical research coordinator. 5. SOP maintenance: 5.1 Historical records of the SOPs must be maintained, so that a copy of each SOP version, whether it has been revised, superseded, or terminated, will be retrievable. WRITE, REVISE, MAINTAIN STANDARD OPERATING PROCEDURES (SOPS) CT 001 REV.00 17 SAMPLE SOPS 5.2 5.3 5.4 SOPs should be protected in order to assure the current version is in use. The official version is the version containing the signature approvals and may be either hardcopy or electronic file. Upon revision, a consecutive revision number is assigned, and the version number placed in the SOP footer. Local (unit or study specific) SOPs may be reviewed at any time for compliance or quality assurance purposes. RESPONSIBILITY MATRIX Responsible Person / Unit Department or Division or Unit head Departmental Research administrator or designee Responsible Person / Unit Principal Investigator Clinical Trial Coordinator or designee Responsible Person / Unit All Clinical Trial Personnel, Research Team members Action for CT Local/Departmental SOPs Review and approve departmental CT SOPs. Ensure compliance within department to SOPs. Maintain current and historical records of departmental CT SOPs. Make available current versions of departmental SOPs to users, assure that obsolete versions are archived. Action for CT local/protocol specific SOPs Review and approve protocol specific SOPs. Write and/or review protocol specific SOPs for accuracy and effectiveness. Maintain SOPs. Assure current version is available to users. Action for All CT SOPs Any qualified person may write an SOP. Follow applicable SOPs. Notify, in writing or by email, the SOP owner or keeper upon observation of a need for update or revision to the SOP. RELATED SOPS: none RELATED FORMS: FORM CT-01 SOP TEMPLATE Implementation/Revision Dates: Last Review Date: Approval Signatures: Effective Date: WRITE, REVISE, MAINTAIN STANDARD OPERATING PROCEDURES (SOPS) CT 001 REV.00 18 SAMPLE SOPS CT 002 DOCUMENTATION PRACTICES PURPOSE: To encourage authenticity and the production of quality data. SCOPE: This SOP covers all source data and source documents supporting human subject studies, especially manual records (paper records / hard copies) such as entries to the Case Report Form. It affects all personnel involved in recording, correcting or keeping information, either hard copy documents or electronic files, supporting a study using human subjects. PROCEDURE 1. Source documents. 1.1 Information must be recorded by authorized study personnel. 1.2 All blanks of a form should be filled in. 1.3 If original records are damaged or obliterated, those records shall be retained when possible with the reconstruction of the record, including an explanation and supervisory signoff. 2. Data must meet quality attributes (ALCOA) to be acceptable, including: Attributable: Entries shall be signed or initialed by the entrant. Legible: All information/entries must be clear and readable. Contemporaneous: Promptly record activities and results, date the signature or initials at the time the entry is recorded. Original: The first record of an event or data collection is source data. Accurate: Records must be true values given with reasonable precision. 2.1 All data entries must be traceable to an individual. Data entry must be signed or initialed. Signature or initials must always be dated at the time of entry. 2.2 Information should be recorded in indelible ink. The record should permit copying; consistent use of a colored ink rather than black ink may help distinguish a copy from an original. Neither pencils nor erasable ink pens should be used. 3. All activities must be recorded. Examples include: Maintain telephone logs, including communications with subject, monitor or Sponsor. Verify data or document reviews with reviewer’s initials, and date of review. Maintain records of research team meetings. 4. Corrections shall not alter or obscure an earlier entry. 4.1 Original entry must remain legible. Do not make erasures. Do not use correction fluids (“white-out”). Do not over-write an entry. Do not use pencil. 4.2 To make a correction to a hard copy: DOCUMENTATION PRACTICES CT 002 REV.00 19 SAMPLE SOPS 4.3 Cross out the wrong entry with a single line that keeps the first entry legible. Write the correct entry near the wrong entry, or indicate location of correction if space is limited. Initial the correction. Date the correction. Explain the correction (if necessary). Any later corrections (those not made the date of the original entry) to a record must be explained. Any corrections not made by the original author/entrant must be explained. Electronic source records are subject to FDA rules, and must maintain a valid audit trail. 5. Data entry must be performed by authorized study personnel, and the meaning of a signature must be indicated or correlated to the entry. 5.1. Signature meaning may be indicated by statement: 5.1.1. An example of signature meaning indicated by statement is that of the informed consent form stating “If you're willing to volunteer for this research, please sign below”: the research subject’s signature on an informed consent form means they have volunteered to participate in the study. 5.2. Signature meaning may be indicated through job descriptions, team organization & responsibilities, or study specific delegation of tasks. (refer to Sample Form 02 “Study Responsibilities Log, Examples”) Examples of “signature meaning” indicated by job description and/or by team responsibilities could be: 5.2.1. Principal Investigator signature would always mean that the material has been reviewed & approved, or reviewed & corrective action instituted as indicated, by PI. 5.2.2. CRC or Research Nurse signature or initials on a CRF would indicate that the person signing has performed the task (such as taking/recording vital signs) or has accurately transcribed data (such as laboratory values) received for the entry, per the study responsibilities assignment log. RESPONSIBILITY MATRIX Responsible Person/Unit Internal auditors or inspectors Principal Investigator All Researchers Documents control personnel Action Review source data and source documents for GCP compliance/ALCOA. Sign-off (with date) documents upon completion of review (i.e. patient records, test results) Assign responsibilities for the data collection and recording. Ensure that information entries result in usable data, conforming to ALCOA. Maintain documents in secure and retrievable locations and formats. RELATED SOPS; CT 01 Write, Revise, Maintain Standard Operating Procedures (SOPs) CT 07 Set-up of the Study Files and Regulatory Documents Binder DOCUMENTATION PRACTICES CT 002 REV.00 20 SAMPLE SOPS RELATED FORMS: FORM CT-02 STUDY RESPONSIBILITIES LOG Implementation/Revision Dates: Last Review Date: Approval Signatures: Effective Date: DOCUMENTATION PRACTICES CT 002 REV.00 21 SAMPLE SOPS CT 003 TRAINING - INVESTIGATOR AND CLINICAL RESEARCH STAFF PURPOSE: To ensure all staff members involved in clinical research are properly trained concerning FDA regulations, ICH guidelines, study protocol/Sponsor requirements, and Emory University policies & procedures. To describe the process for continuous employee training. To describe the procedures for maintaining documentation of initial training and continuing education. SCOPE: The training will include information the investigators and clinical research staff need to properly conduct a clinical trial, including applicable policies and SOPs. It applies to all employees and independent contractors in the study site research staff. All research personnel listed on the IRB submission, regardless of their position, must be trained. Key research personnel includes principal investigators, co-investigators, research nurse, clinical coordinators, and any other research team members who have contact with research participants and/or their research data and identifiers. PROCEDURE 1. Training in HIPAA and privacy protection is required prior to accessing Protected Health Information (PHI); training is provided through ORC or Emory HealthCare. 2. Training in human subjects’ protection required by the IRB (CITI training) must be completed before the researcher is permitted to participate in the conduct of an IRB approved protocol. Certification is valid for two years, and must be maintained by each research staff member without lapse throughout the study duration. 3. Depending on study activities, job specific training may be required through the Emory University Environmental Health and Safety Office (EHSO). Examples of EHSO training include: 3.1 All employees who have potential occupational exposure to bloodborne pathogens will receive training from EHSO on the epidemiology, symptoms and transmission route of bloodborne pathogen diseases. 3.2 Those employees engaged in shipping specimens must complete and maintain approved IATA shipping training for the shipment of infectious agents and biological substances. 3.3 Employees involved in studies in which radiation is used must complete training by the Radiation Safety Office. 4. GCP training is recommended and is generally conducted by the Sponsor prior to subject enrollment. Records should be maintained of date & duration of training, instructor qualifications, and of subject matter covered. Online GCP training is available through CITI. TRAINING OF INVESTIGATOR AND CLINICAL RESEARCH STAFF CT 003 REV.00 22 SAMPLE SOPS 5. Job specific training should be identified and the individual training plan designed and completed. Completion certificates should be kept with study documentation or in the departmental training files. 5.1 Examples of job specific training include ERMS through OCR, or the EHSO training from the earlier item. 5.2 Investigator meetings, monitor or Sponsor training of the researchers should be documented, include agenda or topics covered. (See § 6, this SOP) 5.3 Sample training plan form is provided in Form CT- 003. 6. All new participating investigators and clinical research staff will be provided orientation and training materials to acquaint them with the principles of Good Clinical Practice. 6.1 Study personnel will be trained on applicable departmental and/or study specific SOPs prior to working on a clinical study. 6.2 Training methods may include, but are not limited to: classroom; computer module or web-based; on-the-job or observation of experienced employees who are designated trainers, provided that their training is sufficiently documented in accordance with § 8 below. 7. Before conducting protocol activities, research staff shall receive protocol specific training provided by the Sponsor representative, monitor and/or the Clinical Investigator. 8. Training must be documented. 8.1 Departmental training files should be kept for each employee. The individual’s file should contain: Current licensure and/or professional certification. Curriculum vitae; updated at least biennially. Current job description. Completed training forms or indication/certification of CEUs or training completed, including CITI certifications. 8.2 Departmental training records are cumulative and should be retained for the duration of each employee’s tenure. 