CCRR Data Dictionary - Canadian Association of Cardiovascular
advertisement

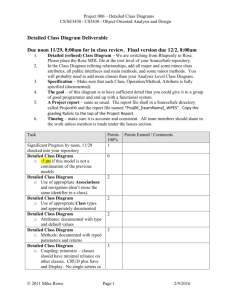
DATA ELEMENT D E F I N I T I O N S 2.0 February 9, 2016 Copyright © Canadian Association of Cardiovascular Prevention and Rehabilitation 2014 To be used with permission only. Not for re-distribution. Copyright © Canadian Association of Cardiovascular Prevention and Rehabilitation 2014 To be used with permission only. Not for re-distribution Table of Contents Patient information Identifying information Sociodemographic characteristics 1 2 Cardiac Rehab Program & Timing 5 Risk Factors at Intake 13 Disease Severity Indicators at Intake 16 Program Components Delivered 18 INTAKE/DISCHARGE Values Anthropometric, Lipid and Hemodynamic Measurements Functional Capacity Tests Other: Self-Report behaviours Psycho-social Indicators 19 22 29 31 Medications 33 Copyright © Canadian Association of Cardiovascular Prevention and Rehabilitation 2014 To be used with permission only. Not for re-distribution PATIENT INFORMATION IDENTIFYING INFORMATION Source Unique ID This number is electronically generated, encrypted, and represents a unique identifier that indicates which clinical record this patient relates to. Unique Patient ID Enter the patient’s permanent chart number (“patient ID number”, “hospital number”, “chart ID”, “hospital ID”) that corresponds to the patient’s permanent unique file number. If you are unsure which is the permanent hospital file number ask a member of the Health Records Department staff which number is sent to the Canadian Institute of Health Information (CIHI). This is not a “visit” number. The CCRR automatically encrypts this number. Data Source: Face sheet of the patient chart or on the Bradma plate stamped on the upper right corner of most pages of the chart. Data Entry: The HID number is institution specific and ranges between 6 and 10 digits. Consent Given Confirm that patient consent was obtained for data collection and analysis. Data Entry: Choices available are: Yes No Unknown: ‘Not documented’ Year of Birth Indicate the patient’s year of birth. Unknown: ‘Not documented’ Sex Select the patient’s sex. Data Entry: Choices available are: Male Female Other (trans-sexual or hermaphrodite) Unknown: Not documented 1 Copyright © Canadian Association of Cardiovascular Prevention and Rehabilitation 2014 To be used with permission only. Not for re-distribution SOCIODEMOGRAPHIC CHARACTERISTICS Ethnocultural Background Refers to the ethnic or cultural group (s) to which the patient and/or their ancestors belong. An ancestor is someone from whom a person is descended and is usually more distant than a grandparent. Ancestry should not be confused with citizenship or nationality. Ethnic or cultural origin refers to the ethnic “roots” of ancestral background of the population. You may need to explain to the patient why this information is necessary. You may choose to say “this information is collected to promote and ensure the equal opportunity for everyone to access cardiac rehabilitation services in Canada”. The information generated will ensure that future patients in Canada will have equal access to services. Data Sources: Patient intake assessment/interview. 1. Data Entry: “Indicate the patient’s ethnocultural background from the following (multiple responses accepted): Note: for mixed ethnocultural background, select all that apply.”(CCS definition), Aboriginal (includes Inuit, Métis peoples of Canada, First Nations – North American Indian)” (CCS definition), Arab (includes Egyptian, Kuwait, Libyan) (CCS definition) West Asian (includes Armenian, Egyptian, Iranian, Lebanese, Moroccan, Afganistan, Assyrian and Iranian)) (CCS definition) Black (includes African, Nigerian, Somali)(CCS definition) Chinese Filipino Japanese Korean Latin American(includes Chilean, Costa Rican, Mexican) (CCS definition) South Asian (includes Bangladeshi, Punjabi, Sri Lankan Bangladeshi, Sri Lankan) South East Asian (i.e. Cambodian, Loatian, Vietnamese, Malaysian) (CCS definition) White/Caucasian Other, if possible, specify (optional to specifiy) (CCS definition) Unknown / Not documented Marital Status Select the most appropriate response that corresponds with the patient’s marital status. Data Source: Face sheet of the patient chart, Admission history, History and Physical, Nursing Admission note, hospital information system, Intake Assessment Data Entry: Choices available are: Single Married or equivalent (i.e.: common law, same sex) Divorced Widowed Separated or equivalent Unknown: Not documented 2 Copyright © Canadian Association of Cardiovascular Prevention and Rehabilitation 2014 To be used with permission only. Not for re-distribution Language Preference Refers to the patient’s preference to communicate in one of Canada’s two official languages (English or French). Data Entry: Choices available are: English French Other Unknown: Not documented Education Indicate the highest level of education the patient has attained: Data Source: Admission history, intake assessment for cardiac rehabilitation. Data Entry: Less than High School (CCS definition) – patient did no complete all high school requirements and no Secondary School Diploma was awarded (or equivalent). High School – patient completed high school and Secondary School Diploma was awarded (or equivalent). Trades certificate (CCS definition) College certificate or diploma (a certificate from a community college, CEGEP, school of nursing, theological college or private college) (CCS definition) University (a certificate below the bachelor level, bachelor’s degree, certificate above the bachelor level, master’s degree, earned doctorate or a professional degree in medicine, dentistry, veterinary medicine or optometry) Unknown: Not documented Support Structure Select the most appropriate response that corresponds with the patient’s living situation. Data Source: Face sheet of the patient chart, Admission history, History and Physical, Nursing Admission note, hospital information system, Intake Assessment Data Entry: Choices available are: Lives alone – patient is living alone. Lives with Spouse/Partner – patient is currently living with a spouse or partner (married, common-law, same sex or equivalent) Lives with Friends/Family – patient is living with others that does not include a spouse or partner. This could include children, parents, in-laws. Other Unknown: Not documented 3 Copyright © Canadian Association of Cardiovascular Prevention and Rehabilitation 2014 To be used with permission only. Not for re-distribution Job Classification Ask the client to describe the degree of force exerted in their job. The job classifications options are taken from the U.S. Department of Labor's Dictionary of Occupational Titles, and are comparable to those classifications as found in the National Occupational Classification Career Handbook (NOC-CH; http://www.wcb.ab.ca/providers/addgjob.asp). Data Entry: Choices available are: SEDENTARY WORK - Exerting up to 10 pounds of force occasionally and/or a negligible amount of force frequently or constantly to lift, carry, push, pull or otherwise move objects, including the human body. Sedentary work involves sitting most of the time, but may involve walking or standing for brief periods of time. Jobs are sedentary if walking and standing are required only occasionally and all other sedentary criteria are met. LIGHT WORK - Exerting up to 20 pounds of force occasionally and/or up to 10 pounds of force frequently, and/or negligible amount of force constantly to move objects. Physical demand requirements are in excess of those for sedentary work. Light work usually requires walking or standing to a significant degree. However, if the use of the arm and/or leg controls require exertion of forces greater than that for sedentary work, and the worker sits most of the time, the job is rated light work. MEDIUM WORK - Exerting