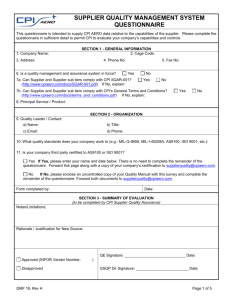
Medical Record Audit Form
advertisement

Medical Record Audit Form Patient MR# ____________ Sex___________ Age _______ Procedure Date ______________ Procedure ______________ Y = Yes Physician ___________________ N = No N/A= Not Applicable Administration Advance Directive Y or N, if Yes or No a copy in chart or patient did not bring Signed acknowledgment of PT rights Pre-Op Operative consent signed and witnessed. Allergies documented in pre-op Phone call. Record, Orders, and Med Rec Pre-op orders signed, dated and timed Laterality and type of anesthesia marked on orders Height and Weight documented on pre-op record If HVG box checked, a result noted on record If a blood glucose performed the time is was performed is documented If patient has an IV, it is documented they have a hep lock or fluid, and an order If IV fluid ordered, documented rate, and amount patient received in Pre-op All medications given have an order Medication route and time completed Peri-Operative Documentation of “time out” procedure Allergies documented on Operative record Procedure performed laterality marked on operative record Surgery check list complete Pain level assessed and documented. Use of approved abbreviations only. Operative record includes procedure, prep, pre-op dx and post procedure dx Operative report note dictated, transcribed and signed Operative record indicates times for start, finish, and out of room PACU Vital signs taken upon admission to PACU Vital signs taken every 15 minutes x 2 and every 30 minutes until discharge Vital signs documented within 10 minutes of discharge Med Rec form completed, eye drops present, added prescriptions present Discharge order is timed after case finish time on operative record Discharge instructions given and documented Documented patient fluids and denial of N&V Patient met discharge criteria Discharge medication addressed including any RX and documented on Med Rec form with how prescribed (paper vs called in) Patient discharge with an adult and documented, except for YAGs as applicable (verify order for no driver on YAGs) Anesthesia Anesthesiologist pre-op evaluation immediately prior to surgery noted. Anesthesia record complete. Required signatures of MD and CRNA present, and dated. Discharge note present. Post-op assessment present and timed Post-op Phone Call Post-op phone call complete All issue documented Follow up documented Medical Record Reviewer Initials: ____________ Date: ____________ Action:_____________________________________________________________________________________________ Follow-up: __________________________________________________________________________________________