8.3 Training records should also be retained with study records for the duration of the study records. RESPONSIBILITY MATRIX Responsible Person/Unit Departmental supervisor, Research Administrator or PI Sponsor Research Administrator/designee or CRC Action Develop individual training plans for research team members and ensure that each individual completes training specified before beginning work. Provide time/resources for requisite training Provide study specific training Ensure all personnel working on protocol understand responsibilities Update and maintain training files TRAINING OF INVESTIGATOR AND CLINICAL RESEARCH STAFF CT 003 REV.00 23 SAMPLE SOPS RELATED SOPS: none RELATED FORMS: FORM CT-003 TRAINING PLAN FORM FORM CT-004 TRAINING RECORD FORM Implementation/Revision Dates: Last Review Date: Approval Signatures: Effective Date: TRAINING OF INVESTIGATOR AND CLINICAL RESEARCH STAFF CT 003 REV.00 24 SAMPLE SOPS CT 004 RESPONSIBILITIES OF THE PRINCIPAL INVESTIGATOR PURPOSE OF THE PROCEDURE: To delineate responsibilities required of qualified researchers in the role of Principal Investigator (PI) in clinical trials. SCOPE: The PI of a clinical study site is responsible at that site for ensuring subject safety, the integrity and validity of the data, oversight of the clinical trial with delegation of research responsibilities and conduct of the research staff. A qualified principal investigator may be, but is not limited to, a physician, nurse, or senior staff member. Emory IRB policy requires that all protocols submitted to the IRB must have prior departmental/school approval and include at least one investigator having faculty rank at Emory. (http://www.irb.emory.edu/researchers/formstools/docs/other/PoliciesAndProcedures.pdf) School of Medicine requires faculty status for PIs unless approval in writing has been obtained from the Dean’s Office. http://www.med.emory.edu/research/PI%20Eligibility%20Policy1.html PROCEDURE 1. Although certain duties may be delegated, the PI retains full accountability for the overall conduct of the study and of any duty assigned to a designee. 1.1 The PI defines and delegates responsibilities for all study protocol activities. 1.2 The PI oversees protocol related conduct of all research team members. 1.3 Co-investigators may jointly conduct the study, and sign the 1572 or the investigator agreement with the Sponsor; however, there must be a single principal investigator identified who is the responsible leader of the team. 1.4 The PI may delegate a medically qualified sub-investigator to perform critical trial related procedures as directed by the PI, i.e., administer and dispense the test article, or to make important trial-related decisions. 2. The PI should: 2.1 Ensure that all medical decisions and activities are performed by an individual qualified according to state and local regulatory and licensure requirements. 2.2 Ensure that adequate medical care is provided to a subject for any adverse events related to the trial, during and following a subject's participation. 2.3 Inform a subject when medical care is needed for intercurrent illness(es) of which the investigator becomes aware. 2.4 Inform the subject's primary physician about the subject's participation in the trial if the subject agrees to the primary physician being informed and an appropriate HIPAA Authorization form is executed. 3. The PI is personally responsible for the conduct of the investigation. The PI may not delegate or assign responsibility for the following items: RESPONSIBILITIES OF THE PRINCIPAL INVESTIGATOR CT 004 REV.00 25 SAMPLE SOPS 3.1 3.2 3.3 3.4 3.5 3.6 The PI shall ensure compliance with IRB requirements, obtaining written approval from the IRB before any human subjects are allowed to participate in a clinical investigation1. Approval from additional committees may be required. The PI ensures the investigation is conducted according to the current written approved protocol and will only enact changes to the protocol after consulting with the Sponsor and obtaining prior approval from the reviewing IRB2. The PI shall thoroughly read and understand protocol, informed consent and HIPAA authorization documents. The PI will become familiar with the information in the device manual or the investigator’s brochure, including the potential risks and side effects of the test article prior to subject recruitment/enrollment for the study. The PI must clearly delineate duties that are delegated, naming the qualified study staff member accepting the task. However, the PI is responsible for the supervision of research staff and the conduct of the study. The investigator’s signature on a study document will indicate that the investigator has reviewed and approved the document. 4. The PI is responsible for fulfillment of the study’s financial and contractual agreements with Emory, the Sponsor, grantor, and/or government agencies, i.e. NIH, FDA. Emory University delineates process requirements including routing and trial management reviews or procedures that are not covered in this SOP. 4.1. Current guidance for study or grant management may be found on Emory University websites: Office of Clinical Research http://www.med.emory.edu/research/cto/routing.cfm Office of Sponsored Programs (OSP) http://www.osp.emory.edu/ and Office of Grants & Contract Accounting (OGCA) http://www.ogca.emory.edu/ . 4.2. Guidance for study management is available on the government websites, i.e.: fda.gov, especially the Office of the Commissioner’s GCP Program at http://www.fda.gov/oc/gcp/ and the (CDHR) Medical Device (Device Advice) http://www.fda.gov/cdrh/devadvice . nih.gov, especially the Office of Extramural Research and the Office of Human Research Protections (OHRP). 4.3. Before any subject is enrolled in a sponsored trial, applicable clinical trial agreements (CTA) must be approved & signed by both the sponsor and an authorized Emory University signatory. 4.3.1. An individual PI is not authorized to enter into CTAs or contracts on behalf of Emory. 4.3.2. A nondisclosure agreement (NDA) is not a CTA (refer to CT006 Assessments of a Study Protocol). 1 Except as provided in 21 CFR 56.104(c) for emergency use, which exception must be handled in accordance with federal regulations and the Emory University IRB policies and procedures. 2 Single exception: if a change is necessary to eliminate immediate hazards to the human subjects the investigator shall immediately effect the change, providing prompt notification to the IRB and Sponsor in accordance with applicable responsibilities and IRB P&Ps. RESPONSIBILITIES OF THE PRINCIPAL INVESTIGATOR CT 004 REV.00 26 SAMPLE SOPS 4.3.3. Pre-award and clinical trial agreements are signed for the university by OSP. 4.4. For FDA regulated studies, the PI submits a binding agreement to the Sponsor wherein the investigator agrees to comply with the protocol (drug) or investigational plan (device) and with FDA regulations. The investigator must have signed the agreement prior to participation in the study. DRUG: Form FDA 1572 Drug studies require the PI to send a “statement of investigator” to the Sponsor. This is a legally binding agreement from the investigator to the FDA (via the Sponsor) of the regulatory commitments made by the PI. DEVICE: Investigator Agreement The agreement must include a signed commitment to: 1. conduct the investigation in accordance with the agreement, the investigational plan, 21 CFR §§ 50, 56, and 812, and any conditions of approval imposed by the IRB or FDA; 2. supervise all testing of the device involving human subjects, and 3. ensure that the requirements for informed consent are met. The investigator statement/agreement may be submitted by the Sponsor to the FDA as part of the application process. 5. While the PI retains full personal responsibility for the conduct of the study, the PI may delegate responsibilities for study records and conduct. Common delegations include: 5.1 Informed Consent Process: inform each study participant that the study agent is being used for investigational (research) purposes and will ensure that the requirements pertaining to obtaining informed consent are met prior to participation in the study. Note: All persons who obtain informed consent must be qualified in accordance with IRB P&Ps. 5.2 Test article use and accountability: shipment, storage, dispensing and administration and final return of unused supply. 5.3 Fiscal management of the investigation. All payments and billing are handled through the Emory University Office of Grants and Contracts (OGCA). At no time should the investigator or investigative team member, Department, Division, Unit, etc., receive any direct payment from the Sponsor without an explicitly written exception statement from the OGCA. Recruitment incentives and other study incentives from a Sponsor are strictly prohibited. 5.4 Reporting task for required notifications to the IRB and/or to the Sponsor that occur in the course of the investigation, e.g. adverse events, protocol deviations, continuing review, amendment/modification submissions, etc. 6. The PI will hire adequate, trained staff to conduct the investigation. The PI will ensure that all sub-investigators are aware of their responsibilities by reviewing the protocol and the individual assignments and commitments prior to study initiation. The content, method, date RESPONSIBILITIES OF THE PRINCIPAL INVESTIGATOR CT 004 REV.00 27 SAMPLE SOPS and time of this review will be documented in the training files of the Regulatory Documents Binder. 7. The PI will provide supervision and guidance to staff relating to the conduct of the investigation or administrative functions. Review activities must be documented. 7.1 The PI must review related reports, decisions and documentation verifying actions taken for those duties that have been delegated. 7.2 The investigator should establish a regular review schedule for each study. 7.3 Examples of primary activities to be reviewed with the designee and a template for a study review schedule are provided in Form CT-06 Studies Activities Review Schedule. 8. The PI is responsible for the maintenance of professional credentials (including accurate, up-todate CVs and licenses for personnel involved in the conduct of clinical research). Healthcare professionals shall maintain applicable license(s) in the state for which they are enrolling subjects and/or credentials in the facility or hospital where the research is conducted. 9. The PI shall upon any request from any properly authorized officer or employee of Emory University, the IRB, FDA, DHHS, OIG, DEA3 or NIH, at reasonable times, permit such officer or employee to have access to, and copy and verify any records or reports made by the investigator. RELATED FORMS: FORM CT-06 STUDY ACTIVITIES REVIEW SCHEDULE FDA REFERENCES “Investigator Responsibilities - Protecting the Rights, Safety, and Welfare of Study Subjects” issued October 2009 http://www.fda.gov/downloads/Drugs/GuidanceComplianceRegulatoryInformation/Guidances/UCM187772.pdf “Guidance for Industry and Clinical Investigators: The Use of Clinical Holds Following Clinical Investigator Misconduct” issued September 2004 http://www.fda.gov/downloads/RegulatoryInformation/Guidances/UCM126997.pdf Implementation/Revision Dates: Last Review Date: Approval Signatures: Effective Date: 3 limited to controlled substances accountability RESPONSIBILITIES OF THE PRINCIPAL INVESTIGATOR CT 004 REV.00 28 SAMPLE SOPS CT 005 RESPONSIBILITIES OF THE RESEARCH STAFF, STUDY TASK ASSIGNMENT PURPOSE: To promote efficient and effective clinical trial administration through the division and allocation of responsibilities, describing the duties of the research staff. SCOPE: This SOP covers initial allocation of responsibilities and changes in personnel or in responsibilities and applies to Principal Investigator (PI), sub-investigators and clinical site research personnel at a study site involved in the coordination and/or implementation of a clinical trial. PROCEDURE 1. Develop and maintain position descriptions for each staff member who will be involved in clinical trials. 1.1 There will be on file a written job description for each employee who performs protocol-required duties, based upon the job classifications delineated by the Emory University Human Resources (HR) department. 1.2 Protocol specific job descriptions shall not exceed the scope of Emory Human Resources job description. 