up to 50 pounds of force occasionally, and/or up to 20 pounds of force frequently, and/or up to 10 pounds of force constantly to move objects. HEAVY WORK - Exerting up to 100 pounds of force occasionally, and/or up to 50 pounds of force frequently, and/or up to 20 pounds of force constantly to move objects. VERY HEAVY WORK - Exerting in excess of 100 pounds of force occasionally, and/or in excess of 50 pounds of force frequently, and/or in excess of 20 pounds of force constantly to move objects Not applicable – patient does not work, or is not going back to work Unknown: Not documented 4 Copyright © Canadian Association of Cardiovascular Prevention and Rehabilitation 2014 To be used with permission only. Not for re-distribution CARDIAC REHAB PROGRAM & TIMING Hospital Discharge Date Enter the day, month and year the patient was discharged from hospital. Data Entry: Not applicable if patient referred following outpatient visit or for stable disease. “Not documented” / unknown Referral Diagnosis The referral diagnosis refers to the most recent diagnosis preceding the patient’s referral to cardiac rehabilitation. This item does not include interventions or procedures. There may be more than one possible referral diagnosis reported if the second referral diagnosis occurred within the same hospitalization period. The following are possible scenarios: 1. If the patient had coronary artery bypass graft surgery with an aortic valve replacement then both CABG and AVR would be considered referral diagnoses. 2. If patient had an MI, was referred for cardiac rehabilitation and had another event during the period between referral and intake, the MI would count as the referral diagnosis and the secondary event would be listed as a secondary referral diagnosis. Data Source: Patient’s chart, referral form, health professional referral letter, patient intake interview. Data Entry: Choices available are: Stable CAD / Angina Acute coronary syndrome (ACS) – Unspecified Acute coronary syndrome (ACS) - Myocardial infarction - Unspecified Acute coronary syndrome (ACS) - Myocardial infarction - STEMI Acute coronary syndrome (ACS) - Myocardial infarction - Non STEMI Acute coronary syndrome (ACS) - Unstable Angina Heart Failure - Unspecified Heart Failure - Cardiomyopathy Cerebral vascular disease - Unspecified Cerebral vascular disease - TIA Cerebral vascular disease - Stroke Peripheral Vascular disease High-Risk Primary Prevention Arrhythmia – unspecified Arrhythmia – atrial fibrillation Arrhythmia – ventricular tachycardia Arrhythmia - other Other Unknown: Not documented 5 Copyright © Canadian Association of Cardiovascular Prevention and Rehabilitation 2014 To be used with permission only. Not for re-distribution Referral Procedure(s) Did the patient undergo a procedure associated with the referral diagnosis(es)? Choose all that apply. Data Source: Patient’s chart Data Entry: Choices available are: Yes – please specify: o Percutaneous coronary intervention (PCI) o Bypass surgery – CABG o Heart Transplant o Valve surgery o Percuteneous valve intervention o VADs Device insertion (e.g., CRT, ICD, Pacemaker) o Ablation o Other No Unknown: Not documented Referral Diagnosis(es)/Procedure(s) Date(s) Enter the date(s) of the diagnosis(es), If there is more than one date as in scenario #2 above, enter a date for each event selected. However, the date corresponding to the most recent referral event will be considered the Referral Diagnosis Date. If the patient did not have an event recently, but a procedure, enter the procedure date. Data Source: Face sheet of the patient chart, hospital information system, nursing admission note, physician referral note, history and physical, or cardiac rehabilitation intake interview. Data Entry: o Not applicable – patient referred for stable disease or high-risk primary prevention o Unknown: ‘Not documented’ History of cardiac event(s) Does the patient have a history of cardiac events? Choose all that apply. Enter dates for each. Data Source: Patient’s chart, referral form, health professional referral letter, patient intake interview. Data Entry: Choices available are: 6 Copyright © Canadian Association of Cardiovascular Prevention and Rehabilitation 2014 To be used with permission only. Not for re-distribution o Yes: Stable CAD/Angina Acute coronary syndrome (ACS) – Unspecified Acute coronary syndrome (ACS) – Myocardial infarction Unspecified Acute coronary syndrome (ACS) – Myocardial infarction – STEMI Acute coronary syndrome (ACS) – Myocardial infarction – NonSTEMI Acute coronary syndrome (ACS) – Unstable Angina Heart Failure - Unspecified Heart Failure – Cardiomyopathy Cerebral vascular disease - Unspecified Cerebral vascular disease - TIA Cerebral vascular disease - Stroke Peripheral Vascular disease High Risk Primary Prevention Arrhythmia – unspecified Arrhythmia – atrial fibrillation Arrhythmia – ventricular tachycardia Arrhythmia - other other o No o Unknown: Not documented History of cardiac procedure(s) Does the patient have history of cardiac procedure(s)? Choose all that apply. Enter dates for each. Data Source: Patient’s chart Data Entry: Choices available are: Yes, please list: - need date field associated with this o Percutaneous intervention (PCI) o Bypass surgery – CABG o Heart transplant o Valve surgery o Percutenous Valve insertion o Ablation o VADs o Device (e.g., CRT, ICD, Pacemaker) No Other Unknown: Not documented 7 Copyright © Canadian Association of Cardiovascular Prevention and Rehabilitation 2014 To be used with permission only. Not for re-distribution Comorbidities Does the patient have a diagnosis of any of the following conditions? Choose all that apply Data Source: Patient’s chart, referral form, health professional referral letter, patient intake interview. Data Entry: Choices available are: Arthritis Musculoskeletal pain Hip or knee replacement Cancer Osteoporosis Renal disease Liver disease Pulmonary disease Infectious disease Other No Unknown / not documented Referral Location Where did the referral come from? Data Source: Patient’s chart Data Entry: Choices available are: In-patient unit Outpatient visit [ambulatory clinic/MD office] Emergency room Cardiac diagnostics / Intervention Other Unknown / Not documented Type of Referring Provider Enter the type of provider who signed the referral form. Data Entry: Choices available are: Cardiologist Cardiovascular surgeon 8 Copyright © Canadian Association of Cardiovascular Prevention and Rehabilitation 2014 To be used with permission only. Not for re-distribution Primary care physician Nurse-practitioner Other Unknown: Not documented Referral Date Enter the date the CR referral document was signed by a physician. For patients referred from an inpatient care team, this may be the date of the discharge orders. Data Source: Face sheet of the patient’s chart, referral form at the CR program, others as indicated. Data Entry: Enter a date. Unknown: ‘Not documented’ Referral Receipt Date Enter the date the patient referral is received by the program. Data Source: Face sheet of the patient’s chart, referral form at the CR program, date received stamped or fax date on referral form, others as indicated. Data Entry: Enter a date. Unknown: ‘Not documented’ Automatic Referral Was this referral initiated automatically? Data Entry: Choices available are: Yes No Unknown: ‘Not documented’ Patient Enrolment CR Program enrollment is defined as patient attendance at any first CR program visit. Please note that all referred patients should be entered in CCRR so that we can assess the proportion of referred patients enrolling (CR quality indicator). For those patients who do not enroll, please complete all available information from their referral form. It is hoped that sex, year of birth, hospital discharge date, referral diagnosis, referral procedure, referral diagnosis / procedure date, referral location, type of referring