Warfarin - Welsh Ambulance Service NHS Trust
advertisement

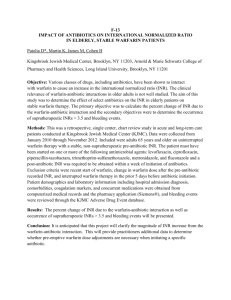
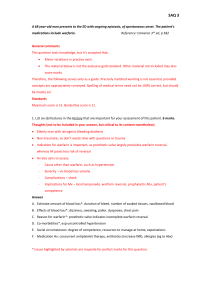
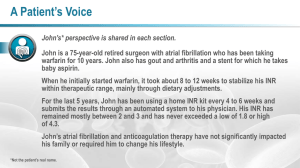
Warfarin - A Patient Information Guide 1|Page What is Warfarin? Warfarin is a drug used to ‘thin’ the blood. Warfarin is described as a blood thinner because it prevents blood from clotting in places where blood should not clot and it prevents existing clots from getting bigger. Why would I need to take Warfarin? Your doctor may prescribe Warfarin to prevent blood clots from forming. Blood clots can form in our bodies for a number of reasons. If a blood clot becomes lodged in a smaller vessel, this can lead to a stroke, a heart attack or a pulmonary embolus (a clot on the lung). All of these can be life-threatening and need urgent treatment. You may be prescribed Warfarin if you have a condition known as atrial fibrillation (an abnormal heart rhythm), or if you have an artificial heart valve. Blood clots can form if you have recently had a hip replacement or abdominal surgery. You could also develop a clot if you are sitting in one position on a long journey such as a flight, car, coach or train journey. Will I need any special tests? All patients taking Warfarin must have regular blood testing. The test is called INR (International Normalised Ratio). These monitor if the blood is too thick and sticky or too thin. The INR of a person who has not been on Warfarin is 1.0, therefore the higher the INR the, thinner the blood. It is important therefore to have close monitoring to measure the INR to see whether more, less or the same dose of Warfarin is required. This will probably be weekly initially and will gradually extend up to 8-12 weeks when stable. If you have not had your INR checked within the last 12 weeks then it is strongly advised that you get your INR checked within the next 7 days 2|Page What happens when I have my INR done? If you have the test at a clinic, a finger prick blood test is done to measure your clotting time (INR). Your GP may do a different kind of blood test where blood is taken from your arm. Identification You should be given Yellow Card, [anticoagulant treatment booklet] when you start treatment with Warfarin. This will contain details specific to your treatment including: The name of the condition requiring treatment The name of your anticoagulant Record of dosage (historic and current) INR (historic, current and target). Your target INR will vary depending on the reason for Warfarin being prescribed and you should be aware of your target INR Advice on your anticoagulant treatment. You should carry the yellow card with you at all times. What will my dosage be? The dose of anticoagulant that you need to take will depend on your INR test result. If your result is out of the range appropriate for your condition, your dose of anticoagulant will be increased or decreased accordingly. The anticoagulant dose required to achieve the target INR varies for each person. Does Warfarin come in different strengths? Warfarin tablets come in four different strengths and are colour coded to help you take the correct dose. Colours are as follows: White - 0.5mg Pink – 5 mg Blue – 3mg Brown – 1mg 3|Page When should it be taken? The dose should be taken regularly at the same time each day. What if I miss a dose? If a dose is missed do not take a double dose the next day. Just take your normal dose the next day. If more than one dose is missed; you should contact the surgery or clinic where you have your blood tests. Will other medicines affect the blood thinning effect of Warfarin? Yes, many medicines interfere with Warfarin. Always tell any doctor or dentist who is about to prescribe other medicine that you are taking Warfarin and do not take any non-prescription medicines without first checking with your doctor or pharmacist. If you are started on any new medication, including over the counter or herbal / alternative medication you must have your INR checked within 5 days. Speak to the Nurse or Doctor who takes your Warfarin blood tests. If you require pain relief, Paracetamol is advisable. If you require anything other than this, check with your pharmacy to obtain a suitable