Read Laura`s report
advertisement
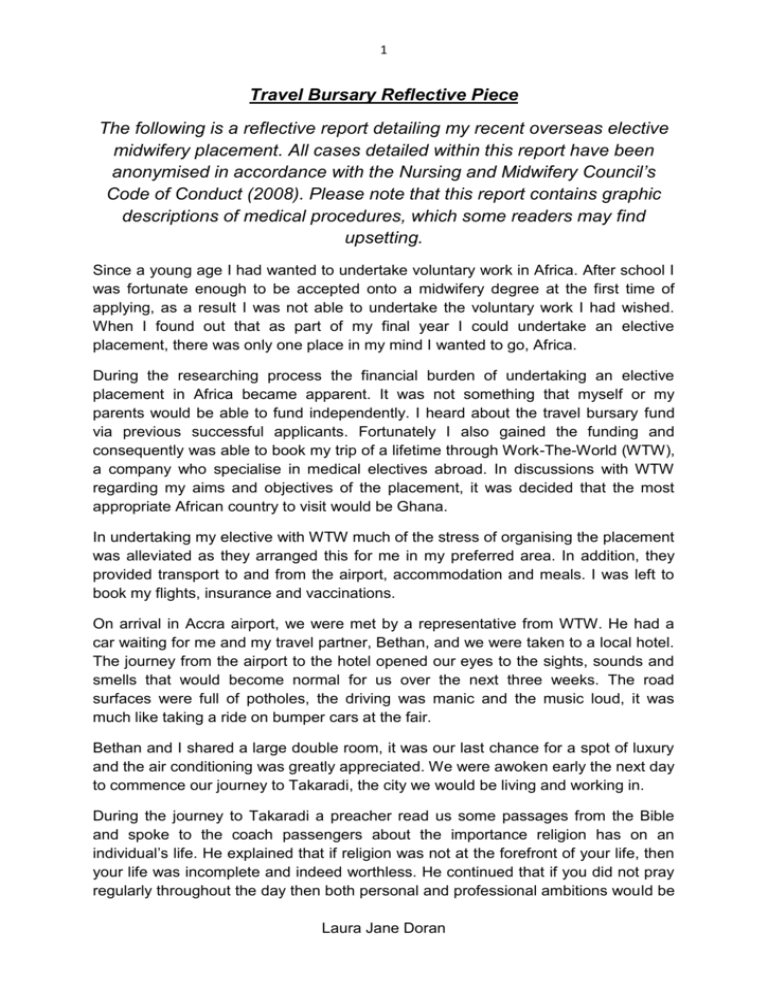
1 Travel Bursary Reflective Piece The following is a reflective report detailing my recent overseas elective midwifery placement. All cases detailed within this report have been anonymised in accordance with the Nursing and Midwifery Council’s Code of Conduct (2008). Please note that this report contains graphic descriptions of medical procedures, which some readers may find upsetting. Since a young age I had wanted to undertake voluntary work in Africa. After school I was fortunate enough to be accepted onto a midwifery degree at the first time of applying, as a result I was not able to undertake the voluntary work I had wished. When I found out that as part of my final year I could undertake an elective placement, there was only one place in my mind I wanted to go, Africa. During the researching process the financial burden of undertaking an elective placement in Africa became apparent. It was not something that myself or my parents would be able to fund independently. I heard about the travel bursary fund via previous successful applicants. Fortunately I also gained the funding and consequently was able to book my trip of a lifetime through Work-The-World (WTW), a company who specialise in medical electives abroad. In discussions with WTW regarding my aims and objectives of the placement, it was decided that the most appropriate African country to visit would be Ghana. In undertaking my elective with WTW much of the stress of organising the placement was alleviated as they arranged this for me in my preferred area. In addition, they provided transport to and from the airport, accommodation and meals. I was left to book my flights, insurance and vaccinations. On arrival in Accra airport, we were met by a representative from WTW. He had a car waiting for me and my travel partner, Bethan, and we were taken to a local hotel. The journey from the airport to the hotel opened our eyes to the sights, sounds and smells that would become normal for us over the next three weeks. The road surfaces were full of potholes, the driving was manic and the music loud, it was much like taking a ride on bumper cars at the fair. Bethan and I shared a large double room, it was our last chance for a spot of luxury and the air conditioning was greatly appreciated. We were awoken early the next day to commence our journey to Takaradi, the city we would be living and working in. During the journey to Takaradi a preacher read us some passages from the Bible and spoke to the coach passengers about the importance religion has on an individual’s life. He explained that if religion was not at the forefront of your life, then your life was incomplete and indeed worthless. He continued that if you did not pray regularly throughout the day then both personal and professional ambitions would be Laura Jane Doran 2 impossible to achieve. Initially I was shocked by the level of importance the preacher was placing on religion, but throughout my time in Takaradi I was able to understand the important role that religion plays for individuals and society. On an individual level religion enabled people to believe that the situation they were in would improve, whether it is in their current life or their afterlife. In addition, it gave people a reason to come together, to pray; sing and support one another. On a larger scale it was apparent that religion played a great part in social control. For example, people were too afraid to disobey the Ten Commandments, this is demonstrated in the low levels of crime within Takaradi. From my time on placement it was interesting to see how religion played an important part of the childbearing continuum. One particular moving aspect was during the postnatal clinic. The clinic is held every Wednesday and women must return on week 2, 4 and 6 postnatally with their baby to check their condition. Before the clinic starts all mothers sit together with their babies and sing and pray for half an hour to give thanks to God for the safe delivery of their child. In England, community postnatal clinics are just starting out, but women have individual appointments, so rarely mix. The postnatal clinic in Ghana allowed mother’s to come together, share experiences and bond, this process was initiated via prayers. Although in England often there is not the same emphasis placed on religion, the idea of a postnatal clinic being held in a setting were mothers can attend at any time, to allow them to meet one another and share experiences with others who have experienced similar things, is something that is extremely interesting to me, and something I hope to develop in my future practice. On our first Monday in Takaradi we were given an orientation to the hospital we would be working in. Before embarking on my journey to Ghana I undertook some research on what to expect from the hospital, I expected a decrepit unit and many patients, but no research or expectations could have prepared me for what I would see at the