1.3 Roles and responsibilities specific to protocol activities shall be related to the personnel log designed for the study. 1.4 Protocol specific job descriptions shall include description of type of identifiable health information that a person may have access to and circumstances under which access is permitted. 2. Maintain current records or curriculum vitae (CV) for each staff member involved in clinical trials, including all investigators. Records must include: 2.1 Training records, including education/continuing education study specific training. 2.2 Licenses, certifications. 3. Research team members must maintain requisite confidentiality. Confidentiality issues may include: subject information and PHI, study data, proprietary information, etc. Confidentiality agreements will ordinarily be routed through the Emory Office of Sponsored Programs (OSP). 4. Identify the research staff members who will be involved in the study. Prepare a detailed list of the duties and responsibilities of each staff member as they relate to specific studies Record the allocation of tasks prior to study initiation (refer to Form CT-02 Examples of Study Responsibilities Log) and promptly record changes to maintain currency of the Task Assignment allocation log. 4.1 The PI may allocate day to day responsibilities to individuals on the research team. The PI or the study responsible person should discuss/agree upon the allocation of tasks with staff members. 4.2 Roles and responsibilities should be clearly defined to ensure that all tasks have been assigned and that persons understand their personal accountability. RESPONSIBILITIES OF THE RESEARCH STAFF, STUDY TASK ASSIGNMENT CT 005 REV.00 29 SAMPLE SOPS 4.3 4.4 4.5 4.6 4.7 4.8 Persons assigned drug administration or medical responsibilities must be qualified according to state and local laws and licensing boards. Persons assigned study tasks are held individually responsible for capably fulfilling those tasks with integrity and competence. Complete the personnel log for Task Assignment/Study Responsibilities. If the Sponsor or contract research organization (CRO) has a similar form, this may be substituted. Changes in personnel or in responsibilities must be tracked and when necessary approved by the IRB and the Sponsor. When appropriate, send the update of the Investigator Agreement or the Form FDA 1572 to the Sponsor, and an amendment/modification submission form to the IRB. When individuals are removed from or newly assigned to the project and when responsibilities have been altered for personnel, the Study Responsibilities log should be updated concurrently with assignment changes. Expect the monitor to review this regularly. 5. Study specific training on the assigned tasks should be provided to the study personnel, including instruction in the use of the CRF. 6. If a research staff member cannot substantially perform their assigned tasks specific to a study protocol, that person must promptly alert the PI and/or the research manager in writing to ensure that all study obligations continue to be met. For example, if the study procedures or the rate of enrollment create more work than can be accomplished, the delegated team member must inform the PI, in writing, that additional personnel or time commitment will be required. 7. The documents described in this SOP shall be available to the clinical monitor, the university or IRB compliance officers or auditors, and to any properly credentialed representative of FDA or other regulatory entity. RELATED FORMS: FORM CT-02 STUDY RESPONSIBILITIES LOG Implementation/Revision Dates: Last Review Date: Approval Signatures: Effective Date: RESPONSIBILITIES OF THE RESEARCH STAFF, STUDY TASK ASSIGNMENT CT 005 REV.00 30 SAMPLE SOPS CT 006 ASSESSMENTS OF A STUDY PROTOCOL PURPOSE: To describe pre-agreement procedures for assessing feasibility of conducting a specific protocol at the investigative site (A, B), and post-conduct assessment of a completed trial (C). SCOPE: This SOP will apply to all clinical studies considered and/or conducted. The Principal Investigator (PI), in conjunction other appropriate scientific and/or business personnel will assess Pre-assessment: o whether or not it would be feasible to conduct the protocol, and o if the protocol is scientifically sound and the study has intrinsic merit. Post-assessment: success of study operation (separate from scientific review) for “lessons learned”. PROCEDURE A. PROTOCOL ASSESSMENT, CHOOSING TO PARTICIPATE 1. The PI must initially assess a study proposal/protocol, considering: 1.1. ethics, 1.2. investigator site capabilities (i.e.: equipment; facilities; staff), 1.3. clinical feasibility and scientific merit, 1.4. business practicality. 2. The PI should consider whether the Sponsor will be charged for an in-depth review of a protocol. (Charges and/or costs for initial study preparation should be included in a budget.) 2.1 Protocol review should be carried out as soon as is practical after the investigator receives a copy of the protocol. 2.2 Feedback regarding the suitability of study acceptance should be given to the Sponsor at the earliest opportunity. Discuss issues identified regarding the protocol that may impact recruitment, safety, etc. 3. A nondisclosure agreement/confidential disclosure agreement (NDA or CDA) is generally required in order to obtain the protocol and study documents from the Sponsor for assessment review. 3.1 Emory University is the designated party to the agreement and the NDA must be sent to OSP for review and execution. 3.1.1 A PI may not sign any legal document, including a NDA, on behalf of Emory University. 3.1.2 Emory’s standard form “Mutual Non-Disclosure Agreement" is found on the Office of Sponsored Programs (OSP) website under ‘Forms and Agreements/ Other Forms and Agreements’ at http://www.osp.emory.edu/forms/other/index.cfm ASSESSING/CHOOSING A STUDY PROTOCOL CT 006 REV.00 31 SAMPLE SOPS 3.2 All persons provided confidential information during this assessment phase should be on the NDA (see last page of document “To be signed by Emory faculty and all other personnel who is expected to receive Confidential Information.”). Note that the NDA is not the same as the contract for the study. The contract or clinical trial agreement (CTA), is sent to OSP via the Office of Clinical Research (OCR) to be negotiated and approved through the standard routing procedures. The signed CTA must be in place before any subject is enrolled. 4. The PI is responsible for ensuring adequate consideration & review of a protocol tendered by a Sponsor. All reviewers should be party to the NDA. 4.1 Refer to Form CT- 007, Choosing a Protocol: Assessment Checklist. 4.2 Review should be carried out by individuals with the appropriate expertise: this may include, when appropriate and/or required, a Co-Investigator together with a Study Site Coordinator, Study Nurse, Research Administrator, financial reviewer, others. 4.3 The Investigators, Study Coordinators, and other appropriate site personnel may review the protocol to ensure the following: 4.3.1 The study objectives are clear. 4.3.2 The study design is feasible. 4.3.3 The study will not expose subjects to undue risk. 4.3.4 The study is ethically acceptable. 4.3.5 The study is financially and logistically feasible. 4.3.6 There are a sufficient number of potential subjects available for the study. 4.3.7 There is sufficient & qualified staff to conduct the study. 4.3.8 The site has the appropriate equipment to conduct the study. 4.3.9 Adequate medical care will be provided to a subject for any adverse events, including clinically significant laboratory values, related to the trial. 4.3.10 The investigator will have sufficient time to properly conduct and complete the trial within the agreed trial period considering other time commitments. 4.3.11 Potential real or perceived Conflicts of Interest between study personnel and study conduct are identified, and may be reasonably managed. 4.3.12 Impediments to IRB approval are identified and resolved. 4.4 If the PI feels the department staff members are inadequately qualified to assess the validity of any aspects of the trial, for example the statistical methods or the trial design, an expert opinion should be sought. 5. Discuss protocol review comments with the Sponsor and research team. 5.1 Team: Discuss comments to determine overall acceptance of study. 5.2 Sponsor: Assess responsiveness of Sponsor to PI’s comments. 5.3 Prior experiences of working with the Sponsor should be a consideration. 6. If PI rejects the study, promptly relay this information to the Sponsor. Include reasons for rejection and a summary of study topics that meet your criteria for acceptance in order to keep the communications open. 7. PI should only accept a study that he/she feels is scientifically justified and that can be satisfactorily performed in accordance with all regulatory and policy requirements. ASSESSING/CHOOSING A STUDY PROTOCOL CT 006 REV.00 32 SAMPLE SOPS B. CASE REPORT FORM (CRF) REVIEW 8. Review of the draft CRF must be performed expeditiously. 8.1. The CRF is reviewed by appropriate staff, which may include the PI, the research nurse, the research coordinator and/or others who will enter data on the CRF. 8.2. If an investigator has been closely involved in designing and writing the protocol, such draft review is better assigned to another study team member. 8.3. Check that adequate space is provided on the CRF to record information. 8.4. When possible, try to complete the test CRF as a true-to-life exercise. Use several staff members to independently complete the CRF. Use real source documents to supply data for the CRF. Compare completed results to identify and clarify ambiguities, difficulties and possibly missing items. 8.5. Avoid use of PHI in a CRF. 8.6. A review checklist is provided in Form CT-09, CRF Review Checklist. 9. Inform the Sponsor of CRF review comments as soon as possible in writing. 9.1. If the CRF under review is a draft, request in writing that the Sponsor inform the individual responsible for the trial of a summary of the changes that will be made following review. 9.2. If the CRF under review is not a draft, request in writing that the Sponsor responds to the comments to the PI responsible for the trial. 10. The CRF is not ordinarily reviewed by the IRB. However, if the CRF version has been approved by the IRB as part of the protocol, then changes to the CRF must be submitted for IRB review and approval before use. 11. Study personnel should be instructed in the use of the CRF. C. STUDY CONCLUSION ASSESSMENT 12. The CRC should prepare a summary of the conduct of the study. 12.1 Refer to Form CT-10, Protocol Completion Assessment. 12.2 List “lessons learned”, include what went wrong and what went right for application to future trials. 12.3 The summary should include the following study events/findings Enrollment history & timeline: subjects screened, enrolled, completed, Serious adverse events, Protocol deviations, amendments, problems encountered, Subject response, Financial balance, specifying areas of credit and loss, CRA/monitor feedback & comments. 12.4 The CRC should circulate the summary to the study staff. 13. The PI should hold a study staff meeting to evaluate study execution. 13.1 Compare post-study finding with pre-assessment. ASSESSING/CHOOSING A STUDY PROTOCOL CT 006 REV.00 33 SAMPLE SOPS 13.2 13.3 13.4 Institute corrective action for procedural changes where indicated to increase efficiency and/or compliance for future work. Determine if the Sponsor is one with whom you want to continue working. Determine if the pre-assessment was accurate. 14. Integrate post-assessment findings in order to 14.1. improve the overall assessment process. 