standardization 2 - MidWest Clinicians` Network
advertisement

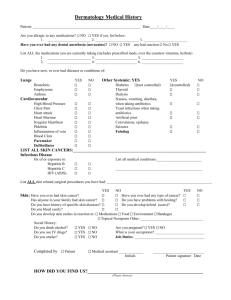
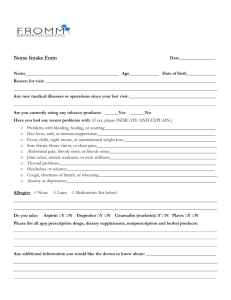
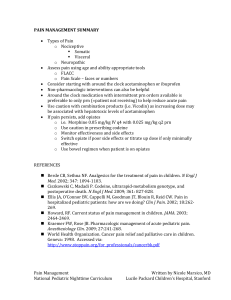
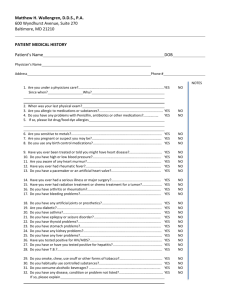
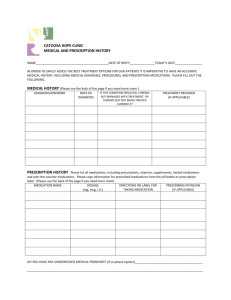
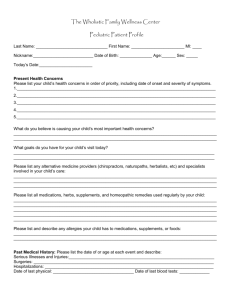
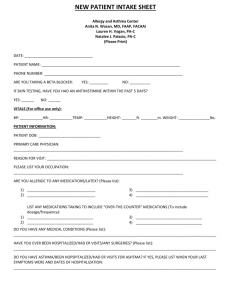
Health Delivery, Inc Core Competencies for Medical Assistants Competency Statement A. Gathers Clinical Data and Accurately Documents that Information in the Patient’s Medical Record Compliance Criteria Obtains: 1. Vital signs 2. Chief Complaint 3. Allergies 4. Patient history 5. Current medications 6. Risk Factors Requirements for Competency Completion/ Notes 1. Vital Signs include: Weight is to be obtained on every patient at every visit. Pediatric patients must be weighed in dry diaper and no more than an undershirt. Height is to be obtained yearly on adult patients and every visit on pediatric patients. Height is only to be obtained without shoes on using a stadiometer or infant measuring board. Temperature is be measured on every patient at every visit Pulse is to be measured on every patient at every visit. Respirations are to measured on every patient at every visit Blood Pressure is to be obtained at every visit starting at 3 years of age. Proper cuff size and placement is required. Blood pressure is to be last vital sign checked to allow for patient to have rest time prior to measurement. Head Circumference is to be measured on every pediatric patient at every visit up to age 2 years. Pain Level is to be obtained at every visit using a 0-5 rating scale. Documentation includes location, description, duration and chronicity 2. Chief complaint is to be completed at every visit and must include the specific reason for the visit. 3. Allergies are to be reviewed and updated at every visit for every patient 4. A complete history is to be collected at every new patient visit or when it has not been previously done. The history is to be reviewed at every visit. Complete history includes Past Medical History, Surgical History, Family History (includes parents, siblings, grandparents, and children of the patient), Social History, and menstrual history (if applicable). 5. The medication list is to be reviewed at every visit. Do not remove any medications from the list. If the patient is not taking a medication that is on the list add text to the note that reflects that information. Every patient (or parent of a pediatric patient) is be asked if they are taking any over the counter and or herbal supplements or medications. Changes to the medication list to reflect prescriptions from hospitals, specialist, etc are to be done only after review of the notes by the provider. 6. Risk factors are to be assessed for every new patient or if they have not yet assessed on 7. Smoking Status 8. Health Maintenance B. Maintains Documentation in the Medical Record to Ensure Accurate and Complete Tracking of the Patient’s Medical Treatment Completes 1. MCIR documentation 2. Patient notification of test results 3. Proper chart documentation related to but not limited to a. Patient care b. Telephone contact 4. Tracking/ Order completion 5. Forms 6. Order entry an established patient. Review of the risk factors is to be done at least yearly. Assessment includes alcohol use, drug use, and sexual history. 7. Smoking status is to be assessed at every visit. Information regarding smoking cessation is to be provided to every smoker at every visit. 8. Reviews the Adult Male/Female Intake form and addresses the need for health maintenance testing or immunizations. Initiates orders for all items. 1. Vaccines must be entered into MCIR within 72 hours of administration. 2. Refer to HDI policy CLIN.79 4. Tracking is to be completed as reports are received. Incomplete orders are to be addressed at least monthly. 5. All forms are to be completed with all/ any available information prior to delivery to a provider. 