provider, referral date, referral receipt date, and automatic referral variables could be completed. Please also record interim events and corresponding dates if applicable. Data Entry: Choices available are: Yes No Unknown: ‘Not documented’ 9 Copyright © Canadian Association of Cardiovascular Prevention and Rehabilitation 2014 To be used with permission only. Not for re-distribution Intake Visit Date Enter the date the patient attended the first appointment at the CR program (this may be the intake assessment, rehabilitation exercise test, educational class, or other services) Data Source: Patient’s chart. Data Entry: Enter a date. Unknown: ‘Not documented’ Program Model Enter the type of program in which the patient is participating. This does not refer to maintenance programs. Data Source: Patient’s chart. Data Entry: Supervised program in a clinical setting (e.g., traditional hospital-based program) Home-based (i.e., includes intake assessment, comprehensive CR elements with monitoring by phone or email, and formal re-assessment at program completion) Community-based (supervised exercise in a community setting) Web-based or mobile phone Other Unknown / not documented Travel Time to Rehab Enter the estimated time for a one-way trip using the form of transportation available and to be used most often by the patient to access cardiac rehab. Data Source: Cardiac rehabilitation intake interview/ assessment. Data Entry: Choices available are: 0-30 minutes 31-45 minutes 46-60 minutes > 60 minutes Unknown: Not documented Date the CR Program Began Enter the date the patient officially began the exercise portion of the cardiac rehabilitation program. Please note that this applies to both on and off-site (home-based) cardiac rehabilitation programs. Unknown: ‘Not documented’ Interim Event(s) List any cardiac event(s) that occurred after referral to and prior to discharge from cardiac rehabilitation. Multiple post-referral events are possible. 10 Copyright © Canadian Association of Cardiovascular Prevention and Rehabilitation 2014 To be used with permission only. Not for re-distribution Data Source: Patient’s chart, physician progress note/assessment, nursing intake assessment note, hospitalization record(s), patient report (must followup with primary care physician to validate). Data Entry: Choices available are: Yes, please choose all that apply: o Acute coronary syndrome (ACS) – Unspecified o Acute coronary syndrome (ACS) - Myocardial infarction – Unspecified o Acute coronary syndrome (ACS) - Myocardial infarction – STEMI o Acute coronary syndrome (ACS) - Myocardial infarction - Non STEMI o Acute coronary syndrome (ACS) - Unstable Angina o Cerebral vascular disease - TIA or stroke o Other o Death – Cardiac o Death - Non Cardiac No, patient had no interim event Unknown: Not documented Interim Event(s) Date(s) Date(s) of cardiac event(s) occurring after referral to and prior to discharge from cardiac rehabilitation. Data Source: Patient’s chart, physician progress note/assessment, nursing intake assessment note, hospitalization record(s), patient report (must follow-up with primary care physician to validate). Unknown: ‘Not documented’ Not applicable (no interim event) Interim cardiac procedure(s) Did the patient have cardiac procedure(s) occurring after referral to and prior to discharge from cardiac rehabilitation? Choose all that apply. Enter dates for each. Data Source: Patient’s chart Data Entry: Choices available are: Yes, please check all that apply o Percutaneous intervention (PCI) o Bypass surgery – CABG o Valve surgery o Percutaneous valve procedure o Device insertion (e.g., CRT, ICD, Pacemaker) o Ablation o VADs o other None 11 Copyright © Canadian Association of Cardiovascular Prevention and Rehabilitation 2014 To be used with permission only. Not for re-distribution Not documented Premature Termination(s) Premature termination refers to the instance where patients do not complete their prescribed exercise sessions or other core components of the program. Indicate the reason for premature termination of the patient's cardiac rehab program, if applicable. Data Entry: Choices available are: Lost to follow-up (patient stopped coming and could not contact them) Patient choice (quit) Relocation Return to work Event – Cardiac Event – Other health problem Death Patient met goals early Not applicable – patient completed program Other Not documented Premature Termination(s) Date If applicable, enter the date that patient prematurely terminated participation in the program. Include Not applicable to indicate that the patient did not premature terminate the CR program. Unknown: ‘Not documented’ CR Program Completion To complete the CR program a patient must have attended at least some of the CR intervention components and also have completed a formal re-assessment by the CR team at the conclusion of the CR intervention. Indicate if the patient completed the CR program. Data Entry: Choices available are: - Yes - No - Not applicable (patient had an interim event or a premature termination of the program) - Unknown: Not documented Discharge Date Indicate the date of discharge from the cardiac rehabilitation program. The discharge date could be based on the patient completing the active CR program, the patient completing all recommended services, or a date prior to completing CR program due to specific reasons. This date should closely correspond to the 12 Copyright © Canadian Association of Cardiovascular Prevention and Rehabilitation 2014 To be used with permission only. Not for re-distribution patient’s last documented rehabilitation visit. Note: it must not be the date of a post-CR program follow-up. Data Source: Patient’s chart. Unknown: Not documented Discharge Summary Sent To Primary Care Physician Was CR discharge summary sent to patient’s primary care provider? Data Source: Patient’s chart Data Entry: Yes No Unknown: Not documented Discharge Summary Elements If there was a discharge summary generated, did it include the following 4 elements? 1. a description of the patient’s lifestyle risk factors (physical activity, diet and smoking as relevant), 2. medical risk factors (blood pressure, lipids and glucose as relevant), 3. cardiac medications, and 4. and long-term management goals. Data Source: Patient’s chart Data Entry: o Yes – all 4 were fully included o Partial – some but not all of these elements were included in the discharge summary o No o Not applicable – there is no discharge summary for this patient o Unknown: Not documented Discharge Summary to Patient Was the patient provided with a lay summary of their progress and updated exercise prescription at program exit? Data Source: Patient’s chart Data Entry: Yes No Unknown: Not documented RISK FACTORS AT INTAKE Physical Activity History 13 Copyright © Canadian Association of Cardiovascular Prevention and Rehabilitation 2014 To be used with permission only. Not for re-distribution Does the patient report that they accumulated at least 150 minutes of moderate- to vigorous-intensity aerobic physical activity per week, in bouts of 10 minutes or more? (CSEP / QI consistent) Data Sources: Initial intake visit, patient interview/questionnaire. Patient asked to describe their physical activity history. Data Entry: Yes – The patient reports that they participate in moderate to vigorousintensity physical activity for 150 minutes per week. Partial – The patient reports that they engage in some physical activity, but not 150 mins per week No - The patient reports that they are not physically active Unknown: Not documented e.g., the patient’s physical activity cannot be determined by the sources defined or the reliability of the information is questionable. Hyperlipidemia Patient has a documented history of dyslipidemia diagnosed and/or treated by a physician. Data Source: History & Physical, Emergency Department record/notes, Nursing Admission