hospital. On our orientation we observed patients and relatives sleeping rough within the hospital grounds. Relatives were only allowed onto the wards during visiting hours, which were after 4pm. However, they had to do all cares for patients, provide all their meals and collect all their prescriptions from pharmacy. The nurses did very little ‘hands on’ nursing for patients. From observations the only real duties they performed involved dispensing medication and performing observations twice a day. During the orientation the standards of care we would see over the next 3 weeks were observed. Accident and Emergency consisted of two rooms, we observed 1 doctor, an emergency technician and numerous nurses, whom were all sitting around a desk laughing and joking. We observed A&E’s ‘waiting room’, which consisted of a wall outside, which was surrounded by patients, suffering from varied ailments. One particular image which will stay with me was that of one woman ‘unconscious’ (likely dead) in a ‘wheelchair’ (A garden chair with wheels attached to it) waiting to be seen, with her relative frantically trying to wake her. Although A&E Laura Jane Doran 3 was well staffed and had only one patient, there was no urgency, or in-fact interest from the staff to see any more patients, regardless of the severity of their condition. This lack of urgency was demonstrated throughout the placement, during numerous emergency situations staff seemed very blasé. It is something I still do not have a valid rationale for. From speaking to hospital staff and local people there were some suggestions that ‘it is too hot to rush’, which in a hospital which largely has no air conditioning and temperatures of up to 36* in the rainy season is reasonable. But in an emergency situation when a life is at risk, and can potentially be saved it is inexcusable. Initially I thought the lack of urgency may be due to a lack of knowledge surrounding emergency situations. However throughout the placement I repeatedly questioned the midwives on their theory and knowledge base and it was very much similar to that currently in the UK, as was the supposed treatment. In reality though, treatment and medical interventions were extremely slow, if at all, even where resources were available. From observations, although the nurse and midwives have the current knowledge base frequently the interventions performed were extremely outdated and unsupported by evidence. One particular case that that will never be forgotten was the case of ‘Paulina’ a 19 year old first time mother. She had progressed well throughout her labour and became fully dilated at around 14.00. Policies in both the UK and Ghana state low risk first time mothers should be given 1 hour for ‘descent’ of the fetal head after confirmation of full dilatation and then a further hour for pushing. In addition the fetal heart should be listened to every 5 minutes throughout this period. Although policies in the UK and Ghana are similar and when asked the midwives were aware of them, in practice they were completely ignored. During the case of Paulina, after confirmation of full dilatation she was transferred to the delivery room, where she was laid flat on her back with her legs in stirrups. Paulina was urged to push by both midwives attending delivery, however no guidance was offered on the best techniques and positions to push and facilitate delivery. At 14.10 Paulina was again encouraged to push, both midwives repeatedly slapped her legs and told her to ‘push properly’, but again never guided her. Myself and Bethan were demonstrating to Paulina the most effective ways to push in the position she was in, but we were shot down by the sister in charge. She then told Paulina that ‘her baby was dying and it was her fault because she was not pushing’, in addition she was asked ‘if that is what she wanted to happen?’ It was very shocking to hear, especially considering the fetal heart had not been listened to for over half an hour, so the condition of the baby was unknown. At 14.15, 15 minutes after confirmation of full dilation, scissors were prepared, in order to undertake an episiotomy. In the UK episiotomies are frequently performed under local anaesthetic when the fetal head is at the perineum but delivery is delayed because perineal tissues are firm. In giving an episiotomy for this reason it Laura Jane Doran 4 allows more room for the head and facilitates delivery. In the case of Paulina the head was still high in the pelvis and not near the perineum, this caused many complications, particularly a great blood loss. Paulina was given no pain relief throughout her labour or attempted episiotomies. In addition the midwife used blunt scissors and attempted to perform the episiotomy numerous times. The combination of the sound of the blunt scissors attempting the episiotomy and Paulina’s subsequent screams were the most horrific things I have experienced throughout my short midwifery carer. As the fetal head was still high in the pelvis when the episiotomy was performed