Thermal Radiofrequency Denervation of
advertisement
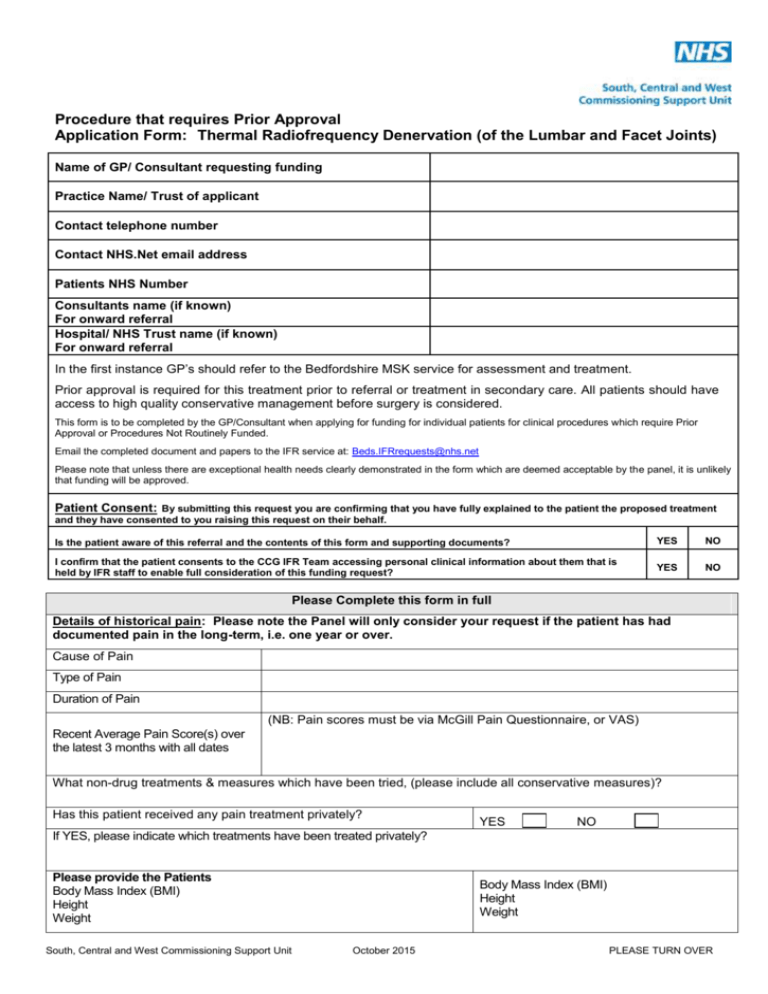
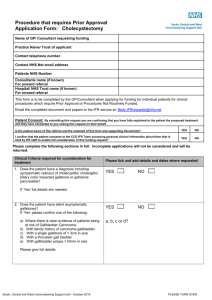
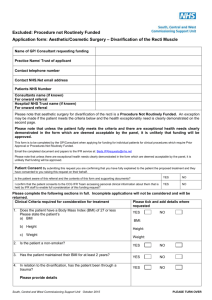
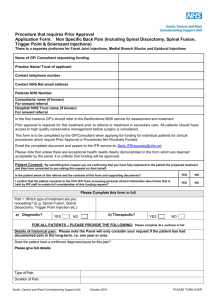
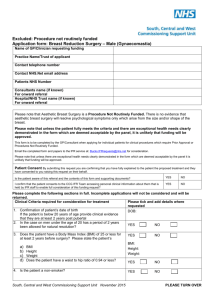
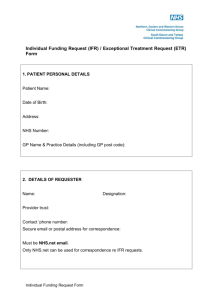
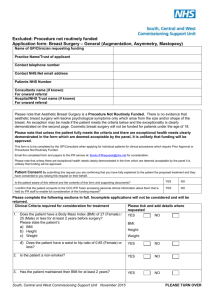
Procedure that requires Prior Approval Application Form: Thermal Radiofrequency Denervation (of the Lumbar and Facet Joints) Name of GP/ Consultant requesting funding Practice Name/ Trust of applicant Contact telephone number Contact NHS.Net email address Patients NHS Number Consultants name (if known) For onward referral Hospital/ NHS Trust name (if known) For onward referral In the first instance GP’s should refer to the Bedfordshire MSK service for assessment and treatment. Prior approval is required for this treatment prior to referral or treatment in secondary care. All patients should have access to high quality conservative management before surgery is considered. This form is to be completed by the GP/Consultant when applying for funding for individual patients for clinical procedures which require Prior Approval or Procedures Not Routinely Funded. Email the completed document and papers to the IFR service at: Beds.IFRrequests@nhs.net Please note that unless there are exceptional health needs clearly demonstrated in the form which are deemed acceptable by the panel, it is unlikely that funding will be approved. Patient Consent: By submitting this request you are confirming that you have fully explained to the patient the proposed treatment and they have consented to you raising this request on their behalf. Is the patient aware of this referral and the contents of this form and supporting documents? YES NO I confirm that the patient consents to the CCG IFR Team accessing personal clinical information about them that is held by IFR staff to enable full consideration of this funding request? YES NO Please Complete this form in full 1. Details of historical pain: Please note the Panel will only consider your request if the patient has had documented pain in the long-term, i.e. one year or over. a) Cause of Pain b) Type of Pain c) Duration of Pain (NB: Pain scores must be via McGill Pain Questionnaire, or VAS) d) Recent Average Pain Score(s) over the latest 3 months with all dates e) What non-drug treatments & measures which have been tried, (please include all conservative measures)? f) Has this patient received any pain treatment privately? YES NO If YES, please indicate which treatments have been treated privately? 2. Please provide the Patients Body Mass Index (BMI) Height Weight South, Central and West Commissioning Support Unit Body Mass Index (BMI) Height Weight October 2015 PLEASE TURN OVER 3. Is the patient a non-smoker? 4. Is the patient aged over 18? 