notes, Physician’s progress notes, lab results Data Entry: Yes - if there is a history of Hyperlipidemia documented, if patient is on lipid-lowering medications prescribed to treat dyslipidemia and/or if LDL >2.0 mmol/L in patients with vascular disease, including CAD, or diabetes No - if there is no documented history of or treatment for Hyperlipidemia Unknown: Not documented or if there is no mention of Hyperlipidemia in any of the recommended sources listed above. Hypertension Patient has a documented history of hypertension diagnosed and/or treated by a healthcare provider. Treatment may include medication, diet and / or exercise. Any of the following terms apply: Accelerated Blood Pressure Benign hypertension Elevated blood pressure (BP) High blood pressure (BP) Hypertension (HTN) Hypertensive heart disease Labile hypertension Renal hypertension Renovascular hypertension Systemic hypertension Systolic hypertension Uncontrolled hypertension 14 Copyright © Canadian Association of Cardiovascular Prevention and Rehabilitation 2014 To be used with permission only. Not for re-distribution Those conditions that should NOT be considered hypertension are: Intraocular hypertension Portal hypertension Pulmonary hypertension (any) Data Source: History & Physical, Emergency Department record/notes, Nursing Admission notes, Physician’s progress notes, current treatment for hypertension. Data Entry: Yes - if there is a history of Hypertension (values 140/90 mmHg for patients without diabetes or 130/85 mmHg for patients with diabetes), or patient is on blood pressure-lowering medication prescribed specifically for hypertension No - if there is no history of Hypertension or if there is no mention of Hypertension in any of the recommended sources listed above; Unknown: Not documented Family History of CAD Patient has/had any direct blood relative (parents, siblings, and children) who have been diagnosed with angina, MI, PCI, CABG or sudden cardiac death for male relatives before age 55 years or for female relatives before age 65 years. Data Source: History & Physical, Emergency Department record/notes, Nursing Admission notes, Physician’s progress notes, patient intake assessment. Data Entry: Yes No Unknown: Not documented / unknown Diabetes Was there a documented diagnosis of diabetes or treatment for diabetes? Any of the following documented terms apply: Adult Onset Diabetes Mellitus Diabetes Diabetes Mellitus (DM) Diet controlled diabetes DM Type I (1) or Type II (2) Drug induced diabetes Juvenile Diabetes Non-insulin dependent Diabetes Mellitus Any treatment/medication for diabetes Those conditions that should NOT be considered as diabetes are: Diabetes insipidus History of gestational diabetes Impaired fasting glucose 15 Copyright © Canadian Association of Cardiovascular Prevention and Rehabilitation 2014 To be used with permission only. Not for re-distribution Glucose intolerance Data Source: History & Physical, Emergency Department record/notes, Nursing Admission notes, Physician’s progress notes, Intake Assessment, current treatment for diabetes. Data Entry: Yes - if diabetes is mentioned in any of the recommended sources listed above or if the patient is on a medication used to treat diabetes. No - if there is no history of diabetes or if there is no mention of diabetes in any of the recommended sources listed above. Unknown: ‘Not documented’ Diabetes Type If “Yes” is indicated above, enter: Type 1 Type 2 Unknown: Not documented Sleep Apnea Patient has a documented history of sleep apnea Data Source: History & Physical, Emergency Department record/notes, Nursing Admission notes, Physician’s progress notes, Intake Assessment, current treatment for diabetes. Data Entry: Yes No Unknown: Not documented . DISEASE SEVERITY INDICATORS AT INTAKE CCS Angina Class Enter the corresponding Canadian Cardiovascular Society Angina Class at the time of intake. The CCS Angina Class must be determined post – referral event and should be assessed at the time of intake. If not assessed at intake and no post-event documentation is available, select Unknown from the pick list. Data Source: Face sheet of the patient chart, Admission history, History and Physical, Nursing Admission note, Physician’s progress notes, hospital information system, Discharge summary or angiography or echocardiography test reports. Data Entry: Choices available are: 0 – Asymptomatic 16 Copyright © Canadian Association of Cardiovascular Prevention and Rehabilitation 2014 To be used with permission only. Not for re-distribution 1 - Ordinary physical activity such as walking or climbing does not cause angina. Angina with strenuous, rapid or prolonged exertion at work or recreation. 2 - Slight limitation of ordinary activity. Walking or climbing stairs rapidly, walking uphill, walking or climbing stairs after meals or in cold or in wind, or under emotional stress or during the few hours after wakening. Walking more than 2 blocks on the level and climbing more than one flight of stairs at a normal pace and in normal conditions. 3 - Marked limitation of ordinary physical activity. Walking one or two blocks on the level or climbing one flight of stairs in normal conditions and at a normal pace. 4 - Inability to carry out any physical activity without discomfort; angina may be present at rest Unknown: Not documented NYHA class Enter a value from I to IV as indicated at intake. The NYHA Functional Class needs to be determined post-referral event and should be assessed at the time of intake. If not assessed at intake and no post-event documentation is available, select Unknown from the pick list. Data Source: Face sheet of the patient chart, Admission history, History and Physical, Nursing Admission note, Physician’s progress notes, hospital information system, Discharge summary or angiography or echocardiography test reports. Data Entry: Choices available are: I - Patients with cardiac disease but without resulting limitations of physical activity. Ordinary physical activity does not cause undue fatigue, palpitation, dyspnea, or anginal pain II - Patients with cardiac disease that results in a slight limitation of physical activity. Patients are comfortable at rest, but ordinary physical activity results in fatigue, palpitation, dyspnea, or anginal pain III - Patients with cardiac disease that results in a marked limitation of physical activity. Patients are comfortable at rest, but less than ordinary physical activity results in fatigue, palpitation, dyspnea, or anginal pain IV - Patients with cardiac disease that results in an inability to carry on any physical activity without discomfort; fatigue, dyspnea, or anginal pain may be present; if any physical activity is undertaken, symptoms increase. Symptoms may be present at rest. Unknown: Not documented LV Function or LV Function Exact – if one is chosen, the other should grey out. 17 Copyright © Canadian Association of Cardiovascular Prevention and Rehabilitation 2014 To be used with permission only. Not for re-distribution Enter the exact left ventricular ejection fraction (LVEF), if available. OR If exact LVEF unavailable, enter the appropriate value from the pick list provided to indicate the patients LVEF or degree of left ventricular function. LV Function to be assessed post-referral event and/or within 6 months of Intake. If there is no available documentation, select Unknown from the pick list. Data Source: Physician notes: Admission history, History and Physical, Admission note, Physician’s progress notes, Discharge summary, or referral note; Primary source documentation: angiography or echocardiography test reports. Data Entry: Select only one of the following that corresponds to the patients level of left ventricular function. Normal ≥50% or greater CCS = Normal >50% Mild 40% and 49% CCS = Slightly reduced (41-50%) Moderate 30% and 39% CCS = Moderately reduced (31-40%) Severe <30% CCS = Severely reduced (≤30%) LV Function not assessed (CCS definition) Unknown: Not documented. PROGRAM COMPONENTS DELIVERED Information regarding the service referral data elements can most likely be found in the patient chart. This could be offered internal or external to the CR program. Exercise Sessions Prescribed Enter the total number of exercise classes scheduled for the patient’s cardiac rehab program. Unknown: ‘Not documented’ Exercise Sessions Completed Enter the total number of exercise classes attended by the patient during their rehab program. Unknown: ‘Not documented’ Education Was the patient offered group or individual education within the program, particularly that counselled patients regarding self-management for heart-healthy behavior changes? Offered and Accepted Offered and Declined - If a patient does not accept or declines the offer Not Offered Unknown: Not documented Nutrition counselling Was the patient offered group or individual nutrition counselling? 