Bay Street Pediatrics Book Excerpts
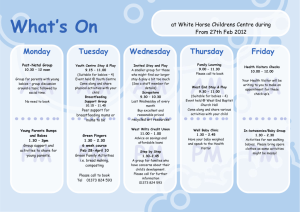
advertisement

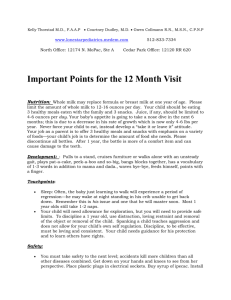
Excerpts from the Bay Street Pediatric Book Bay Street Pediatrics Associates offers complete care to infants, children and adolescents. Located in downtown Westport, we enjoy our convenient location and are lucky to be near ample parking. Our group was founded in 1978 and we pride ourselves on provide personal and friendly care while keeping abreast of the most current advances in pediatric health. We have close contacts with many pediatric specialists in the immediate area, as well as the New York and Yale-New Haven Children’s Hospitals. When necessary, our patients are admitted to Norwalk Hospital’s pediatric unit where nurses and physician’s assistants, trained in pediatrics, assist us in providing your child’s care. We see our hospitalized patients, as well as all newborns, on a daily basis. We pride ourselves on offering our families a small and warm practice where we can get to know each patient and their family personally. You may arrange well child physical exams with the doctor of your choice. We will try to accommodate your choice of doctors for sick visits as well, but please realize that it is not always possible. Extra time may always be scheduled in advance if a special issue arises. We hope you always find our office helpful and pleasant. Again, welcome and please feel free to contact us with any questions. OFFICE INFORMATION Hours of operation Monday - Friday 8:00am – 5:30pm Saturday 8:30am - Noon During office hours a registered nurse is always available to return phone calls. Please try to call early in the day if you think your child might need to be seen, so that we can schedule an appointment. The doctors are available to answer questions during the day as well, but usually cannot return non-urgent calls until the lunch hour or end of the day. We are always available after office hours for urgent problems. Please call our regular phone number and the answering service will forward calls to our physicians or the on-call covering physician group until 10pm. During other off-hours, our Pediatric Nursing Advice Line will answer questions and notify the on call physician of any urgent medical problems. Please call back if your phone call is not returned within 30-60 minutes. Occasionally, we are given the wrong phone number or some other issue arises preventing us from reaching you right away. Please also remember to unblock your caller ID. We ask that our patients please refrain from calling about routine issues after office hours. Prescription refills and non-urgent problems are time consuming tasks for a single physician who may be managing another child’s medical emergency and can be better handled when the office is fully staffed. Of note, "immunization only" visits can be scheduled with our nurses on Tuesdays - Thursdays from 9am - 11am and 2pm - 4pm. We accept patients from numerous insurance companies and send out claims on a weekly basis. We need to know immediately if there is any change in your insurance and expect copays to be made at the time of your visit. We accept Visa/MasterCard for those patients with private insurance, however, due to cost constraints, copays must be made by check or cash. GENERAL NEWBORN/EARLY INFANT CARE We realize that babies don’t come with instructions and that many new parents have questions. We provide this next section in hopes of answering some common newborn and childhood care questions. Please call the office if you have further concerns or questions. FEEDING: It is normal for well fed, healthy babies to lose 5-10% of their birth weight in the first few days of life. They should return to their birth weight by 2 weeks of age. Full term, healthy babies get all of the nutrition they need from breastmilk or formula. They do not need any supplementation until 4-6 months of age. In certain situations we might recommend vitamins and or fluoride for older infants. It is normal for babies to spit up/vomit a little after feeding. Babies should be burped in the middle of and after each feeding. We recommend introducing a cup at approximately 9 months of age and weaning your child totally off the bottle by 12 - 18 months. BREASTFEEDING: It takes time and practice for you and your baby to learn to breastfeed. Patience and relaxation are 2 important qualities you will need during this time. Please take advantage of the nurses and the lactation consultant in the hospital. They are valuable resources and can help you with many aspects of breastfeeding, especially latching on and positioning. Every full term healthy newborn has a built in 2-3 day food supply. Milk production usually "comes in" on the baby’s 3rd or 4th day of life. Initially, we suggest that you feed at least every 3 hours, or more frequently if the baby is fussy, until your milk comes in and then