Acute Kidney Injury Stage 3 Outcomes following Intensive Care
advertisement

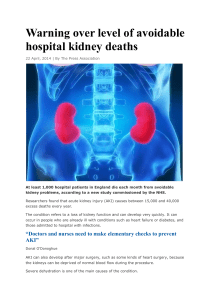
P25 Acute Kidney Injury Stage 3 Outcomes following Intensive Care Admission. A Single Centre Report Maharajan Raman1, Rajkumar Chinnadurai1, Samuel Niteh1, Rob Nipha1, Paul Ferris2 Department of Renal Medicine1 and Intensive Care Medicine2, Salford Royal NHS Foundation Trust Introduction: Acute Kidney Injury (AKI) is seen in about 5 -20% of acute hospital admissions. The mortality following AKI in the setting of sepsis and multi-organ failure could be as high as 50% or more. It is also associated with long-term consequences like Chronic Kidney Disease (CKD) and Dialysis, which has a significant impact on the health care system. AKI is preventable and recent National Confidential Enquiry into Patient Outcome and Death (NCEPOD) review stated that in 14% of the cases AKI could have been avoided. We aim to evaluate our performance against National outcomes Methods: Retrospective analysis of patients admitted to ICU between March 2013 and May 2013 who fulfilled the diagnostic criteria of AKI stage 3(AKI3). 190 case notes were reviewed which picked up 21 cases of AKI3. We measured against the criteria’s that were set out as early AKI management, subsequent AKI management and outcomes in the Acute Kidney Injury Audit of Outcomes and Care Processes, which was published in March 2013. Outcomes: 95% of the admitted patients were Caucasians. Senior review of patients within 12 hours was achieved in 90% of the cases. Urine dip was available only in 24% of patients. 80% of the patients had either an ultrasound or computed tomography (CT) of their abdomen. Imaging of the kidney was done within 12 hours in 24% of the cases. Early Warning Score (EWS) was implemented in 71% of the cases and 81% of them had a documented medication review. 43% of patients were discussed with Nephrology team. The average time for patient to be transferred to Intensive care unit was about 4 hours and during this period there was deterioration in EWS in 10% of patients but no deaths were reported while waiting for transfer. 24% of Intensive care admission required Renal Replacement Therapy. Patient’s kidney function one month after achieving the definition of AKI3 showed that 52% of them returned to their baseline, 19% of them to a level above their baseline and none of them were on dialysis. The in hospital mortality was about 19% and the mortality at one month was about 29% from the diagnosis of AKI3. The average length of stay in hospital was 22 days since the diagnosis of AKI3. The main presumptive causes of AKI are shown in the table 1. 60% 50% 40% 30% 20% 10% 0% Table 1: Presumptive causes for AKI3 Conclusion: The in-patient mortality rate following AKI3 in our study is lower than what is reported in literature, which is around 36%. This is perhaps due to evaluation of patients admitted to Intensive Care Unit with onsite Nephrology cover. Only 5% of the Nephrology referrals where accepted for transfer to the Nephrology unit. We plan to evaluate the outcomes of all AKI3 referred to this Nephrology unit and assess the need for an AKI care bundle, which in turn would help in early recognition and appropriate management of these patients.