5. Does the patient have non-radicular lumbar, facet or cervical pain? 6. Please give details: Does the patient have persistent symptoms despite non-operative treatments for at least 6 months? (e.g. optimum analgesia/ medication, physical therapy, bed rest etc.) YES NO YES NO YES NO YES NO YES NO Please give details: Does the patient have an average pain level of ≥6 on a scale of 0 to 10? Note: Levels of pain must be assessed using a validated tool e.g. McGill Pain Questionnaire, Pain Visual Analogue Score (VAS) Does the patient have radiological imaging ruling out any correctable structural lesion? Level: YES NO YES NO YES NO Please forward a copy of the radiological report (e.g. MRI) or give details: Has the patient had at least 2 anaesthetic diagnostic blocks, one of which must be of the medial branch of the dorsal ramus innervating the target facet joint with at least 80% reduction in pain? Please give full details: Does the patient have pain significantly affecting the activities of daily living? Full details must be given: What drugs have been tried for this condition? Drug Dose Date Started (approx) Date Stopped (approx) Outcome & Reason for Stopping/ Continuing – (e.g. state the side effect if it did not work, or reason for continuing) Why do you think this patient should be an exception to current policy or considered to have an exceptional health need for the intervention requested? (please see footnote for definition) South, Central and West Commissioning Support Unit October 2015 2 PLEASE TURN OVER : If funding is not approved what is the possible alternative treatment? SIGNATURE OF CLINICIAN ……………………………………………………………. DATE: ………………………………………………….. Exceptional Status (what makes the individual sufficiently different from the ‘usual’ in policy terms) Central to consideration of individual requests for funding is the concept of the case being exceptional. In order for funding to be agreed there must be unusual or unique clinical factors about the patient that suggest that they are: Significantly different to the general population of patients with the condition in question and likely to gain significantly more benefit from the intervention than might be expected from the average patient with the condition. However: The fact that a treatment is likely to be efficacious for a patient is not, in itself, a basis for an exception. If a patient's clinical condition matches the 'accepted indications' for a treatment that is not funded, their circumstances are not, by definition, exceptional. Social value judgements (the 'worth’ of patients) are not relevant to the consideration of exceptional status but there may rarely be exceptional circumstances where benefits may go beyond the patient (e.g. as a carer) in respect of social or health related benefits for others. Please email the completed form to Beds.IFRrequests@nhs.net for consideration. South, Central and West Commissioning Support Unit October 2015 3