you can feed at least every 2-4 hours for 10-20 minutes a side. We recommend starting approximately 5 minutes per side and gradually increasing the time the baby feeds on each side. Frequent feedings help stimulate production of more milk. Drink at least 8oz of water every time your baby feeds. Water, prenatal vitamins and adequate nutrition (including 300-500 extra calories a day) are all you need to keep yourself healthy to continue to breastfeed. Please contact us if you are taking any regular medications. Helpful indications that your baby is getting enough to eat include: 6-8 wet diapers in 24 hours; 3-4 bowel movements in 24 hours; 8-12 feedings in 24 hours and audible sucking/swallowing at feedings. It is common to experience nipple soreness in the first week of breastfeeding. Correct positioning is the best prevention. Nurse on the least sore side first. You may apply a lanolin breast cream after feeding and wearing a good nursing bra is also important. You may choose to pump and store your breast milk. We recommend that you breastfeed exclusively until your baby is 2-3 weeks old and then introduce of the bottle, if you choose. Collect your pumped breast milk in plastic bags or a bottle/container marked with the date. We usually recommend storing 2-4oz per container. Expressed milk may be stored in the refrigerator for up to 72 hours and frozen for up to 3 months. You may defrost milk in the refrigerator (this usually takes about 12hrs) or by placing it in warm water. Hot water and microwaving can change the milk’s composition and have the potential to burn your baby. Never refreeze thawed breastmilk. The hospital and the office have literature on some common breastfeeding questions. We can also refer you to a lactation consultant for more complicated issues. FORMULA FEEDING: If you plan on formula feeding your baby, many formulas have been formulated to resemble breastmilk, for example Similac with Iron®. If there is a concern about cow’s milk based formulas, we will be happy to discuss soy-based formulas like Isomil®. Low iron based formulas are not recommended. Be sure that you are mixing formula correctly. Formula comes 3 ways: ready-to feed, concentrate and powder. Follow directions on the can closely for the latter 2. Formula can be mixed with unboiled tap water (well water should be first tested for safety). It can be given at room temperature or straight from the refrigerator (cold formula will not harm your baby). Never microwave formula and you should test the temperature on the inside of your wrist if you are warming it. Once opened or mixed, formula can be kept refrigerated for 48hours. It is not necessary to sterilize or boil bottles or nipples. Washing with soap and hot water or in the dishwasher is sufficient. At first, the average baby will feed ½-2 ounces every 2-3 hours and work up to 2-4 ounces per feeding by the 1st week of life. We recommend that children stay on iron fortified formula until 1 year of age and not start solid foods until 4-6 months of age. SOLIDS: The new recommendation from the American Academy of Pediatrics (AAP) is to delay solid foods until 6 months of age, especially in families with strong food allergies. At 4-6 months, we recommend starting with 1-2 tsp. of cereal (e.g. rice, barley, oatmeal) 1-2 times per day and then advancing to yellow vegetables, fruits then green vegetables, and finally meats. You may also gradually advance your child to 3 solid meals a day. We recommend not feeding your child egg yolks, citrus fruits/juices, berry fruits, shellfish and peanut butter until 1 year. Avoid feeding your child nuts, popcorn, sunflower seeds until 4-5 years of age due to the risk of aspiration. UMBILICAL CARE: We recommend placing rubbing alcohol at the base of the umbilical cord with every diaper change or at least 4 times a day. Do not be afraid to tug gently at the cord and get to the very base. This will help the cord dry and fall off and prevent infection. Call the office if there is any foul discharge or redness of the abdomen around the cord. Small amounts of blood are not unusual. You can expect the cord to fall off around 2 weeks of life, but it occasionally will remain attached a little longer. CARE OF GENITALIA: Circumcision care is relatively easy. You should put Vaseline or A&D ointment on your child’s penis with each diaper change to prevent his penis from sticking to the diaper. It is a normal part of the healing process for a yellowish membrane to appear on the circumcision a few days after the procedure. If your son is not circumcised, no special care is needed. Do not retract his foreskin until after 2-3 years of age (after which you may do so in the bath) to avoid causing adhesions. A whitish, thick vaginal discharge is normal for newborn females and at times it might be blood tinged. Wipe her vagina from front to back and avoid bubble baths to prevent vaginal