18 Copyright © Canadian Association of Cardiovascular Prevention and Rehabilitation 2014 To be used with permission only. Not for re-distribution Offered and Accepted Offered and Declined - If a patient does not accept or declines the offer Not Offered Unknown: Not documented Smoking Cessation Counselling or Treatment Was the patient offered smoking cessation counselling or treatment? Offered and Accepted Offered and Declined - If a patient does not accept or decline the offer please Not Offered Not applicable - If patient is a non-smoker Unknown: Not documented Stress Management Was the patient offered a stress management class or program? Offered and Accepted Offered and Declined Not Offered Not applicable Unknown: Not documented Depression Counselling or Treatment Was the patient offered a depression counselling program or other treatment (e.g., anti-depressants)? Data Entry: Choices available are: Offered and Accepted Offered and Declined - If a patient does not accept or declines the offer Not Offered not applicable – patient is not depressed Unknown: Not documented Promotion of Post-CR Physical Activity Was patient provided an exit exercise prescription and an intervention to promote long-term physical activity post-CR (e.g., motivational interviewing?) Data Entry: Choices available are: Yes No Unknown: Not documented INTAKE & DISCHARGE MEASUREMENTS The following measures are to be completed at program intake and discharge. If the patient is scheduled to have labs done as part of his/her admission and/or discharge evaluation, you can use those results in the corresponding sections. 19 Copyright © Canadian Association of Cardiovascular Prevention and Rehabilitation 2014 To be used with permission only. Not for re-distribution Use the values from the most recent test date you can find in the medical record that is no earlier than one (1) year prior to the assessment date. Do not use values that are more than one year old at the time of the assessment. For example, if the patient’s enrollment date is in November and he/she had lipid results from three months earlier (in August), use these values. If there are no entry values within the one-year time limit, enter “unknown”. If the patient’s discharge was subsequently in January but he/she did not have any repeat lipid tests done, DO NOT repeat the previous values. Instead, enter “unknown”. BIOCHEMISTRY Note: Blood work must be done under standard fasting conditions (9- 12 hours since last meal; Canadian Lipid Guidelines, 2006). Blood Sugar Profile FBS (mmol/L) This refers to the patient’s fasting blood glucose level. Data Source: (1) Lab Report, (2) Emergency Department record/notes, (3) History & Physical, (4) Progress note. Data Entry: Enter in the space provided the value obtained for fasting glucose. Add other options in a dropdown format: - Not documented /unknown HBA1c (percent) This refers to the patient’s glycosylated hemoglobin level. Data Source: (1) Lab Report, (2) Emergency Department record/notes, (3) History & Physical, (4) Progress note. Data Entry: Enter in the space provided the value obtained for glycosylated hemoglobin. This value should be entered as a decimal. For example, an HbA1c of 6% should be entered as 0.06. Add other options in a dropdown format: Not documented /unknown Lipid Profile (mmol/L) Total Cholesterol (TC) (mmol/L) What was the patient’s total cholesterol value. Data Source: (1) Lab Report, (2) Emergency Department record/notes, (3) History & Physical, (4) Progress note. Data Entry: Enter the value for total cholesterol in mmol/L Add other options in a dropdown format: - Not documented / unknown Triglycerides (TG) (mmol/L) What was the serum triglycerides (TG) result? 20 Copyright © Canadian Association of Cardiovascular Prevention and Rehabilitation 2014 To be used with permission only. Not for re-distribution - Data Source: (1) Lab Report, (2) Progress note. Data Entry: Enter value obtained for serum Triglycerides in mmol/L. Add other options in a dropdown format: Not documented / unknown High Density Lipoprotein (HDLC) (mmol/L) What was the HDL cholesterol result? Data Source: (1) Lab Report, (2) Progress note. Data Entry: Enter value obtained for HDL cholesterol (HDL) in mmol/L. Add other options in a dropdown format: - Not documented / unknown Low Density Lipoprotein (LDLC) (mmol/L) What was the LDL cholesterol result? (may be called non-HDL) Data Source: (1) Lab Report, (2) Progress note. Data Entry: Enter value obtained for LDL cholesterol (LDL) in mmol/L. Add other options in a dropdown format: - Unknown (If there are no entry values within the one-year time limit; or, the patient did not have any repeat lipid tests done at discharge) - Not documented / unknown ANTHROPOMETRIC Weight (KG) Weigh the patient prior to exercise without shoes, pockets emptied, and while wearing his/her typical or usual exercise clothes. Record weight to the nearest tenth of a kilogram if using a digital scale, to the nearest quarter pound if using a balance beam scale. The scale should be placed on a solid, level surface. Data Source: Direct measurement at the intake assessment. Data entry: Enter the patient’s weight to the nearest 10th of a kilogram (i.e. 78.0 kg). Add other options in a dropdown format: - Not documented (unknown) Height (cm) Measure the patient’s height in stocking feet to the nearest whole centimetre. Have the patient stand erect with the heels, buttocks, back of shoulders, and back of head against the vertical scale. With the patient holding their breath, bring the horizontal bar into contact with the highest point on the head. Data Source: Direct measurement at the intake and discharge assessment visit. Data Entry: Enter the patient’s height to the nearest cm. The number you enter will be three digits (e.g. 172). Add other options in a dropdown format: - Unknown: Not documented Waist (cm) 21 Copyright © Canadian Association of Cardiovascular Prevention and Rehabilitation 2014 To be used with permission only. Not for re-distribution Enter the patient’s waist measurement in centimetres (cm), at the approximate midpoint between lower margin of the last palpable rib and top of the iliac crest (WHO). Patient should stand with arms at sides, feet positioned close together, with weight evenly distributed across feet. Assess at end of normal expiration when lungs are at functional residual capacity. Take without clothing – directly over skin; if not possible, over light clothing. Data Source: Direct measurement at the intake and discharge assessment. Data entry: Enter value obtained from patient’s waist measurement to the nearest centimetre. Add other options in a dropdown format: - Not documented (unknown) HEMODYNAMIC 2009 Canadian Hypertension Education Program (CHEP) Recommended Technique for Measuring Blood Pressure Place the cuff so that the lower edge is 3 cm above the elbow crease and the bladder is centered over the brachial artery. The patient should be resting comfortably for 5 minutes in the seated position with back support. The arm should be bare and supported with the antecubital fossa at heart level, as a lower position will result in an erroneously higher SBP and DBP. There should be no talking, and patients’ legs should not be crossed. At least three measurements should be taken in the same arm with the patient in the same position. The first reading should be discarded and the latter two averaged. 