alternative. What should I do if I take too much Warfarin? Signs of having taken too much Warfarin could include bruising, nose bleeds and blood in the urine. Contact the clinic that monitors your blood for advice if you have any symptoms. If this happens outside of normal working hours e.g. in the evening or on a weekend, contact your GP out of hours’ service or NHS Direct Wales. Diet and Alcohol As Warfarin works by inhibiting the action of vitamin K, changes to your dietary intake of vitamin K can alter the effect of your Warfarin. For this reason, avoid making sudden major changes to your diet, particularly your consumption of green tea, salad and green vegetables (e.g., broccoli, brussel sprouts, or spinach), which contain large amounts of vitamin K. Large amounts of green vegetables (more than 500g daily) can reduce the effect of Warfarin and should be avoided. 4|Page Changes to your consumption of fats and oils can also alter the effect of Warfarin, as vitamin K is a fat soluble vitamin. The effects of Warfarin can also be altered by other foods, for example soya bean products can reduce the effect of Warfarin, and avocados and large amounts of ice cream (over a litre a day) have also been reported to have this effect. Cranberry juice should be avoided, as should large amounts of alcohol, as these may increase the effect of Warfarin. The effect of Warfarin can also be altered by sudden increases or decreases in your body weight. For these reasons you should avoid making sudden major changes to your diet during treatment with Warfarin. For more information, please speak to your pharmacist. If you drink alcohol, you should only drink small amounts and avoid binge-drinking, so that the alcohol does not have an adverse effect on your INR. Are there any risks if I take Warfarin? There are risks associated with taking all medicines. The main risk with Warfarin is bleeding. Usually this is a minor problem. For example, you may bleed for slightly longer if you cut yourself. However, sometimes the risk is high. Even if the risk is high, the risk of not taking the Warfarin and of a clot developing may be greater than the risks from taking Warfarin. It is important that you discuss the risks and benefits of taking Warfarin with your doctor. There is no increase in risk if you take Warfarin over a long period of time. In fact, the most difficult time is at the beginning when the doctors are trying to find the right dose for you. About 600,000 people in the UK take Warfarin. That’s about 1 in every 100 people. Out of these 600,000, each year 2 in every 100 will have a major bleed requiring hospital admission. About 1 in 100 may die from the bleed. However, the risk of having a major bleed is less than the chances of a fatal clot forming. 5|Page Is there anything else that could cause a problem? You should avoid contact sports if you take Warfarin, as they increase the risk of severe internal bleeding. If you are planning to become pregnant and you take Warfarin, you should discuss this carefully with your doctor before you become pregnant, as Warfarin can affect an unborn baby If you have any concerns you should not stop taking your Warfarin medication unless told to do so by your GP/Hospital Doctor 6|Page Useful organisations Anticoagulation Europe PO Box 405 Bromley Kent BR2 9WP Phone: 020 8289 6875 www.anticoagulationeurope.org British Heart Foundation Heart Help Line (For information and advice) 0300 330 3311 (Monday to Friday 9am to 6pm) www.bhf.org.uk Email: internet@bhf.org.uk NHS Direct Wales: Telephone: 0845 46 47 Minicom: 0845 606 46 47 Type talk: 1 8001 0845 46 47 Website: www.nhsdirect.wales.nhs.uk There is a Health Information Online enquiry and information prescription facility available on the website References: Net Doctor 2006. Marevan (Warfarin) [WWW] http://www.netdoctor.co.uk/medicines/100004290.html Hughes Jones S & Griffiths R (2008) Warfarin Therapy Information Sheet, North West Wales NHS Trust British Heart Foundation. 2007. Warfarin [WWW] http://www.bhf.org.uk/publications/view_publication.aspx?ps=1000763 National Patient Safety Association. 2008. Oral Anticoagulation Therapy. Important Information for Patients [WWW] http://www.npsa.nhs.uk 7|Page