it did not facilitate delivery of the head. Instead one midwife placed both hands inside the vagina, she stated she was “stretching the vagina and attempting to pull the baby out”. Whilst another midwife (who was in excess of 20 stone) sat on Paulina (a very slim girl) and placed pressure on the top of her uterus, she stated she was “trying to push the baby out’. Both aspects of practice are massively contraindicated and can have major negative complications for both mother and baby. When asked the midwives were aware of the contraindications but chose to perform the practices regardless. During the labour I got out a ‘bag and mask’ to resuscitate the baby should it need it once delivered. When the baby was born, there were again multiple demonstrations of bad practice, which I shall not go into detail about. But the baby was born in a poor condition and needed resuscitation. The midwife seemed to understand the baby needed resuscitation but was not very keen to perform it, I was trying to dry the baby and stimulate it and repeatedly suggesting to the midwife that she should start resuscitation. Eventually she obliged, I passed her the bag and mask, she put it down, went to a cupboard and came back with a cut off top of a coke bottle. She detatched the mask from the resus bag and attached the nozzle of the cut of bottle onto the bag and began to perform ‘resus’. Unsurprisingly the bottle top was not properly attached to the bag, as a result the pumped air was simply escaping and the baby was deteriorating. I asked the midwife if I could take over the resus attempts, she thankfully obliged. I reattached the mask and placed the baby in the correct position, after 15 minutes of resus, the baby had a good heart rate and good respirations. This ‘resuscitation’ attempt is one example of how midwives appeared to have the theory, knowledge and to a certain extent resources but choose not to utilise them. Although an appalling experience, I was able to improve my non communication skills. I tried to advise Paulina and comfort her throughout, even though we did not speak the same language. I was able to act as an advocate for Paulina and challenge the practice of senior staff; something I believe will give me confidence in my practice within the UK. In addition I was able to improve my skills in neonatal resuscitation – something I have had limited experience of in the UK. Laura Jane Doran 5 Throughout my time in Ghana the staff at WTW were fantastic. Within the house we had a project manager, who organised placements and accompanied us on our hospital orientation. We had a tourist guide, who gave us a local orientation, helped us organise weekend trips, activities and local visits, such as visiting an orphanage, in addition to facilitating weekly Fante lessons. We had a house keeper who cleaned the house each day and a cook who made us breakfast and an evening meal. In addition we had two security guards, who ensured we were living in a safe environment. Throughout my time in Ghana, I felt so well looked after by all the staff, we were able to contact them 24/7 with any issue we had. Both the WTW staff and the other students Bethan and I met during our elective were amazing and made our trip to Ghana extremely special!! As an organisation I cannot praise WTW highly enough and would definitely recommend them to any healthcare students wishing to travel abroad for an elective placement. Although at times this elective placement was extremely challenging, it was the best experience of my life. I feel I have developed both individually and professionally. I am a more confident individual and I hope this will be reflected within my future practice. I believe this elective placement has strengthened non-verbal communication skills in addition to my basic caring skills. I have recently gained a midwifery post in a multi-cultural city so I aim to utilise these newly strengthened skills within my practice, as I again may be caring for women were English is not their first language. In addition I feel I have more confidence in my own midwifery practice, this placement enabled me to relate theory to practice and I was able to identify deviations from normal parameters, although they were not always acted upon. One aspect of Ghanaian health care I hope to one day replicate in the UK is the idea of communal postnatal clinics. The idea of a postnatal clinic being held in a provision that has the facilities to provide a communal area and a private room. In doing this women still have their individual private appointments with their midwife but also have an opportunity to join together and share their birth, postnatal and feeding experiences. This is something I believe would benefit many women and something I hope to develop within my trust. I would like to take this opportunity to thank you for the funding provided as this trip would not have been possible without you, it is greatly appreciated and something I believe will shape the rest of my personal and professional life. Laura Jane Doran