2014 Updated CHEP Recommendations for accurate measurement of blood pressure: https://www.hypertension.ca/en/professional/chep/diagnosis-measurement/accuratemeasurement-of-blood-pressure Systolic Blood Pressure / Diastolic Blood Pressure (SBP / DBP) (mm) Enter the patient’s systolic blood pressure (mmHg) and the patient’s diastolic blood pressure (mmHg). BP assessement should be undertaken manually or with a validated automated device only (e.g., see: http://www.dableducational.org/). Data Source: Direct measurement at the intake assessment. Data entry: Enter value obtained from patient’s SBP and DBP. Add other options in a dropdown format: Not documented /unknown 22 Copyright © Canadian Association of Cardiovascular Prevention and Rehabilitation 2014 To be used with permission only. Not for re-distribution Pulse Rate (bpm) Enter the patient’s heart rate (bpm). Data Source: Direct measurement at the intake assessment. Data entry: Enter value obtained from patient’s pulse measurement. Add other options in a dropdown format: Not documented / unknown FUNCTIONAL CAPACITY TESTS The following measures are required at program intake and discharge. NOTE An exercise stress test on a treadmill using a standardized protocol such as the Ramp, Bruce or Modified Bruce is recommended. A previously-completed symptomlimited maximal stress test can be entered, providing it was completed postreferral event and within 1 month of the intake date. Alternatively a cycle test can be performed (see below for calculation to convert watts to METs). Some programs do not perform routine stress tests. In this instance, another functional capacity test such as a 6 minute walk test should be reported. Type of Functional Capacity Assessment Was an assessment of functional capacity performed? Data Entry: Check all that apply: GXT 6 minute walk test Duke Activity Status Index Other None Not applicable Not documented Patient Cleared for Stress Testing Did the patient meet the ACSM safety recommendations for undertaking a stress test. For example, patients who cannot walk on a treadmill unaided, or who cannot cycle on a bike ergometer. Yes No N/A - this program does not do stress testing (see below for other functional tests) Unknown: Not documented Functional Test Date When was the functional test performed? Data Entry: Please use the calendar to enter the date of the exercise stress test. Add other options in a dropdown format: 23 Copyright © Canadian Association of Cardiovascular Prevention and Rehabilitation 2014 To be used with permission only. Not for re-distribution Not applicable Unknown: Not documented GXT Protocol What was the GXT protocol used for the exercise stress test? Data Source: Exercise stress test report. Data Entry: Choices available are: Bruce Bruce-Modified Ramp Other Not applicable Unknown: Not documented GXT Modality Data Source: Exercise stress test report. Data Entry: Choice available are: Treadmill Cycle Other Not applicable Not documented /Unknown Exercise Capacity Directly Measured Indicate if exercise capacity level was directly measured using gas analysis. Data Source: Exercise stress test report. Data Entry: Yes - if exercise capacity was directly measured by oxygen uptake (CPA test) No - if exercise capacity was estimated using standard equations from final workload level completed. Not applicable Unknown: Not documented Resting SBP (mm) What was the patient's resting systolic blood pressure immediately before the functional stress test? Data Source: Exercise stress or other functional test reports. Data Entry: If two BPs were recorded for the same time or it was taken in both arms enter the highest systolic reading. If a range is given, record the mid-value i.e. 120-130 record 125. not applicable (e.g., patient has a VAD) Not documented / unknown Resting DBP (mm) What was the patient's resting diastolic blood pressure immediately before the functional test? 24 Copyright © Canadian Association of Cardiovascular Prevention and Rehabilitation 2014 To be used with permission only. Not for re-distribution Data Source: Exercise stress test report. Data Entry: If two BPs were recorded for the same time and have the same diastolic BP record the one with the highest diastolic value. If a range is given, record the mid-value i.e. 60 – 70 record 65. If the first diastolic BP is recorded in the chart as “p” for palpatation find the next BP with both systolic and diastolic values recorded numerically. Not documented / unknown Peak SBP (mm) What was the patient's peak systolic blood pressure during the funtional test? Data Source: Exercise stress test reports. Data Entry: If two BPs were recorded for the same time or it was taken in both arms enter the highest systolic reading. If a range is given, record the mid-value i.e. 120-130 record 125 not applicable (e.g., patient has a VAD) Not documented / unknown Peak DBP (mm) What was the patient's peak diastolic blood pressure during the functional test? Data Source: Exercise stress test or other functional test report. Data Entry: If two BPs were recorded for the same time and have the same diastolic BP record the one with the highest diastolic value. If a range is given, record the mid-value i.e. 60 – 70 record 65. If the first diastolic BP is recorded in the chart as “p” for palpatation find the next BP with both systolic and diastolic values recorded numerically. Not documented / unknown Resting Heart Rate (HR) What was the patient’s resting heart rate immediately prior to the start of the functional test? Data Source: Exercise stress test or other functional test report. Data Entry: Enter the resting heart rate (beats per minute) recorded on the electrocardiogram during the exercise test. In the event that the HR is not accurate on the cardiogram, a palpated HR (apical or radial) may be used. Not documented / unknown Peak Heart Rate (HR) What was the patient’s peak heart rate during the exercise stress test? 25 Copyright © Canadian Association of Cardiovascular Prevention and Rehabilitation 2014 To be used with permission only. Not for re-distribution Data Source: Exercise stress test or other functional test report. Data Entry: Enter the peak heart rate (beats per minute) recorded on the electrocardiogram during the exercise test. In the event that the HR is not accurate on the cardiogram, a palpated HR (apical or radial) may be used. Not documented / unknown Exercise Time What was the duration of exercise during the funtional stress? Data Source: Exercise stress test or other functional test report. Data Entry: Enter the duration of exercise in minutes. For example, a duration of 14 minutes and 30 seconds would be entered as 14.5. Add other options in a dropdown format: Not applicable Not documented / unknown 6 min walk distance (m) Report the distance attained during the 6-minute walk test in feet or meters. (Please refer to “ATS Statement: Guidelines for the Six-Minute Walk Test” [Am J Respir Crit Care Med. 2002; 166: 111-117. doi: 10.1164/rccm.166/1/111] Data Entry: o Enter meters walked o Not applicable o Not documented / unknown Symptom-Limited Was the functional test stopped early due to patient symptoms? Data Source: Exercise stress or other functional test report. Data Entry: Yes No Not applicable Not documented / unknown Reason for Premature Termination If the exercise stress or other functional test was terminated, provide the reason why. Data Source: Exercise stress test or