14.2. improve study operations/management. RELATED FORMS: FORM CT-08, PROTOCOL ASSESSMENT LOG FORM CT-09, CRF REVIEW CHECKLIST. Form CT-10, PROTOCOL COMPLETION ASSESSMENT Implementation/Revision Dates: Last Review Date: Approval Signatures: Effective Date: ASSESSING/CHOOSING A STUDY PROTOCOL CT 006 REV.00 34 SAMPLE SOPS CT 007 SET-UP OF THE STUDY FILES & REGULATORY DOCUMENTS BINDER PURPOSE: To define the preferred method for the set-up and use of the study files, including the regulatory documents binder (“Reg. Binder”), to assure regulatory compliance for completeness and retrievability of records. SCOPE: This SOP defines the essential documents that must be on file for each clinical study. Essential documents are those that individually and collectively permit evaluation of the conduct of a study and the quality of data produced. These documents assist in the: management of a trial, comparison of the practices and procedures used by the clinical investigator with the commitments made in the protocol and the investigator agreement or the Form FDA 1572, comparison of the data submitted to the Sponsor with supporting data in the clinical investigator's files; and authenticate compliance of the investigator and study staff to GCP. All personnel permitted access to the research study files and regulatory binder must follow this SOP. PROCEDURE Organization of study files - The files/binders suggested here may be subdivided, consolidated, and/or re-organized to conform to specific study needs. Study sites are not required to adopt the structure outlined in this procedure, but are urged to consider a standardized approach such as this when developing their filing approach to study data management. It is strongly recommended that sites adhere to the order of documentation of the binder checklist appended to this SOP (Form CT-012, Critical Documents Checklist) in order to facilitate routine inspection by study monitors, internal auditors or regulatory agencies. Study sites not following this SOP must establish an SOP to document their filing approach. The study files are best subdivided into sections: Financial contracts (Procedure item 9 following) Study management (Procedure item 10 following) Case history records (Procedure item 11 following) (The formalized compilation of study records dealing with the conduct of the study as a whole will be referred to as the “Reg. Binder”.) The following procedures apply to all of the study files. 1. GCP requires that all study related activities be documented. 1.1 The checklists provided for this SOP include the documents expected to fully capture study activities. An explanation should be given if a document on the checklist is not generated in the course of a study. SET-UP OF THE STUDY FILES AND REGULATORY BINDER CT 007 REV.00 35 SAMPLE SOPS 1.2 Specific studies may require additional documents. 2. Essential documents shall be stored in files and/or in binders and maintained for the required retention duration. 2.1 Study files must be stored in a secure location. 2.2 Files or file room shall be locked to prevent unauthorized access. 3. The filing system shall be segmented so that individual trials remain separate, in particular when sponsored by different entities. 3.1 Participant case history records are generally stored separately from the other documents with CRFs for one study stored together. 3.2 Monitors are limited to the review of their assigned studies only; monitors sent by a Sponsor may only review CRFs belonging to that Sponsor. 4. A contents sheet should be maintained and inserted as the first page(s) of each file/binder. Within each topic, it is recommended that documents be filed in ascending date order (most recent documents in front). 5. A complete record must be maintained of all approved documents; all versions of approved documents must be retained. 5.1 When required documents are modified or updated, the original and all modified or updated versions must be maintained. Some workable ways to control use of the correct version include: a. Documents that have been superseded may be moved from the active binder to an “historical” binder. Although all required documentation must be available for inspection at any time, all documents need not be stored together in one location. The historical binder should maintain the same contents format (#3 above) as the active binder. b. All version copies may be kept together, with the most recent version to the front of the binder. Indicate on the obsolete document that it has been replaced, i.e. write “superseded by ----- (new) version date” on the cover or top copy of the obsolete document. (Reminder: initial and date any comment you write on a document.) 5.2 A Study File should be prepared as soon as is practical after the first contact with a potential Sponsor (or CRO). a. All correspondence regarding a potential study should be kept. b. If the PI decides not to participate in the study then confidential materials should be returned or destroyed, as agreed between the two parties. Verification of destruction (include method, date, responsible party) should be sent to the Sponsor, with the PI retaining a copy of the notification. c. Keeping the information as to why a study was declined may help with future decisions. 5.3 When the Reg. Binder is supplied by the Sponsor, the initial departmental Study File should be converted to the Sponsor format upon its availability. 6. To preserve blinding, certain documents related to the investigational study products may be stored separately, e.g. in site pharmacies, until after the final “data-lock” following study close-out. SET-UP OF THE STUDY FILES AND REGULATORY BINDER CT 007 REV.00 36 SAMPLE SOPS 7. Source documents must be defined for the study and be traceable. When warranted, use a source document matrix. Refer to sample Form CT-014. Where original records are kept elsewhere, i.e. patient chart, it is recommended that when practicable, a copy be kept in the research subject’s case history record binder. 8. Label each binder with the Sponsor name and contact information, the protocol number and the binder number. Disclosure issues should be considered regarding labeling information in order to protect both subject privacy and Sponsor confidentiality, e.g., avoid use of study title, subject PHI, Sponsor information exposed to competitors. 9. Financial Contracts & Disclosures - Refer to checklist Form CT- 011 for financial contracts. 9.1 Emory University policy is that all financial agreements for clinical studies are made through the institution NOT with an individual. 9.2 Routine FDA inspections include review of financial disclosure statements only; other financial data, e.g. salaries, budgets, are not provided to an FDA inspector 10. Study Management documents - Refer to checklist Form CT- 012 for Critical Documents Binder content. 10.1 These are documents that pertain to the study as a whole. They may include: the Protocol & supporting documents, approvals and IRB communications, study personnel, screening & enrollment logs, consent log, Sponsor communications. 10.2 Routine FDA inspections limit review of personnel data to training & qualifications information, i.e. job description, CV; other personnel data such as performance review is not part of the study record, nor provided to the FDA inspector. 11. Case History Records - Refer to checklist Form CT- 013 for Case History Records. 11.1 This includes the clinical & research information comprising an individual case, including the Case Report Form (CRF), supporting data and source documents. 11.2 A separate case history record is accrued and maintained for each enrolled subject. 11.3 Where source documents are stored elsewhere, make a copy for the research record, or place a note to file stating where the source document is kept. Note that for records stored elsewhere: retention and retrieval of records must be considered for document storage following the close of the study. 11.4 When study subject charts are kept in a clinical or hospital setting apart from the research office, then prominently marking the chart for return to the PI may prevent confusion with patient charts. RELATED FORMS: FORM CT-011 FINANCIAL DOCUMENTS BINDER CHECKLIST FORM CT- 012 CRITICAL DOCUMENTS BINDER CHECKLIST FORM CT- 014 SAMPLE SOURCE DOCUMENT MATRIX FORM CT- 013 CRFS AND SOURCE DOCUMENTS BINDER CHECKLIST FORM CT- 015 Note to File Format SET-UP OF THE STUDY FILES AND REGULATORY BINDER CT 007 REV.00 37 SAMPLE SOPS Implementation/Revision Dates: Last Review Date: Approval Signatures: Effective Date: SET-UP OF THE STUDY FILES AND REGULATORY BINDER CT 007 REV.00 38 SAMPLE SOPS CT 008 MANAGEMENT OF CASE HISTORY RECORDS & SOURCE DOCUMENTS PURPOSE: An investigator is required to prepare and maintain adequate and accurate documentation that records all observations and other data pertinent to the investigation for each individual participating in the study. Prior to subject enrollment, source documents must be identified or designed to acquire essential data for capturing subjects’ study activity. Case report forms (CRFs) are a common tool for capturing study data and provide a means to organize Sponsor reporting. CRFs are used in a study is to collect/coordinate necessary information about: the study subject(s) the administration of the study drug. the outcome of the assessments. SCOPE: Case histories are those essential documents that individually and collectively permit evaluation of the conduct of a trial and the quality of the data produced. These documents serve to demonstrate the compliance of the investigator, Sponsor, and monitor with the standards of GCP and with all applicable regulatory requirements. Additionally, these documents demonstrate the investigator’s adherence to the study protocol. Case histories contain all the information related to a participant’s protocol participation; they include the case report forms and supporting data ( i.e. signed and dated consent forms; and medical records such as progress notes of the physician, the individual’s hospital chart(s), and the nurses’ notes). Source documents frequently comprise a part of the medical record whereas a CRF is always a research document; even when a CRF is used as a source document, it is never part of the medical record. Those research study source documents that are part of a patient’s medical records should be clearly indicated in the study protocol. Note: there are inherent difficulties in totally depending on Emory HealthCare medical records as repositories for study related data since records retention requirements differ between medical records and research requirements. Original source documentation may legitimately be discarded from a medical record if it is not approved by the Documents Committee for inclusion in the MR. Any such source documents must be kept in the case history files to ensure proper ongoing retention. Worksheets, data management forms and source documents should be identified and clearly distinguished before subject enrollment. Proposed CRFs should be designed and reviewed for simplicity, clarity and ease of use; transcription should be minimized. Difficulties encountered in CRF use must be reported to the Sponsor; retain a copy of such reports and document any followup or corrective action taken. All personnel permitted access to the research study files must follow this SOP. The study Sponsor is responsible for the design and preparation of the CRF. Whenever possible, at least one member of the research team should review the proposed CRF. PROCEDURE MANAGEMENT OF CASE HISTORY RECORDS & SOURCE DOCUMENTS CT 008 REV.00 39 SAMPLE SOPS 1. The CRF should generally be a stand-alone document, typically providing the summary or collation of data from original source documents. 2. A CRF is designed for collecting data pertaining to the study objectives as defined by the protocol. 