6. Responsible for entering orders for any completed testing during an office visit or any needed health maintenance measures. Collects 7. ER visit notes, diagnostic test results, specialty notes prior to patient visits 8. Information from patient regarding other health care providers that the patient has seen C. Provides Patient Education as Directed and Documents Appropriately in the Patient Record D. Prepares and Administers Medications and Immunizations 1. Advanced Directives 1. Advanced Directives are to be addressed and documented per HDI protocol CLIN.47 2. PCMH 2. Must be able to accurately provide PCMH information to patients. 1. Properly prepares medications and vaccines. 2. Administers medications and immunizations according to policy/ protocol. 3. Recognizes and reports adverse drug reactions. 2. Refer to CLIN.61 Controlled Substance Documentation and Storage Protocol. Medications and immunizations may be administered per provider order at a visit, standing order, or per protocol. E. Follows Procedures for Collecting and Handling Various Specimens and Cultures F. Properly Uses and Maintains Equipment Used for Providing Patient Care G. Performs Tests and Quality Controls for CLIA Waived Testing 4. Administers medications/ vaccines via: a. Subcutaneous injection b. Intramuscular injection c. Intradermal injection d. Dropper e. Oral administration f. Sublingual administration g. Nebulizer 1. Throat 2. Wound 3. Stool 4. Urine 5. Sputum 6. Genital 7. Blood via venipuncture 8. Blood via capillary sampling 1. Scales (Adult and Infant) 2. Stadiometer/ Infant measuring board 3. Thermometer 4. Pulse Oximeter 5. Oxygen tank, nasal cannula, masks 6. Nebulizer and tubing 7. Spirometer 8. Hemocue 9. Tympanometer 10. AED 11. Ear Irrigation System 12. Cryosurgical System 13. EKG 14. Refrigerator/ Freezer 1. Glucometer blood sugar 2. Urinalysis 3. Hemoglobin A1c 4. Hemocue hemoglobin 5. Rapid strep 6. Monospot 7. Rapid HIV 8. Cholesterol 1-10 Must be able to perform test and quality controls per manufacturer instruction. Tests are to be done in anticipation of need based on the patient’s chief complaint or per protocol. Refer to In-House Lab Test Reference sheet, CLIN.68, CLIN.13., CLIN.43 H. Prepares and Assists with Procedures I. Performs Additional Testing or Screening per Protocol or Provider Order J. Follows Instrument Sterilization Protocol K. Properly Handles Patient Prescriptions L. Respond to and Initiate Written Communication 9. Hemosure iFOB test 10. Urine pregnancy 1.Initiates consent process 2. Maintains sterile field Sets up for and participates in procedures including but not limited to: 3. Lesion removal 4. Mole excision 5. Colposcopy 6. Pelvic Exam (with and without PAP) 7. Biopsy 8. Toenail Removal 9. Wound Care 10. IUD placement and/ or removal 11. Implanon insertion/ removal 1. Snellen vision testing 2. ASQ-3 and ASQ-SE developmental screening 3. PHQ-9 1. Prepares instruments for autoclaving 2. Properly operates and maintains the autoclave. 1. Calls in medications appropriately to pharmacies 2. Appropriately routes prescription requests via the EMR 3. Properly prepares and routes medication refill requests for provider review 4. Initiates and follows up on prior authorizations as requested by a provider. 1. Compose and respond to flags in the EMR 2. Compose and process patient 1. Refer to In-House Test Reference 1.-2. Refer to HDI policy CLIN.19 M. Practice Standard Precautions N. Prepare and Maintain Examination and Treatment Areas O. Accurately and Appropriately Accesses Computer Systems letters in the EMR. 1. Hand washing 2. Removing contaminated gloves 3. Disposal of biohazardous materials 4. Possesses knowledge of procedure to follow in the event of an exposure. 1. Room Stocking 2. Anticipate provider needs for visit, obtain all necessary supplies. 1. Scheduling appointments in the Centricity system 2. Accesses MCIR 3. Accesses hospital systems to obtain patient records 6/20/2012 4. Refer to HDI policy CLIN.11 2. MCIR reports are to be available for every pediatric patient at every visit.