other functional test report. Data Entry: Choices available are: Fatigue/leg pain Dyspnea Angina ST changes Arrhythmias 26 Copyright © Canadian Association of Cardiovascular Prevention and Rehabilitation 2014 To be used with permission only. Not for re-distribution Drop in BP Hypertensive response Presyncopal Patient request Equipment problems MD instruction Other Not applicable – no premature termination Not documented / unknown Angina Indicate if patient had documented angina during the exercise stress or other functional test. Data Source: Exercise stress test report and or exercise test ECG or other functional test report Data Entry: Choices available are: None Non-limiting Stopped Test Not documented / unknown Borg 10 Scale If the Borg 10 Scale was used, enter the maximum Borg rating achieved at completion of the exercise stress or other functional test. The Borg rating is used to assess perceived level of exertion. Data Source: Exercise stress test or other functional test report. Data Entry: Value from 0-10 Add other options in a dropdown format: Not applicable – did not use the Borg 10 scale Not documented / unknown 0 0.5 1 2 3 4 5 6 7 8 9 10 10-Grade Scale Nothing Very, very weak Very weak Weak (light) Moderate Somewhat strong Strong (heavy) Very strong Very, very strong Borg 15 Scale 27 Copyright © Canadian Association of Cardiovascular Prevention and Rehabilitation 2014 To be used with permission only. Not for re-distribution If the Borg 15 Scale was used, enter the maximum Borg rating achieved at completion of the exercise stress or other functional test. The Borg rating is used to assess perceived level of exertion. Data Source: Exercise stress test or other functional test report. Data Entry: Value from 6-20 Add other options in a dropdown format: Not applicable – did not use the Borg 15 scale Not documented / unknown 15-Grade scale 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 Very, very light Very light Fairly light Somewhat hard Hard Very hard Very, very hard Max ST Depression Indicate the maximum level of ST segment depression. ST depression is defined as horizontal or down-sloping ST depression measured at 60 or 80ms after the J point. Data Source: Physician interpretation on the exercise stress test report and/or exercise test ECG. Data Entry: Write in number of millimeters noted on the test. Add other options in a dropdown format: o Not applicable – no exercise ECG performed o Not documented / unknown Peak METs Indicate the peak METs achieved during the test or assessment in the space provided. The METs can be estimated from standard equations using speed and grade, or can be calculated from the direct measurement of oxygen consumption using gas analysis. To calculate METs from watts see: http://sportsartamerica.com/SAF/support/technicalsupport/techtips/General%20Info/Watt s_to_METs_Conversions.pdf Data Source: Exercise stress test or other functional assessment. 28 Copyright © Canadian Association of Cardiovascular Prevention and Rehabilitation 2014 To be used with permission only. Not for re-distribution Data Entry: Enter the numeric value of the peak METs as indicated by the exercise stress test report to the nearest 1/10 of a MET (i.e. 5.4 METs). other options in a dropdown format: o Not applicable – METS not assessed o Not documented / unknown Risk assessment Was a risk assessment for adverse cardiovascular assessment performed? Data Source: CR chart Data Entry: Check all that apply: Duke treadmill score Cardiometabolic fitness risk stratification Framingham risk score Other No Not documented / unknown Duke Treadmill Score The DTS is a weighted index combining treadmill time, ST segment deviation (depression or elevation), and exercise-induced angina. It provides accurate diagnostic and prognostic information. DTS = Exercise Time (regular Bruce protocol minutes)* – (5x ST deviation) – (4x Angina index) Can be “back-calculated” from non-Bruce protocols solving for METs. Angina Index: 0=none, 1=during test, and 2=angina stopped test. Distinction between exercise-induced angina and non-anginal chest pain is based on the clinical judgement of the physician supervising the stress test. Emphasis is placed on reproducing the patient’s usual presenting symptoms and the classic features of typical angina. Data Source: Exercise stress test report Data Entry: Enter value between –25 (highest risk) and +15 (lowest risk) Add other options in a dropdown format: o Not applicable as appropriate assessments were not performed to compute DTS o Not documented / unknown * OTHER ASSESSMENTS: SELF-REPORTED HEALTH BEHAVIOURS & RETURN TO WORK The following measures are recommended at program intake and discharge. 29 Copyright © Canadian Association of Cardiovascular Prevention and Rehabilitation 2014 To be used with permission only. Not for re-distribution Physical Activity -Total Canadian Physical Activity Guidelines recommend that individuals accumulate at least 150 minutes per week of moderate-to vigorous-intensity physical activity, performed in 10 minute bouts or longer. Based on the last 7 day period, how many minutes does the patient report they accumulated of moderate-to vigorous-intensity aerobic physical activity per week (i.e., at least brisk walking), in bouts of 10 minutes or more? Data Sources: Initial intake and discharge visit, patient interview/questionnaire. Patient asked to describe their physical activity level. Data Entry: enter number of minutes Unknown: Not documented Physical Activity -Frequency Based on the last 7 day period, how many days does the patient report they engaged in moderate-to vigorous-intensity aerobic physical activity (i.e., at least brisk walking)? Data Sources: Initial intake and discharge visit, patient interview/questionnaire. Patient asked to describe their physical activity frequency. Data Entry: enter number of days Unknown: Not documented Resistance Training Canadian Physical Activity Guidelines recommend that individuals perform resistance training using major muscle groups for at least two days per week to add muscle and strength. Based on the last 7 day period, does the patient report that they perform resistance training at least two days per week? Data Sources: Initial intake and discharge visit, patient interview/questionnaire. Patient asked to describe their strength training routine. Data Entry: Yes – The patient reports that they perform resistance training at least two days per week. Partial – The patient reports that they perform resistance training, but not two days per week. No - The patient reports that they do not engage in strength training or the patient’s strength training cannot be determined by the sources defined or the reliability of the information is questionable. Unknown: Not documented Smoking Does the patient smoke at the present time (intake and discharge)? Note: pertains to cigarette, cigar and pipe smoking Data Entry: Choices available are (CCS): Never = no history of any form of tobacco, Current = use of any form of tobacco (cigarettes, cigar, pipe) within one month of referral date, Former = use of any form of tobacco > one month of referral date, 30 Copyright © Canadian Association of Cardiovascular Prevention and Rehabilitation 2014 To be used with permission only. Not for re-distribution Unknown: Not documented Dietary - % Kcal saturated fat Use the results from a standardized, validated tool or assessment by a registered dietitian for estimating the percentage of daily calories as saturated fats (AACVPR). Data Entry: Report value to the nearest whole number. Add other options in a dropdown format: Unknown: Not documented Daily fruit/vegetable servings Self-reported daily fruit and vegetable servings / day. Report value to the nearest whole number (AACVPR). Data Entry: Report value to the nearest whole number. Add other options in a dropdown format: Unknown: Not documented Employment Status Select