Chromium Debate Paper
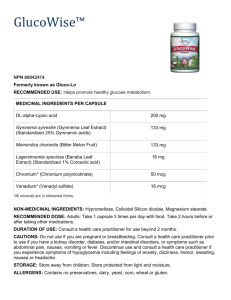
advertisement

Danielle Taylor Chromium is an abundant element found in nature in a variety of forms, mainly as metallic chromium (Cr0), trivalent chromium (Cr3+), and as hexavalent chromium (Cr6+) (1). Chromium is found in a variety of foods such as meats, poultry, grains, cheese, dark chocolate, certain fruits and spices, tea, beer, and wine as trivalent chromium (2). Chromium supplements are advertised to have health benefits for glucose metabolism, increased insulin action, increased muscle mass, weight control, and diabetes prevention and it was estimated that in 2002 “…sales of chromium-based supplements was $85 million” (3). The interest in chromium supplementation began in 1977 when it was reported by Jeejeebhoy et al that a patient receiving total parenteral nutrition (TPN) developed diabetic like symptoms such as impaired glucose tolerance, weight loss, and neuropathy and required exogenous insulin was given supplemental chromium (4). After receiving the chromium supplements the patient’s symptoms were eliminated and exogenous insulin was no longer needed (4). Since this was reported, numerous other studies have proven similar findings and chromium is now added to TPN solutions (1). This study established the possible link between chromium and its biochemical role in those with diabetes. Although it remains a controversial topic, it has been shown that specific dosages of chromium are a safe and effective treatment for achieving glycemic control in a number of specific populations. Once ingested, trivalent chromium binds to a variety of ligands including amino acids and picolinate. This interaction increases the solubility and absorption of the chromium. It has also been found that vitamin C can increase chromium absorption. It is thought that chromium is absorbed in the jejunum of the small intestine either by diffusion or by a carrier-mediated transporter. In supplements chromium is available as chromium chloride, chromium picolinate, or combined with acetate, nicotinic acid or with amino acids. Once chromium has been absorbed, it binds to transferrin, albumin, globulins, or lipoproteins in the blood and is transported to cells (2). After insulin is released, chromium bound to transferrin binds to transferrin receptors on the surface of cells and is endocytosed into the cell. Due to a decreased pH inside the cell, the chromium is released from the transferrin molecule (1). Chromium then binds to an oligopeptide of glycine, cysteine, aspartate, and glutamate called apochromodulin converting apochromodulin to holochromodulin or chromodulin (2). Chromodulin then binds to the insulin receptor and activates tyrosine kinase activity. “The result of this process is the activation of insulin receptor kinase and potentiation of the actions of insulin” (1). The activity 1 Danielle Taylor of insulin is also enhanced as chromium inhibits phosphotryosine phosphatase, an enzyme that normally decreases insulin sensitivity (1). Due to the chromium involved mechanisms that increase the activity of insulin along with the fact that those with diabetes are found to have increased chromium excretion rates, chromium supplementation has and is continuing to be extensively researched for its application as a treatment in those with type 2 Diabetes Mellitus (DM) (5). The current research on chromium supplementation demonstrates the variety of conclusions on the effectiveness of this supplement. One of the main causes for the discrepancies is the form of chromium used in the study, usually either chromium picolinate or chromium chloride, and the dosage of the supplement administered. As mentioned previously, chromium is often bound to ligands to increase it solubility. Picolinate is a ligand that is lipophilic, which allows the chromium bound to the picolinate to be absorbed through cell membranes. Chromium picolinate is absorbed more efficiently than other chromium formulations and for this reason is often chosen for supplementation experiments. It has been reported that chromium picolinate may cause chromosomal damage, renal failure, and hepatic dysfunction at certain concentrations (2). On account of these potential toxic side effects, other researchers have used chromium chloride supplements. Chromium chloride is not absorbed as efficiently as chromium picolinate in the body, but it is considered less toxic. In 1997 Jovanovic et al published a paper demonstrating the effect of chromium picolinate supplementation on both glucose and insulin variables in individuals with type 2 DM. One hundred eighty individuals were randomly assigned into three groups: placebo, 200 g/d