2.1 Information such as subject number, demographics, medical history and measurements of efficacy and adverse events are recorded on the Case Report Form at the site by investigator, sub-investigator or study coordinator as delineated in the study responsibilities log. 2.2 Study subject documents filed separately from the CRF should be identified and an entry made in the CRF detailing where the source data is stored. 2.3 When the CRF contains the first place an original observation is recorded, that information must be signed and dated by the original observer/recorder. Data originally recorded directly on the CRFs is source data (where there is no prior written or electronic record of data). 3. The finished CRF should be as easy to complete as possible. 3.1 CRFs should capture only essential information 3.2 CRF design should limit PHI entry to the minimum possible. 3.3 Data entry should follow a logical sequence. 3.4 The need to transcribe data should be minimized. RELATED FORMS FORM CT- 09 CASE REPORT FORM (CRF) REVIEW CHECKLIST Implementation/Revision Dates: Last Review Date: Approval Signatures: Effective Date: MANAGEMENT OF CASE HISTORY RECORDS & SOURCE DOCUMENTS CT 008 REV.00 40 SAMPLE SOPS CT 009 CASE REPORT FORM (CRF) COMPLETION, CORRECTIONS, HANDLING QUERIES PURPOSE: To describe the procedure for completing, signing and correcting case report forms in order to ensure that quality data is captured on the CRF and to describe the procedure of reconciling the copy of the CRF at the study site with the Sponsor's database. SCOPE: The data from the CRFs is the basis for the trial report, regulatory submissions, and for publications and should be completed as soon as possible after the subject assessment or test results are available. Improper, inadequate or ambiguous entries in CRFs identified during the data entry process generate a query to request clarification or explanation of such unclear or unexpected entries. These responsibilities must be identified and assigned in the study responsibilities log. PROCEDURE 1. The research staff member assigned in the study responsibilities log will complete each subject's CRF when the information becomes available. This may consist of original data entry or transcription of the appropriate data from the source documents. Only authorized study staff can make CRF entries and/or corrections. DO NOT ALLOW the Clinical Monitor/Sponsor to make entries or corrections in the CRF. 2. Supply all information requested on a CRF. 2.1. Do not leave blank spaces. 2.2. Ensure legibility of all data entries. 2.3. Explain corrections if the reason for the change is not obvious. 2.4. All data entered in a CRF should be understandable: i.e. use adequate units of measure for laboratory results, indicate and document when transformation of units has taken place, use only codes which have been predefined by the Sponsor. 2.5. Supply the reason for missing data, i.e. “test not performed”, “test results missing”, etc.; avoid using an ambiguous phrase such as 'not available'. 3. CRFs are the principle means of data transfer from the study site to the Sponsor. 4. 5. 6. 7. 8. 3.1. The most recent CRF version must be used for the current subject activity. 3.2. CRFs should be completed concurrently with or as soon as possible after the subject assessment or results are available; with the expectation for completion within one business day. 3.3. Use of PHI of subjects in the study shall be limited to the greatest extent possible. The PI must keep a SEPARATE record consisting of the subject's full name and the subject code number This PI record must be archived by the PI after completion of the trial. 5.1. Original source documents for medical care, treatment that is standard of care, will be kept in the subject's medical chart. A separate folder for each subject may be created. Any worksheets used for the study should be retained with the CRF. Minimize use of PHI on CRFs. CASE REPORT FORM (CRF) COMPLETION, CORRECTIONS, HANDLING QUERIES CT 009 REV.00 41 SAMPLE SOPS 9. Especially delete PHI from material faxed or sent to the Sponsor or on copies taken off site by the monitor. 9.1. Ensure CRFs are up to date prior to a scheduled monitor visit. 10. Include comment(s) on abnormal or unexpected results in the CRF. 10.1. Comment on laboratory values (and any action taken) outside the laboratory's reference range or some other range agreed upon with the Sponsor 10.2. Comment if a value (and any action taken) shows significant variation from one assessment to the next, and explain on the CRF. 10.3. Comment on all events (an event is a change from initial baseline results). 11. The CRF should be able to verify that all study activities are accomplished according to the protocol and FDA regulations. 11.1. Data transcribed to the CRF are supported by source documents. 11.2. Protocol deviations are noted in the CRF and/or source document. 11.3. The CRFs must be signed where indicated by the Principal Investigator to indicate that PI has reviewed the information for completeness and accuracy. 12. Investigator site data is transferred to the Sponsor according to the Sponsor agreement. A query will be sent by the Sponsor to the investigative site if inconsistencies or unclear items are found in the investigator supplied data. 12.1. Corrections or addendums to a CRF resulting from a query must be explained. 12.2. Corrections and changes to the CRF must be transmitted to the Sponsor so that the Sponsor data continuously agrees with all data at the investigative site. 13. Early query resolution should limit repetition of the same query from the Sponsor or permit clarification of procedures or data capture by the investigative site. 13.1. The PI or designee must promptly follow up on all requests for corrections or clarifications of data. Queries should be addressed within one week of receipt. 13.2. Ensure query responses are up to date prior to a scheduled monitor visit. 13.3. Review all queries & responses with the monitor. 14. The investigator is to maintain copies of CRFs/research records, according to the Emory University records retention policy and the agreement with the Sponsor, even though the research Sponsor may have the (original) records. 14.1. CRFs are part of the clinical study, property of the study Sponsor. Usually, the originals are maintained by the Sponsor after study close-out/termination. 14.2. Copies must be retained at the research site for the document retention period. Refer to Emory records and information management schedule at http://records.emory.edu/ RELATED FORMS Implementation/Revision Dates: Last Review Date: CASE REPORT FORM (CRF) COMPLETION, CORRECTIONS, HANDLING QUERIES CT 009 REV.00 42 SAMPLE SOPS Approval Signatures: Effective Date: CASE REPORT FORM (CRF) COMPLETION, CORRECTIONS, HANDLING QUERIES CT 009 REV.00 43 SAMPLE SOPS CT 010 CONTROL & ACCOUNTABILITY OF TEST ARTICLE PURPOSE: The purpose of this procedure is to delineate requirements for control and recordkeeping of inventory of test articles. SCOPE: THIS SOP covers control and recordkeeping of test articles obtained for use in human subjects’ research. “Test article” includes the investigative product(s) (drug or device) that is the object of the investigation, placebo(s) and/or comparator(s) used in the clinical study. NOTE: All investigational drugs or drugs that are provided free of charge by an external entity in human subjects’ research at Emory Facilities shall be managed according to the Emory University Investigational Drug Service (IDS) policy, available on the Emory policies website: http://policies.emory.edu/7.14 .This policy may permit an exception to the use of the IDS, refer to §7.14-D, using the “IDS Exception Request Form”. Inventory and accounting for medical device test articles must be managed by the PI; Policy 7.14, Investigational Drug Management for Clinical Studies, does not apply to a test article that is designated as a medical device. This applies to the clinical investigator and to delegated staff responsible for control or inventory management of any test article. PROCEDURE 1. An investigator shall permit an investigational product to be administered or used only by subjects under the investigator’s personal supervision. 1.1. The PI may delegate a qualified subinvestigator, who is responsible to the investigator, to administer or dispense the test article. 1.2. The investigator/subinvestigator must be permitted/licensed in accordance with state law to dispense, apply or administer the test article. 2. The investigator should ensure that the investigational product(s) are used only in accordance with the approved protocol. An investigator shall not supply or dispense a test article to any person not authorized to receive it. The test article may ONLY 2.1. be used in accordance with the specific protocol. 2.2. be provided to persons participating in the study. 3. Upon completion or termination of the investigator’s part of an investigation, or at the Sponsor’s request, an investigator shall return to the Sponsor any remaining supply of the test article or otherwise dispose of the test article as the Sponsor directs. 4. Investigators should maintain records that document adequately that the subjects were provided the test article/doses specified by the protocol. 4.1. The investigator, or a person designated by the investigator/institution, should explain the correct use of the investigational product(s) to each subject and should check, at intervals appropriate for the trial, that each subject is following the instructions properly. CONTROL OF TEST ARTICLES CT 010 REV.00 44 SAMPLE SOPS 4.2. The PI must maintain accountability records for test articles provided by the IDS to the study staff for administration or dispensing to subjects. Quantity, lot number, etc., of test article dispensed to or received back from individual subjects must be recorded, and records maintained according to study protocol. 5. For test articles not controlled by the IDS, the PI is responsible for full accountability and record keeping of receipt, dispensing and return of all test articles. 5.1. Proper storage conditions and security must be defined, controlled and verifiable. 5.2. The investigator shall ensure that records are kept of the receipt and the use/disposition of the test article. These records should include dates, quantities, batch/serial numbers, expiration dates (if applicable), and the unique code numbers assigned to the investigational product(s) and trial subjects. Records should relate to: 5.2.1. Delivered to the trial site: type and/or quantity of test article with dates of its receipt, and the batch number or code mark. 5.2.2. Use by each subject: type and/or quantity of test article supplied to and/or returned from each study participant, including date and batch/lot number. 5.2.3. Inventory, storage and destruction/disposition, to reconcile all investigational product(s) received from the Sponsor. 5.2.4. Return and reconciliation of unused drug from a study subject must be documented according to the investigator’s agreements 6. If the investigational drug is subject to the Controlled Substances Act, DEA regulations apply. The PI shall ensure adequate precautions to prevent theft or diversion, and ensure compliance with requisite controls for inventory tracking, access, and disposal. RELATED FORMS Form CT- 018 DISPENSING LOG TO STUDY SUBJECT FORM Implementation/Revision Dates: Last Review Date: Approval Signatures: Effective Date: CONTROL OF TEST ARTICLES CT 010 REV.00 45 SAMPLE SOPS CT 011 SUBJECT SCREENING AND ENROLLMENT PURPOSE: Describes the procedures used by a clinical investigative team to identify qualified subjects for a trial, in order to substantiate the efforts made to foster ethical and scientific choice of enrollment. SCOPE: All clinical studies using human subjects conducted by Emory staff or using Emory facilities should maintain a subject screening and enrollment log and apples to all investigators who are conducting clinical trials. The investigator may appoint research staff to coordinate and record subject recruitment screening information. Note: This SOP does not cover screening logs of the Emory Health Connection; nor other general format screening efforts prior to the information list’s transfer to a principal investigator. PROCEDURE 1. The exact procedure for subject recruitment should be detailed in the study protocol. 