the most appropriate response to describe the patient’s employment status at the time of intake to and discharge from cardiac rehabilitation. Note: Participation in the labour market takes precedence e.g. code as ‘part-time’ if an individual is both a student and is employed part-time. (CCS) Data Source: Admission history, History and Physical, Consultant’s notes, Nursing Admission note, Intake Assessment. Data Entry: Available choices are: Employed full-time, that is 35 or more hours per week Employed part-time, that is, less than 35 hours per week Self-employed (primary occupation) Unemployed, but looking for work Student Retired Not in the paid workforce (homemaker, unemployed, not looking for work) On disability Other Unknown: Not documented Desired Occupation Status Achieved Was the patient’s desired occupational status achieved by discharge from cardiac rehabilitation? Data Source: Discharge assessment/interview, patient’s chart. Data Entry: Indicate: Yes - patient achieved his/her desired occupation status by discharge No - patient did not achieve his/her desired occupation status by discharge Not applicable Unknown: Not documented 31 Copyright © Canadian Association of Cardiovascular Prevention and Rehabilitation 2014 To be used with permission only. Not for re-distribution Work Return Date Date that patient returned to work, if applicable. Data Entry: Write in date: Add other options in a dropdown format: - Not applicable – patient retired or on long-term disability - Unknown: ‘Not documented’ PSYCHO-SOCIAL INDICATORS The following measures are recommended at program intake and discharge. DEPRESSION Because the HADS-D costs money to administer and the BDI-II is used more as a research tool, in this iteration of the data dictionary we are recommending administration of the PHQ-2. It is recommended as a screener by AHA (Lichtman et al., Circulation 2008), and also as an option for screening in the CCS CR Quality Indicators. PHQ-2: Ask the patient: over the past 2 weeks, how often have you been bothered by any of the following problems? 1. Little interest or pleasure in doing things 2. Feeling down, depressed or hopeless Response options are: not at all (0), several days (1), more than half the days (2), nearly every day (3). Measure Performed Was a depression measure administered? Data Entry: Choices available are: Yes No Unknown: Not documented Measure What tool was used to measure depression? Data Entry: Choices available are: Hospital Anxiety & Depression Scale Depression Score (HADS-D) Beck Depression Inventory (BDI-II) PHQ-2 Other Unknown: Not documented Measure Score What was the score of the depression measure? If the PHQ-2 was used, please add up the number corresponding to the patient response to questions 1 and 2. Data Entry: Enter the numerical value. 32 Copyright © Canadian Association of Cardiovascular Prevention and Rehabilitation 2014 To be used with permission only. Not for re-distribution Add other options in a dropdown format: o Unknown: Not documented At or above cutoff Was this score at or above the cutoff for depression? For the PHQ-2, the cut-off is 3. Data Entry: Choices available are: Yes No Unknown: Not documented QUALITY OF LIFE We suggest administering the 1-item Ladder of Life (Cantril H. The pattern of human concerns. New Brunswick: Rutgers University Press, 1965.; see also Jaarsma et al., Measuring quality of life in heart failure: one versus multiple items. Neth Heart J: 2005; 13:338-42). Measure Performed Was a QOL measure administered? Data Entry: Choices available are: Yes – Ladder of Life Yes – SF-12 Yes - other No Not documented / unknown SF-12 Score What was the score of the SF-12 measure? Data Entry: Enter the numerical value. Add other options in a dropdown format: o Not documented / unknown Ladder of Life Here is a picture of a ladder. The top of the ladder represents the best possible life and the bottom the worst for you. Where on the ladder do you feel you personally stand at the present time? 10 BEST POSSIBLE LIFE 9 8 7 6 5 4 3 2 1 33 Copyright © Canadian Association of Cardiovascular Prevention and Rehabilitation 2014 To be used with permission only. Not for re-distribution 0 WORST POSSIBLE LIFE Data Entry: Enter the numerical value from 0 - 10. o Unknown: Not documented MEDICATIONS Enter all prescribed medications at intake and discharge from the CR program. Intake medications could be those documented at the intake assessment or intake functional testing. Discharge medications could be those documented at the time of the exit Functional Test or during the Exit Assessment. Be sure to include any diabetic or anti-depressant agents. Contraindicated Medications Does this patient have any contra-indications to cardiac medications? Data Entry: Choices available are: Yes No Unknown Not documented/ unknown Contraindication class If patient has a contraindication, to which class of drug? Data Entry: Choices available are: Statin Beta-blocker Aspirin Other Not applicable Not documented / unknown Medication Class Indicate the therapeutic class of the medication(s). Data Entry: All of the following classes should be reported, where prescribed: angiotensin converting enzyme inhibitors, angiotensin II inhibitors, ARBs, centrallyacting antiadrenergic agents, peripherally-acting antiadrenergic agents, antianginal agents, antiarrhythmic agents, anticoagulants, antihypertensive combinations, bile acid sequestrants, calcium channel blocking agents, cardioselective beta-blockers, fibric acid derivatives, HMG-CoA reductase inhibitors, inotropic agents, loop diuretics, miscellaneous antihyperlipidemic agents, non-cardioselective beta blockers, platelet aggregation inhibitors, potassium-sparing diuretics, salicylates, sulfonylureas, thiazide diuretics, thiazolidinediones, vasodilators. Diabetes drugs should also be reported: metformin, DPP4’s, LLP-1s, insulins. 34 Copyright © Canadian Association of Cardiovascular Prevention and Rehabilitation 2014 To be used with permission only. Not for re-distribution Name Choose the generic and brand name of all cardiovascular-realted medications the patient is prescribed at intake and discharge. Data Entry: Please see Appendix A for the list of medications and therapeutic classes. - Include option for unknown / Not documented Dose, units Indicate the doses of all noted medications. Data Entry: Enter numeric value. Indicate the medication unit(s) of the dose(s). Data Entry: Choices available are: mg ug g U mL mg/hr packet mg/day ug/day Not documented / unknown Frequency Indicate the frequency that the patient was prescribed to take the medication(s). Data Entry: Enter the number of times per day that patient was prescribed to take the medication(s). Indicate the medication schedule (frequency and/or time of day). Data Entry: Choices available are: od qam ac breakfast ac lunch qpm ac dinner qhs bid tid qid tid on a qid schedule on in am, off at bedtime q 5min x 3 prn od prn as needed (max 20 pieces/day) as needed (max 80 sprays/day) as needed (6-16 cartridges/day) 35 Copyright © Canadian Association of Cardiovascular Prevention and Rehabilitation 2014 To be used with permission only. Not for re-distribution q4h prn Not documented / unknown NOTE: By clicking “»” next to each medication on the Medication home screen, the exact same information will populate the Discharge medication list. This is useful for medications and dosages that do not change from intake to discharge from the CR program. Vitamins Is the patient taking any vitamins? Data Entry: Choices available are: Yes No Unknown/not documented Herbal / complementary or alternative pills Is the patient taking any herbal or unprescribed non-evidence-based therapies? Data Entry: Choices available are: Yes No Unknown/not documented 36 Copyright © Canadian Association of Cardiovascular Prevention and Rehabilitation 2014 To be used with permission only. Not for re-distribution