chromium picolinate, or 1000 g/d chromium picolinate. Participants ingested tablets either containing chromium picolinate or the placebo twice per day for 4 months. The fasting blood glucose, fasting insulin, hemoglobin A1C (HbA1C), total cholesterol, HDL cholesterol, and triglycerides were measured before the study began, after two months, and after 4 months. Researchers found that both dosages of chromium picolinate improved fasting insulin and fasting glucose concentrations. HbA1C is used to more accurately measure changes in the blood glucose levels over time. The HbA1C levels measured correlated with the glucose and insulin measurements and was decreased in those receiving the chromium supplements. The researchers concluded that although results were seen in the 200 g/d group, it did not seem to be the optimal dosage since greater effects were observed in the 1000 g/d group. A potential criticism of this article is the possible harmful side effects 2 Danielle Taylor associated with intakes of chromium picolinate (5). A article by Pei et al in 2006 referenced an article by DR Mattews et al in 1985 that 400-600 g/d chromium picolinate has been shown to improve insulin sensitivity and lower blood glucose and HbA1C levels (6). It is evident from this study that more research needs to be done to determine the optimal dosage of chromium picolinate supplements, but the chromium picolinate can aid in glycemic control in those with type 2 DM (5). Another study was published in 2006 by Pei et al that analyzed the effect of chromium chloride supplementation in those with type 2 DM. Sixty participants were divided into two treatment groups: placebo and 400 g/d chromium chloride milk powder. The groups were instructed to take the supplement twice per day dissolved in a glass of water for 16 weeks. Blood samples were drawn before the experiment began and after it concluded and it was discovered that the group receiving chromium chloride supplements had lower fasting plasma glucose, fasting plasma insulin, and HbA1C levels than the placebo group, specifically in male patients. It was reported that there were no adverse side effects in either treatment group except for mild constipation in the chromium chloride group. This paper concluded that chromium chloride supplementation of 400 g/d was a “…safe, effective, and well tolerated…” treatment for those with type 2 diabetes mellitus (6). Another paper discovered that doses of chromium chloride of 50-200 g/d did not significantly lower blood glucose in diabetic patients (6). The variation in the type of supplement used and the dosage given in experiments greatly effects whether a study produces encouraging data for those with diabetes or finds inclusive/absent results. The previously mentioned studies demonstrate that there are safe and effective chromium supplements for controlling blood glucose levels in those with type 2 DM at a dosage of 400-600 g/d chromium picolinate and 400 g/d chromium chloride. An essential component in analyzing whether chromium is an effective supplement for glycemic control is the population of people participating in the study. It has been found that chromium supplementation can work for specific populations but will have no effect on the blood glucose levels of nondiabetic people. Deficiencies in chromium have been show to result in diabetic like symptoms including weight loss, neuropathy, and elevated blood glucose levels. Studies have shown that chromium supplementation can help control blood glucose levels in those receiving parenteral nutrition and those with diabetes including gestational, corticosteroidinduced, and type 2 DM (1). A paper published in 1999 by Javanovic et al found that chromium picolinate supplementation improved glucose intolerance in women with gestational diabetes (7). 3 Danielle Taylor It has been shown that people with diabetes have higher chromium excretion compared to those without diabetes and those with diabetes can lose the ability to convert chromium to a useable form (5). The Jeejeebhoy article about a patient on TPN, the Anderson article about chromium picolinate supplementation, and the Pei article concerning chromium chloride supplementation mentioned previously all demonstrate the ability of chromium supplementation to control blood glucose levels in patients on TPN or with type 2 DM (4, 5, 6). A study by Ravina et al in 1998 revealed that urinary excretion of chromium increased after corticosteroid treatment and patients developed corticosteroid-induced diabetes with high blood glucose measurements. The researchers collected urine samples from 13 patients 24 hours before receiving a corticosteroid treatment of prednisone