1.1. All advertisement material must be approved by the IRB. 1.2. Study should be registered with the Emory Health Connection. 1.3. Recruitment and screening activities must be budgeted for cost and time. 1.4. Preparation of a flowchart helps assure that informed consent process is initiated prior to any specifically directed study related activities. (refer to Form CT- 016 Screening and Enrollment Log) 2. Every individual considered as a potential candidate for the study should be entered on the “screening log” or “screening and enrollment log”. 2.1. A HIPAA waiver approved by the IRB may be required prior to recruitment and/or screening. 2.2. Determine availability and suitability of candidates using HIPAA permitted review of records based on the protocol eligibility criteria. 2.3. All potential subjects identified should be entered on the log without consideration of how likely you believe them to volunteer. Reminder: HIPAA waiver from the IRB is sufficient for records review to screen potential subjects, but no research related testing is permitted without consent. Informed consent from a research subject must be obtained before participation in any screening tests that are not required for patient care. SUBJECT SCREENING AND ENROLLMENT CT 011 REV.00 46 SAMPLE SOPS 3. For each person considered a potential candidate for the study, enter the following information on the screening log: Subject initials Remember that all of this information is Date of birth considered PHI and is subject to HIPAA. Date screened Screening number assigned, Subject number or study identifier if enrolled, Reason for declining if not enrolled, when provided. 4. Screening and enrollment information should be retained by the PI. 4.1 De-identified information should be shared with the study Sponsor. 4.2 Identifiable records should be confidential to the study site. 4.3 A HIPAA waiver (from IRB) or authorization (from subject) must be obtained to share PHI with a study Sponsor or others outside of the HIPAA authorized uses within a covered entity. 5 Master enrollment information should be retained by the PI. (refer to Form CT-017 Master Subject Log) 5.1 De-identified information may be shared with the study Sponsor. 5.2 A HIPAA waiver or authorization must be obtained to share PHI with a study Sponsor or others outside of the covered entity. 5.3 ERMS should be used to produce reports. RELATED FORMS FORM CT- 016 SCREENING AND ENROLLMENT LOG FORM CT- 017 MASTER SUBJECT LOG Implementation/Revision Dates: Last Review Date: Approval Signatures: Effective Date: SUBJECT SCREENING AND ENROLLMENT CT 011 REV.00 47 SAMPLE SOPS CT 012 INTERACTIONS WITH THE INSTITUTIONAL REVIEW BOARD (IRB) PURPOSE: To assure the ethical review and continuing oversight of clinical trials conducted by or for Emory University personnel or using Emory University facilities. Refer to the Emory IRB website at http://www.irb.emory.edu/researchers/res_index.cfm, and to the Emory University Institutional Review Board Policy & Procedure (P&P). SCOPE: This SOP covers all clinical trials at Emory; an authorized IRB must approve all research using human subjects. Written approval is needed before starting research activity. Research activities include screening, planned ‘wash-out’/medication change, exposure to an investigational agent, or any study related interactions, tests or procedures. This procedure applies to all Emory investigators who are conducting clinical trials. While the investigator may appoint research staff to coordinate and manage IRB communications, the PI retains responsibility for both content and timeliness of all IRB submissions including approval, renewal, personnel or protocol changes, and reporting. PROCEDURE 1. IRB approval must be granted prior to subject recruitment or enrollment. 1.1. All human subject research must be conducted according to an IRB approved protocol. 1.2. All studies using human subjects conducted by Emory staff or using Emory facilities must be submitted to the Emory IRB. 2. Study submissions will be reviewed either through the Emory IRB, or the Western Institutional Review Board (WIRB). Refer also to the Emory IRB website. 3. While the PI may delegate responsibilities to specified study personnel for study preparation and management of communications with the IRB, the PI is the only person authorized to submit study documents to the IRB, including, a study application, renewal, amendment, adverse event report or termination/close-out. Eligibility and Use of the WIRB 1. New Phase III studies will be sent to WIRB for review where the study is industry designed, initiated, Sponsored and funded. (http://www.irb.emory.edu/researchers/wirb/wirb.cfm) 1.1. The PI must submit Form A (WIRB Eligibility Checklist) to confirmation of the study’s WIRB eligibility. 1.2. For WIRB eligible studies, send Form B to the Emory IRB for processing and shipping the initial application to WIRB. Timelines, forms and supporting documents are delineated on the Emory IRB webpage. the Emory IRB for 2. During the trial the investigator must provide to the WIRB all required documents. 2.1. Emory will not be the IRB of record for these studies. INTERACTIONS WITH THE INSTITUTIONAL REVIEW BOARD CT 012 REV.00 48 SAMPLE SOPS 2.2. All communication regarding a study reviewed by the WIRB will be between the PI and WIRB. Emory IRB 3. Studies approved prior to eIRB implementation may still use paper documentation rather than electronic. Refer to http://www.irb.emory.edu/ 4. The PI is the only person authorized to make study submissions in eIRB. 4.1. The PI is responsible for the content, accuracy and timeliness of submissions to the IRB. 4.2. Clearly formulate the experimental design and the planned implementation of the experimental procedure(s) in the protocol transmitted for IRB review. 4.3. Use Emory IRB forms and electronic paths for submissions 5. The PI’s departmental reviewer must approve an initial study application submission. Any IRBs 6. During the trial the investigator must provide to the IRB all required documents subject to its review. 6.1. IRB must approve consent form or protocol changes prior to implementation. 6.2. Required documentation to the IRB may include: 6.2.1. Personnel changes 6.2.2. Modification or amendments to protocol 6.2.3. Changes to consent/assent, advertisements 6.2.4. Reportable events 6.2.5. Protocol deviations 6.2.6. Study termination /closeout 7. Prior to initial clinical trial submission, the PI or study coordinator should: 7.1. Define with the Sponsor what if any administrative or financial support will be provided for the study’s IRB oversight. 7.2. Obtain the IRB membership letter and/or DHHS assurance and registration number. For the Emory IRB, this information is available from the Researcher section under the “Forms & Tools” listings. 7.3. Prepare the informed consent document using the Emory template and guidance (refer also to CT 013 “Informed Consent Process”). Obtain the Sponsors “sign off” of the ICF final draft. Sending the Sponsors an unrevised consent template is not acceptable. 8. Follow submission instructions using the IRB submission process. 8.1. All new submissions to the Emory IRB are done through the eResearch portal. Required information includes current: 8.1.1. version of the protocol, 8.1.2. most recent version of the Investigator's Brochure (IB), 8.1.3. ICF draft that has been reviewed by the Sponsor, INTERACTIONS WITH THE INSTITUTIONAL REVIEW BOARD CT 012 REV.00 49 SAMPLE SOPS 8.1.4. copy of advertisements (specify website listings if appropriate, print media, radio ads etc), subject diaries, recruitment scripts, or other subject information sheets. 8.2. Resolve issues or recommendations for improvement identified by the IRB on a point by point basis within specified time period as allowed by IRB for return to the appropriate committee 8.3. Provide certified foreign language translations for review/approval, when required, of the approved English version informed consent forms (information available on the IRB website). 8.4. Retain the written IRB approval notification with the approved documents. The approval must identify the trial and state the date and duration of the approval. 8.5. Document the Sponsor’s acceptance of the final IRB-approved consent form(s). 9. The investigator is not permitted to implement changes to the protocol without prior review and documented approval from the IRB, and agreement by the Sponsor, except where necessary to eliminate an immediate hazard(s) to trial subjects. 10. At study termination, the Principal Investigator will notify the IRB of the study's completion using the IRB Protocol Closeout/Termination Form. 10.1. Study termination or completion occurs when all study activity is concluded. 10.2. If there is any ongoing subject care/follow-up, data analysis, etc., the study is ongoing and must maintain approved status, including its periodic renewal. 11. The Reg. Binder should be kept current regarding communications with the IRB. 11.1. Maintain copies of all correspondence, e-mails, and telephone logs. 11.2. Retain copies of all reports submitted to the IRB; keep copies of response(s). 11.3. File initial and updates of the IRB membership roster or DHHS assurance. 11.4. Update file upon receipt of the written and dated approval from the IRB, including for: 11.4.1. the approved trial protocol, 11.4.2. original written informed consent form (with approval stamp and dates), 11.4.3. consent form updates or translations (with approval stamp and dates), 11.4.4. subject recruitment procedures (e.g., advertisements), and any other written information to be provided to subjects. 11.4.5. HIPAA authorization form 11.5. Ensure that all documents contain identifying information, especially for dates or version numbers of an approved document. RELATED FORMS FORM CT- 019 CHECKLISTS FOR IRB OVERSIGHT Implementation/Revision Dates: Last Review Date: Approval Signatures: INTERACTIONS WITH THE INSTITUTIONAL REVIEW BOARD CT 012 REV.00 50 SAMPLE SOPS Effective Date: INTERACTIONS WITH THE INSTITUTIONAL REVIEW BOARD CT 012 REV.00 51 SAMPLE SOPS CT 013 INFORMED CONSENT PROCESS The Emory Institutional Review Board (IRB) Policy and Procedures (P&P) must be followed, especially §43, “Informed Consent”. PURPOSE: To establish procedures for obtaining and documenting informed consent. Each potential subject, or their legally authorized representative (LAR), must provide legally effective informed consent prior to joining a research study, unless otherwise permitted by the IRB. SCOPE: This Standard Operating Procedure (SOP) covers the responsibilities of the Principal Investigator (PI), and study team members to whom the PI has delegated informed consent process duties. PROCEDURE 1. FOLLOW THE IRB P&P FOR INFORMED CONSENT AND THE STUDY SPECIFIC PROCESS APPROVED BY THE IRB. 1.1. Use the most recent IRB-approved consent version. 1.2. Give the subject a copy of the consent document. 1.3. The following individuals should perform the consent process (a) the PI or (b) a person who is: 1.3.1. qualified to explain the protocol, and the medical procedures, and 1.3.2. formally delegated this responsibility by the PI. 1.3.3. If the person who presents the consent is not a physician, s/he will ensure that an authorized medical practitioner is available to answer the potential subject's questions as necessary. 