irritation. It is also normal to see some enlargement of your baby’s breasts (male and female) during the first few months of life. This is due to maternal hormones and will resolve on its own. SKIN CARE: Until the umbilical cord falls off, babies may have sponge baths with a moisturizing, baby soap. Afterwards a baby tub is recommended. It is not necessary to bathe your baby daily, but it will do no harm. NEVER leave a baby unattended in the bathtub. A mild moisturizer (preferably non-scented) may be used as well as a non-talc baby powder. It is common for babies to develop a variety of different rashes for the first 4 months or so of life. If you have any questions about these rashes please call the office, especially if you notice blisters, pus or if the rash is associated with a fever. Parents occasionally complain of crusts or scales on their child’s scalp. This is probably what is known as cradle cap and can be treated by placing baby oil on the infant’s scalp about 1 hour before washing and then using a comb to brush out the flakes. After 4-6 months of age you may use a dandruff shampoo such as Sebulex® or Selsun Blue® 2-3 times a week. We recommend that all children be protected from the sun with proper clothing and a hat with a brim to keep sun out of their eyes. You should also use a PABA-free sunscreen with at least SPF-15 protection. The AAP now recommends sunscreen on infants less than six months if you are unable to cover exposed areas. DIAPER RASH: Babies commonly get diaper rash caused by irritation from urine, stool and occasionally reactions to diapers, wipes, etc. If diaper rash develops, change your baby’s diaper often and wash the area with water and a mild soap. Try to expose the rash to the air for some time and use a barrier cream (with zinc oxide). If the rash is not improving in 2-3 days or is spreading call the office. STOOLS: It is not the number of stools per day, but the consistency of the stools that is more important. Breast fed babies can have a stool after every feeding initially and then as they get older may have only one every 3-4 days. Many bottle-fed babies only have one stool a day. If the stools are watery (and more than approximately 10 a day) or if they are pebble-like and appear painful please notify the office. It is common for babies to strain when stooling (they don’t have gravity’s help). FUSSINESS/COLIC: It is unfortunately common for babies to have fussy times during their first few weeks home. This time can be extremely frustrating for parents, but try to be patient … colic usually peaks at 3-6 weeks and rarely lasts beyond 3 months of age. This period usually is in the evening and can appear as if the baby is having "gas pains" or is hungry. Overfeeding can worsen the problem. Frequently, parents find different consoling measures by trial and error. Motion, a warm towel on a lap with the baby lying with their abdomen down on the towel, or a pacifier are some examples. If the period of fussiness seems excessive or if you need some support please call the office. SLEEP: Newborns sleep an average of 16 hours a day and frequently confuse night with day at first. Try keeping the lights low and providing little stimulation at night. ALL INFANTS SHOULD SLEEP ON THEIR BACK (OR SIDE AS A SECOND CHOICE) until they are able to roll over on their own. Some other recommendations to decrease the chances of SIDS (Sudden Infant Death Syndrome) are: do not smoke or allow visitors to smoke in your house; avoid having your baby sleep in your bed; do not use pillows, heavy blankets or have many stuffed animals in the baby’s crib; and keep the baby’s room comfortably warm, but not too hot. A good resource for questions about SIDS is the Back to Sleep campaign line at 1-800-505-crib. OTHER GENERAL ADVICE FEVER: Fever is a sign of infection in children, but even a high fever is not dangerous in itself. Fever does not cause brain damage. It is the body’s way of killing viruses that can’t live at high temperatures. The height of your child’s fever is no indication of the severity of the illness. A sick newborn may not have a fever but show other signs of infection (poor feeding, lethargy) while an older child may have fevers up to 105 with a common cold. We are, however, concerned about RECTAL TEMPERATURES HIGHER THAN 100.4 IN INFANTS LESS THAN 2 MONTHS OF AGE because of their immature immune systems. Notify the office immediately if this occurs. If a fever of 101 or higher is making your child uncomfortable and they are not drinking well, we recommend treating it with acetaminophen every 4 hours. Encourage extra fluids!! If your child is still uncomfortable or the fever is still high after 30-60 minutes, you may give ibuprofen every 8 hours to infants older than 6 months (only if well hydrated). If a child is otherwise acting well, you can choose not to treat the fever. NEVER give a child aspirin. You may also try