and then the three days following treatment. Chromium excretion in all patients except two increased from 115 +/- 28 to 244 +/- 33 ng/d after prednisone treatment. Upon observing these results, the scientists conducted a pilot study with three patients receiving prednisone treatments. The first patient had type 2 DM, was on haemodialysis for diabetic nephropathy, blind in her right eye from keratitis, and had macular neuritis on her left eye. She was given 60 mg of prednisone for treatment of her left eye. After two days of prednisone treatment, the patient’s blood glucose levels significantly increased. She was then given 600 g/d chromium picolinate taking 200 g with each meal. One week after beginning the chromium supplementation, the patient’s blood glucose level dropped from 15.5 mmol/l to 7.6 mmol/l. The chromium picolinate dosage was then decreased to 200 g/d and was able to control her diabetes. The second patient studied had terminal renal failure and was given 60 mg/d prednisone as an immunosuppressant after a kidney transplant. The patient’s body rejected the kidney and prednisone treatment was stopped after one week. After receiving the prednisone his blood glucose levels increased, when the prednisone treatment ceased his glucose levels returned to normal. After nearly 3 years the patient received a second kidney transplant, again receiving prednisone resulting in increased blood glucose levels. Ten days after the operation the patient was released from the hospital but quickly readmitted to the Diabetes Clinic with very high blood glucose levels despite exogenous insulin treatments. The patient was given chromium picolinate at the same dosage as the previously described patient, 600 g/d. Once the patients blood sugar was under control, the dosage was decreased to 400 g/d while the patient continued to take prednisone. The third patient in the pilot study had type 2 DM, which was controlled with metformin and 200 g/d chromium picolinate. After being hospitalized for a 4 Danielle Taylor glioblastoma, the patient was given dexamethasone, an immunosuppressant glucocorticoid, and 200 g of chromium three times per day. The patient’s blood glucose levels remained normal even though she was taking the dexamethasone. The three patients in the pilot study showed that blood glucose levels increase upon corticosteroid treatment but improved after administering supplemental chromium picolinate. The researchers have since treated 41 patients with steroidinduced diabetes with 200 g three times per day of chromium picolinate and have seen the diabetes eliminated in 38 of the 41 patients. A potential criticism of this article is the small patient size and the fact that it was not a placebo controlled study. The researchers state that “[d]ouble-blind, placebo controlled studies are needed to confirm these observations” (8) but that they have shown that corticosteroid treatment can increase chromium losses resulting in corticosteroid-induced diabetes that can than be alleviated by chromium picolinate supplementation (8). These studies show that chromium supplementation can be an effective solution for blood glucose regulation for specific populations of people including those receiving TPN, with gestational diabetes, type 2 DM, or corticosteroid-induced diabetes (4, 5, 6, 7, 8). Two main criticism surrounding the use of chromium supplementation for glycemic control is the number of studies with inconclusive or no results in patients receiving chromium supplementation and the possible toxicity of chromium. A number of studies that have found chromium supplementation to be ineffective in improving insulin sensitivity and blood glucose levels have been conducted in those who do not have DM. They have studied those thought to be at risk for DM of those with metabolic syndrome. A study conducted by Iqbal et al found that chromium picolinate supplementation of 1000 g /d did not have any significant change on insulin sensitivity in those with metabolic syndrome. The study states, however, that those with metabolic syndrome can have a wide range of insulin sensitivity levels and that “…only 52% of our metabolic syndrome subjects had impaired glucose metabolism…” (9). The purpose of chromium supplementation is to enhance insulin sensitivity, this treatment is not effective for those who do not have impaired glucose metabolism. Thus the study should have only seen results in 48% of its subject group if the supplementation was effective for all those with impaired glucose metabolism (9). A study by Ali et al in 2011 analyzed those thought to be at risk for DM stated that the researchers did not have “…a biomarker assessing serum chromium