1.4. The person obtaining consent must make sure that: 1.4.1. The subject's questions are answered. 1.4.2. The subject appears to understand the study requirements; the risk/benefits; and the fact the study is an experiment, not treatment. 1.4.3. The subject signs and dates the consent document voluntarily, and understands he/she may withdraw from study participation at any time. 1.4.4. The subject makes no changes to the Informed Consent Document (ICD). 1.4.5. All signature/initial lines/boxes on the ICD have been appropriately completed. 1.4.6. A copy of the ICD is provided to the subject; if possible the copy provided should be of the fully signed ICD. NOTE: a patient declining to participate in the research study must still be offered a copy of the (unsigned) ICD. 2. The signed original ICD must be kept in the research study file. It should be retained with the study documents for the duration of record retention period. INFORMED CONSENT PROCESS CT 013 REV.01 52 SAMPLE SOPS 3. DOCUMENTATION OF INFORMED CONSENT PROCESS 3.1 Document the following steps in a clinic note, progress note, or other source document: that the PI or person obtaining consent explained the study (include who explained, where, when), any questions were answered, the subject was given adequate opportunity to consider all available options, the subject agreed to participate. the date and time signed. A notation of the time is especially important when consent is obtained the same day that randomization/enrollment occurs. that a copy of the signed consent form was given to subject. 3.2 A template or detailed informed consent checklist incorporating the items above can be used to document the informed consent process. For an example see Form CT-20 Informed Consent Process Documentation. 4. REVISIONS TO THE ICD 4.1 When the Investigator receives updates to the Investigator's Brochure, IND Safety Reports, or protocol amendments, s/he should also review the informed consent to determine if it should be revised. 4.2 IRB approval of the revised ICD must be received prior to implementation. 4.3 A subject must be re-consented if changes to the ICD indicate a change in the risk-benefit ratio or new risks. 4.3.1 Explain any ICD changes to the subject at the next contact. In some situations, with IRB approval, the revised consent document may need to be mailed to the subject. 4.3.2 A copy of the revised consent must be provided to each study subject. This copy will be unsigned if the subject declines to continue as a study participant. 4.3.3 To continue in the study, the subject must voluntarily agree to the revised consent. Subject, person presenting the consent, and any required witness must sign & date the revised consent. Provide the subject with a copy of the revised consent and place the original signed revised ICD in the study file. Retain earlier, superseded signed forms. 4.4 If the PI/Study Coordinator discovers that an outdated or inappropriate version of the consent form was used for a subject still actively participating in the trial, s/he will: 4.4.1 Contact the subject and explain changes in the ICD to the subject. 4.4.2 As soon as feasible, have the subject sign the correct version, if the subject wants to continue to participate. 4.4.3 Instruct the subject to use the present date when signing the correct version. 4.4.4 A copy of the signed correct consent version must be provided to the subject. INFORMED CONSENT PROCESS CT 013 REV.01 53 SAMPLE SOPS 4.4.5 Maintain both signed versions of the ICD in the files. 4.4.6 Write an explanatory memo to the file so that future auditors will understand why two signed informed consent documents for the same subject are present in the file. If the study staff can’t contact the subject, the memo should also document the dates and methods by which the attempts to reach the subject were made. 4.4.7 Notify the IRB of non-compliance, according to standard reporting process. 5. When a minor subject turns 18, he/she should sign a consent form if an assent form had been used to enroll the subject as a minor. RELATED FORMS: Form CT-20 Informed Consent Process Documentation Implementation/Revision Dates: Last Review Date: Approval Signatures: Effective Date: INFORMED CONSENT PROCESS CT 013 REV.01 54 SAMPLE SOPS CT 014 MONITORING AND AUDIT VISITS PURPOSE: To describe the activities associated with periodic site visits or audits. SCOPE: This SOP applies to all clinical studies using human subjects conducted by Emory staff or using Emory facilities The PI may appoint research staff to coordinate and interact with study monitors and auditors. PROCEDURE Monitoring: The act of overseeing the progress of a clinical trial, and of ensuring that it is conducted, recorded, and reported in accordance with the protocol, standard operating procedures (SOPs), Good Clinical Practice (GCP), and the applicable regulatory requirement(s). Auditing: A systematic and independent examination of trial-related activities and documents to determine whether the evaluated trial-related activities were conducted, and the data were recorded, analyzed, and accurately reported according to the protocol, sponsor's SOPs, GCP, and the applicable regulatory requirement(s). 1. Monitor’s site visit (routine) 1.1. Prior to a monitor visit, the study coordinator will: 1.1.1 Prepare a list of questions related to the study. 1.1.2 Ensure all original signed informed consent documents are available. 1.1.3 Ensure all CRFs are complete and signed. 1.1.4 Ensure the appropriate documents are filed in the Regulatory Documents binder. 1.1.5 Ensure specific CRFs and source documents that will be reviewed are available on the visit date. 1.1.6 Set up appointments for the monitor to meet with the pharmacist and the PI. 1.2. Prior to a monitor visit, the PI will: 1.2.1. Review data collected and sign CRFs for completed subjects. 1.2.2. Prepare a list of questions related to the study. 1.3. During the site visit: 1.3.1. The study coordinator will ensure that the monitor signs the Monitoring log. 1.3.2. PI and study coordinator will interact with the monitor to help validate data in the CRFs; answer questions about the data or regulatory documents. 1.3.3. PI and study coordinator will follow-up on data clarifications. 1.3.4. PI and study coordinator will meet with the Monitor to discuss findings. 1.4. Following a monitor visit: 1.4.1. The PI and others as per delegation log will resolve monitor’s findings. 1.4.2. Establish and retain records of the visit, the findings, the resolutions and/or corrective actions to findings, including correspondence with the monitor/sponsor. MONITORING AND AUDIT VISITS CT 014 REV.00 55 SAMPLE SOPS 2. For a Sponsor audit or an FDA inspection (audit) Refer to the “Guidelines for an FDA Inspection” on the ORC website: http://www.orc.emory.edu/orc_documents/glinesfoFDAinsp41409.doc and to the “AUDIT PREPARATION CHECKLIST” follow link on the ORC website: http://www.orc.emory.edu/Clinical_Trials/index.cfm NOTE: Notify Emory’s Office of Research Compliance (ORC) and Office of General Counsel (OGC) immediately if an FDA investigator arrives at your site unannounced or the reason for the inspection is “directed” (i.e., for cause). 2.1. When the auditor calls, obtain details of the planned audit. 2.2. Notify appropriate Emory offices, including department, research administration and support units (i.e ORC, OCR, IRB, medical records). (SOP should list units to notify.) 2.3. Arrange for rooms, staffing for visit duration. 2.4. Study coordinator should organize and review study documents, review with PI, and arrange for an internal review of study & documents with ORC. 2.5. For an FDA inspection (only), PI should prepare a: 2.5.1. List of all clinical trials for which PI has been the primary investigator. 2.5.2. Summary of the trial and the PI’s responsibilities in it. RELATED FORMS FORM CT- 024 MONITORING LOG FDA REFERENCES “Information Sheet Guidance for IRBs, Clinical Investigators, and Sponsors FDA Inspections of Clinical Investigators” http://www.fda.gov/downloads/RegulatoryInformation/Guidances/UCM126553.pdf “Bioresearch Monitoring - Clinical Investigators and Sponsor Investigators” Guidance for FDA Staff, issued December 8, 2008 http://www.fda.gov/ICECI/EnforcementActions/BioresearchMonitoring/ucm133562.htm especially Part II Implementation, and Part III Inspectional Implementation/Revision Dates: Last Review Date: Approval Signatures: Effective Date: MONITORING AND AUDIT VISITS CT 014 REV.00 56 SAMPLE SOPS CT 015 EVENT RECORDING, REPORTING REQUIREMENTS PURPOSE: TO describe the process used to elicit, record, and/or report events, including but not limited to unanticipated problems, adverse events, and deviations from a protocol. Timely and adequate reporting of events is necessary to promote the welfare of the individual research subject and the continued patient safety during use of a subsequently marketed product. This SOP provides guidance for event reporting. This SOP should be used in conjunction with the IRB P&P, especially §64 Investigator Reporting Obligations to IRB. Scope: All potentially related study events, propitious or adverse, both serious and non-serious, must be recorded in the research record - case report form or case history. Additional reporting of events may be required. Appropriate staff members should conduct study visits, assessments, etc., and ensure that all potentially related study events are discovered or comprehensively elicited. Each research team member in contact with a subject is responsible for documentation of events that are reported by the subject and making those known to appropriate staff (e.g. medical, nursing, research staff). The Principal Investigator is responsible for the accuracy, completeness and timeliness of records and reports. The PI should review all reports before signature or transmission. PROCEDURE 1. Document and evaluate all events, propitious or adverse, discovered by the study team during the study, protocol testing or as reported by the subject. 1.1. An adverse event may develop into a serious adverse event, or compiled records of seemingly unrelated symptoms may reveal statistically significant patterns in a greater population. 1.2. Adverse events ongoing at completion of the study should be followed up as clinically indicated and as required by the protocol. Capture resolution of the event in the research case history. 1.3. Develop a study-specific tracking system to ensure that reportable events are identified, evaluated by the PI, and reported, in a timely manner. 2. At each study visit or during evaluations/assessments, the responsible researcher must make a conscientious effort to elicit candid information of any events undergone by the subject since the previous visit or assessment. Document events as unambiguously as possible in the case history and CRF. 2.1. Help subject provide precise information; use the subject’s own words, then elaborate as needed for clarity. i.e. if the subject reports: “felt sick” elicit greater description of symptoms, such as upset stomach, queasy but not vomiting. “device failure” elicit greater description, such as description of inaccurate readings, battery life shorter than anticipated, etc. 2.2. Obtain date and duration, start/stop, of event or series of events. REPORTING SAFETY, AND ADVERSE EVENTS (AES) OR SAES CT 015 REV.00 57 SAMPLE SOPS 2.3. 2.4. 2.5. 2.6. Document severity using standard scales or as directed by the protocol. Document all treatment/medication provided and/or taken for the event. Document event followup and/or outcome. Track findings, evaluations and reports of events affecting subjects. 