bathing with lukewarm water. NEVER use rubbing alcohol, because it can cause some young children to experience febrile convulsions with rapid rises in temperature. Try not to panic. These episodes usually last a few minutes. Place your child in a safe place where they will not get hurt and call us. If you have any concerns/doubts or if the fever is associated with other symptoms that make you worried, call the office. COLDS/COUGHS/CROUP: Most are caused by viruses and although scary, usually can be treated at home with symptomatic treatment. Examples include a cool mist humidifier, bulb syringe with saline nose drops, acetaminophen, and liquids. We, in general, do not recommend using antihistamine/decongestant medications in children younger than 2 years old due to increased side effects and decreased efficacy in children, but this should be discussed with each individual doctor. Many infections do not need to be treated with antibiotics. CALL THE OFFICE IF YOUR CHILD IS HAVING RAPID BREATHING, CHEST PAIN, OR LOOKS ILL. A "barky" cough and hoarse voice worsening at night is a common presentation of croup, a viral infection of the voice box/larynx. The symptoms usually last 5-7 days and can be improved either in a steamy bathroom or in the cool night air. Running a humidifier can also be helpful. CALL THE OFFICE IF YOUR CHILD LOOKS AIR HUNGRY, TURNS BLUE, HAS DIFFICULTY SWALLOWING OR DOESN’T IMPROVE WITH WARM MIST/COOL AIR AFTER 20 MINUTES. VOMITING/DIARRHEA: DIARRHEA is also frequently caused by a viral infection and can often be managed at home with proper treatment. The new recommendation from the AAP is that if your child is not dehydrated with his/her diarrhea, you may continue feeding an age appropriate diet as tolerated. This includes breastmilk, formula or regular milk; avoid fatty/greasy foods and fruit juices. Feeding the BRAT diet (bananas, rice, applesauce & toast) will not harm your child, but need not be your child’s exclusive diet. If your child has any of the signs of dehydration described below start feeding a glucose-electrolyte solution like Pedialyte® and call the office for further instruction. We do not recommend any antidiarrheal medications. Viral cases of diarrhea are frequently associated with VOMITING. The key to avoiding dehydration with vomiting is to feed small amounts of clear liquids frequently (even if it’s only a teaspoon at a time) and gradually increase the amount. In younger children and infants, you should use a glucose-electrolyte solution like Pedialyte® and then gradually advance to ½ strength formula and then full strength as tolerated. Exclusively breastfed infants should have shorter more frequent feedings and may return to a regular feeding schedule if they have no vomiting for 6-8 hours. Older children may have clear liquids, flat soda, Pedialyte® or frozen glucose-electrolyte popsicles for a few hours and if tolerated advancing to a bland diet. In both cases, it is crucial to assess the hydration status of your child. Call the office if your child has not urinated in 8 hours, had a dry mouth and no tears, is lethargic and not playful or shows any other troubling symptoms. TEETHING: Your baby’s first teeth may appear any time between 3 months and 1 year with varying degrees of discomfort and symptoms. We recommend first trying to massage the gums with your finger or letting your child chew on a smooth hard cool object (e.g. teething ring). If these interventions are not helpful, you may try a dose of acetaminophen every 4 hours as needed for 1-2 days. Special teething gels are not necessary, but if used should not be applied more than 4 times a day or for more than 1-2 days. SOME SAFETY INFORMATION Automobile/Bicycles: Your child should be seated in the back seat of your car until age 12. Infants must be in a rear facing car seat until they are 20 lbs. AND 1 year of age. From 20-40 lbs. they should be in a front facing, toddler car seat. They may move to a booster seat from 40-80 lbs. Once children are above 8 years old and 80 lbs. and above 4 feet 5 inches, they may be belted with an adult seat belt. Make sure you have properly installed your car seats!!!! Many towns have programs that will check that your car seats are properly installed. Contact the Fairfield County Safety Kids Program 203-325-5566 for information. Also remember children, by law, must wear correctly fitting bicycle helmets (including while rollerblading, skateboarding, etc.). Poisoning: As with all safety issues, prevention is the key to avoiding accidents. Make sure all of your medications and hazardous materials are out of reach of children and have safety caps. We recommend that you have a bottle of Syrup of Ipecac at home and that you call the poison control center in the event of an exposure/ingestion BEFORE using the Ipecac. POISON CONTROL CENTER 1-800-343-2722 The office can provide you with more information on safety!!!