levels at baseline and during therapy” (3). This is a major flaw in this research because it has been found that those consuming adequate chromium from their diets will not respond to 5 Danielle Taylor additional chromium. “Chromium is a nutrient and not a drug, and it will therefore benefit only those who are deficient or marginally deficient in chromium” (6). It was also been found that stress or genetic diversity may result in ambiguity in the studies since both of these factors can influence chromium levels in the body (6). Another controversial topic concerning chromium supplementation is the possible toxic effects including DNA damage and renal failure from chromium picolinate supplementation. It has been shown that supraphysiological doses of chromium picolinate can cause DNA damage in cell culture studies, but there is still no evidence that chromium picolinate causes DNA damage in vivo. The relationship between chromium picolinate and renal failure is still unknown (1). Other scientists have researched the effect of chromium supplementation on Drosophila melanogaster (D. melanogaster) and shown that the hexavalent and tetravalent forms of chromium have recombinogenic activity while the trivalent form of chromium chloride found in supplements does not. The article stated none of the studies examined the effect of chromium picolinate on somatic cells so the comparison between D. melanogaster cells and mammalian cells could not be established (10). Since scientists discovered the ability of chromium supplements to reverse diabetic symptoms including the control of blood glucose levels in those receiving TPN in the 1970s, the debate has continued of whether chromium supplementation can be used to control glycemic levels in others. It has been discovered that those with type 2 DM and with corticosteroidinduced diabetes excrete chromium more rapidly than those without those illnesses making them more likely to be deficient in chromium (5, 8). Anderson, Pei, and Ravina have shown in clinical studies that supplements of 400 g/d chromium chloride or 200-600 g/d chromium picolinate are effective in controlling blood glucose levels in patients with type 2 DM or corticosteroid-induced diabetes (5, 6, 8). Although the topic remains controversial today, the majority of evidence seems to support the fact that chromium supplementation can be both a safe and effective treatment for glycemic control in either the chromium chloride or chromium picolinate form when given at the correct dosage to those with impaired glucose metabolism. 6 Danielle Taylor References 1. Cefalu, WT, Hu FB. Role of Chromium in Human Health and Diabetes. Diabetes Care. 2004; 27(11): 2741-2751. 2. Gropper SS, Smith JL, Groff JL. Advanced Nutrition and Human Metabolism. 5th ed. Belmont, CA: Wadsworth; 2009 3. Ali A, Ma Y, Reynolds J, Wise JP Sr, Inzucchi SE, Katz DL. Chromium effects on glucose tolerance and insulin sensitivity in persons at risk for diabetes mellitus. Endocrine Pract. 2011; 17(1): 16-25. 4. Jeejeebhoy KN, Chu RC, Marliss EB, Greenberg GR, Bruce-Robertson A. Chromium deficiency, glucose intolerance, and neuropathy reversed by chromium supplementation, in a patient receiving long-term total parenteral nutrition. The American Journal of Clinical Nutrition. 1977; 531-538. 5. Anderson RA, Cheng N, Bryden NA, Polansky MM, Cheng N, Chi J, Feng J. Elevated intakes of supplemental chromium improve glucose and insulin variables in individuals with type 2 diabetes. Diabetes. 1997; 46(11): 1786-1791. 6. Pei D, Hsieh CH, Hung YJ, Li JC, Lee CH, Kuo SW. The influence of chromium chloride-containing milk to glycemic control of patients with type 2 diabetes mellitus: a randomized, double-blind, placebo-controlled trial. Division of Endocrinology and Metabolism. 2006; 55: 923-927. 7. Jovanovic L, Gutierrez M and Peterson CM, Chromium supplementation for women with gestational diabetes mellitus. The Journal of Trace Elements in Experimental Medicine. 1999; 12: 91–97. 8. Ravina A, Slezak L, Mirsky N, Bryden NA, and Anderson RA. Reversal of corticosteroid-induced diabetes mellitus with supplemental chromium. Diabetic Medicine. 1999; 16: 164-167. 9. Iqbal N, Cardillo S, Volger S, Bloedon LT, Anderson RA, Boston R, and Szapary PO. Chromium picolinate does not improve key features of metabolic syndrome in obese nondiabetic adults. Metabolic Syndrome and Related Disorders. 2009; 7(2): 143-150. 10. Hepburn D, Xiao J, Bindom S, Vincent J B, O'Donnell J. Nutritional supplement chromium picolinate causes sterility and lethal mutations in Drosophila melanogaster. Proceedings of the National Academy of Science of the United States of America. 2003; 100(7): 3766-3771. 7