3. Notify the IRB of reportable events using the current submission/reporting process, according to the Emory IRB website. Follow the IRB P&P, especially §64 Investigator Reporting Obligations to IRB and §55 Complaints. 3.1. Reportable events/actions may include: adverse events, unanticipated problems (UPs), safety reports, protocol deviations, breaches of confidentiality or others. 3.2. Follow-up information for events should be reported as available. 3.3. Death of a subject at an Emory study site must always be reported to the IRB; study related deaths are to be reported promptly, unrelated deaths are reported in periodic summaries. 3.4. Forward to the IRB external unanticipated problems or safety reports to the PI from a Sponsor. Report promptly to the IRB: 3.4.1. DSMB reports that might alter risk assessment for study participants. 3.4.2. Sponsor reports to the PI of (external) unanticipated problems. 3.4.3. Any safety reports or new information that may indicate Altered risk profile, Considerations that may adversely affect the safety of the subjects or Considerations that may adversely affect the conduct of the trial. 3.5. The PI must report complaints that he/she receives from participants or others. 3.5.1. Report to the IRB those complaints that involve potential risks to participants or others, or that may change the risk/benefit ratio, within 10 calendar days of the PI/staff member’s receipt of the complaint. 3.5.2. Report complaints concerning subject rights submitted by subjects or concerned parties, family members, or study personnel. 3.6. Report proposed modifications to approved protocol via current notification process, including proposed changes to protocol or personnel. 3.6.1. Protocol modifications should be submitted to the IRB after the Sponsor has agreed to the change. 3.6.2. IRB must approve changes before implementation, except to immediately protect the health of a subject. Emergency change to the protocol to protect the health of the subject must be reported as soon as possible and no more than five working days after the occurrence. 3.7. In the periodic report/renewal submission to the IRB, report summaries of: 3.7.1. Findings from the Sponsor and/or external DSMBs, 3.7.2. External UPs. 3.7.3. Emory sites’ UPs and SAEs related to the research; subject deaths not associated with the protocol interventions. 3.8. Protocol deviations that affect the safety or wellbeing of a subject; refer also to next SOP, §016 Reporting Protocol Deviations. 3.9. Submit a final report to the IRB shortly (within 3 months) after termination or completion of the investigator’s part of the research. 3.10. Submit reports according to the timeframes mandated in the IRB P&P. REPORTING SAFETY, AND ADVERSE EVENTS (AES) OR SAES CT 015 REV.00 58 SAMPLE SOPS 4. Notify the Sponsor according to the contract, the protocol and applicable regulations. 4.1. SAEs 4.1.1. Immediately inform the Sponsor of an unanticipated SAE: within 24 hours of knowledge of the SAE by anyone on the investigative site team. An initial SAE report must include or be followed promptly by a detailed written report. 4.1.2. Promptly report anticipated SAEs, identified in the protocol or other document such as the Investigator's Brochure; these generally have a ten day report window, check your protocol and contract. 4.2. Safety Evaluations: Adverse events and/or laboratory abnormalities identified in the protocol as critical to safety evaluations should be reported to the Sponsor according to the reporting requirements and within the time periods specified by the Sponsor in the protocol. 4.3. In addition to reports, all events should have been captured in CRFs and case history records. 4.3.1. Such events include any untoward medical occurrence, including anticipated AEs, and AEs that appear unrelated to the study activities. 4.3.2. Analyses of data may disclose associations not previously anticipated. 4.4. Report to the Sponsor any change to the protocol. 4.4.1. Report promptly any emergency change to the protocol to protect the health of the subject, and no more than five working days after the occurrence. 4.4.2. Except in such an emergency, prior approval by the Sponsor is required for changes in or deviations from the approved plan. 4.5. The PI should periodically review the accumulated study-specific data tracking of the events & reporting in order to assess trends. 4.6. Notify the Sponsor within 5 working days if the IRB suspends or withdraws approval of the PI’s participation in the study. Refer to IRB P&P §58 Suspensions and Terminations of Previously Approved Research. 4.7. Submit a final report to the Sponsor shortly after termination or completion of the investigator’s part of the investigation, no more than 3 months later. 5. Notify subjects of: 5.1. Any suspension or termination of the study. 5.2. Findings or protocol changes that might alter the risk/benefit balance or the subject’s willingness to continue participation. RELATED LINKS Refer to the “Emory IRB Reportable Events Guidelines”: http://www.irb.emory.edu/researchers/formstools/docs/other/RepEventsGuidelines6192008.pdf §64 Investigator Reporting Obligations to IRB of the Emory IRB P&P Emory IRB Reportable Events Form: http://www.irb.emory.edu/researchers/formstools/docs/paper/Reportable%20Event%20Form.doc RELATED FORMS Form CT- 022 Adverse Event Log REPORTING SAFETY, AND ADVERSE EVENTS (AES) OR SAES CT 015 REV.00 59 SAMPLE SOPS Implementation/Revision Dates: Last Review Date: Approval Signatures: Effective Date: REPORTING SAFETY, AND ADVERSE EVENTS (AES) OR SAES CT 015 REV.00 60 SAMPLE SOPS CT 016 REPORTING PROTOCOL DEVIATIONS PURPOSE: To provide instructions for handing deviations from a clinical protocol, including tracking, correction and reporting of deviations. SCOPE: This SOP covers the responsibilities of the PI and responsible research staff in reporting protocol deviations. This SOP applies to all persons participating in the clinical trial at the investigative site, including the PI and all members of the research team. Study participants, study site staff, or the investigator could be the source of the noncompliance. All deviations from the protocol should be reported to the study coordinator for tracking. It is the responsibility of the PI in cooperation with the research team to identify, correct and prevent further deviations as they are detected. PROCEDURE 1. Except in emergency situations, a protocol deviation requires prior IRB and Sponsor approval. Prior FDA approval may be required for certain trials, if the deviation may affect the scientific soundness of the plan or the rights, safety, or welfare of subjects. 2. In an emergency, the investigator may implement a deviation from the protocol to eliminate an immediate hazard(s) to trial subject(s). Prior IRB approval is not required, but the deviation must be promptly reported: 2.1. To the IRB for review; 2.2. To the Sponsor, according to protocol or contract. Maximum permissible times given here may be reduced by the contract. 2.2.1. For a drug, must be reported within ten working days; and 2.2.2. For a device, the Sponsor must report to the FDA as soon as possible but no later than ONE week after the emergency occurs. 2.3. Submit a deviation report for a single occurrence: 2.4. If the deviation is likely to be repeated or ongoing, then the report to the IRB should be on the current form to propose a protocol amendment(s), including justification for the change to the protocol. 2.5. Reports to regulatory authorities are made by the IRB and/or the Sponsor. 3. The investigator, or person designated by the investigator, should document and explain any deviation from the approved protocol in the case report form, research notes or elsewhere that is readily retrievable/recognizable in the case history record. 4. Standardizing the process of detecting and tracking deviations should engender: 4.1. Early identification of deviation trends 4.2. Timely development of appropriate corrective action 4.3. Consistent reporting by site staff of protocol deviations; 4.4. More accurate statistical analysis of the protocol outcomes with integration of deviations data; 4.5. Followup of corrective action to evaluate effectiveness. REPORTING PROTOCOL DEVIATIONS CT 016 REV.00 61 SAMPLE SOPS 5. Promptly report substantive protocol deviations to IRB according to the IRB P&P and to the Sponsor according to the contract and the protocol. 5.1. Substantive protocol deviations are those that do any of the following: 5.1.1. Increases the risk to subjects. 5.1.2. Damages the scientific integrity of the data collected. 5.1.3. Affects the privacy of the subject. 5.1.4. Affects a subject’s willingness to participate in the study. 5.2. Deviation reports (also called “non-compliance reports”) should include: 5.2.1.1. What was violated – e.g. protocol requirement, IRB policy, procedure, law or regulatory requirement that was not followed, 5.2.1.2. Description or manner in which actions deviated from or failed to comply with requirement(s); include date and time of event, and of discovery of deviation, 5.2.1.3. Effect of the non-compliance, especially any effect on the subject, 5.2.1.4. Reason for the deviation, 5.2.1.5. Corrective action that will be taken to ensure such action is not repeated. 5.3. Refer to Form CT- 021, Protocol Deviations Lists of Examples. 6. Minor protocol deviations should be reported to the IRB at the time of continuing review submission. Reports of protocol violations should be submitted to the Sponsor according to the Sponsor’s protocol. 6.1. Minor protocol deviations do NOT result in a change in the: 6.1.1. protocol 6.1.2. consent form 6.1.3. risk/benefit ratio for the study. 6.2. Minor protocol deviations may become significant if: 6.2.1. Occurrence is frequent or persistent. 6.2.2. Evince willful or knowing misconduct on the part of the researcher. 6.3. Refer to Form CT- 021, Protocol Deviations Lists of Examples. 7. Study participants’ failure to follow the study design or procedures are deviations. 7.1. Subjects protocol deviations may include: 7.1.1. failure to attend scheduled visits 7.1.2. not complying with drug administration instructions 7.1.3. not completing a diary card. 7.1.4. failure to adhere to dietary or other instructions (e.g. limit alcohol intake, maintain exercise schedule) 7.2. The PI must determine if subject non-adherence results in either a significant or minor deviation. 8. Review deviations and formulate corrective action plans. 8.1. Review CRF and early study activities following enrollment of the first and/or second subject to ensure that the pattern of compliance is set and there are no misunderstandings of expectations from the monitor/Sponsor. 8.2. Review of specific deviation or non-compliance items and of tracked trends should be part of the research team meetings. 8.3. Determine if subject deviations can be controlled. REPORTING PROTOCOL DEVIATIONS CT 016 REV.00 62 SAMPLE SOPS 8.3.1. Evaluate if compliance can be improved through more careful supervision of the subject, better understanding of protocol activities, assistance from family members, etc. 8.3.2. Consistent or repeated non-compliance may require removal of the subject from the study for concerns of subject safety, data integrity or statistical validity. 9. Determine cause of deviations and institute corrective actions. 9.1. Protocol amendment may be required for non-compliance due to errors in study design or testing schedule. 9.2. Organizational aids or checklists for protocol activities, or instruction regarding protocol requirements may improve protocol compliance. 9.3. Additional staff may be needed to accomplish required tasks. 9.4. Followup and document corrective action. RELATED FORMS Form CT- 021 Protocol Deviations Lists of Examples Implementation/Revision Dates: Last Review Date: Approval Signatures: Effective Date: REPORTING PROTOCOL DEVIATIONS CT 016 REV.00 63